To the Editor:
Chronic subdural hematomas (CSDHs) are encapsulated collections of blood breakdown products and fluid between the dura mater and the arachnoid.1 Their global incidence is estimated to be about 5/100 000/yr in patients younger than 65 yr,2 increasing to 58/100 000/yr in patients over 65 yr.1 Surgery usually allows a good outcome even in elderly. The clinical outcome of CSDH is conditioned by comorbidities including pulmonary diseases.
Nowadays, we are facing a new possible condition related to coronavirus disease 2019 (COVID-19) that could affect the outcome. The spread of this infection started in 2019, December 31st when China alerted WHO about cases of unusual amount of interstitial pneumonia (IP) in Wuhan. After 7 d, on January 7th, scientists announced they had identified a new virus named COVID-19 similar to SARS-CoV. Italy is dealing with pandemic spread of COVID-19. As a matter of fact, on 19th March, it became the country with the highest number of confirmed deaths in the world. On March 23rd 2020 Italy was the world's centre of the epidemic with 69.176 confirmed cases, 6.820 deaths, and 21.137 recoveries.3
Clinically COVID-19 could lead to a severe IP and acute respiratory distress syndrome (ARDS), especially in older patients with multiple comorbidities.4 No studies about surgery in COVID-19 patients have been reported so far. We aim to describe our surgical experience with CSDH in a COVID-19 neurosurgical center.
We admitted 5 patients with CSDH to the Neurosurgical Department of Brescia University Hospital between February 21, 2020 (first COVID-19 case reported in Italy) and March 23, 2020. The patients were positive for COVID-19 real-time polymerase chain reaction obtained by nasopharyngeal swab.5,6 We gathered the following data for each patient: age and sex, Cumulative Illness Rating Scale,7 antithrombotic therapy and perioperative mortality (within 30 d). All the patients had signed a consent form approved by the Local Ethic Committee regarding the use of their clinical data. We compared the mortality rate of this new cohort with the data extracted from our pre-COVID-19 CSDH case series.
All the patients underwent pre-operative chest X-Ray (CXR) or computed tomography (CT) and routine blood test. An anesthesiological evaluation was performed for each patient. We cohortized our neurosurgical ward to separate COVID-19 positive from negative cases. COVID-19 positive patients started anti-retroviral therapy with lopinavir/ritonavir and hydroxychloroquine. Daily arterial blood gas analysis and CXR were performed.
Surgery or endovascular treatment were indicated when the CSDH was symptomatic (presence of focal neurological deficits or mental status changes) and the maximum thickness was greater than 1 cm (Figures 1-4). One case did not present severe neurological impairment and was treated conservatively (Figure 5). No preoperative respiratory impairment was observed.
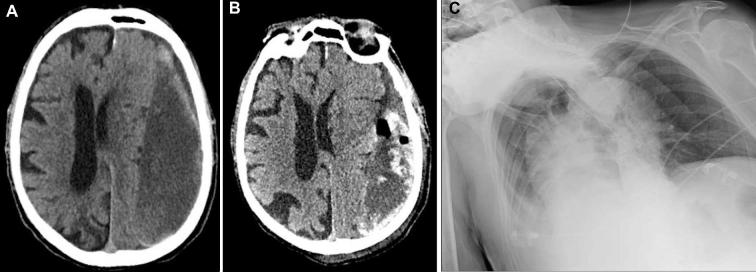
FIGURE 1.
A and B, Head CT scan, axial view: pre- and postoperative CDSH. C, CXR showing bilateral and diffuse IP.
FIGURE 4.
A, Head CT scan, axial view: preoperative left CSDH. B, Head CT scan, axial view: postoperative CSDH with signs of recent rebleeding. C, CXR showing bilateral IP.
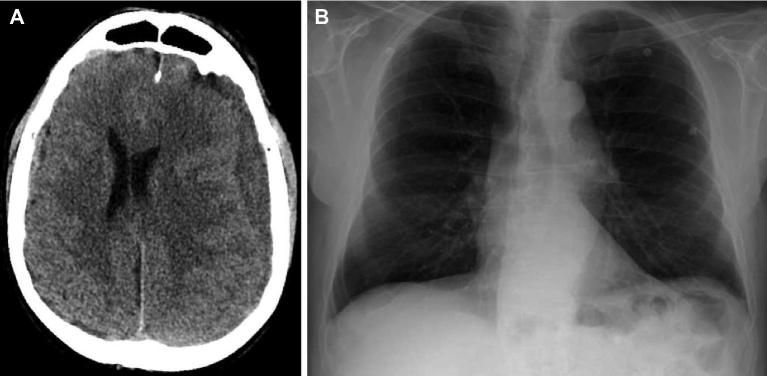
FIGURE 5.
