Abstract
The novel coronavirus disease-19 (COVID-19) pandemic has altered our economy, society, and healthcare system. While this crisis has presented the U.S. healthcare delivery system with unprecedented challenges, the pandemic has catalyzed rapid adoption of telehealth, or the entire spectrum of activities used to deliver care at a distance. Using examples reported by U.S. healthcare organizations, including ours, we describe the role that telehealth has played in transforming healthcare delivery during the 3 phases of the U.S. COVID-19 pandemic: (1) stay-at-home outpatient care, (2) initial COVID-19 hospital surge, and (3) postpandemic recovery. Within each of these 3 phases, we examine how people, process, and technology work together to support a successful telehealth transformation. Whether healthcare enterprises are ready or not, the new reality is that virtual care has arrived.
Keywords: telemedicine, telehealth, COVID, pandemic
The novel coronavirus disease 2019 (COVID-19) pandemic has altered our economy, society, and healthcare system. While this crisis has presented the U.S. healthcare delivery system unprecedented challenges, it has catalyzed rapid adoption of telehealth and transformed healthcare delivery at a breathtaking pace.1,2 The term telehealth refers to the entire spectrum of activities used to deliver care at a distance—without direct physical contact with the patient. Telehealth encompasses both provider-to-patient and provider-to-provider communications, and can take place synchronously (telephone and video), asynchronously (patient portal messages, e-consults), and through virtual agents (chatbots) and wearable devices. A brief summary of the opportunities and limitations of each type of telehealth encounter is offered (Table 1).
Table 1.
Classification of telehealth encounters
| Platform | Use Case(s) | Opportunities | Limitations |
|---|---|---|---|
| E-consult: Asynchronous clinician-to-clinician communication based on record review (inpatient and outpatient) |
|
|
|
| Remote patient monitoring:Gather patient outside traditional healthcare setting via connected device or patient reported outcomes (synchronous or asynchronous) | All phases: efficient method of patient care, especially those with chronic conditions |
|
|
|
All phases: time-efficient handling of straightforward issues. |
|
|
| Telephone visit: Synchronous patient-clinician communication by phone | During and after initial surge: replace some face-to-face visits | Universally accessible, even in the most ill/low socioeconomic status patients | Currently devalued by most payers, inability to conduct a physical exam, loss of nonverbal cues |
| Video visit: Synchronous patient-clinician communication with both audio and video, with possible ancillary and telemetry equipment |
|
|
|
COVID-19: coronavirus disease 2019; EHR: electronic health record.
Telehealth programs overcome physical barriers to provide patients and caregivers access to convenient medical care. Healthcare systems with telehealth sustain the continuity of outpatient patient care during this pandemic—in the midst of “stay-at-home” orders and physical distancing measures, while reducing community and nosocomial spread. Telehealth also proves useful for inpatient care, in particular to help balance the supply of clinical services with surge in demand across physical or geographical boundaries, conserve personal protective equipment, and provide isolated patients connection to family and friends.3,4
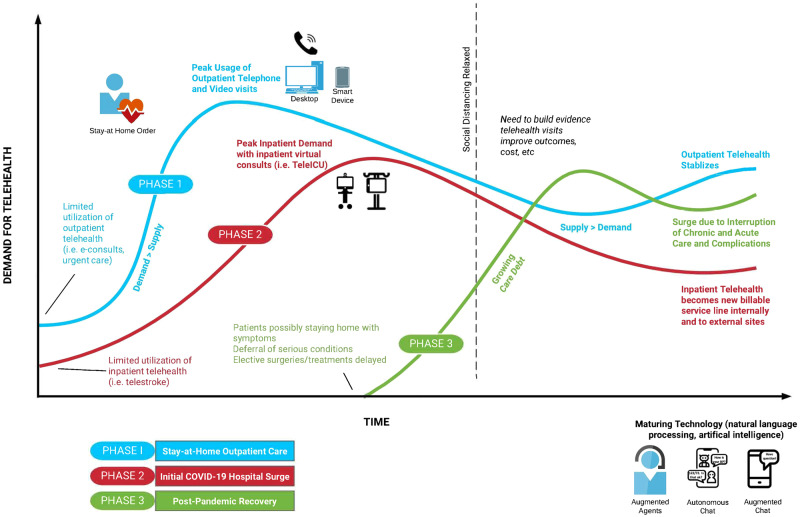
Using examples reported by U.S. healthcare organizations, including ours, we describe the role telehealth has played in transforming healthcare delivery during the 3 phases of the U.S. COVID-19 pandemic: (1) stay-at-home outpatient care, (2) initial COVID-19 hospital surge, and (3) postpandemic recovery (Figure 1). Within each of these 3 phases, we examine how people, process, and technology work together to support this telehealth conversion.5 This framework offers health systems integral components for a successful transformation.
