Objectives:
To develop and implement a protocol to increase patient mobility in three adult ICUs using an interdisciplinary approach and existing resources.
Design:
The Iowa Model of Evidence-Based Practice was used for synthesis of literature and intervention planning. A retrospective pre- and post-intervention data collection design was used to compare outcomes of interest.
Setting:
Three adult ICUs (64 total beds) in an urban, academic hospital. Physician, nursing, respiratory therapy, physical therapy, and occupational therapy representatives participated in planning and development. All adult ICU patients were included.
Interventions:
Development and implementation of an inclusive early mobility protocol in three adult ICUs. Focus on interdisciplinary collaboration to restructure workflow, focusing on optimization and coordination of standard tasks. Multimodal education occurred in an interdisciplinary setting and on-site champions facilitated implementation.
Measurements and Main Results:
Time from admission to ambulation, overall frequency of ambulation, and frequency of ambulation by age group were assessed across three time periods: no awareness (Time 1), awareness without protocol (Time 2), and protocolization (Time 3). Decrease in hours from admission to ambulation were seen in the cardiovascular ICU (62.3 vs 56.1; p = 0.10) and surgical ICU (64.9 vs 58.6; p = 0.022). Significant increase demonstrated in the proportion of patients who ambulated while in the ICU (24.6% vs 33.0%; p < 0.001). All age groups had increase in frequency of ambulation. The largest gains in patients over 65 years old (T1 = 19.7%, T2 = 26.6%, T3 = 30.9%; p < 0.001). No change found in ICU length of stay, hospital length of stay, or ventilator days.
Conclusions:
This single-center evidenced-based practice project demonstrated increased mobility for ICU patients without addition of staff resources following implementation of an early mobility protocol using an interdisciplinary approach. Successful implementation led to creation of mobility protocol toolkit for use across all ICUs in the broader health system.
Keywords: early ambulation, early mobilization, evidence-based practice, intensive care, interdisciplinary health team, nursing
It is well documented in the literature that ICU survivors can suffer long-term deleterious effects after hospital discharge. Some of these are psychologic in nature, such as cognitive impairment, post-traumatic stress disorder, or persistent anxiety (1–3) often linked to increased occurrence of ICU delirium (1, 3). Additionally, survivors may experience a severely decreased level of physical function which can result in permanent disability (4, 5) and a persistent decrease in quality of life (6). Early mobility and exercise programs have been shown to improve outcomes for critically ill patients by decreasing the incidence of delirium (3, 7, 8), reducing the number of ventilator days (3, 7–9) and length of stay (LOS) (3, 7–9) as well as achieving a higher functional status at hospital discharge (7, 9). Early mobility has been recommended as part of the Society of Critical Care Medicine (SCCM) ICU Liberation Bundle aimed at reducing long-term consequences for ICU survivors (10). Unfortunately, implementation of early mobility programs continues to encounter barriers such as resource allocation, current clinical practice, and ICU culture (8, 11).
As in many ICUs, mobility practice at the University of Minnesota Medical Center (UMMC) was inconsistent. No established guidelines for mobilization were in place. Patients were assisted with activity as the medical providers or nurses subjectively determined appropriate. Often this activity included mechanical lift devices, further removing the physical involvement of the patient. Although staff was peripherally aware of the benefits of mobility, an informal review of practice and discussion with ICU nursing staff was able to identify several barriers to consistent early mobility practice including misconceptions surrounding safety of mobilizing ICU patients, lack of knowledge surrounding impact of mobility on patient outcomes, scarcity of resources, and inefficiencies in interdisciplinary coordination. This inconsistency was recognized by a multidisciplinary team on surgical ICU (SICU) and medical ICU (MICU) as an opportunity for quality improvement.
The objective of this evidence-based practice initiative was to develop and implement a protocol to increase patient mobility in three adult ICUs using an interdisciplinary approach and existing resources.
MATERIALS AND METHODS
Design
This evidence-based practice initiative applied The Iowa Model of Evidence-Based Practice (12) for synthesis of literature and intervention planning. A retrospective pre- and post-intervention data collection design was used to compare outcomes of interest. The local Institutional Review Board reviewed the study and waived the need for approval.
