Background
China confirmed person to person transmission of a novel coronavirus (now named SARS-CoV-2) on 21st Jan 20201 with more than 200 cases and 4 deaths. The World Health Organization (WHO) declared the COVID-19 outbreak as one of international concern on 30th Jan 20202. By 11th Mar 2020 the WHO Director-General declared the COVID-19 outbreak a pandemic with 118,00 cases in 114 countries and 4291 deaths3. COVID-19 is currently understood as a droplet spread illness with a reproduction number of approximately 2.24, transmitted via respiratory droplets, contact, fomites and fecal-oral routes5,6 and with high lethality (3.4%)7. Many more patients with COVID-19 than SARS (Severe Acute Respiratory Syndrome)8 have mild symptoms that contribute to spread as these patients are not picked up by current screening mechanisms9. The current outbreak is expected to last at least till the end of 202010 with the possibility of a second deadlier wave several months after the current outbreak like the 1918 Spanish Flu11. There is no known specific treatment or vaccine.
Challenges Facing ECT during COVID-19
This situation poses significant challenges for ECT services around the world. ECT is an essential psychiatric service that provides lifesaving treatment for severe mental illnesses like depression and catatonia if given in a timely fashion12,13 and for which there is no viable alternative. However, ECT service is often not prioritized in hospitals14 and may be stopped if anaesthesia resources are limited. This occurred at the beginning of the COVID-19 situation in a general hospital in Singapore, resulting in an acute ECT course stopping halfway for a patient with recurrent depression previously responsive to ECT. The team adjusted pharmacotherapy for the next two weeks before referring her to our ECT service. Unfortunately, the patient completed suicide 2 days before her scheduled ECT in our service. This tragic vignette underscores the importance of not just having an ECT service but having one that can respond in a timely fashion to patient needs. While 5 of the 7 ECT services15 in Singapore were still operational at the time of this writing, the other 2 have shut down due to lack of anaesthesia manpower while others now require case by case approval for ECT by the operating theatres.
There are other inherent challenges of an ECT service in a COVID-19 environment. ECT requires general anaesthesia which involves close contact with patient oral and airway secretions and actively encouraging the patient to cough in the recovery room after ECT. Each patient contact with the team can last for several hours in a small, confined environment with recirculated air and repeated 10 to 20 times over a period of weeks to months. Patients from a wide geographical region16 and are often kept in close contact in small rooms for several hours before and after ECT. Patients receiving ECT tend to be older14 and have a high chance of having comorbid medical conditions like hypertension or diabetes17 all of which increases their mortality if infected with COVID-197. Further, patients receiving ECT often have poorer hygiene18, live in crowded wards or housing19 and are hence less able to observe the recommendations of good personal hygiene and social distancing to prevent COVID-19 infection. This was sadly demonstrated in Korea by a COVID-19 super spreader infecting an entire psychiatric ward with COVID-1920. Other challenges facing ECT services include the common practice of a high rotation of ECT practitioners and anaesthetists within a single service which increases the risk of both ECT staff being infected by a large pool of high risk patients and infected ECT staff infecting other units when they rotate out of their ECT duties.
Common challenges facing ECT and other medical services in an COVID-19 environment include potential shortages of personal protective equipment (PPE) like N-95 masks, face masks, protective eye goggles, gowns and hospital grade disinfectants like 70% ethanol wipes21. An even greater challenge is the lack of manpower to have a full backup team or allow staff to rest sufficiently.
ECT in Singapore
Despite these numerous challenges it is possible to maintain a safe, high volume and high quality ECT service during a COVID-19 pandemic. COVID-19 was not Singapore’s first brush with a deadly coronavirus. In 2003 Singapore was struck by SARS (Severe Acute Respiratory Syndrome) caused by a novel coronavirus resulting in 238 cases and 33 deaths, including healthcare workers8. We learnt the importance of screening, contact tracing and isolation of cases and contacts to effectively manage a novel coronavirus22 outbreak. We also enhanced our institutional and national capability to deal with pandemics by establishing a national centre for infectious diseases (NCID) to provide infectious disease outbreak management and public health preparedness to strengthen Singapore's capabilities in infectious disease prevention and management. NCID became fully operational in 201823.