Figure 1.
Three phases of coronavirus disease 2019 (COVID-19) pandemic and demand for telehealth services.
PHASE 1: OUTPATIENT CARE DURING “STAY-AT-HOME” ORDERS
Social distancing and “stay-at-home” orders began in earnest in the United States in March 2020 and will likely remain for an extended period after the peak surge period. Telehealth services provide the opportunity to maintain access and continuity of medical care while reducing the potential for community and nosocomial spread of the virus. Adoption of telehealth requires changes in both patient-related and clinical care processes. The target is to dramatically decrease the proportion of in-person care, offering in-person clinic visits only for patients who cannot access telehealth technology or who have urgent (but not emergency-level) clinical concerns that require detailed physical examination.
Before the outbreak, many health systems had low rates of telehealth utilization for routine care.6 Even health systems with relatively high telehealth adoption performed fewer than 100 video visits per day.7 Now, many are seeing >600 patients per day via video, with many in-person clinic replaced with video or telephone visits. At our institution, the share of telehealth visits has increased within a 4-week period from <1% of total visits to 70% of total visits, reaching more than 1000 video visits per day (Figure 2).
Figure 2.
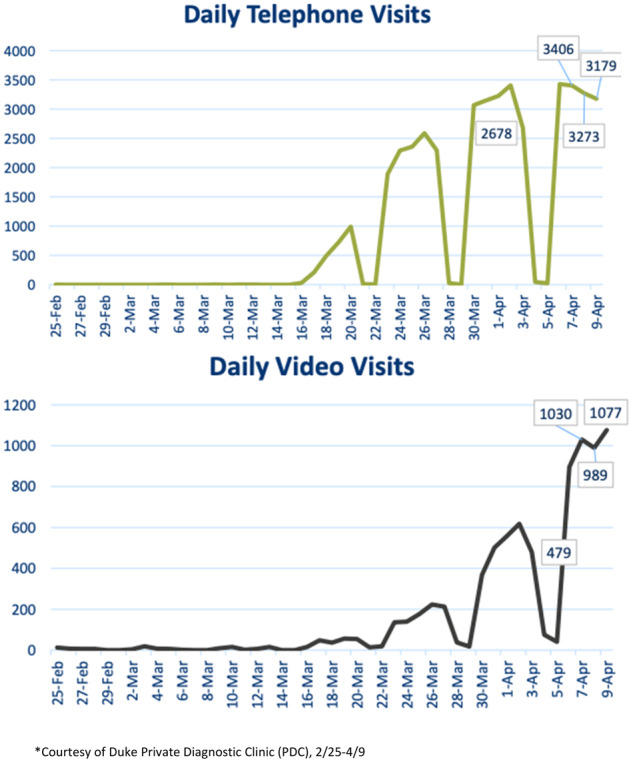
Duke institutional operations data of telehealth visits: telephone and video.
