Abstract
A dynamic evolution is occurring in transanal surgery. Transanal techniques began with intraluminal surgical removal of rectal masses and have progressed to transanal total mesorectal excision (taTME) for rectal cancer. TaTME was first performed in 2009 by Sylla, Rattner, Delgado, and Lacy. This article documents the training pathway followed by pioneers in the taTME technique as well as consensus reports outlining the process of learning the taTME technique. A literature search was performed for taTME training, learning, and technique. Key elements in learning the taTME technique include appropriate indications, cadaver training, and outcomes reporting such as participating in a taTME registry. Consensus reports also agree on the following facets associated with improved outcomes: (1) appropriate case selection of mid and low rectal cancers, (2) prerequisite completion of an accredited training program in laparoscopic colorectal surgery and prior experience in transanal endoscopic surgery, (3) a two-team taTME approach from above and below is ideal, and (4) higher rectal cancer volume surgical practice. The unifying international recommendation for surgeons interested in learning the taTME technique conveys the following message: taTME is an advanced and complex technique that requires dedicated training and experience in TME surgery.
Keywords: taTME, transanal, total mesorectal excision, rectal cancer, training
The surgical technique associated with the highest rate of cure and lowest rate of rectal cancer recurrence is called “total mesorectal excision (TME).” 1 The execution of TME using a minimally invasive abdominal surgical approach (laparoscopic, robotic) is a technically challenging operation with reduced working space, retraction capabilities, and visibility. Initially, there was a slow adoption rate of this technique with less than 10% minimally invasive surgical procedures being performed for rectal cancer in the United States by 2011. 2 These challenges led to the trend toward increased interest and utilization of robotic rectal surgery. However, even with robotic visualization and instrumentation, there remain several technical hurdles in the minimally invasive approach to rectal cancer. Most notably, the division of the distal rectum remains technically challenging due to the limitations of the pelvic working space and articulation of modern stapler technology.
The standard approach for both minimally invasive and open TME for rectal cancer is performed using the abdomen to access the rectum located deep in the pelvis. Alternatively, TME can be performed through the anus, a natural portal to access and perform the TME pelvic dissection. Transanal access for performing TME has many potential advantages compared with the transabdominal surgical approach: (1) a transanal approach utilizes pneumatic pressure to assist with the dissection through the avascular embryologic tissue plane surrounding the rectum. This pneumatic pressure dissection does not occur when using a transabdominal approach to rectal surgery. (2) The retraction of the rectum is technically less difficult from the transanal approach as rectal retraction is a “forward pushing motion” for transanal rectal surgery compared with a “pulling up and out of the pelvis motion” required for transabdominal rectal surgery. (3) Rectal division can be performed without using modern endoscopic staplers when performing a transanal approach. This maneuver allows the surgeon to more precisely select the distal margin transection site and perform the transection in a linear fashion and under direct visualization. (4) The low pelvic anastomosis can be performed using a double circular stapler technique or hand-sewn technique, thereby avoiding the multiple staple line and staple crossover lines when creating a low pelvic anastomosis that may be associated with an increased rate of anastomotic leak.
The combined transabdominal–transanal (TATA) approach for the surgical management of low lying rectal cancers was initially described by Dr. Gerald Marks and colleagues 3 4 in 1984 as an alternative to abdominal perineal resection with permanent end colostomy in patients with cancers in the distal third of the rectum. 3 4 A total of 79 patients underwent laparoscopic TATA resection for locally advanced low lying rectal cancer located within 3 cm or less of the anorectal ring. There was no perioperative mortality. The conversion rate was very low (2.5%), as was the local recurrence rate (2.5%). All patients underwent a temporary diverting ileostomy at the time of the laparoscopic TATA procedure. After completion of systemic chemotherapy, 90% of the patients were able to undergo ileostomy reversal. 4
With increasing interest in natural orifice surgical access, there has been an increased interest in the evolution of transanal natural orifice and endoluminal surgical techniques. These techniques began with transanal intraluminal surgical removal of rectal masses 5 6 7 8 9 10 11 and have progressed to transanal endoscopic surgical resection of the rectum without abdominal laparoscopic assistance. 12 13 14 Investigative activity has escalated in the evaluation of proctectomy via a completely transanal approach. 15 The feasibility and safety of transanal proctectomy and transanal rectosigmoid resection has been demonstrated in human cadavers and porcine survival models using a variety of transanal access platforms. 16 17 18 19 20 21 22 23 24
The largest cadaveric series investigating transanal rectosigmoid resection for rectal cancer via natural orifice transluminal endoscopic surgery (NOTES) with TME using a rigid transanal endoscopic platform in 32 cadavers was published by Telem et al in 2013. 25 The mean operative time was 5.1 hours, and the mean specimen length of 53 cm. Transanal dissection alone using the TEM platform was performed in 19 cases (17 cases with the use of a gastroscope). Intra-abdominal assistance was performed using multiport laparoscopy in eight cases and transgastric endoscopic assistance in five cases. The mesorectum was intact in all of the specimens. 18 25 26 27 28 29 30 31 32 33 34
The first clinical case utilizing a rigid transanal endoscopic platform to perform a transanal TME (taTME) with laparoscopic assistance in a 76-year-old woman with uT2N2M0 stage III rectal cancer was safely executed by Sylla et al in 2009 and published in 2010. 35 The outcome of this case demonstrated patient safety, accelerated recovery, and equivalent short-term oncologic outcomes. After more than 5 years of survivorship screening and surveillance, the patient is doing well and has not demonstrated any evidence of locally recurrent or metastatic disease.