During SARS the ECT service in the Institute of Mental Health (IMH) was not prepared and had to shut down due to the need to protect staff and patients. At the time ECT nursing manpower came from over 10 different wards and the cross-contamination risk was assessed to be too high to continue and there was no contingency plan at the time to keep ECT operational during SARS.
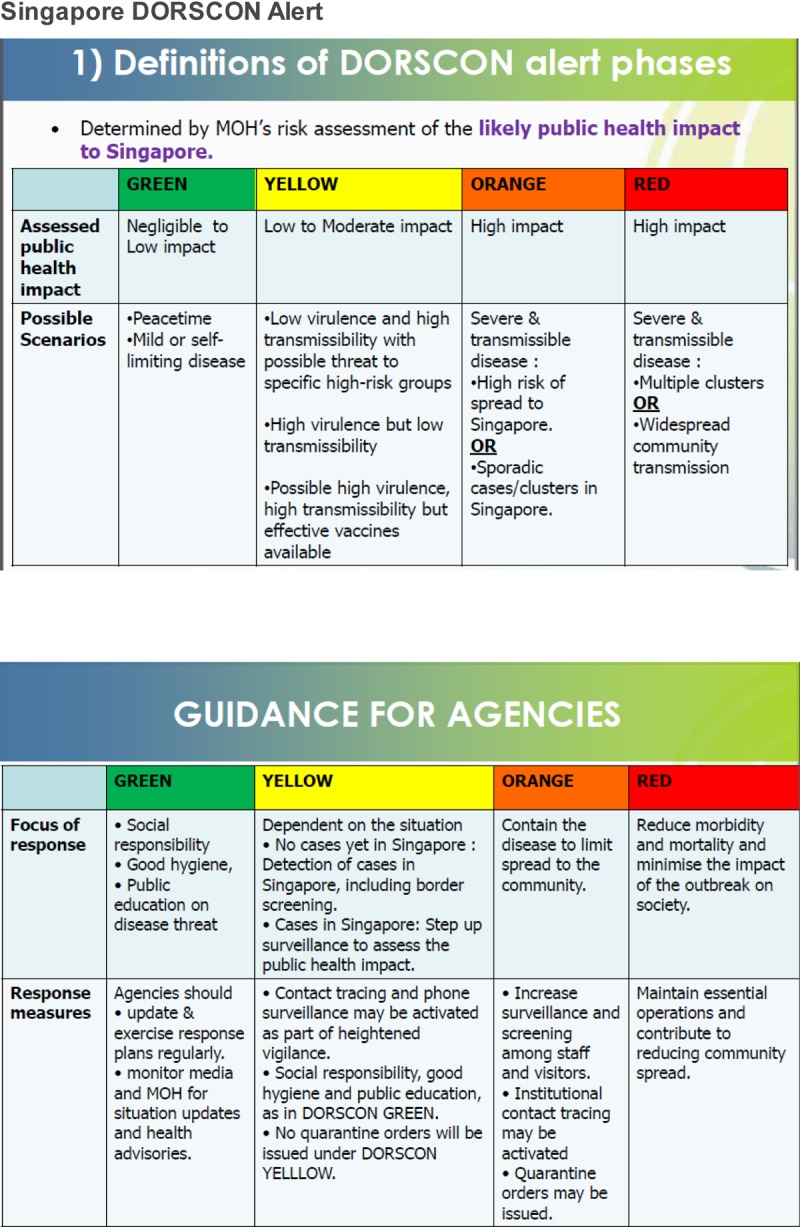
Singapore first heightened its awareness of the impending COVID-19 pandemic on 2nd Jan 202024, informing all healthcare providers to be vigilant about fever or acute respiratory cases with a travel history to Wuhan. Singapore diagnosed its first COVID-19 case on 23rd Jan 2020 with local transmission reported by 7th Feb 2020. The Disease Outbreak Response System Condition (DORSCON) alert was raised to Orange on 7th Feb 2020, indicating that the disease is severe and spreads easily from person to person but was not widely spreading and being contained25 (See Table 1 for details of DORSCON).
