Supplemental Digital Content is available in the text.
Keywords: emergency medicine, hyperkalemia, hypoglycemia, insulin, intensive care units, length of stay
Objectives:
The objectives of this study were to evaluate the safety and efficacy of insulin dosing of less than 10 units versus 10 units in patients receiving hyperkalemia treatment.
Design:
Retrospective single-center study.
Setting:
Emergency department at a large academic medical center in the United States.
Patients:
Seven hundred adults treated for hyperkalemia with IV regular insulin between April 1, 2013, and September 27, 2018.
Interventions:
Patients that received less than 10 units of insulin were compared to those that received 10 units of insulin.
Measurements and Main Results:
Patients treated with less than 10 units had significantly lower frequency of hypoglycemia (11.2% vs 17.6%; p = 0.008). Reduction in serum potassium was significantly more modest in size in patients treated with less than 10 units (mean reduction 0.94 ± 0.71 mMol/L) compared with patients treated with 10 units (mean reduction 1.11 ± 0.8 mMol/L; p = 0.008). There were no statistically significant differences between groups in time to hypoglycemia, nadir serum glucose, severe hypoglycemia (<40 mg/dL), dextrose requirements, use of concurrent agents for hyperkalemia, need for repeat insulin dosing, length of stay, or mortality.
Conclusions:
Patients treated for hyperkalemia with insulin doses less than 10 units had reduced frequency of hypoglycemia; however, potassium reduction post treatment was more modest in these patients. These findings suggest providers choosing to administer 10 units IV insulin should ensure patients have adequate monitoring for hypoglycemia.
Hyperkalemia is a common, life-threatening electrolyte disorder characterized by a serum potassium level greater than 5 mMol/L (1, 2). Hyperkalemia may result in neuromuscular, gastrointestinal, and metabolic abnormalities and induce fatal cardiac arrhythmias (1, 2). Current treatment options focus on temporizing measures to stabilize the cardiac membrane, redistribute extracellular potassium into cells, and enhance elimination of excess potassium until the underlying cause of hyperkalemia can be addressed (1, 2).
IV regular insulin is often used during acute hyperkalemia management due to its quick onset of action and moderate duration of redistribution effect (off-label use) (1, 2). Insulin 10 units is estimated to lower serum potassium by 0.6–1.2 mMol/L within 15 minutes of administration with effects lasting 4–6 hours (1–3). However, insulin may also induce unwanted effects, such as hypoglycemia (1, 2). Guidelines often recommend administration of 10–20 units of insulin with concurrent dextrose to prevent hypoglycemia during treatment (1, 2, 4–6). Despite coadministration with dextrose, hypoglycemia may still occur in 8.7%–28.6% of patients (7–9).
Because hypoglycemia has been associated with increased mortality, it is imperative that providers identify strategies for reducing hypoglycemia risk during insulin administration (10–13). Recent studies have identified that lower insulin doses, such as 5 units or 0.1 U/kg, may reduce the risk of hypoglycemia (8, 14, 15). However, these lower doses may reduce the ability to reduce serum potassium (15). The objective of this study was to evaluate the safety and efficacy of insulin doses less than 10 units for the treatment of adults with hyperkalemia.
MATERIALS AND METHODS
This was a retrospective chart review of adults treated for hyperkalemia (serum potassium > 5 mMol/L) with IV regular insulin in the emergency department (ED) at a 507-bed, academic teaching hospital between April 1, 2013, and September 27, 2018. The 65-bed ED treats adult and pediatric patients and has approximately 76,000 visits per year. Patients were initially identified if they received any medication order for regular insulin while in the ED. Patients were excluded if they did not have pretreatment and posttreatment (within 12 hr of insulin administration) serum potassium and glucose measurement, if they received more than 10 units of insulin as a single dose, if they did not received insulin IV if they were less than 18 years old, or if they were a prisoner. The study was approved by the institutional review board (no 5180329), and the requirement for informed consent was waived.
At the study site, hyperkalemia treatment was not protocolized, and providers could select any desired agent and dose. A hyperkalemia order set, which included calcium, albuterol, and insulin, was available to providers; however, use was not required when ordering IV insulin. All ED medication orders were required to be reviewed and approved by a pharmacist prior to administration. ED pharmacists were present in the ED for 10 hours per day, 7 days per week, and evaluated all ED medication orders when present. Outside of those hours, inpatient pharmacists located in the main pharmacy evaluated ED medication orders.
