The World Health Organization has declared COVID-19 as a pandemic. The health service is likely to face unprecedented pressure in the coming weeks to months as it battles to cope with the increased demand during the COVID-19 crisis. Hence, the requirement of the tertiary cardiac centers to formulate emergency plans in preparation for the impending surge in demand on the hospitals. As part of this preparation, the following document outlines a proposed strategy for the management of ST-elevated myocardial infarction (STEMI) and non-ST-segment elevation acute myocardial infarction (NSTEMI) patients during the COVID-19 crisis.
GENERAL PRINCIPLES
In order to minimize the spread of.... of infection when dealing with COVID-19 confirmed/suspected cases, the following are recommended: bypass the assessment area with full evaluation done in a designated cath laboratory, culprit vessel only to be done, and use of full personal protective equipment (PPE) as per local hospital policy and available guidelines.1
PROTOCOL FOR STEMI
Stage I (Prearrival)
This stage includes inquiry regarding COVID-19 status and evaluation for the current designated coronary care unit (DCCU) bed capacity. These are dedicated beds in the CCU for suspected/confirmed cases (Fig. 1).
FIGURE 1.
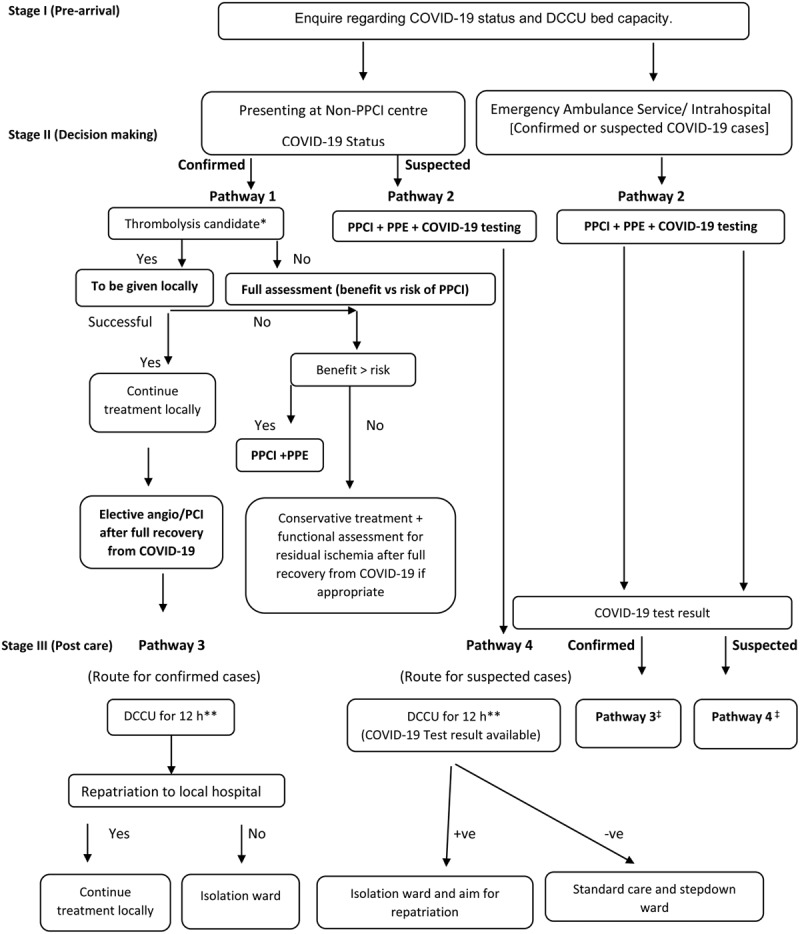
Proposed management strategy for STEMI patients. *Confirmation of wall motion abnormalities by bedside echo may be considered. **Twelve hours for uncomplicated cases. ‡No repatriation if patients present through emergency ambulance service or intrahospital.
Stage II (Decision-Making)
Patient Presenting at Local Nonprimary Percutaneous Coronary Intervention Center
COVID-19 Confirmed Cases (Pathway 1)
Thrombolysis suitable
Proceed for thrombolysis locally. In view of the recent reported cases of COVID- 19 induced myocarditis and possible microvascular obstruction and subsequent angiogram showing no thrombotic occlusion, a case by case discussion is advised and adjunctive bedside echocardiogram might help to confirm AMI. Then, reassess the outcome of thrombolysis. If thrombolysis is successful, treatment should be continued locally and plan for elective angiogram/percutaneous coronary intervention (PCI) after full recovery from COVID-19 infection. If thrombolysis is unsuccessful, comprehensive assessment should be done balancing...... the benefit versus risk of primary percutaneous coronary intervention (PPCI; case-by-case discussion):
◦ Benefit > risk: PPCI + PPE.
◦ Risk > benefit: Conservative treatment locally and functional assessment for residual ischemia after full recovery from COVID-19 if appropriate.