Sample and Setting
UMMC is a 347-bed urban, academic medical transplant center serving a high acuity population. It is the largest hospital in a system with 12 tertiary care centers and 56 primary care clinics. The adult ICUs are comprised of 64 beds divided into three distinct units: medical, surgical/neurologic, and cardiovascular. All ICUs currently employ the intensivist model of care, where one of four intensivist teams assumes primary care of a patient for the duration of their ICU stay.
Intervention
An interdisciplinary workgroup comprised of physician, nursing, physical and occupational therapy, respiratory therapy, and pharmacy representatives was formed and met biweekly. Since strong leadership support has been shown to be a key component of successful early mobility programs (8), the work group’s first task was confirming the change was in line with current organizational priorities through meetings with leaders at the local and system levels (12). Once organizational support had been confirmed, a review of the literature, practice recommendations by professional groups, and an assessment of current practice were performed. As previous work groups had successfully introduced a standard protocol for both spontaneous awakening trial and spontaneous breathing trial, this project was considered a continued investment in the ICU Liberation Bundle (10).
Evidence suggests that programs which use a set protocol have a multidisciplinary approach, address knowledge gaps, and occur in a setting with a culture that embraces quality improvement have had the greatest impact on patient outcomes (4, 8, 11, 13). Additionally, programs that use formal protocolization are shown to have a larger impact on patient outcomes than programs which use awareness promotion alone (4).
An interdisciplinary protocol was created for UMMC drawing from templates published in previous studies (4, 8, 14–17), recommendations from local expert ICU clinicians, and input from bedside staff. The protocol (Fig. 1) was designed to include all ICU patients unless they met exclusion parameters broken out into two categories: “hard stop” criteria, which denied participation due to clinical instability and “yield” criteria, which require consultation with the care team before proceeding. The “yield” criteria encourage shared decision-making in the context of the complete clinical picture. This was intended to avoid summary exclusion of patients because of therapies such as high levels of supplemental oxygen and low dose vasopressors, which may represent their baseline clinical condition. Guidelines were included for mobility progression, tolerance assessment, and reevaluation. An additional section in the template was included to highlight foundational principles and best practice regarding early mobility for reference by staff.
Figure 1.
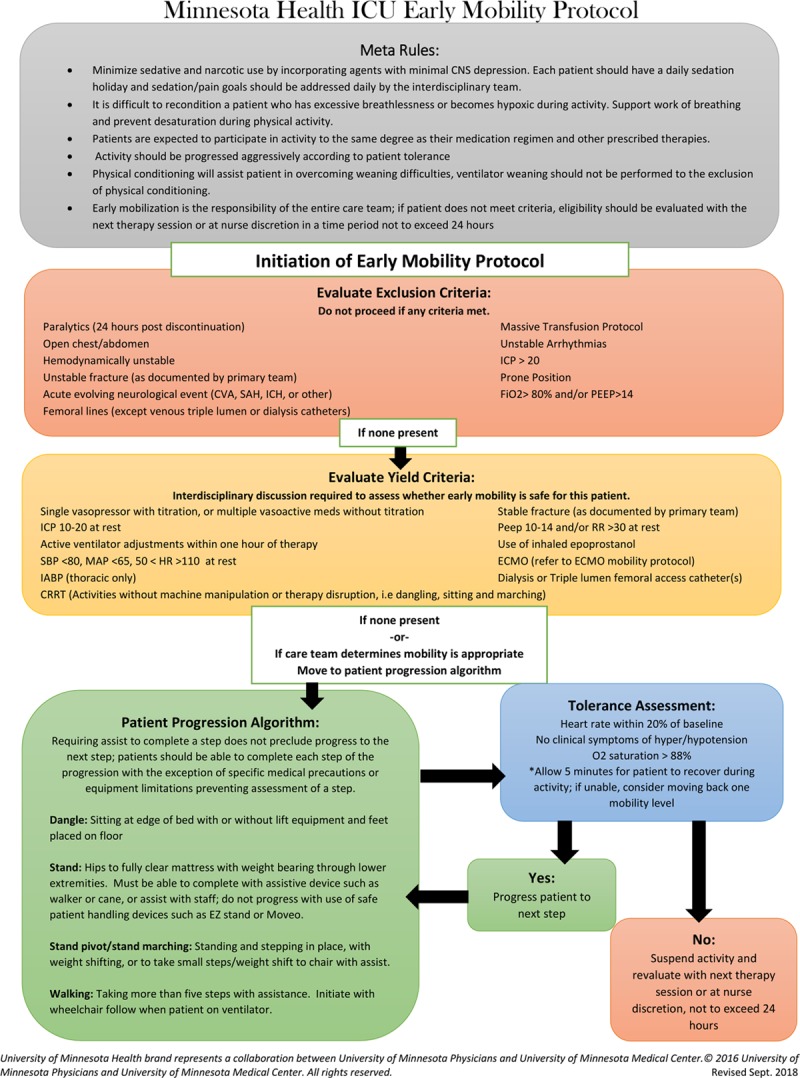
Minnesota Health ICU Early Mobility Protocol. Protocol developed for evaluating and completing early mobilization of critical care patients in the surgical, medical, and cardiovascular ICUs at the University of Minnesota. Protocol includes meta rules, evaluation criteria, progression algorithm, and tolerance assessment. CRRT = continuous renal replacement therapies, CVA = cerebrovascular accident, ECMO = extracorporeal membrane oxygenation, EZ stand = patient handling device, HR = heart rate, IABP = intra-aortic balloon pump, ICH = intracerebral hemorrhage, ICP = intracranial pressure, MAP = mean arterial pressure, PEEP = positive end-expiratory pressure, RR = respiratory rate, SAH = subarachnoid hemorrhage, SBP = systolic blood pressure.