Table 1.
DORSCON Definitions and Guidance for Agencies
Singapore is a small nation state at the tip of the Malaysian archipelago. It has a population of approximately 5.5 million people consisting of 74.3% ethnic Chinese, 13.3% Malays and 9.1% Indian. The average per capita GDP in 2015 was USD $53,947.9326. The Mental Health (Care and Treatment) Act 27 directs all patients in Singapore requiring involuntary psychiatric admission to a single site, the Institute of Mental Health (IMH). Patients who are involuntarily admitted or assessed to lack capacity (as defined in the Mental Capacity Act 28 as the ability of the patient to understand the information, weigh up the information, remember the information, or communicate the decision) can be prescribed ECT by their treating psychiatrist. Singapore adopted a Whole-of-Government (WOG) approach with a multi-ministry task force coordinating all COVID-19 related activity. Specific measures that related to healthcare included travel restrictions placed on healthcare staff travelling to high risk areas, home quarantine for staff returning from high risk areas and restriction of practice locations to a single or limited number of sites for all healthcare personnel to reduce risk of cross-institutional transmission of COVID-1929. All healthcare staff were to take and document their temperature twice a day to monitor for symptoms of COVID-19 and mask fitting exercises (for N95 masks) for all clinical staff were completed in Jan 2020. All leave for healthcare staff was cancelled to facilitate business continuity plans (BCP) of having backup teams so that if a team member was infected with COVID-19, the alternative team would come to replace them while the exposed team would be put on quarantine30. Staff who could not get refunds for travel cancellations were reimbursed by IMH.
The Singapore Institute of Mental Health (IMH) is the only tertiary psychiatric hospital in Singapore with 1900 inpatient beds and about 40,000 outpatients and treats about 80% of the national load of psychiatric patients. In IMH, ECT is prescribed primarily for schizophrenia (47%) with schizoaffective disorder (20.3%), depression (20.4%) and mania (6.8%) being the other major indications15. In 2015 IMH moved from a one-size-fits-all approach (age based dosing with bitemporal electrode placement) to an individualized seizure threshold titration based approach31,32 with a range of electrode placements (Bitemporal, Bifrontal, Right unilateral) and pulse parameters (Brief or Ultrabrief pulsewidth) using the CARE network system to collect ECT data33. Treatment results at IMH for ECT have been comparable with international norms34–36. ECT was conducted over 3.5 days a week with an average of 15 treatments per half day session.
Adapting ECT to a COVID-19 environment
IMH set up a disease outbreak task force (DOTF) at DORSCON Yellow (1 level below Orange) in Jan 2020 to direct all COVID-19 activities in IMH after the Ministry of Health raised the alert on 2nd Jan 2020 of a possible new virus. The DOTF consisted of all senior management (CEO, Chairman Medical Board, Chief Operating Officer, Chief Nurse, Heads of Departments for all services, corporate communications, finance and human resources). The DOTF also had executive branches for coordination, infection control and audit and contact tracing. The standing daily agenda was a review of global and local updates on COVID-19, updates on suspected case definition, PPE stock review and daily indicator updates. It had 3 guiding principles (1) Protect our staff from infection (2) Protect our patients from infection (3) Continue to support critical national psychiatric treatment needs. The DOTF met almost daily and promulgated regular updates to all staff on the national COVID-19 situation and IMH COVID-19 actions via internal email, Facebook Workplace apps and Townhall sessions. Besides adhering to all national COVID-19 guidelines, IMH further identified core psychiatric services that were tasked to develop specific BCPs to continue operations in DORSCON Orange and Red. As there is no specific treatment or vaccine for COVID-19, we adopted a hierarchy of controls approach to protecting staff and patients: Engineering, Administrative and PPE25. The most effective level of control (Engineering) refers to the placement of barriers between COVID-19 and healthcare staff (e.g. batching patients by location). Administrative controls refer to policies to reduce exposure to COVID-19 (e.g. travel restrictions for healthcare staff) and PPE being the final level of control for frontline healthcare staff.