Patients treated with insulin 10 units were compared with those treated with less than 10 units. The primary outcome was frequency of hypoglycemia (serum glucose < 70 mg/dL) within 12 hours of insulin administration. This 12-hour interval was selected due to previous literature reporting prolonged insulin duration of action in patients with renal impairment (16, 17). Secondary outcomes included the following: time to hypoglycemia, nadir serum glucose, frequency of severe hypoglycemia (serum glucose < 40 mg/dL), change in serum potassium, IV dextrose requirements, use of concurrent agents for hyperkalemia treatment, length of ICU stay, length of hospital stay, and in-hospital mortality. With the exception of ICU and hospital length of stay and mortality, all secondary outcomes were evaluated after 12 hours of insulin dose. If patients required multiple insulin doses within 12 hours of initial hyperkalemia treatment, safety- and efficacy-related outcomes (i.e., change in serum glucose and potassium) prior to the second dose were evaluated. Demographic data, including data related to past medical history, home medication use, and severity of hyperkalemia presentation, were also collected. Kidney status at baseline and presence of arrhythmias prior to or after hyperkalemia treatment were determined using provider progress notes. All data were collected by retrospective review of electronic medical records.
A sample size calculation indicated that 690 patients (345 in each group) were necessary to detect a 9.1% difference in hypoglycemia frequency, assuming two-sided test with an alpha of 0.05 and a power of 0.8. This estimated difference in hypoglycemia frequency was based on the findings of LaRue et al (8), which demonstrated hypoglycemia in 28.6% of patients treated with 10 units and 19.5% in those treated with 5 units (difference 9.1%).
Descriptive statistics for quantitative variables are presented using the mean with sd for parametric data or the median with first and third quartile (interquartile range [IQR]) for nonparametric data. Categorical variables are presented as number and percentage. The two-independent samples t test was used to compare quantitative variables between groups, whereas the Mann–Whitney U test was used when the data were not normally distributed. Chi-square test, or Fisher exact test when assumptions of chi-square were not met, was used to assess associations between categorical variables between groups. Univariate and multiple regression analyses were used to evaluate predictors of hypoglycemia and serum potassium response to treatment. Variables included in these analyses were determined by statistically significant differences in baseline demographics. Because lower pretreatment glucose, no previous diagnosis of diabetes, kidney dysfunction, lower body weight, and female sex have been previously identified as risk factors for hypoglycemia, these factors were selected for univariate analysis a priori (7, 14, 15, 18). ICU admission was expected to affect risk of hypoglycemia and serum potassium reduction and was included in univariate analyses a priori. Statistically significant predictors from the univariate analyses for hypoglycemia frequency and potassium reduction were entered simultaneously into multiple regression analyses. Statistical significance was set at a p value of less than 0.05. Statistical analysis was performed using SPSS Statistics software (Version 25.0; IBM Corp., Armonk, NY).
RESULTS
Three-thousand thirteen patients who received regular insulin were screened for inclusion. Seven hundred patients met inclusion criteria (Fig. 1). Demographic data are summarized in Supplemental Table 1 (Supplemental Digital Content 1, http://links.lww.com/CCX/A145). Patients treated with less than 10 units of insulin had significantly lower initial serum glucose versus patients who received 10 units of insulin (114 [IQR, 92–171] vs 139 [IQR, 102–212] mg/dL; p = 0.0001). There were no other significant differences in demographics.
Figure 1.