Resource scarcity was of high concern in this project. Dedication of additional personnel has been shown to be a facilitator of mobility (4, 10). In this case, adding staff was not an option due to existing budgetary restrictions. As an alternative, resolving inefficiencies in the existing process was targeted to free up resources required (8, 11, 13). Workflow for each discipline was examined, focusing on optimization and coordination of standard tasks and optimal timing for labor-intensive mobility sessions. A formalized communication process was developed which established a daily planning discussion regarding patients requiring the assistance of multiple disciplines to mobilize. The respiratory, physical, and occupational therapists assigned to the ICUs met each morning to discuss timing and equipment required for complex patients. A representative from this group would then coordinate planning with the bedside nurse to prevent the mobility session from coinciding with other planned tests or procedures. This also allowed the bedside nurse to plan to be available and to have the patient ready for the mobility session. Coordinating in this fashion streamlined planning, decreased the amount of staff downtime experienced during preparation for each session, ensured all required staff were present, and allowed for equitable allocation of mobility sessions if the number of patients exceeded the available resources.
Equipment that is easily accessible and dedicated to ICU mobility may also decrease required staff time. Since funds were not available through traditional means, monies were requested and obtained from the Fairview Foundation, a philanthropic organization dedicated to supporting efforts which positively impact the patients and communities served by the Fairview Health System, which includes UMMC. These funds were used to purchase mobility carts designed to organize essential equipment, such as monitors, ventilator, IV pumps, and drains, and dedicated transport ventilators.
An intensive, multimodal education plan was developed targeting all members of the interdisciplinary team. Education strategies included as follows: communication through email and staff meetings, poster displays in common staff areas, and face-to-face education. In-person education was offered to an interdisciplinary cohort of volunteer champions, allowing for shared ownership of the process between all members of the care team. Two hours of education centered on the negative effects of bed rest, benefits of early mobilization for ICU patients, safety of early mobility programs, and how to use the protocol was offered on two dates and was paid for by each unit. The teach-back method was used to validate learning.
The start date of the protocol was accompanied by the introduction of the new mobility carts. On-site support was provided for 3 weeks postimplementation, consisting of two volunteers per day who volunteered to round the ICU departments for 2 hours before and after shift change. During this time, project team members and champions rounded through each of the ICUs answering questions, providing real-time staff education, and assisting in patient mobility.
Measurement Methods and Tools
Since ambulation is the highest level of activity, it was chosen as the desired process outcome. Time from admission to first occurrence and frequency of ambulation were both assessed. Patient outcome metrics included ICU LOS, hospital LOS, and average length of ventilator episode. Adverse safety events such as a fall or loss of tube were evaluated as a negative outcome. Staff perceptions surrounding mobility were assessed using a five-question survey, four questions on a 5-point Likert scale, and one free text question targeting existing barriers to mobility.
Data Collection and Statistical Analysis
Process and patient outcomes were compared during three time periods: Time 1, no awareness of early mobility (January 2015 through August 2015); Time 2, awareness without protocol (September 2015 through August 2016); and Time 3, after formalization of the protocol (September 2016 through June 2017). Time 1 occurred before any staff had been educated on the benefits of early mobilization, Time 2 was defined as when an interdisciplinary cohort with increased awareness began to share protocol information using a persistent word of mouth initiative, and Time 3 occurred after implementation of the protocol. Staff surveys were distributed 4 months postimplementation of protocol.