There was an initial discussion about whether the ECT service should continue during DORSCON Orange. There was a projected need to redeploy staff to man 24-hour screening centres and bolster the rosters of certain wards like the medical ward, emergency clinic, forensic ward and satellite clinics. This was to ensure enough manpower for wards to be fully independent if there was a need to stop any cross-ward movement of staff which was commonly done to optimize manpower usage. In addition, the ECT service mixed staff and patients from almost all the wards in IMH daily, creating a high-risk area for cross infection of patients and staff.
However, it was recognized early in DOTF discussions that ECT was the only treatment for severe life-threatening conditions like catatonia and was a treatment commonly used to enhance patient recovery for earlier discharge. Stopping the ECT service would result in a delay of discharge for many inpatients at a time when it was even more critical to return patients to their home expeditiously rather than keep then housed with other patients and increase their risk of infection. Hence the ECT service was identified as an essential service and our BCP was formulated with 5 key considerations: (1) Calibrate the infection control measures to the DORSCON level (2) Ensure adequate PPE and disinfection capability (3) Revise ECT operations to minimize infection risk to staff and patients and establish an alternate team if the primary team was quarantined (4) Train and audit staff in the use of PPE (5) Manage Demand
Calibrate infection control measures to DORSCON level
The ECT team worked closely with our infection control team to determine the risks posed to staff and patients by the COVID-19 virus with our current operations. After a review of the risks inherent in ECT, it was decided that all staff involved with clinical ECT operations (both doing ECT and in the recovery room) required full PPE (N95 masks, protective eye wear, full surgical gown, gloves) while non-clinical ECT staff interacting with patients would require a 3 ply facemask and gloves at all times when interacting with patients and that PPE would be changed between each batch of patients. It was also decided to enhance ECT room disinfection with 70% ethanol wipes between patients to minimize the chance of cross infection between patients.
Ensure Adequate PPE and Disinfection Capability
IMH had a small stockpile of PPE but quickly increased its holding stock after the infection control measures (i.e. full PPE) were confirmed and our projected usage of PPE would be several orders of magnitude higher than pre-COVID-19. Increased disinfectant hand rub and 70% ethanol wipes were also ordered in bulk. Decontaminating the ECT room pre-COVID-19 was done by estate management after a half-day session. The COVID-19 situation necessitated more cleaning and disinfection services. We arranged with our estates management team to have a cleaner on site during ECT operational hours to respond expeditiously to ECT room decontamination between batches of patients and ECT staff helped with cleaning their own area of work with 70% ethanol. We switched to single use Mapleson C circuits for anaesthesia for each batch of patients with disposable bite blocks, oral airways and HEPA (high efficiency particulate air) filters for each patient.
Revise ECT operations to minimize infection of staff or patients and establish alternate ECT team
Pre-COVID-19 ECT operations emphasized efficiency and hence patients often spent a significant amount of time waiting pre/post ECT in the ECT room. There was routine mixing of patients from different wards and inpatient with outpatients. Staff were also routinely rotated with a pool of 10 different ECT practitioners, approximately 30 public and private sector anaesthetists and 30 nursing staff rotating to fill 12 staff positions (1 ECT practitioner, 1 Anaesthetist, 10 nursing staff) on any given day.
