Abstract
This study provides data on the feasibility and impact of video-enabled telemedicine use among patients and providers and its impact on urgent and nonurgent healthcare delivery from one large health system (NYU Langone Health) at the epicenter of the coronavirus disease 2019 (COVID-19) outbreak in the United States. Between March 2nd and April 14th 2020, telemedicine visits increased from 102.4 daily to 801.6 daily. (683% increase) in urgent care after the system-wide expansion of virtual urgent care staff in response to COVID-19. Of all virtual visits post expansion, 56.2% and 17.6% urgent and nonurgent visits, respectively, were COVID-19–related. Telemedicine usage was highest by patients 20 to 44 years of age, particularly for urgent care. The COVID-19 pandemic has driven rapid expansion of telemedicine use for urgent care and nonurgent care visits beyond baseline periods. This reflects an important change in telemedicine that other institutions facing the COVID-19 pandemic should anticipate.
Keywords: COVID-19, telemedicine, ambulatory care, remote patient monitoring
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic is rapidly transforming the U.S. healthcare system, with telemedicine, or virtual health, being one of the key drivers of the change. This report, drawn from a large academic healthcare system with an existing telehealth infrastructure in New York City, at the epicenter of the COVID-19 pandemic, empirically demonstrates telemedicine’s transformative effect on healthcare delivery and the rapid shift in telemedicine adoption among both patients and providers.
In recent years, telemedicine’s growth has been incremental, and used by only 8% of Americans in 2019.1 Key barriers to wider adoption included limited reimbursement, lack of comfort with telemedicine technologies by patients and providers, and fundamentally, outside of rural medicine, few compelling cases for the replacement of in-person care.2 Despite these barriers, many healthcare systems have been investing in building a telemedicine capacity anticipating a future in which it would become more ubiquitous.
COVID-19 is transforming the telemedicine landscape with breathtaking speed. With no vaccine or effective therapies, social distancing and quarantine have been the only widely available interventions, creating a compelling reason for in-person care alternatives. U.S. insurers have quickly expanded coverage to include all telemedicine visit types including from home,3 and states relaxed their licensure requirements for care delivered across state boundaries.4 In addition to allowing for broad reimbursement of virtual visits, HHS waived enforcement of Health Insurance Portability and Accountability Act regulations to allow the use of consumer audio and video communication for telemedicine visits.4
With these changes, telemedicine is being leveraged with enormous speed and scale, turning into the forward “front line” of the battle against the pandemic. While the utility of telemedicine approaches in such a pandemic situation have been previously conceptualized,5 this report illustrates the largest experience to date describing the speed, scale, and reception of video-enabled visits by patients and providers in diverse settings (urgent care, primary care, specialty care) and charts implications for long-term healthcare delivery.
The emerging literature on the role of telemedicine in the response to COVID-19 has focused on health informatics infrastructure aspects,6 and primary care visits using mostly audio technologies.7 However, little data on both patient and provider telemedicine volume, the scalability of video visits, and in particular, trends of patients and providers’ migration to telemedicine have been reported. This case study describes the impact of the COVID-19 pandemic on telemedicine at one large health system.
MATERIALS AND METHODS
NYU Langone Health (NYULH), a large academic healthcare system in New York City, consists of 8077 healthcare providers across 4 hospitals and 500+ ambulatory locations all connected on a single electronic health record (EHR) system (Epic, Verona, WI). NYULH uses a single instance of the Epic health record with 7 545 427 active patients leveraging deep integration with the Vidyo (Hackensack, NJ) platform to enable its virtual health services. Prior to COVID-19, NYULH implemented telemedicine capabilities in approximately 25 locations. Its largest investment was in virtual urgent care, a fully integrated video visit experience tightly integrated into its enterprise EHR and its patient portal. Patients accessing the virtual urgent care were able to check in, pay, and have a video-enabled consultation with an NYULH emergency medicine physician that was reimbursed by multiple local payors. This system had been running since 2018 and on a typical day had <100 visits managed by a pool of about 40 ED providers who took visits either on site or at home.