A, Head CT scan, axial view: left CSDH. B, normal CXR.
We treated all the CSDH patients under general anesthesia. Three patients were operated (2 through craniotomy and 1 with a burr hole). Endovascular occlusion of the middle meningeal artery (MMA) was performed in 1 case (Figure 2). In the surgical cases we placed a subdural drainage for 48 h. After its removal patients underwent a CT head scan (Figures 1, 3, and 4). Afterwards the patients started low-molecular-weight heparin at prophylactic dose before mobilization. The cases are reported in the supplementary material section (Supplemental Digital Content).
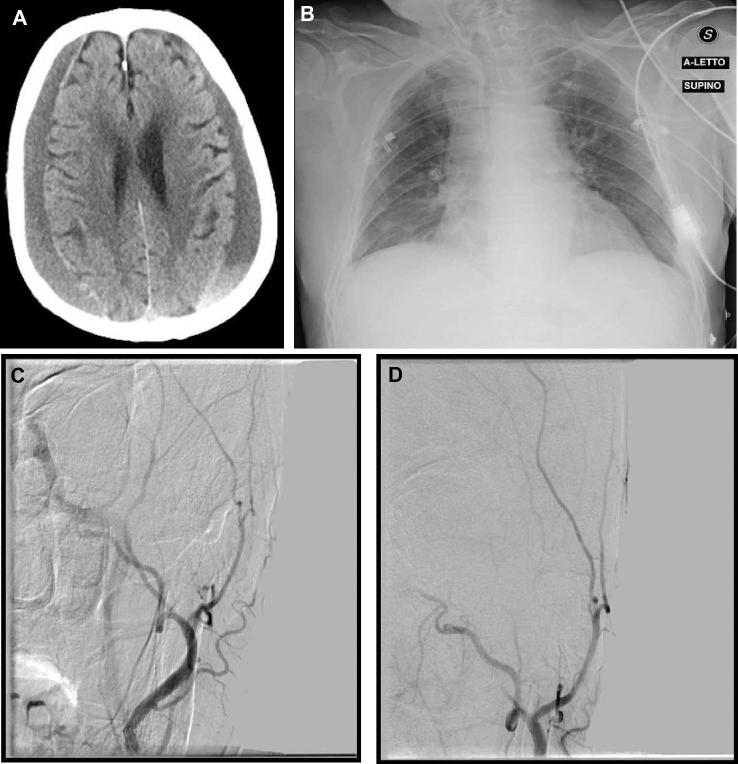
FIGURE 2.
A, Head CT scan, axial view: bilateral CSDH. B, CXR showing bilateral and diffuse IP. C and D, MMA embolization procedure.
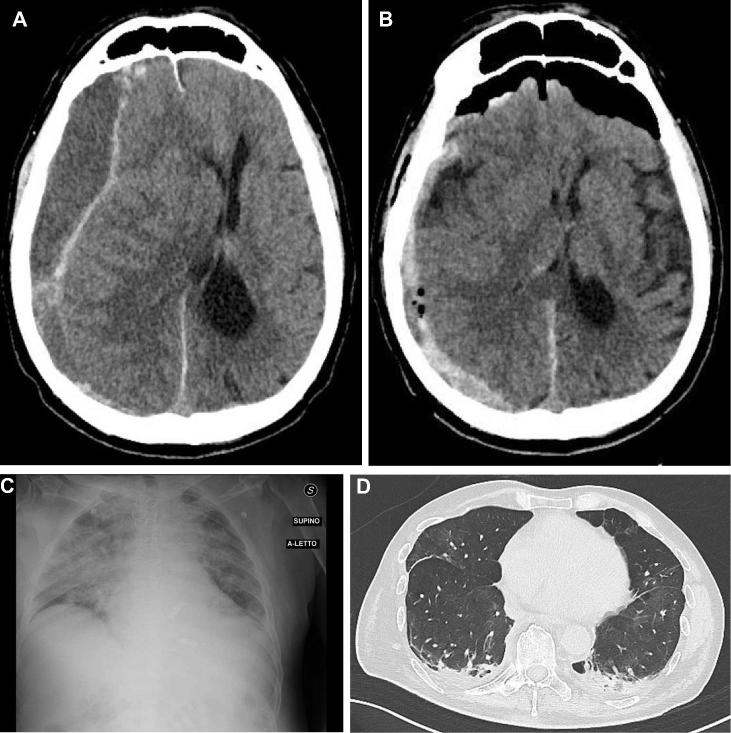
FIGURE 3.