The status quo operations resulted in an unacceptably high level of patient and staff interaction with correspondingly high risk of exposure to COVID-19. A decision was made to restrict the pool of staff down to just 2 ECT practitioners, 2 anaesthetists and 11 nursing staff and reduce the number of staff required at any time to 11 (down from 12). We were able to reduce the number of staff required by enlisting the ward and outpatient staff to assist with ECT patient transportation. One of the ECT nursing staff would have a new role of receiving ECT patients and conducting COVID-19 risk screening and temperature taking before letting the patient into the ECT room. This nursing staff also ensured that a maximum of 1 visitor equipped with a face mask could accompany the patient. This was on top of IMH measures of restricting all access to a single entrance operated 24/7 by a dedicated screening team using the current suspect COVID-19 case definition and temperature screening. These changes required a concerted effort from nursing and human resources to adjust contracts and staff allocation. We were also fortunate to have recently trained an advance practice nurse (APN) to be an ECT practitioner37 which allowed for a backup ECT practitioner as 8 of the original 10 ECT practitioners were requisitioned for other roles in IMH during DORSCON Orange. The alternate ECT practitioner and anaesthetist did not meet their counterparts to prevent cross team infection and 2 reserve nurses were similarly deployed outside the ECT room as alternative nursing staff. The alternative team allowed the primary team to take short local leave of up to 3 days at a stretch for staff rest and recuperation.
The most significant change was to batch patients by location (i.e. by ward and outpatients), fully decontaminate the ECT room and change staff PPE between batches of patients. There was an initial thought of having 1 patient in the ECT room at any one time and decontaminating the entire room between patients. While this would minimize cross infection risk, it would have reduced capacity by about 70-80% as each patient required at least 30 minutes of post-ECT continuous monitoring, rendering this option unfeasible. Consistent with the principle of a calibrated approach to COVID-19 infection control measures38 and low rates of COVID-19 community spread, we decided on a balanced approach of batching patients by physical location (inpatients by ward, outpatients separately from inpatients) to minimize the chance of infection while only losing 30-40% capacity. This required a full review of all locations patients came from and calculating the load from each location to optimize scheduling. The intent was to minimize mixing of patients from different locations and decrease the chance of infection. With the new strategy of listing patients by location, a new operations board was set up as a visual management aid for staff. It gave staff a comprehensive view of patients’ locations and let us realize that some wards had as few as 1 patient receiving ECT and others as many as 10. (See Image 1 below)
Figure 1.
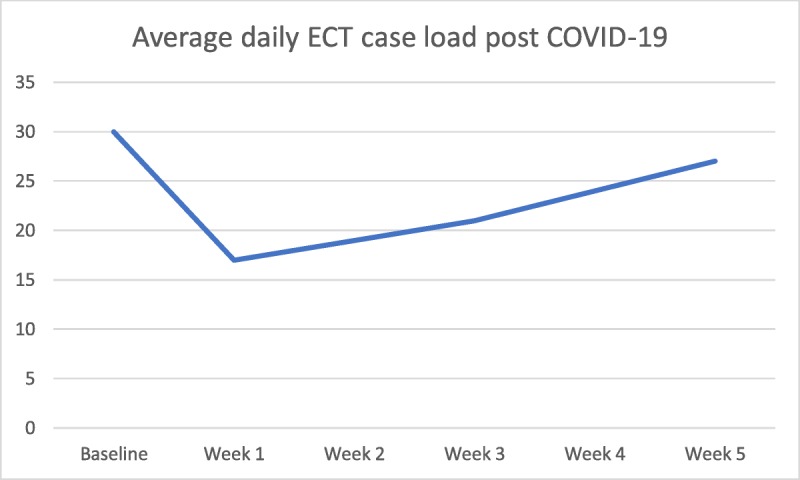
Average daily ECT case load post COVID-19
The need to decontaminate the ECT room between batches of patients meant that we had to spread out the ECT for wards with only a few patients over different days to minimize decontamination time. This way we were able to decrease the decontamination sessions (each lasting almost 30 min) from 5-6 to 3-4 a day. Figure 1 below illustrates the large decrease in ECT capacity in the first week of DORSCON Orange but with the measures described above capacity slowly increased over the next 5 weeks.