Patients access these virus services through the NYU Langone Health app built upon the Epic MyChart suite of patient tools and using standard application programming interfaces made available by Epic. In addition, NYU Langone has deployed native open scheduling technologies as well as custom features enabling simplified virtual care access and matriculation. Patient satisfaction and engagement is assessed via brief text message surveys at the close of telemedicine encounters leveraging Q-Reviews (New York, NY). The questions in the survey assess domains including satisfaction with the visit, likelihood to use it again, and likelihood to refer a friend to the service. The mean of the responses to these 3 questions is reported in this article as the satisfaction rating.
Data for this survey were queried from the hospital system EHR from January 1 to April 14, 2020. We captured COVID-related visits by considering diagnosis codes containing relevant respiratory issues via partial matching with any of the following key words: (1) COVID, (2) RESP, (3) FLU, (4) PNEU, (5) FEVER, (6) SHORTNESS OF BREATH, (7) COUGH, (8) DYSPNEA, (9) PHARYNGITIS, (10) BRONCHITIS, (11) SINUSITIS, and (12) URI. Telemedicine encounters were then categorized into 2 groups: (1) urgent care and (2) nonurgent ambulatory care visits. Descriptive statistics were then conducted to estimate rates of telemedicine visits in urgent care and nonurgent care settings both COVID-19–related and not COVID-19–related.
RESULTS
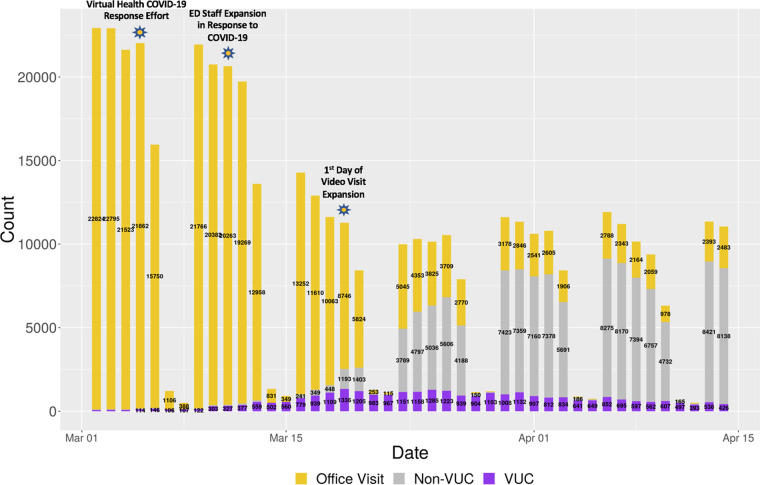
A mass migration to telemedicine has been taking place during March and April 2020, co-occurring with a decline of over 80% in in-person visits (see Figure 1). Telemedicine urgent care volume grew from 82 visits on March 4 to 1336 after 15 days. Of these visits, 55.3% were COVID-19–related, outpacing the 381 COVID-19 visits in all the NYULH emergency rooms that day. Telemedicine visits for urgent care were spread across age strata with the largest use in the group 20 to 44 years of age (see Table 1). The increase in telemedicine urgent care was enabled by a rapid increase in urgent care workforce from <40 emergency medicine providers to 289 “surge” providers from multiple specialties.
Figure 1.
Visit volumes increase in telemedicine urgent care (VUC) and nonurgent care (non-VUC) and decrease in in-person care. Each bar represents 1 day. Key dates are annotated above corresponding bars. COVID-19: coronavirus disease 2019; ED: emergency department.
Table 1.