A, Head CT scan, axial view: preoperative CSDH. B, Head CT scan, axial view: postoperative CSDH with signs of recent rebleeding. C, CXR showing bilateral and IP. D, Chest CT scan, axial view, showing ground glass opacity.
CSDHs mostly occur in elderly, with an average age of 63.1 Head trauma is the major risk factor, identified in less than 50% (often minor head trauma).8 Other risk factors are described like alcohol abuse, seizures, CSF shunts and coagulopathies, including therapeutic anticoagulation. CSDHs are bilateral in 20% to 25% of cases.9 At present there is no scientific experience regarding surgical outcome of COVID-19 patients.
We compared the recent cohort of COVID-19 CSDH patients with our historical series. Between May 2018 and September 2019, we operated 142 patients for CSDH and we observe 5 death at our Institution. Our mortality rate was 3.7% according to the literature.10 In our recent experience, we observed 4 death in 5 COVID-19 patients suffering from CSDH. Therefore, we observed a mortality rate of 80% about 21,6 times greater than our control data.
HEMATOLOGICAL DISORDERS
We observed 2 cases of mild thrombocytopenia (Table). In these cases, we observed a re-bleeding (Figures 3 and 4) that led from a rapid neurological worsening to death within 5 d. This condition could be related to COVID-19 infection, as reported in literature.11 Independently from the hemorrhagic risk, Lippi et al12 showed that low platelet count is associated with increased risk of severe disease and mortality in patients with COVID-19, and this should serve as clinical indicator of worsening illness during hospitalization.12 In our series, we suppose that thrombocytopenia led to re-bleeding and was associated with poor outcome.
TABLE.
Clinical Features of our Cohort
| Sex | Age | CIRS | AT | Side | COVID-19 | IP | TP* | Surgery | Time to death(d) |
|---|---|---|---|---|---|---|---|---|---|
| M | 82 | 13 | Yes | Left | + | + | No | Burr-hole | 14 |
| M | 86 | 18 | No | Bilateral | + | + | No | MMA embolization | 10 |
| M | 77 | 20 | No | Right | + | + | Yes | Craniotomy | 5 |
| M | 85 | 22 | Yes | Left | + | + | Yes | Burr-hole | 5 |
| M | 78 | 19 | Yes | Left | + | – | No | NO | Alive |
*TP (Thrombocytopenia): 100.000<PLTs<150.000
All patients developed IP after surgery. Thrombocytopenia was observed in 2 cases (40%). The patients suffered rebleeding and showed a shorter time to death. CIRS (Cumulative Illness Rating Scale), AT (antithrombotic drugs), IP (Interstitial Pneumonia), COVID-19 (Coronavirus Disease 2019).
INTERSTITIAL PNEUMONIA
Dyspnoea and fatigue occurred in all our patients within 48 hours from surgery. CXR revealed severe IP (Figures 1-4). Ground glass opacity and bilateral patchy shadowing were observed on the chest CT (Figure 3).5,13 All our patients had COVID-19 infection without pre-operative respiratory symptoms. Immune system could be impaired following surgical procedures and this may have unmasked a subclinical infection.14,15 On the other hand no respiratory failure was observed in the conservative-treated case (Figure 5).
In our experience IP occurred in all cases after treatment and worsened the outcome. This evenience represents a possible complication, often fatal, of COVID-19 infection.5
HEALTH EMERGENCY
Nowadays, Italian health care system is the most afflicted in the pandemic scenario.16 The overload of the intensive care units in Lombardy, despite the efforts made, has necessarily influenced the resuscitation possibilities of elderly patients.17 Therefore, we cannot exclude that our results could be affected by the health emergency status.