By May 1, 2020, our institution will have fully provisioned and trained all clinicians to provide both inpatient and outpatient telehealth services. To manage this shift, a centralized telehealth call center was created, staffed by newly hired and repurposed existing staff, medical students, and “superusers” to train providers and patients to use telehealth systems. A “train the trainer” model allowed rapid staff development in order to onboard over 1300 providers in 3 weeks, while providing technical online support during live patient visits. Using ExtendedCare (STA Group, Chicago, IL), we offered scheduled outpatient video visits integrated into the patient portal of our electronic health record (EHR) (Epic, Verona, WI) so that patients could interact with their clinicians from either their personal computers or smartphones. Virtual patient waiting rooms, privacy and security, and easy scheduling were important when evaluating a platform. Home peripheral devices were used with certain patients to facilitate remote visits. For example, blood pressure machines and cuffs were sent to high-risk obstetrics patients.
PHASE 2: INITIAL INPATIENT COVID-19–RELATED SURGE
As demand for COVID-19–related hospital care increases, medical personnel may be reassigned to cover inpatient clinical services. These personnel changes reflect the changes in healthcare delivery processes during the COVID-19 surge, which are similar to those in other disasters: providing screening and forward triaging to manage response, distinguishing the critically ill from those less ill, and maximizing efficient use of system capacity.8 Where COVID-19 differs from standard disaster management is the pathogenicity and virulence of the virus. As such, telehealth is ideally suited to meet the demands of inpatient care while at the same time reducing virus transmission, stretching human and technical resources, and protecting patients and healthcare workers in the inpatient care setting.
Initial reports suggest that 5% of COVID-19–infected patients require intensive care unit (ICU) services.9,10 Demands on clinicians (pulmonologists, intensivists, respiratory therapists, and nursing and other staff) may outstrip their ability to evaluate and monitor patients. Physical contact with COVID-19–infected patients significantly increases the chance of illness transmission and the need to quarantine exposed healthcare workers.11–13 Telehealth approaches allow staff—including those in quarantine, those in high-risk groups (older, immunosuppressed), and those with childcare responsibilities—to work remotely, supplementing in-person clinical services during the surge.
Healthcare enterprises may already have in place technologies that can be employed to accomplish telehealth. For example, telehealth carts used for telestroke programs can be redeployed for use in COVID-19 surge care. Alternatively, new devices, such as tablets, can be secured with an adjustable clamp on mobile structures such as intravenous medication poles and moved to locations as needed; these are a relatively inexpensive and quick alternatives to traditional telehealth carts. As an example, at Duke, we created a virtual pulmonologist or intensivist service (Tele-ICU) that allows specialists to remotely manage intubated patients. Physicians are able to see the ventilator settings, patients’ work of breathing, and remotely consult with the bedside team, while decreasing exposure risk and preserving personal protective equipment (Figure 3).
Figure 3.
Tele-ICU (iPad on a stick): rapidly deployed mobile virtual consult service. (A) The complete unit; (B) clamp attached to pole; (C) positioned bedside in patient room; (D) view for remote physician.
Table 2 describes the considerations necessary for executing a Tele-ICU service, including key stakeholders, changes to process, and the technologies we employed. Additional considerations (eg, equipment durability, infection prevention, data security, clinical usability) are also illustrated. The Tele-ICU approach is easily extended to the non-ICU setting, particularly for clinician-clinician communication and care of patients on isolation. As an added feature, our Tele-ICU approach allows medical trainees, who have been largely removed from clinical encounters because of COVID-19, to participate and support clinical staff, including inpatient rounds or outpatient experiences.
Table 2.
Rapidly Developing and Deploying a Tele-ICU Service During a Crisis
| People affected by the new approach |
|
| Processes/policieschanged to accomplish the new approach |
|
| Technologies implemented for the new approach |
|
HIPAA: Health Insurance Portability and Accountability Act; ICU: intensive care unit.
Strict visitor restrictions implemented by most hospitals can also cause patients to feel socially isolated. Mobile technologies, such as tablets or even personal smartphones, can allow patients to communicate with their families and friends using video or voice platforms. We have supplied isolation patients a dedicated portable device with video conferencing software for both their loved ones and our clinical staff to improve communication and support.
