To the Editor:
In the ongoing global pandemic, the practice of all medical specialties is affected, either primarily or secondarily. At this day, the 2 countries with the highest death rate are Italy and Spain. Medical resources and all personnel have been directed towards the COVID-19 pandemic, while depriving other patients of timely and effective medical care. We may refer to these untreated patients as collateral casualties. This has been observed initially in Wuhan1 and a few days ago in Thailand.2 We are seeing the same medical situation in our 2 countries, and while facing an unusually high number of casualties ourselves, we are also concurrently witnessing the exponential growth of cases in the United States3 and fear that this collateral damage situation may soon become a pandemic as well.
In our neurosurgical practice, we have noticed an increasingly alarming number of non-COVID-19 patients being affected by the current pandemic. The same has been seen by our cardiovascular surgical colleagues (personal communication). Given the growing demand for regular hospital and intensive care unit (ICU) beds, the care of patients with diverse neurosurgical pathologies is being delayed or directly canceled, bringing dire consequences to what should be a standard clinical outcome. For example, a 70-yr-old woman who developed a central cord syndrome after traumatic vertebral body fractures, involving the end plates of C4 and C5, underwent an uneventful regular anterior cervical fusion. We usually send such patients to the ICU overnight, but given the high proportion of COVID-19 cases in our ICU, we decided to send her to a regular hospital bed instead, after a few hours in the recovery room. Once there, she developed epiglottic edema, and not being immediately intubated or tracheostomized, she died. We consider her to be the collateral casualty of this viral pandemic, knowing well that she would have been saved if the regular protocol could have been followed.
In certain hospitals in Spain and in Northern Italy, the neurosurgeons and cardiac surgeons are currently serving on the COVID-19 teams, given the shortage of medical personnel. Due to the scarcity of ICU and hospital beds in Italy and Spain, the health administrations have designated the university hospitals or tertiary referral centers for the critical or complex COVID-19 patients, while other hospitals are being used for other emergencies and the treatment of virus-free patients. This policy may be unsuitable given that the neurosurgical patients require specialized equipment for the treatment of their conditions, which may be available only in the tertiary care medical centers. The most striking examples are young patients harboring neurological tumors or vascular lesions that require urgent nonelective intervention and intensive around-the-clock perioperative care.
Perhaps to some this may seem like an acceptable trade, a pawn sacrifice1 as in a chess game or in a war, but this is certainly not the case. An increased number of COVID-19 patients are occupying beds, while non-COVID-19 patients, some of whom are young and with life-threatening conditions, including tumors, aneurysms, and other vascular malformations, are not receiving timely neurosurgical procedures. In the past 2 wk, we have been following this alarming tendency, and it looks like it will not diminish, at least in the short term. These cases stand to increase during this viral pandemic and in the immediate aftermath to the extent that at some point the number of collateral victims may surpass the direct COVID-19 casualties.
Worldwide, the top 2 causes of deaths are ischemic heart disease and stroke, with more than 15 million deaths per year, while the non-COVID lower respiratory disease, be it communicable or otherwise, claims yearly close to 3 million victims.4 As the mainstream media seem to be more concerned about the mortality rates of the respiratory COVID-19 catastrophe, the collateral damage in this viral war is incurred by other patients, suffering from non-COVID-19 diseases, who deserve the same level of life-saving measures, in our case being the timely administration of appropriate and procedure intensive neurosurgical care.
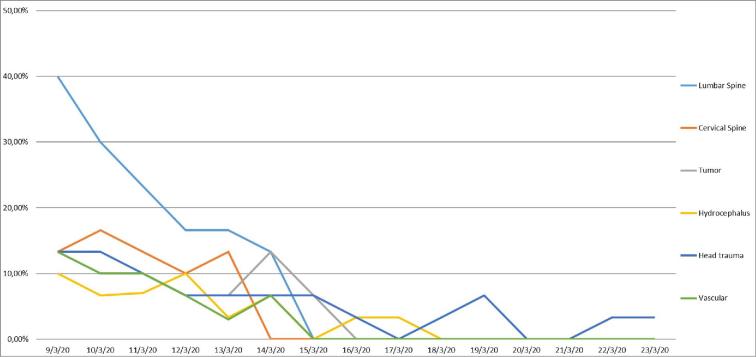
In our hospitals, we perform around 30 cases per day; operating on cerebral tumors and vascular conditions, and some of them in young patients, is being delayed while severe progressive cervical myelopathy cases are being canceled. Needless to say, so are lumbar cases with severe pain (Table and Figure). We are being forced to allocate patients with posterior fossa tumors or with other potential life-threatening conditions. In the United States, the American Association of Neurological Surgeons (AANS) has recommended a tiered framework regarding the election of surgeries5; however, our countries are currently so overwhelmed that this cannot be applied here, but we fear that, as this pandemic progresses to grow globally, the same situation may be shortly seen elsewhere, including the United States.