We separately increased the number of ECT sessions from 7 to 8 half-day sessions to maintain ECT capacity with plans to increase to a full 10 half-day session a week. A daily huddle was conducted before and after ECT sessions to iron out teething issues and help bolster staff morale by addressing their concern and incorporating their suggestions.
Train and audit staff in the use of PPE
ECT staff did not routinely use full PPE (see Image 2) so dedicated refresher training sessions were held by infection control staff for the ECT team on how to apply and remove PPE safely and revise disinfection protocols for equipment. It was insufficient to just teach the proper usage of PPE as its usage was cumbersome and initial staff adherence was poor. Twice daily audits of ECT staff adherence was conducted to ensure proper usage of PPE and infection control procedures.
Image 1.

New Operations Board indication patients by location
Image 2.

Full Personal protective equipment
Reducing demand
Despite our best efforts our ECT capacity would have decreased from about 115 treatments a week to only 80 to 90 treatments a week despite increasing the number of half-day sessions from 7 to 8. While planning to increase the number of ECT sessions it became evident that we also need to enlist the help of our colleagues in reducing ECT demand to prevent a situation where we would have to use “wartime triage” to decide on who would be able to access lifesaving ECT akin to the situation in Italy with respirators for COVID-19 patients39. We started communicating with referring psychiatrists about the decreased ECT treatment capacity which would necessitate a decrease of ECT frequency from thrice a week to twice a week for most cases and had individual case discussions with clinicians about decreasing the frequency of outpatient maintenance ECT. Lastly, we used our routine pre-ECT assessments clinics to assess the severity, urgency and likelihood of response to ECT vis-à-vis the availability of ECT treatment capacity to prioritize patients for ECT.
Testing the system
The system was tested in the third week of DORSCON Orange when a confirmed COVID-19 contact was diagnosed in an inpatient ward where there were 10 patients receiving ECT. The contact was immediately quarantined in our medical ward isolation bed and the ward “buttoned up” (i.e. no patient movement in or out of the ward). A discussion between the ECT service, infection control and NCID was conducted to assess the risk of infection to staff and patients. After a review and audit of our infection control procedures and assessing the need for ECT for the 10 patients on the ward, the collective decision was that our current infection control protocols was enough to allow for continued ECT for other patients in the ward. This was in large part due to the full PPE for staff, physical separation of patients by ward location and decontamination of the ECT room between different batches of patients from separate wards. Fortunately, the contact eventually tested negative for COVID-19 but the system was robust enough to continue providing timely ECT despite the infection risk.
Conclusion
The WHO Director general recommended a comprehensive strategy of preparation, detection, transmission reduction and innovation to combat COVID-193. The descriptions of the IMH ECT service adaptations for COVID-19 covered the first 3 points but continuous innovation was implicit in all 3 steps. As of this writing the IMH ECT service has been operating in DORCON Orange for 6 weeks and each week brings new revisions to our operations to improve safety or increase capacity.
We are increasingly looking into the sustainability of our operations with the realization that the COVID-19 situation was not going to last for a few short months as initially hoped, but possibly a year or more10. Staff morale would be key in sustaining the fight against COVID-19 and was bolstered by strong leadership communicating a clear patient-oriented mission that staff could rally behind, balanced with staff safety and welfare. It is a time of great fear and uncertainty, but as Winston Churchill famously said, we will never surrender in this fight against an invisible and invidious enemy; our patients and families need us to win this war.
Footnotes
Conflict of interest: All authors declare that they have no competing interests.
References
- 1.China confirms coronavirus can pass person-to-person as fourth death reported. 2020. (Accessed 14th Mar, 2020, at https://www.cnbc.com/2020/01/21/china-coronavirus-human-to-human-transmission-confirmed.html.)
- 2.Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020. (Accessed 14th Mar, 2020, at https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov).)