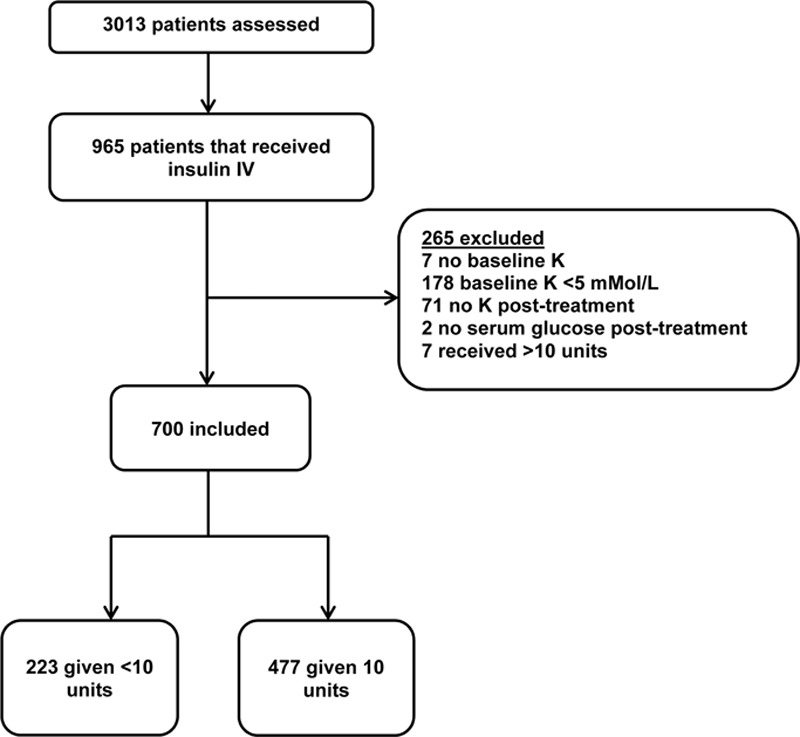
Inclusion and exclusion flow chart. K = serum potassium.
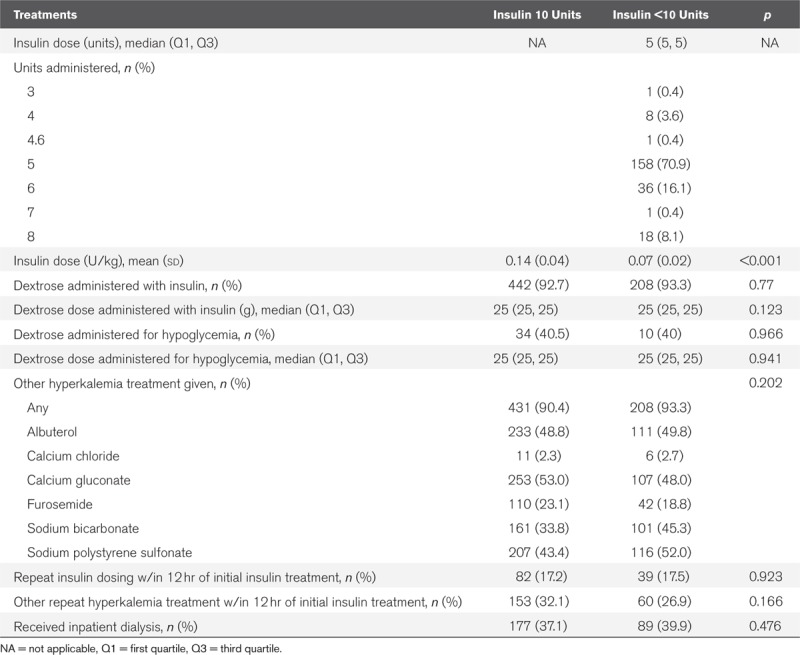
For the primary outcome, patients treated with less than 10 units had significantly lower frequency of hypoglycemia (11.2% vs 17.6%; p = 0.008). However, patients treated with less than 10 units had a significantly smaller reduction in serum potassium post treatment (0.94 ± 0.71 vs 1.11 ± 0.8 mMol/L; p = 0.008) (Fig. 2). There were no other significant differences in safety and efficacy-related outcomes (Table 1). Notably, the range for hypoglycemia onset was 0.78–10.22 hours in patients treated with less than 10 units and 0.8–11.33 hours in patients treated with 10 units. Dextrose requirements, use of concurrent agents for hyperkalemia treatment, and need for repeat insulin dosing were comparable between groups (Table 2).
Figure 2.
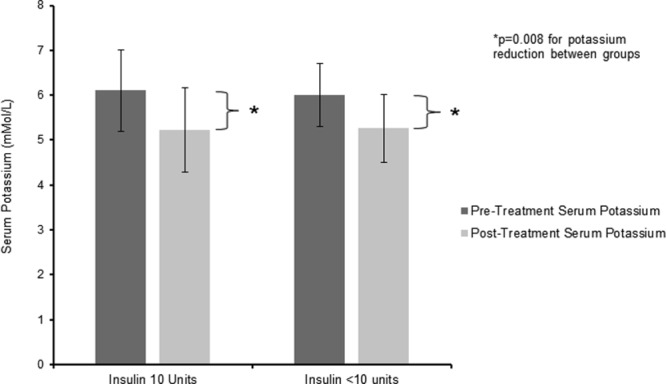
Pre and posttreatment serum potassium levels. Pretreatment levels are reported as medians with interquartile range, and posttreatment levels are reported as means with sd. Reduction in serum potassium was significantly more modest in size in patients treated with less than 10 units (mean reduction 0.94 ± 0.71 mMol/L) compared with patients treated with 10 units (mean reduction 1.11 ± 0.8 mMol/L; p = 0.008).