As these devices are adopted, hospitals must also consider how to disinfect them; protective cases should allow for easy cleaning. Key considerations for the adoption of these new devices include coordinated purchasing and registration through hospital information technology departments, ensuring data security of these devices and patient privacy. Although the surge crisis has meant that some individual institutions are temporarily allowing the use of popular video conferencing software, decisions about long-term adoption must include analysis of not only security vulnerabilities, but also current or future EHR integration. Further, hospital and patient broadband Internet must be evaluated, in particular given that many Americans still lack high-speed broadband.14,15
PHASE 3: POSTPANDEMIC RECOVERY
As of this writing, this phase is still unknown. Longer-term preparation for additional surge(s) of patients may materialize. There may also be a re-emergence of COVID-19 cases after movement restrictions are lifted. A growing “care debt” or deferred medical or surgical treatment may lead to increasing demand on a constrained healthcare system. This may include COVID-19 patients as well as those with other forms of acute and chronic diseases. For example, during the COVID-19 pandemic, emergency departments are reporting a decrease in visits, and unpublished reports describe a dramatic decrease of 40% to 70% in acute ST-segment elevation myocardial elevation cases.16 Deferral of care for serious conditions can cause downstream consequences, such as complications of unmanaged conditions including acute coronary syndromes, causing a surge in demand for care unrelated to COVID-19 infections. Cancelled elective surgical cases and treatments during the pandemic can add to this “care debt” that both patients and health systems may face. Along with the economic uncertainty of many healthcare organizations, further constraints to care capacity may be present during the postpandemic recovery phase.
Proactive patient engagement through telehealth may help a healthcare system to effectively manage these contingencies. Specifically, health systems should work to create a strong, sustainable telehealth infrastructure now that will allow for more efficient use of hospital space and staff. Telehealth service lines can be strengthened and even grow at affiliate and referring hospitals, including rural and critical access hospitals, linked into existing health systems’ telehealth networks.
With the transition to a postpandemic phase, the key transformation of telehealth systems is to shift from crisis mode (where the use of stopgap or unproven technologies has been permitted) to sustainable, secure systems that properly preserve data security and patient privacy and that offer sustained technical support for postcrisis care. The most straightforward approach is to extend and operationalize the changes to people, processes, and technologies explored in the first 2 phases, anticipating a sustained higher level of telehealth services. Of note, this will require the re-evaluation of regulation and policies and reimbursement models across multiple stakeholders including local healthcare organizations, state medical board, federal government, and payers. Both payers and healthcare professionals will need to re-examine their historical insistence on face-to-face patient-provider interactions where laying of hands is considered a sacrosanct component of care. While geographic and site restrictions for Medicare reimbursement have largely been waived with the Coronavirus Preparedness and Response Supplemental Appropriations Act of 2020,17 compensation models for different telehealth services will need to be actively updated by payers, including the federal government. In addition, the clinical outcomes of different types of visits (in-person, video, and telephone) must be examined to prevent potential perverse incentives leading to unnecessary increased video over potentially also effective telephone encounter caused by differential visit reimbursement. Planning for outcomes research is also needed to evaluate how COVID-19 changed our healthcare system, for better and worse. Given recent Federal Bureau of Investigation warnings about the vulnerability of some teleconferencing and televideo platforms,18 telehealth must not sacrifice privacy safeguards and digital security measures. The EHR can play a role here; most already allow patients to privately and securely obtain laboratory and imaging results, and recent reports of EHR-based clinical decision support and reporting tools are encouraging.19 Of note, a full assessment of the strengths and weaknesses of each type of encounter requires further study of clinical outcomes, financial return on investment for payers and society, improvement in patient experience, and provider wellbeing when the immediate crisis ends.
CONCLUSION
The COVID-19 pandemic has forced all healthcare systems, hospitals, and clinics to rapidly implement telehealth services, and delivery of patient care by the American health system will be forever changed. We are “going virtual” in the middle of a crisis, but we must still keep in mind the most essential phases of transformation and how best to deploy telehealth effectively. Whether or not healthcare enterprises are ready, the new reality is that virtual care has arrived.