- 3.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. (Accessed 14th Mar, 2020, at https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.)
- 4.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. New England Journal of Medicine 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.How COVID-19 spreads. 2020. (Accessed 14th Mar, 2020, at https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html.)
- 7.Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. (Accessed 14th Mar, 2020, at https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=2ahUKEwi1ouu_zpnoAhVKbn0KHUpHAEcQFjAAegQIBxAB&url=https%3A%2F%2Fwww.who.int%2Fdocs%2Fdefault-source%2Fcoronaviruse%2Fwho-china-joint-mission-on-covid-19-final-report.pdf&usg=AOvVaw1gO_RTfaIWQuEkjdvq_O7i.)
- 8.Severe Acute Respiratory Syndrome (SARS). 2019. (Accessed 26th Mar, 2020, at https://www.healthhub.sg/a-z/diseases-and-conditions/126/topic_sars.)
- 9.Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? The Lancet Infectious Diseases 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Covid-19 likely to last till end-2020 at least: Experts. 2020. (Accessed 14th Mar, 2020, at https://www.straitstimes.com/singapore/health/coronavirus-covid-19-likely-to-last-till-end-2020-at-least-experts.)
- 11.Pandemic Influenza - Report with Evidence HL 88, 4th Report of Session 2005-06. 2005. (Accessed 14th Mar, 2020, at https://www.webcitation.org/5gcuRTA6L?url=http://www.parliament.the-stationery-office.com/pa/ld200506/ldselect/ldsctech/88/88.pdf.)
- 12.The UK ECT Review Group Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. The Lancet 2003;361:799–808. [DOI] [PubMed] [Google Scholar]
- 13.Fink M, Kellner CH, McCall WV. Optimizing ECT technique in treating catatonia; LWW; 2016. [DOI] [PubMed] [Google Scholar]
- 14.Slade EP, Jahn DR, Regenold WT, Case BG. Association of electroconvulsive therapy with psychiatric readmissions in US hospitals. JAMA psychiatry 2017;74:798–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tor P-C, Galvez V, Ang A, et al. Electroconvulsive practice in Singapore: a cross-sectional national survey. Singapore Medical Journal 2019;60:590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kramer BA. Use of ECT in California, revisited: 1984-1994. The journal of ECT 1999;15:245–51. [PubMed] [Google Scholar]
- 17.Casey DE. Metabolic issues and cardiovascular disease in patients with psychiatric disorders. The American Journal of Medicine Supplements 2005;118:15–22. [DOI] [PubMed] [Google Scholar]
- 18.Brewer WJ, Edwards J, Anderson V, Robinson T, Pantelis C. Neuropsychological, olfactory, and hygiene deficits in men with negative symptom schizophrenia. Biological Psychiatry 1996;40:1021–31. [DOI] [PubMed] [Google Scholar]
- 19.Nelson G, Hall GB, Squire D, Walsh-Bowers RT. Social network transactions of psychiatric patients. Social Science & Medicine 1992;34:433–45. [DOI] [PubMed] [Google Scholar]
- 20.South Korea is bracing for a spike in coronavirus cases after a ‘super-spreader’ event occurred at a church ‘cult’. 2020. (Accessed 14th Mar, 2020, at https://www.businessinsider.sg/shincheonji-church-cult-south-korea-super-spreader-coronavirus-spike-2020-2?r=US&IR=T.)
- 21.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and its inactivation with biocidal agents. Journal of Hospital Infection 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chowell G, Fenimore PW, Castillo-Garsow MA, Castillo-Chavez C. SARS outbreaks in Ontario, Hong Kong and Singapore: the role of diagnosis and isolation as a control mechanism. Journal of theoretical biology 2003;224:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Centre for Infectious Diseases to open progressively from December 2018. 2018. (Accessed 26th Mar, 2020, at https://www.ncid.sg/News-Events/News/Pages/National-Centre-for-Infectious-Diseases-to-open-progressively-from-December-2018.aspx.)