TABLE.
Total of Cases for Each Day
| 9/3/20 | 10/3/20 | 11/3/20 | 12/3/20 | 13/3/20 | 14/3/20 | 15/3/20 | 16/3/20 | 17/3/20 | 18/3/20 | 19/3/20 | 20/3/20 | 21/3/20 | 22/3/20 | 23/3/20 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lumbar spine | 40.00 % | 30.00 % | 23.30 % | 16.60 % | 16.60 % | 13.30 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % |
| Cervical spine | 13.30 % | 16.60 % | 13.30 % | 10.00 % | 13.30 % | 0.00 % | 0 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0 % | 0 % | 0.00 % | 0 % |
| Tumor | 13.30 % | 10.00 % | 10.00 % | 6.66 % | 6.66 % | 13.30 % | 6.66 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % | 0.00 % |
| Hydrocephalus | 10 % | 7 % | 7 % | 10 % | 3 % | 7 % | 0 % | 3 % | 3 % | 0 % | 0 % | 0 % | 0 % | 0 % | 0 % |
| Head trauma | 13.30 % | 13.30 % | 10.00 % | 6.66 % | 6.66 % | 6.66 % | 6.66 % | 3.33 % | 0.00 % | 3 % | 6.66 % | 0.00 % | 0 % | 3.33 % | 3.33 % |
| Vascular | 13 % | 10 % | 10 % | 7 % | 3 % | 7 % | 0 % | 0 % | 0 % | 0 % | 0 % | 0 % | 0 % | 0 % | 0 % |
| Median daily cases | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 |
| Total cases | 31 | 26 | 22 | 17 | 15 | 14 | 4 | 2 | 1 | 1 | 2 | 0 | 0 | 1 | 1 |
On Saturdays and Sundays, we perform selected elective or emergency cases. We divided our cases into 5 groups, and we did not include peripheral nerve, trans-sphenoidal surgery, radiosurgery, functional, including epilepsy, surgery and pain-related procedures, congenital anomalies, excluding hydrocephalus, or endoscopic procedures. Endovascular procedures are done by the radiology department in our centers.
Tumor cases include all cerebral types except those mentioned above.
Vascular cases include all cerebral types except those spinal.
Trauma includes all cerebral types, including chronic subdural hematomas.
Lumbar and cervical include all types of surgeries, including trauma.
Hydrocephalus includes all types of procedures, except those mentioned above.
Overall we included some pediatric cases, mainly hydrocephalus and tumors, but we are not working in a pediatric unit.
FIGURE.
We present the evolution of our surgical cases since the lockdown in Italy and Spain, and how it affected our practice. We perform from 27 to 35 cases per day, around 30 cases per day in four different hospitals. The relative percentages presented are related to the median number per day (n = 30).
Even though this “collateral epidemic” is not yet a pandemic itself, because it is not globally evident, the increasing proportion of cases and casualties may lead to a real “collateral pandemic” to be felt in all specialties. As this global crisis fades away, the economic rebound effect will surely follow, but for us this may be a mixed blessing being unable to bring back to life our patients whom we will have lost because they were denied a fair chance. It will be too late.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Acknowledgments
The authors are extremely thankful to Dr Gerald Chaban for his timely critical revision of the text.
REFERENCES
- 1. Time Magazine Hospitals in China, Overwhelmed by Coronavirus, Turn Away Patients With Other Pressing Needs, February 20, 2020. https://time.com/5788495/china-hospital-shortage. Accessed March 27, 2020.
- 2. Roxas MF. Collateral Damage in the Coronavirus Pandemic, March 27, 2020. https://www.rappler.com/thought-leaders/. Accessed March 27, 2020.
- 3. WHO Coronavirus Disease (COVID-19) Pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed March 28, 2020.
- 4. WHO. The Top 10 Causes of Death, May 24, 2018. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed March 27, 2020.
- 5. AANS Recommendations on Elective Surgery. https://www.aans.org/COVID-19-Update/COVID-19-Information-Hub. https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf. Accessed March 27, 2020.