Seung et al. reported good bleeding control from CSDH membrane with MMA embolization, prevention of further growth of hematoma and even spontaneous resolution without surgery.18 Anyway our endovascular treated patient showed the same poor outcome of the surgical cases.
Although statistical analysis of these preliminary data is not possible, COVID-19 patients appear to suffer from a negative surgical outcome. It is our belief that conservative treatment should be preferred whenever surgery could be postponed.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Supplementary Material
Supplemental Digital Content. Report of the case series. Case 1, 3, and 4: surgical series. Case 2: endovascular MMA occlusion. Case 5: conservative treatment.
REFERENCES
- 1. Mehta V, Harward SC, Sankey EW, Nayar G, Codd PJ. Evidence based diagnosis and management of chronic subdural hematoma: a review of the literature. J Clin Neurosci Off J Neurosurg Soc Australas. 2018;50:7-15. [DOI] [PubMed] [Google Scholar]
- 2. Santarius T, Hutchinson PJ. Chronic subdural haematoma: time to rationalize treatment? Br J Neurosurg. 2004;18(4):328-332. [DOI] [PubMed] [Google Scholar]
- 3. Emergency Coronavirus: The National response. http://www.protezionecivile.gov.it/en/risk-activities/health-risk/emergencies/coronavirus. Last Accessed March 23, 2020. [Google Scholar]
- 4. Sohrabi C, Alsafi Z, O’Neill N et al.. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Huang C, Wang Y, Li X et al.. Clinical features of patients infected with 2019 novel coronavirus in wuhan, china. Lancet (London, England). 2020;395(10223):497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang D, Hu B, Hu C et al.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, china. JAMA. published online: February, 2020. (doi:10.1001/jama.2020.1585). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Holcomb EM, Millis SR, Hanks RA. Comorbid disease in persons with traumatic brain injury: descriptive findings using the modified cumulative illness rating scale. Arch Phys Med Rehabil. 2012;93(8):1338-1342. [DOI] [PubMed] [Google Scholar]
- 8. Kawamata T, Takeshita M, Kubo O, Izawa M, Kagawa M, Takakura K. Management of intracranial hemorrhage associated with anticoagulant therapy. Surg Neurol. 1995;44(5):438-443. [DOI] [PubMed] [Google Scholar]
- 9. Robinson RG. Chronic subdural hematoma: surgical management in 133 patients. J Neurosurg. 1984;61(2):263-268. [DOI] [PubMed] [Google Scholar]
- 10. Camel M, Grubb RL. Treatment of chronic subdural hematoma by twist-drill craniostomy with continuous catheter drainage. J Neurosurg. 1986;65(2):183-187. [DOI] [PubMed] [Google Scholar]
- 11. Guan W-J, Ni Z-Y, Hu Y et al.. Clinical characteristics of coronavirus disease 2019 in china. N Engl J Med. published online: February, 2020. (doi:10.1056/NEJMoa2002032). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lippi G, Plebani M, Michael Henry B. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. published online:2020. (doi:10.1016/j.cca.2020.03.022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E et al.. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. published online: March, 2020. (doi:10.1016/j.tmaid.2020.101623). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. O’Dwyer MJ, Owen HC, Torrance HDT. The perioperative immune response. Curr Opin Crit Care. 2015;21(4):336-342. [DOI] [PubMed] [Google Scholar]
- 15. Torrance HDT, Pearse RM, O’Dwyer MJ. Does major surgery induce immune suppression and increase the risk of postoperative infection? Curr Opin Anaesthesiol. 2016;29(3):376-383. [DOI] [PubMed] [Google Scholar]
- 16. Coronavirus Latest : Italy death toll overtakes china's. Nature. published online: March, 2020. (doi:10.1038/d41586-020-00154-w). [Google Scholar]
- 17. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in lombardy, italy. JAMA. published online:2020. (doi:10.1001/jama.2020.4031). [DOI] [PubMed] [Google Scholar]
- 18. Ban SP, Hwang G, Byoun HS et al.. Middle meningeal artery embolization for chronic subdural hematoma. Radiology. 2018;286(3):992-999. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.