Distribution of telemedicine visits by age
| Age (y) | Urgent care (%) | Nonurgent care (%) |
|---|---|---|
| <20 | 2.1 | 9.9 |
| 20-44 | 58.3 | 32.4 |
| 45-54 | 17.9 | 16.8 |
| 55-64 | 13.3 | 19.3 |
| 65-74 | 5.8 | 14.1 |
| 75-84 | 2.0 | 5.8 |
| >85 | 0.6 | 1.7 |
The increase in telemedicine urgent care was paralleled by a delayed but larger increase in ambulatory care video encounters (see Figure 1). Pre–COVID-19, <50 visits were conducted across nonurgent care specialties in a typical day. On March 19, the first day of expanded video visits to all ambulatory care, this volume increased to more than 1000 and reached over 7000 visits within 10 days (representing >70% of all ambulatory volume), with 19.9% COVID-19–related. In contrast to urgent care, these ambulatory visits were more evenly distributed among the age groups, though the 20 to 44 years of age group was still the largest utilizer.
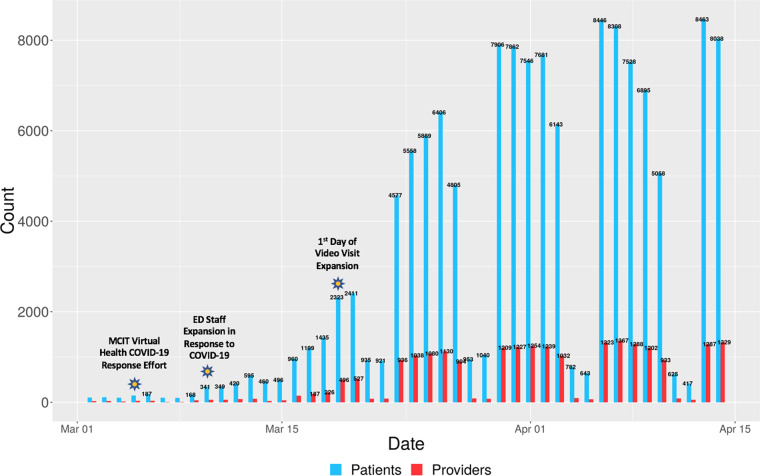
These changes in visit volume were driven by large-scale video-based telemedicine adoption by both patients and providers (see Figure 2), whose numbers increased hundredfold. Over an approximately 6-week period, there were 144 940 video visits conducted, involving 115 789 unique patients and 2656 unique providers. The virtual urgent care team alone conducted 16 545 COVID-19–related visits. At the same time, patients’ satisfaction ratings with telemedicine visits remained unchanged despite the rapid uptake of telemedicine by virtually inexperienced providers (pre-COVID: n = 847, mean satisfaction = 4.38/5; post-COVID: n = 1693, mean satisfaction = 4.38/5).
Figure 2.
Telemedicine adoption: daily count of unique patients and providers. Each 2 bars represent 1 day, and each bar is the volume of unique patients and providers using telemedicine each day. Key dates are annotated above corresponding bars. COVID-19: coronavirus disease 2019; ED: emergency department; MCIT: Medical Center Information Technology.
DISCUSSION
This report demonstrates the transformational impact of COVID on telemedicine-driven health care at the epicenter of the pandemic. Given NYU’s existing implementations, efforts during the COVID pandemic and reflected in the data presented here, specifically focus on types of expansions connected to the COVID-situation, rather than building our new systems. In all, results reflect what may become a new norm of future health care, and in particular during periods of contagious disease outbreaks. With a mass mobilization of healthcare providers onto diverse telemedicine platforms, an aspiration of the industry for years has materialized in a matter of days. In the telemedicine urgent care setting, this diversion of clinical care from in-person care has been a critical bulwark slowing the volume in more acute settings. With virtual urgent care utilization double that of emergency room visits at the height of the pandemic, these data substantiate the critical role of telemedicine in expanding emergency room capacity during a pandemic.
In the nonurgent care setting, the forced transition to video visits has demonstrated its feasibility, satisfaction, and value in promoting social distancing. In addition, telemedicine use enabled the mobilization of quarantined but asymptomatic providers who could now provide care remotely from their homes, thus mitigating the loss of highly needed resources.