TABLE 1.
Efficacy and Safety Outcomes

TABLE 2.
Characteristics of Hyperkalemia Treatment
Univariate regression analyses revealed that insulin dose, age, dialysis dependence, diabetes history, and initial serum glucose were significantly associated with hypoglycemia during treatment (Supplemental Table 2, Supplemental Digital Content 2, http://links.lww.com/CCX/A146). A multiple regression model with all factors entered simultaneously revealed that only insulin dose, dialysis dependency, and initial serum glucose were significantly associated with hypoglycemia (Supplemental Table 3, Supplemental Digital Content 3, http://links.lww.com/CCX/A147).
Univariate analyses for effects on serum potassium revealed that insulin dose, sex, weight, dialysis dependence, diabetes history, hyperkalemia severity, and initial serum potassium were significantly associated with serum potassium reduction (Supplemental Table 4, Supplemental Digital Content 4, http://links.lww.com/CCX/A148). A multiple regression model entered all factors simultaneously, and the result was that only weight, dialysis dependence, diabetes history, and initial serum potassium were significantly associated with potassium reduction (Supplemental Table 5, Supplemental Digital Content 5, http://links.lww.com/CCX/A149).
DISCUSSION
Key Findings and Implications
This is the second large single-center study reporting a higher frequency of hypoglycemia with 10 units of regular insulin compared with lower doses. LaRue et al (8) observed that in adults with hyperkalemia, hypoglycemia (<70 mg/dL) occurred in 28.6% of patients receiving 10 units of insulin and in 19.5% of patients receiving 5 units of insulin (difference, –9.1%; 95% CI, –16.8% to –1.3%). Other smaller studies have not observed significant differences in hypoglycemia frequency between patients given 10 units versus lower doses (5 units or 0.1 U/kg) (14–16, 19). However, Garcia et al (15) reported that after multivariate analysis, insulin dose of 5 units significantly reduced risk of hypoglycemia compared with 10 units (odds ratio, 0.307; 95% CI, 0.117–0.806; p = 0.016). We observed that insulin dosing was significantly associated with hypoglycemia after unadjusted, single-predictor, and multiple-predictor analyses. Although we did not detect differences in hospital length of stay or in-hospital mortality between 10 units and less than 10 units groups, hypoglycemia has been associated with increased mortality in other studies (10–13). Our findings reinforce those of LaRue et al (8) and question the safety of traditional insulin dosing recommendations of 10 or more units in patients with acute hyperkalemia (1, 2, 4–6, 8, 20).
In addition to insulin dose, we observed other risk factors for hypoglycemia during hyperkalemia treatment with insulin. Univariate analysis revealed that younger age, dialysis dependence, no diabetes history, and lower pretreatment serum glucose increased the risk of hypoglycemia. Multiple variable analysis revealed that only dialysis dependence and lower initial serum glucose significantly increased the risk. Previous literature has reported that risk factors for hypoglycemia include the following: lower pretreatment glucose, no previous diagnosis of diabetes, kidney dysfunction, lower body weight, and female sex (7, 14, 15, 18). Our findings and those of previous studies suggest that from a safety perspective, providers should consider reduced insulin dosing if any hypoglycemia risk factor is present.
Regardless of selected insulin dosing strategy, providers should ensure patients have adequate hypoglycemia monitoring after insulin administration. We observed that median time to hypoglycemia onset was 1.72 hours (IQR, 1.12–4.13 hr) in patients given less than 10 units and 2.17 hours (IQR, 1.54–3.39 hr) in patients given 10 units. Surprisingly, the range of hypoglycemia onset was 0.78–10.22 hours in those given less than 10 units and 0.8–11.33 hours in those given 10 units. Over 91% of patients in our study had some degree of renal impairment. Previous studies have reported hypoglycemia 6–7.5 hours after insulin administration in patients with renal dysfunction (16, 17). These findings suggest that effects of insulin are prolonged in those with kidney dysfunction. Based on our findings, we propose that all patients given insulin for hyperkalemia be monitored for hypoglycemia hourly for at least 4 hours after administration or longer with increasing severity of renal impairment (e.g. at least 6 hr if dialysis dependent).