Thrombolysis non-suitable
Comprehensive assessment is balancing the benefit versus risk of PPCI (case-by-case discussion).
COVID-19 Suspected Cases (Pathway 2)
PPCI + PPE + COVID-19 testing.
Patient Presenting via Emergency Ambulance Service/Intrahospital Cases
Follow pathway 2 (COVID-19 confirmed or suspected cases).
Stage III (Postreperfusion Care)
Patients Who Presented Initially at Non-PPCI Center
COVID-19 Confirmed (Pathway 3)
Admission in DCCU for 12 hours is advised, then repatriation to local referring hospital for admission in isolation ward.
COVID-19 Suspected (Pathway 4)
Admission in DCCU for 12 hours is advised whilst awaiting COVID-19 test result. COVID-19 positive- transfer to isolation ward and then repatriation; COVID-19 negative - for standard care.
Patients Presenting via Emergency Ambulance Service/Intrahospital
Confirmed or suspected COVID-19 cases should follow pathway 3 or 4 respectively (no repatriation).
Postcardiac Arrest Patients
These are considered the highest risk group both from a cardiac and COVID-19 perspectives. Therefore, decisions need to be individualized, balancing the benefit versus risk of PPCI, mechanical ventilation need, availability of intensive care beds, and contraindication for thrombolysis.
PROTOCOL FOR NSTEMI
All patients with suspected COVID-19 and NSTEMI should be tested for the virus locally, if feasible. Where possible, the result should be awaited before cath laboratory transfer decisions are made. The proposed protocol is outlined in Figure 2.
FIGURE 2.
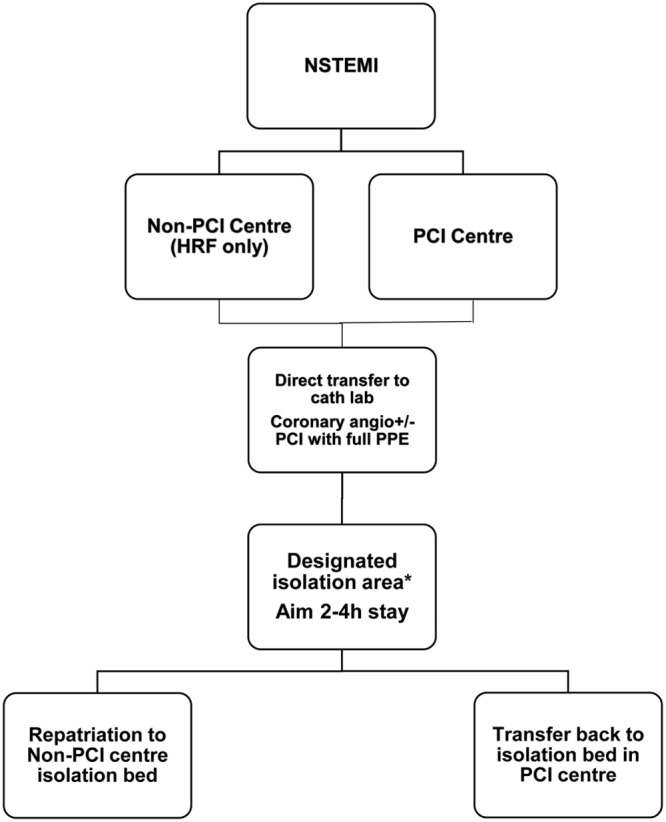
COVID-19 positive NSTEMI flowchart. *The designated isolation areas for postprocedure care would include DCCU (designated area on coronary care unit for out of hours), D1 (designated area near cath laboratory for COVID-19 confirmed patients within hours), and D2 (designated area near cath laboratory for COVID-19 suspected patients within hours in whom test results not back).
Patients Presenting at Non-PCI center
Routine transfer of NSTEMI patients to the tertiary center for PCI is discouraged, unless in high-risk features (HRF), in view of the risk of virus transmission between centers and to ambulance crew as well as the need to maintain staff and resources in the PCI center during the COVID-19 pandemic. HRF include:
◦ ongoing/recurrent chest pain and ECG changes;
◦ transient ST elevation;
◦ hemodynamic/electrical instability;
◦ left main ECG; and
◦ Wellen type ECG.
All other NSTEMI patients should be managed medically at their local hospital.
Patients Presenting Directly to PCI Center
We recommend treating all NSTEMI patients as per standard revascularization guidelines (priority for HRF). This will facilitate early discharge and hence free up bed capacity. This policy will need ongoing review and is likely to change with the epidemiologic dynamics of COVID-19 and might move to a situation where HRF only patients are taken to the cath laboratory.
DISCLOSURES
Nothing to declare.
REFERENCES
- 1.World Health Organization. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance, 19 March 2020. 2020.. World Health Organization; Available at: https://apps.who.int/iris/handle/10665/331498. Accessed 21 March 2020. [Google Scholar]