Clinical data were collected using aggregated reports generated from the electronic health record (EHR); staff feedback was obtained via anonymous staff surveys. Data were collected and examined retrospectively. No individual-level data were examined. Descriptive statistics, counts of patient encounters, were compiled overall and per unit. chi-square tests were to compare the percentage of patients that were ambulated across the time periods, overall and by unit. Patient outcomes were compared across the time periods using an analysis of covariance. Hours from admission to ambulation were compared between T1 and T3. All data analysis was completed using SAS version 9.4 (SAS Institute, Cary, NC) and a 0.05 alpha level was considered statistically significant.
RESULTS
After protocol implementation, a significant increase was seen in the proportion of patients who ambulated while in the ICU (24.6% vs 33.0%; p < 0.001). No significant changes were noted in ICU LOS, hospital LOS, or ventilator days (Table 1). Frequency of ambulation occurrence was also examined by age group (Figs. 2–4). All age groups demonstrated significant overall increase, with the largest gains seen in patients over 65 years old (T1 = 19.7%, T2 = 26.6%, T3 = 30.9%; p < 0.001). Decreases in the hours from admission to ambulation were seen in the cardiovascular ICU (CVICU) (62.3 vs 56.1; p = 0.10) and SICU (64.9 vs 58.6; p = 0.022), while the MICU showed an increase (62.1 vs 72.3; p = 0.035) (Fig. 5).
Table 1.
Demographics and Outcomes
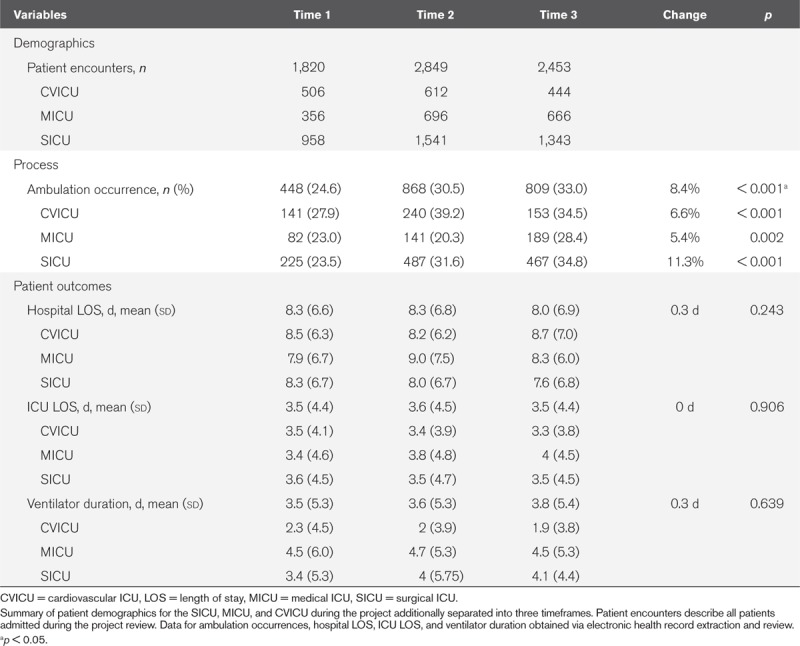
Figure 2.
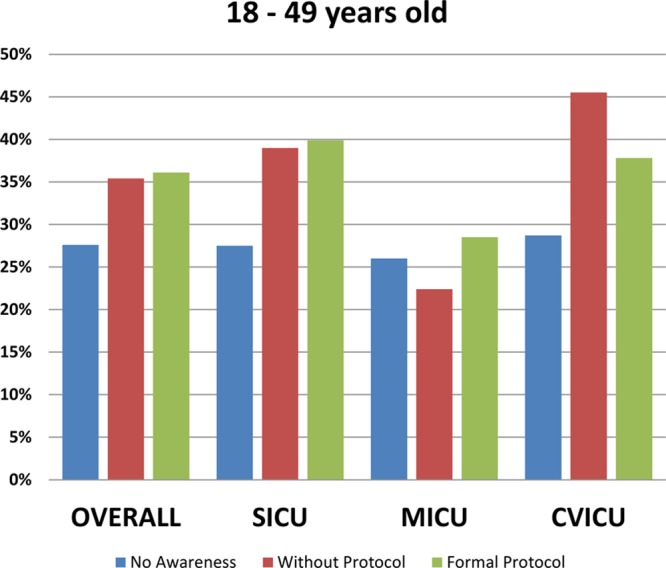
ICU ambulation (18 to 49). Percentages of patients 18 to 49 yr old mobilized to ambulation in the ICU across three timelines: “No Awareness” indicates staff did not have an awareness of an early mobility protocol, “Without Protocol” defines the timeframe staff was aware of value and importance of early mobilization of ICU patients but did not have a formal protocol, and “Formal Protocol” designates the timeframe staff had a protocol to direct early mobility in the ICU. CVICU = cardiovascular ICU, MICU = medical ICU, SICU = surgical ICU.