In contrast to findings of LaRue et al (8), we observed significant differences in potassium reduction between 10 and less than 10 units groups. Patients treated with less than 10 units had a smaller reduction in potassium versus those given 10 units (0.94 vs 1.11 mMol/L). LaRue et al (8) observed no difference in potassium reduction between those given 5 (1 ± 0.8 mEq/L) and 10 units (1 ± 0.7 mEq/L) of insulin (difference, 0; 95% CI, –0.1 to 0.1 mEq/L). In a post hoc subgroup analysis of patients with baseline serum potassium of 6 mMol/L or greater, Garcia et al (15) noted a smaller potassium reduction in patients given 5 (0.83 mMol/L) versus 10 units (1.08 mMol/L) of insulin (difference = 0.238, 95% CI 0.042–0.434; p = 0.018). In our study, use of concurrent potassium reducing agents, such as albuterol and sodium bicarbonate, was similar between groups. This suggests that difference in concomitant hyperkalemia treatment agents did not account for the difference in potassium reduction between groups and that difference could have been due to reduced potassium lowering properties of insulin doses less than 10 units. However, multivariate analysis revealed that insulin dose was not independently associated with potassium reduction. Additionally, it is unclear if an additional 0.17 mMol/L potassium reduction provided by 10 unit doses would counter the risk of harm due to hypoglycemia. There were also no differences in posttreatment potassium, arrhythmias, need for repeat insulin dosing, or need for repeat other hyperkalemia treatment within 12 hours of initial insulin treatment between groups. This suggests the smaller potassium reduction in those given less than 10 units did not result in harm or provide adequate treatment of hyperkalemia.
Strengths and Limitations
The main limitation of this study is the retrospective design. Erroneous data collection, incomplete data entry, or failure to account for confounders limit this study’s ability to determine causal associations of insulin dosing and outcomes. However, this study was adequately powered and one of the largest studies evaluating insulin dosing in patients with hyperkalemia to date. Second, this study was performed in a single ED at an academic medical center and may not be generalizable to other practice settings. Third, the presence of ED pharmacists could have influenced providers to select 10-unit or less than 10-unit doses and could explain why patients who received less than 10 units had significantly lower pretreatment serum glucose. We did not account for the potential impact of ED pharmacist recommendations in our study, for example, by assessing if insulin orders were approved by an ED pharmacist. However, literature suggesting pretreatment serum glucose increases risk of hypoglycemia after insulin treatment was available prior to our study period (7). Therefore, providers at our study site may have preferred to use lower insulin doses without the influence of ED pharmacists. Fourth, we did not require a specific dose for inclusion in the less than 10-unit group (e.g. 5 units or 0.1 U/kg). This was to include patients receiving weight-based (e.g. 0.1 U/kg) and nonweight-based (e.g. 5 units) dose reduction strategies. Both strategies had been described in literature published during our study period (8, 14–16, 19). The mean insulin dose in the less than 10-unit group was 0.07 U/kg which suggests that future studies may consider evaluating the safety and efficacy of insulin 0.07 U/kg versus standard dosing. Fifth, we only included adult patients that received insulin in the ED, of which over 90% had acute or chronic renal impairment. Our findings may not be applicable to pediatric patients, those receiving insulin outside the ED, or in those without renal impairment. Finally, our study was not powered to detect differences in hospital length of stay or mortality. Larger studies evaluating insulin administration for hyperkalemia may be needed to determine if differences in safety or efficacy influence broader clinical outcomes.
CONCLUSIONS
Patients treated for hyperkalemia with IV insulin doses less than 10 units had reduced frequency of hypoglycemia; however, potassium reduction post treatment was smaller in these patients. Our findings also suggest providers choosing to administer 10 units IV insulin should ensure patients have adequate monitoring for hypoglycemia.
Supplementary Material
Footnotes
This work was performed at Loma Linda University Medical Center, 11234 Anderson Street, Loma Linda, CA 92354.
Supplemental digital content is available for this article. Direct URL citations appear in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
The authors have disclosed that they do not have any conflicts of interest.