AUTHOR CONTRIBUTIONS
All authors contributed sufficiently and meaningfully to the conception, design, drafting, editing, and revising the manuscript. All authors approved the final version for submission and agree to be accountable for all aspects of the work.
CONFLICTS OF INTEREST STATEMENT
JW reports working as a consultant with Access Physicians, a telemedicine company, outside the submitted work. All authors report no conflicts of interest related to the topic of the article.
REFERENCES
- 1. Augenstein J. Opportunities to expand telehealth use amid the coronavirus pandemic. Health Affairs Blog 2020. https://www.healthaffairs.org/do/10.1377/hblog20200315.319008/full/ Accessed March 23, 2020.
- 2. Galewitz P. Telemedicine surges, fueled by coronavirus fears and shift in payment rules. Kaiser Health News 2020. https://khn.org/news/telemedicine-surges-fueled-by-coronavirus-fears-and-shift-in-payment-rules/ Accessed March 29, 2020.
- 3. Hollander JE, Carr BG.. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020. Mar 11 [E-pub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4. Keesara S, Jonas A, Schulman K.. Covid-19 and health care's digital revolution. N Engl J Med 2020. Apr 2[E-pub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5. Leavitt HJ. Applied organisational change in industry: structural, technological and humanistic approaches In: March JG, ed. Handbook of Organization. Chicago, IL: Rand McNally; 1965: 1144–70. [Google Scholar]
- 6. Harvey JB, Valenta S, Simpson K, et al. Utilization of outpatient telehealth services in parity and nonparity states 2010-2015. Telemed J E-Health 2019; 25 (2): 132–6. [DOI] [PubMed] [Google Scholar]
- 7. Gough P. UPMC sees ‘phenomenal increase’ in telemedicine use in COVID-19 crisis. Pittsburgh Business Times 2020. https://www.bizjournals.com/pittsburgh/news/2020/03/28/upmc-sees-phenomenal-increase-in-telemedicine-use.html Accessed March 29, 2020.
- 8. Lurie N, Carr BG.. The role of telehealth in the medical response to disasters. JAMA Intern Med 2018; 178 (6): 745–6. [DOI] [PubMed] [Google Scholar]
- 9. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020. Feb 28 [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med 2020. Apr 6 [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Lancet. COVID-19: protecting health-care workers. Lancet 2020; 395 (10228): 922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ng K, Poon BH, Kiat Puar TH, et al. COVID-19 and the risk to health care workers: a case report. Ann Intern Med 2020. Mar 16 [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Remuzzi A, Remuzzi G.. COVID-19 and Italy: what next? Lancet 2020; 395 (10231): 1225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Perrin A. Digital gap between rural and nonrural America persists. Pew Research Center FactTank. 2019. https://www.pewresearch.org/fact-tank/2019/05/31/digital-gap-between-rural-and-nonrural-america-persists/ Accessed March 27, 2020.
- 15.Federal Communications Commission. 2019 Broadband Deployment Report. https://docs.fcc.gov/public/attachments/FCC-19-44A1.pdf Accessed April 1, 2020.
- 16. Wood S. The mystery of the missing STEMIs during the COVID-19 Pandemic; 2020. https://www.tctmd.com/news/mystery-missing-stemis-during-covid-19-pandemic Accessed April 1, 2020.
- 17. Lowey N. Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, H.R. 6074, 116th Congress, Public Law No. 116–123.
- 18. Setera K. FBI warns of teleconferencing and online classroom hijacking during COVID-19 pandemic. 2020. https://www.fbi.gov/contact-us/field-offices/boston/news/press-releases/fbi-warns-of-teleconferencing-and-online-classroom-hijacking-during-covid-19-pandemic Accessed April 1, 2020.
- 19. Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc 2020. doi: 10.1093/jamia/ocaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]