Figure 4.
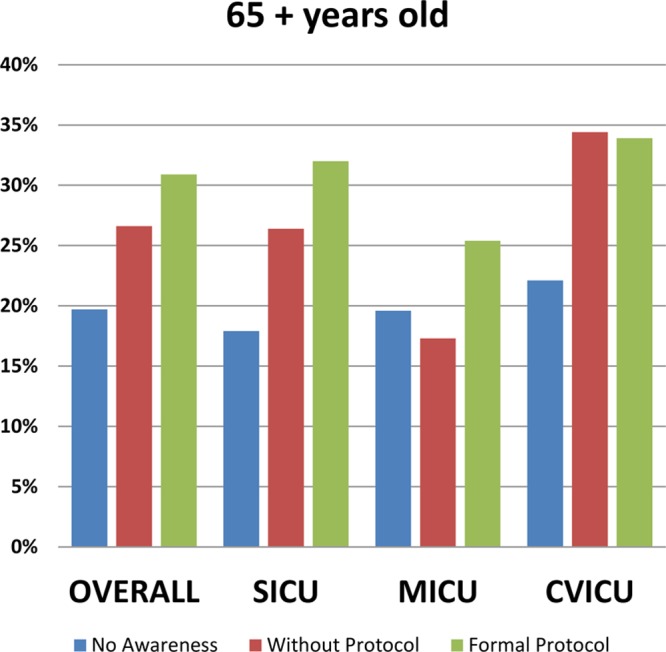
ICU ambulation (65 and older). Percentages of patients 65 yr old and older mobilized to ambulation in the ICU across three timelines: “No Awareness” indicates staff did not have an awareness of an early mobility protocol, “Without Protocol” defines the timeframe staff was aware of value and importance of early mobilization of ICU patients but did not have a formal protocol, and “Formal Protocol” designates the timeframe staff had a protocol to direct early mobility in the ICU. CVICU = cardiovascular ICU, MICU = medical ICU, SICU = surgical ICU.
Figure 5.
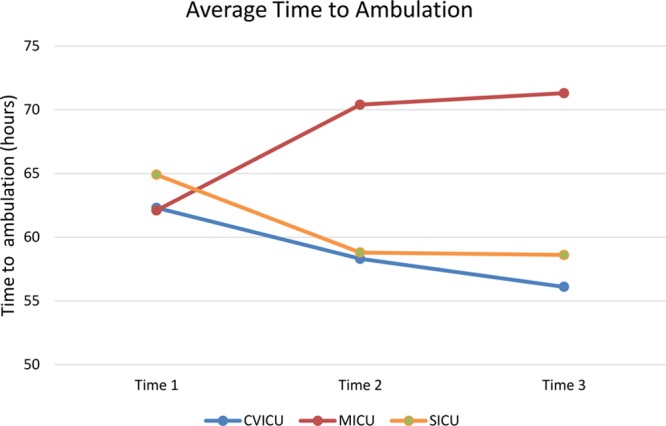
Average time to ambulation. Length of time required to initiate early mobilization of ICU patients in the cardiovascular ICU (CVICU), medical ICU (MICU), and surgical ICU (SICU) across three defined time periods. Time 1 is in which staff did not have an awareness of an early mobility protocol, Time 2 defines the timeframe staff was aware of value and importance of early mobilization of ICU patients but did not have a formal protocol, and Time 3 designates the timeframe staff had a protocol to direct early mobility in the ICU.
Figure 3.