- 24.Precautionary Measures In Response to Severe Pneumonia Cases In Wuhan, China 2020. (Accessed 26th Mar, 2020, at https://www.moh.gov.sg/news-highlights/details/precautionary-measures-in-response-to-severe-pneumonia-cases-in-wuhan-china.)
- 25.Wong J, Goh QY, Tan Z, et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Canadian Journal of Anesthesia/Journal canadien d'anesthésie 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singapore per capita GDP. 2016. (Accessed 16th July 2016, 2016, at http://www.singstat.gov.sg/statistics/latest-data#1.)
- 27.Mental Health (Care and Treatment) Act. 2012. (Accessed 18th July, 2019, at https://sso.agc.gov.sg/Act/MHCTA2008.)
- 28.Krishna LK. Decision-Making at the End of Life: A Singaporean Perspective. Asian Bioethics Review 2011;3:118–26. [Google Scholar]
- 29.Coronavirus: Docs in public sector must limit work to one hospital. 2020. (Accessed 14th Mar, 2020, at https://www.straitstimes.com/singapore/health/docs-in-public-sector-must-limit-work-to-one-hospital.)
- 30.Public health personnel to defer all travel and leave. 2020. (Accessed 14th Mar, 2020, at https://www.tnp.sg/news/singapore/public-health-personnel-defer-all-travel-and-leave.)
- 31.Rasmussen K. Stimulus titration and ECT dosing: commentary. The Journal of ECT 2002;18:10–1. [DOI] [PubMed] [Google Scholar]
- 32.McCall WV, Reboussin DM, Weiner RD, Sackeim HA. Titrated moderately suprathreshold vs fixed high-dose right unilateral electroconvulsive therapy: acute antidepressant and cognitive effects. Archives of General Psychiatry 2000;57:438–44. [DOI] [PubMed] [Google Scholar]
- 33.Martin DM, Gálvez V, Lauf S, et al. The Clinical Alliance and Research in Electroconvulsive Therapy Network: an Australian initiative for improving service delivery of electroconvulsive therapy. The journal of ECT 2018;34:7–13. [DOI] [PubMed] [Google Scholar]
- 34.Chan CYW, Abdin E, Seow E, et al. Clinical effectiveness and speed of response of electroconvulsive therapy in treatment-resistant schizophrenia. Psychiatry and clinical neurosciences 2019;73:416–22. [DOI] [PubMed] [Google Scholar]
- 35.Wong VKH, Tor PC, Martin DM, Mok YM, Loo C. Effectiveness and Cognitive Changes With Ultrabrief Right Unilateral and Other Forms of Electroconvulsive Therapy in the Treatment of Mania. The journal of ECT 2019;35:40–3. [DOI] [PubMed] [Google Scholar]
- 36.Zhao YJ, Tor PC, Khoo AL, Teng M, Lim BP, Mok YM. Cost-Effectiveness Modeling of Repetitive Transcranial Magnetic Stimulation Compared to Electroconvulsive Therapy for Treatment-Resistant Depression in Singapore. Neuromodulation: Technology at the Neural Interface 2018;21:376–82. [DOI] [PubMed] [Google Scholar]
- 37.Rosedale M, Knight C, Standard J. The Role of the Psychiatric Mental Health: Advanced Practice Registered Nurse in the Scope of Psychiatric Practice. The journal of ECT 2015;31:205–6. [DOI] [PubMed] [Google Scholar]
- 38.Coronavirus: Singapore mindful of need to calibrate social distancing measures, says Lawrence Wong. 2020. (Accessed 14th Mar, 2020, at https://www.straitstimes.com/singapore/spore-mindful-of-need-to-calibrate-social-distancing-measures.)
- 39.The Extraordinary Decisions Facing Italian Doctors 2020. (Accessed 14th Mar, 2020, at https://www.theatlantic.com/ideas/archive/2020/03/who-gets-hospital-bed/607807/.)