Beyond the clinical benefits and more effective utilization of providers in very atypical circumstances, the changes instigated initially by the COVID-19 pandemic have likely irreversibly altered the position of telemedicine in the U.S. healthcare system. When prior literature speculated about the potential primacy of telemedicine over in-person care,8 it seemed futuristic, but it is now a reality practiced in multiple healthcare systems around the world. Using telemedicine platforms, providers and patients are being forced into a new normal that includes communicating with each other through video and audio.
For providers, this means quickly developing skills in virtual rapport building, empathy, “facilitated” physical exams, diagnosis, and counseling as curriculums get developed to train these new skills and new modalities of ensuring quality are developed. Trainees at our institutions now join our providers in multiparty video visits to observe and learn from these rapidly evolving skills and new norms. Moreover, providers quickly began asking for the ability to upload remote patient monitoring data (particularly temperature and pulse oximetry data in addition to blood pressure and glucose) into the EHR, a capability that had existed for years but was previously leveraged only by few providers in specialized use cases. The impact of widespread video visits on team-based care is also being reimagined, with new roles for ambulatory nurses, medical assistants, and front desk staff being created.
While recent reports of telemedicine rapid response focused on phone-based communication owing to technical, training and operational issues,7 telemedicine at NYULH is video based and characterized by consistently high patient satisfaction levels. Patients of all ages have quickly become used to sharing biometric data via their patient portal and answering screeners on their phones before their video visits. Pregnant women with hyperglycemia or hypertension now routinely sync their home monitoring devices to their providers through the EHR and are having expedited postpartum hospital stays enabled by telemedicine and remote monitoring. This experience will likely create future expectations of care convenience and accessibility that will be hard to reverse once the COVID crisis abates. Similarly, the regulatory changes invoked to support easily accessible widespread telemedicine may be equally difficult to reverse.
The ongoing battle against COVID-19 in the United States is still ongoing, and will likely stay at the top of healthcare systems’ agenda in the coming months. Yet telemedicine has already proved to be an invaluable tool to not only divert an overwhelming volume of patients from the emergency rooms, but also transform the work practices of thousands of providers, across multiple specialties. As demonstrated by the experience at an academic healthcare system at the epicenter of the pandemic in the United States, well-integrated virtual health tools can reliably manage thousands of patients over a short period of time, and provide care at times of acute shortage in healthcare personnel. The impact of telemedicine on COVID-19 response is matched by a likely enduring impact of COVID-19 on telemedicine, and through it on healthcare delivery in general, with a new reality of a broad population of Americans and their providers who are getting a crash course in using telemedicine tools, experiencing their capabilities, and establishing comfort and expectations of their widespread availability.
FUNDING
This work was supported by the National Science Foundation award #1928614.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to conception and design as well as acquisition of data or analysis and interpretation of data; were involved in drafting the manuscript or revising it critically for important intellectual content; gave final approval of the version published; and agreed to be accountable for all aspects of the work.
ACKNOWLEDGMENTS
The authors thank Dr Leora Horwitz for her thoughtful review and Tiffany Martinez for her assistance in the manuscript preparation.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.AmericanWell. Telehealth Index: 2019 Consumer Survey. https://static.americanwell.com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf Accessed March 30, 2020.
- 2. Dorsey ER, Topol EJ.. State of telehealth. N Engl J Med 2016; 375 (2): 154–61. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare and Medicaid Services. Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Accessed March 30, 2020.
- 4.U.S. Department of Health & Human Services. Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Accessed March 28, 2020.
- 5. Hollander JE, Carr BG.. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020; 382 (18): 1679–81. [DOI] [PubMed] [Google Scholar]
- 6. Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc 2020. Mar 24 [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA.. Rapidly converting to “virtual practices”: outpatient care in the era of covid-19. N Engl J Med Catalyst 2020; 1 (2). [Google Scholar]
- 8. Duffy S, Lee TH.. In-person health care as option B. N Engl J Med 2018; 378 (2): 104–6. [DOI] [PubMed] [Google Scholar]