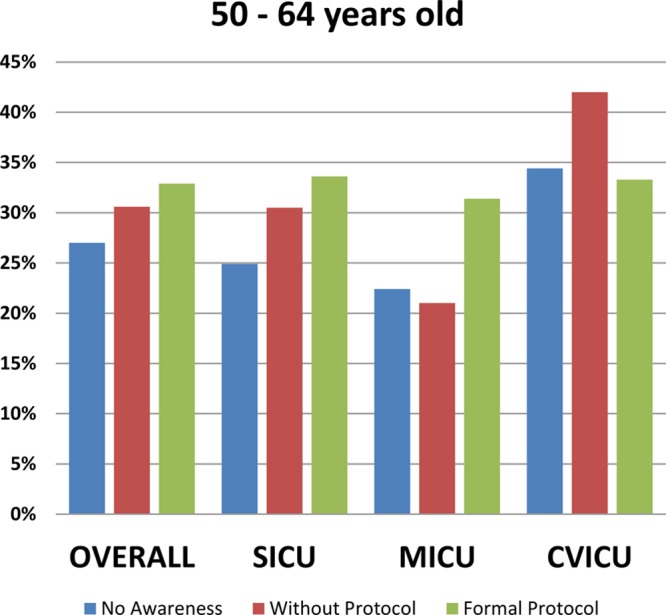
ICU ambulation (50 to 64). Percentages of patients 50 to 64 yr old mobilized to ambulation in the ICU across three timelines: “No Awareness” indicates staff did not have an awareness of an early mobility protocol, “Without Protocol” defines the timeframe staff was aware of value and importance of early mobilization of ICU patients but did not have a formal protocol, and “Formal Protocol” designates the timeframe staff had a protocol to direct early mobility in the ICU. CVICU = cardiovascular ICU, MICU = medical ICU, SICU = surgical ICU.
A response rate of 16.5% was achieved for the nursing, nursing aide, and respiratory therapy staff survey (56 registered nurses, 3 nursing assistants, and 13 respiratory therapists; total n = 72). Of the respondents, 55.6% indicated that they felt comfortable to very comfortable using the protocol, 55.5% almost/always mobilize patients per protocol, and 69.5% indicated they have the resources they need for patient mobility. The most common barrier recorded (50% of comments) during the survey period was presence of additional staff required to mobilize complex patients (n = 28).
There were 2,125 occurrences of ambulation in the ICUs during the study period. No adverse events including accidental loss of IV access, unintended extubations, or patient falls directly associated with mobility were reported during the project. Since there was no way to track adverse events in the EHR, these numbers are based on reporting alone.
DISCUSSION
This study offered the unique opportunity to study the difference in initiation and frequency of early mobility across three ICUs in three distinct time periods, demonstrating the evolution of practice from no awareness (Time 1) to awareness without protocol (Time 2) to formal protocolization (Time 3). The notable increase in patient mobilization in Time 2 indicates that awareness is a key component of practice change. All members of the multidisciplinary workgroup were actively promoting early mobility through demonstration and word of mouth. Although the gains seen from Time 2 to Time 3 were more modest, it demonstrates the value of formalizing practice through validated education and protocolization. Unit level data suggested that the increase in proportion of patients who ambulated was not linear; however, each unit ended with a significant increase in the proportion of patients who ambulated during their ICU stay when compared with Time 1, making the project an overall success. The variation in increases may indicate differences in patient population and unit culture. This could be an area for further investigation.
Patients over 65 years old made the greatest gain in frequency of ambulation, both overall and at the unit level. This age group had the lowest mobility level in Time 1 by a significant margin which increased to nearly the same level as the 50–64 age group by Time 3. This is an important finding as increased age is associated with worse overall ICU outcomes (18, 19); increased mobility may be a way to mitigate that. The variation between baseline practice and subsequent increase after education may reflect staff comfort level in aggressively mobilizing older patients; however, further studies about staff perceptions of patient tolerance relative to age would be required.
It is unclear why there is a discrepancy in the trends for the units with respect to hours from admission to ambulation. The observed decreases in the SICU and CVICU were the expected outcome considering that the ICU nurses, nursing aides, and respiratory therapists that participated in the project survey stated that they felt more comfortable. Further investigation of current data controlling for other variables, such as patient acuity and overall hospital LOS, or a more in-depth examination of staff perceptions broken out by unit would be helpful in better understanding this pattern.