REFERENCES
- 1.Weisberg LS. Management of severe hyperkalemia. Crit Care Med. 2008; 36:3246–3251 [DOI] [PubMed] [Google Scholar]
- 2.Long B, Warix JR, Koyfman A. Controversies in management of hyperkalemia. J Emerg Med. 2018; 55:192–205 [DOI] [PubMed] [Google Scholar]
- 3.Allon M, Copkney C. Albuterol and insulin for treatment of hyperkalemia in hemodialysis patients. Kidney Int. 1990; 38:869–872 [DOI] [PubMed] [Google Scholar]
- 4.National Kidney Foundation: Best Practices in Managing Hyperkalemia in Chronic Kidney Disease. Available at: https://www.kidney.org/sites/default/files/02-10-7259_DBH_Best-Practices-in-Managing-Hyperkalemia-in-CKD.pdf. Accessed August 19, 2019
- 5.Mushiyakh Y, Dangaria H, Qavi S, et al. Treatment and pathogenesis of acute hyperkalemia. J Community Hosp Intern Med Perspect. 2012; 1:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Putcha N, Allon M. Management of hyperkalemia in dialysis patients. Semin Dial. 2007; 20:431–439 [DOI] [PubMed] [Google Scholar]
- 7.Schafers S, Naunheim R, Vijayan A, et al. Incidence of hypoglycemia following insulin-based acute stabilization of hyperkalemia treatment. J Hosp Med. 2012; 7:239–242 [DOI] [PubMed] [Google Scholar]
- 8.LaRue HA, Peksa GD, Shah SC. A comparison of insulin doses for the treatment of hyperkalemia in patients with renal insufficiency. Pharmacotherapy. 2017; 37:1516–1522 [DOI] [PubMed] [Google Scholar]
- 9.Scott NL, Klein LR, Cales E, et al. Hypoglycemia as a complication of intravenous insulin to treat hyperkalemia in the emergency department. Am J Emerg Med. 2019; 37:209–213 [DOI] [PubMed] [Google Scholar]
- 10.Fischer KF, Lees JA, Newman JH. Hypoglycemia in hospitalized patients. Causes and outcomes. N Engl J Med. 1986; 315:1245–1250 [DOI] [PubMed] [Google Scholar]
- 11.Glynn N, Owens L, Bennett K, et al. Glucose as a risk predictor in acute medical emergency admissions. Diabetes Res Clin Pract. 2014; 103:119–126 [DOI] [PubMed] [Google Scholar]
- 12.Bruno A, Gregori D, Caropreso A, et al. Normal glucose values are associated with a lower risk of mortality in hospitalized patients. Diabetes Care. 2008; 31:2209–2210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nirantharakumar K, Marshall T, Kennedy A, et al. Hypoglycaemia is associated with increased length of stay and mortality in people with diabetes who are hospitalized. Diabet Med. 2012; 29:e445–e448 [DOI] [PubMed] [Google Scholar]
- 14.Wheeler DT, Schafers SJ, Horwedel TA, et al. Weight-based insulin dosing for acute hyperkalemia results in less hypoglycemia. J Hosp Med. 2016; 11:355–357 [DOI] [PubMed] [Google Scholar]
- 15.Garcia J, Pintens M, Morris A, et al. Reduced versus conventional dose insulin for hyperkalemia treatment. J Pharm Pract. 2018. Sep 6 [DOI] [PubMed] [Google Scholar]
- 16.Pierce DA, Russell G, Pirkle JL., Jr Incidence of hypoglycemia in patients with low egfr treated with insulin and dextrose for hyperkalemia. Ann Pharmacother. 2015; 49:1322–1326 [DOI] [PubMed] [Google Scholar]
- 17.Coca A, Valencia AL, Bustamante J, et al. Hypoglycemia following intravenous insulin plus glucose for hyperkalemia in patients with impaired renal function. PLoS One. 2017; 12:e0172961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Apel J, Reutrakul S, Baldwin D. Hypoglycemia in the treatment of hyperkalemia with insulin in patients with end-stage renal disease. Clin Kidney J. 2014; 7:248–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown K, Jr, Setji TL, Hale SL, et al. Assessing the impact of an order panel utilizing weight-based insulin and standardized monitoring of blood glucose for patients with hyperkalemia. Am J Med Qual. 2018; 33:598–603 [DOI] [PubMed] [Google Scholar]
- 20.Elliott MJ, Ronksley PE, Clase CM, et al. Management of patients with acute hyperkalemia. CMAJ. 2010; 182:1631–1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