The interdisciplinary nature of this effort was integral to its success. The original interdisciplinary workgroup members first became aware of early mobility practice in the context of the SCCM ICU Liberation Bundle (21). This project was intentionally inclusive of multiple disciplines in concordance with recommendations from the SCCM. The interdisciplinary nature guaranteed that all stakeholders had a voice during protocol development and fostered interdisciplinary collaboration during the protocol launch. The working group was able to identify challenges and strengths unique to each discipline and incorporate those into implementation strategies. Additionally, the protocol was designed to be owned by the entire ICU team, spreading the responsibility of patient mobility over all disciplines.
The presence of the project champions to address barriers and provide real-time education was invaluable. Demonstration of how best to use the mobility carts and reinforcing the safety of patient mobilization served to further integrate the education. Following the interdisciplinary model, there were representatives of each group on the champion team. This developed collaborative working relationships while utilizing opinion leaders from all disciplines.
It was with this model in mind that the decision to offer multidisciplinary education sessions was made. The interdisciplinary education allowed staff to interact with other disciplines in a way that had not occurred in the previous milieu. These personalized interactions and dialogs fostered interdisciplinary relationships and challenged preconceptions about involvement, role expectations, and time constraints. Project leaders were able to identify potential challenges and collect feedback during the education sessions, allowing for the identification and reduction of barriers prior to implementation.
Sustainability of projects such as this is always a concern. At UMMC, all critical care nurses were presented with a review of the evidence, current protocol, and practice expectations embedded in annual required education 1 year after implementation. This review ensured the education of new staff and provided an opportunity to address concerns of existing staff. The physical therapy and occupational therapy departments both include ICU early mobility education in their orientation. Continued in-person presentation of the early mobility protocol versus an annual electronic learning module for sustainment remains an active discussion.
Early in the implementation staff were limited by lack of activity orders; to avoid this, the early mobility protocol was incorporated into the standard ICU admission order set in January of 2018. This change added the protocol as reference link within each activity order regardless of type (up ad lib, ambulate with assist, etc.). Finally, the early mobility effort is also included in subsequent practice improvement projects such as the implementation of a structured patient care rounding format.
The successful implementation of an early mobility program at UMMC has led to the movement toward widespread adoption in all ICUs in the Fairview Health System. A toolkit has been created to guide interdisciplinary teams through the implementation process. It includes recommendations regarding key members of the project workgroup, education materials for champions and staff, possible metrics, and reference materials. Members of the original workgroup have made themselves available to help facilitate protocol implementation at other sites.
Finally, concerns about patient safety during activity in the ICU are a common barrier. During this project, there were 2,125 occurrences of ambulation in the ICUs, covering a broad range of patient acuity levels. No adverse events were reported to the hospital patient event reporting system during the project further supporting the evidence that early mobility in the ICU is safe for patients (21, 22).
This quality improvement project has some limitations. First, this was is a single-center project and our results may not be generalizable to all ICUs. Protocol specifics and education strategies may require adjustments based on available resources such as funding for equipment, staff education, and presence of PT/OT staff on the unit. Our center has a dedicated PT and OT on each ICU who play a very active role in the daily planning and execution of early mobility practice. We understand that this is an advantage over centers with fewer available staff.
A second factor that makes this project unique is the time period between when staff was unaware of the benefits of early mobility and when the formal protocol was created. This time period comprised a significant period of raising awareness by local opinion leaders and formal leadership. This led to the allocation of funding for specialized equipment and also likely contributed to the significant culture change that transpired with respect to early mobility.
Finally, ambulation was chosen as the outcome of interest for this project because it was considered the highest level of mobility. Successful increase in ambulation likely corresponds to an increase in other mobility events. However, current documentation inconsistencies prevented other events from being accurately measured. The data on ambulation may have been affected by these limitations as well. Under-documentation or documentation in a nonqueried EHR field may have led to overall underreporting of mobility events.
CONCLUSIONS
This single-center evidenced-based practice initiative demonstrated successful design and implementation of an early mobility protocol across three adult ICUs, demonstrating an overall increase in occurrence of ambulation, decreased time from ICU admission to ambulation in two of the three ICUs, and high proportion of ICU staff who feel comfortable using the protocol to mobilize patients. Interdisciplinary collaboration to develop consistent workflow and communication was key to the success of the project. This has resulted in a lasting, positive culture change in the adult ICUs without an increase in personnel. Ongoing efforts have led to incorporation of the protocol in the standard ICU admission order set, continuing education for all disciplines, development of an implementation toolkit, and plans to expand the protocol throughout the health system.
ACKNOWLEDGMENTS
Statistical review provided by Michelle Mathiason Moore and data extraction assisted by Lisa Hienrich.
Footnotes
This quality initiative was financially supported by the Fairview Foundation’s “Greatest Needs Fund.”
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Parker AM, Sricharoenchai T, Raparla S, et al. Posttraumatic stress disorder in critical illness survivors: A metaanalysis. Crit Care Med. 2015; 43:1121–1129 [DOI] [PubMed] [Google Scholar]
- 2.Patel MB, Jackson JC, Morandi A, et al. Incidence and risk factors for intensive care unit-related post-traumatic stress disorder in veterans and civilians. Am J Respir Crit Care Med. 2016; 193:1373–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barr J, Fraser GL, Puntillo K, et al. ; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; 41:263–306 [DOI] [PubMed] [Google Scholar]
- 4.Morris PE, Goad A, Thompson C, et al. Early. intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008; 36:2238–2243 [DOI] [PubMed] [Google Scholar]
- 5.Herridge MS, Tansey CM, Matté A, et al. ; Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011; 364:1293–1304 [DOI] [PubMed] [Google Scholar]
- 6.Herridge MS, Cheung AM, Tansey CM, et al. ; Canadian Critical Care Trials Group. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003; 348:683–693 [DOI] [PubMed] [Google Scholar]
- 7.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet. 2009; 373:1874–1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engel HJ, Needham DM, Morris PE, et al. ICU early mobilization: From recommendation to implementation at three medical centers. Crit Care Med. 2013; 41:S69–S80 [DOI] [PubMed] [Google Scholar]
- 9.Li Z, Peng X, Zhu B, et al. Active mobilization for mechanically ventilated patients: A systematic review. Arch Phys Med Rehabil. 2013; 94:551–561 [DOI] [PubMed] [Google Scholar]
- 10.Society of Critical Care Medicine: ICU Liberation Bundle. Available at: https://www.sccm.org/ICULiberation/ABCDEF-Bundles. Accessed March 25, 2020
- 11.Parker A, Sricharoenchai T, Needham DM. Early rehabilitation in the intensive care unit: Preventing physical and mental health impairments. Curr Phys Med Rehabil Rep. 2013; 1:307–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Titler MG, Kleiber C, Steelman VJ, et al. The iowa model of evidence-based practice to promote quality of care. Crit Care Clin. 2001; 13:497–509 [PubMed] [Google Scholar]
- 13.Phelan S, Lin F, Mitchell M, et al. Implementing early mobilization in the intensive care unit: An integrative review. Int J Nur Stud. 2018; 77:91–105 [DOI] [PubMed] [Google Scholar]
- 14.Brummel NE, Jackson JC, Girard TD, et al. A combined early cognitive and physical rehabilitation program for people who are critically ill: The activity and cognitive therapy in the intensive care unit (ACT-ICU) trial. Phys Ther. 2012; 92:1580–1592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hodgson CL, Stiller K, Needham DM, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014; 18:658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hopkins RO, Spuhler VJ. Strategies for promoting early activity in critically ill mechanically ventilated patients. AACN Adv Crit Care. 2009; 20:277–289 [DOI] [PubMed] [Google Scholar]
- 17.Mendez-Teller P, Needham DM. Early physical rehabilitation in the ICU and ventilator liberation. Respir Care. 2012; 57:1663–1669 [DOI] [PubMed] [Google Scholar]
- 18.Fuchs L, Chronaki CE, Park S, et al. ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med. 2012; 38:1654–1661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peigne V, Somme D, Guérot E, et al. Treatment intensity, age and outcome in medical ICU patients: Results of a French administrative database. Ann Intensive Care. 2016; 6:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ely EW. The ABCDEF bundle: Science and philosophy of how ICU liberation serves patients and families. Crit Care Med. 2017; 45:321–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adler J, Malone D. Early mobilization in the intensive care unit: A systematic review. Cardiopulm Phys Ther J. 2012; 23:5–13 [PMC free article] [PubMed] [Google Scholar]
- 23.Taito S, Shime N, Ota K, et al. Early mobilization of mechanically ventilated patients in the intensive care unit. J Intensive Care. 2016; 4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]