Methods
A literature search was performed using PubMed.gov and the following keywords: taTME, cadaver training, rectal cancer, TME, total mesorectal excision, transanal, and natural orifice surgery. Published manuscripts outlining a training pathway, model, platform, and/or curriculum were included in the review. This manuscript outlines the training pathway followed by pioneers in the taTME technique and consensus reports outlining the process of learning the taTME technique. The reported training pathways, training courses, and consensus statements are summarized in the next sections.
Results
There are seven elements consistently highlighted throughout the published manuscripts to date reviewing the process of learning taTME ( Fig. 1 ): (1) accredited training and expertise in TME for rectal cancer, (2) expertise in minimally invasive (laparoscopic and/or robotic) TME from the abdominal approach, (3) expertise in transanal endoscopic surgery, (4) experience in intersphincteric dissection for very low rectal invasive neoplasms, (5) practice in taTME techniques in human cadaver models and modular training, (6) proctorship and ongoing mentorship, and (7) institutional review board approved data collection with publication of outcomes and/or participation in a clinical registry. 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50
Fig. 1.
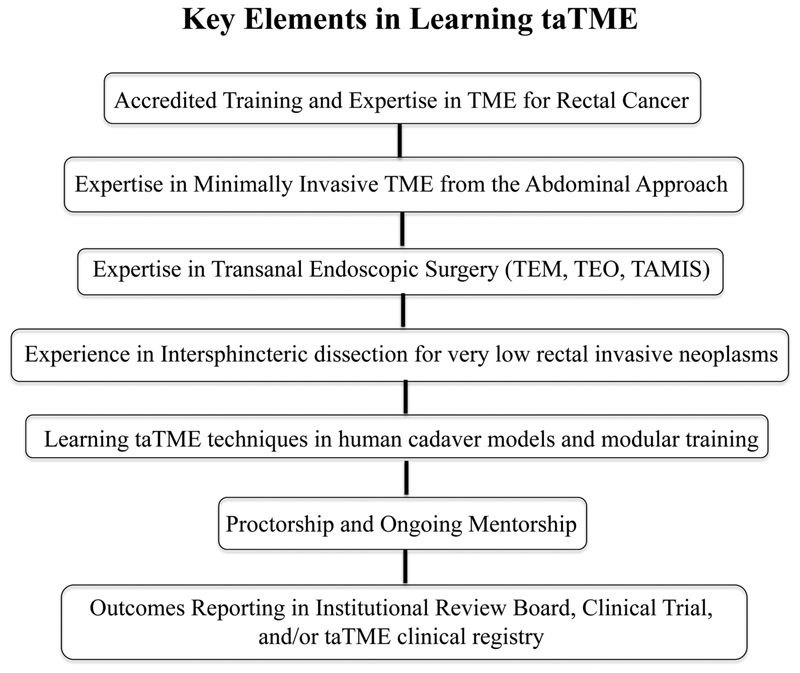
Seven elements consistently highlighted throughout the published manuscripts to date reviewing the process of learning transanal total mesorectal excision (taTME). TEO, transanal endoscopic operation; TAMIS, transanal minimally invasive surgery.
First Author's taTME Learning Experience
After a few years of experience with laparoscopic and robotic TME for rectal cancer including intersphincteric dissection, the senior author trained in transanal endoscopic microsurgery (TEM) and transanal minimally invasive surgery (TAMIS). 30 31 32 33 Thereafter, following in the pathway of pioneers in the taTME technique, the two team surgical group underwent cadaver training in taTME in 2012. A grade I TME dissection quality was achieved in all eight male cadaver models, of which the results of the first five were published in 2013 34 followed by initial experience with taTME. 36 This pathway has been followed by numerous pioneers in the taTME technique. To date, all published consensus statements and collaborative group reports reviewing taTME training and education have continued to highlight and emphasize these vital steps in learning the taTME technique.
TaTME Cadaver Models and Curricula
TaTME pioneers and educators Penna, Whiteford, Hompes, and Sylla reported the outcomes after conducting four taTME cadaveric workshops in the U.S. and U.K. from 2013 to 2016. 40 A total of 52 surgeons with previous surgical experience in laparoscopic TME and transanal endoscopic surgery but limited taTME exposure performed 47 taTME cases in fresh human cadaveric models. The distal rectal purse-string remained occluded throughout the taTME dissection in 93% of U.K. and 60% of U.S. cases. Nearly all (96%) of the trainees dissected transanally to a level of S2 or above with a mean time of 80 minutes (range: 25–155) from the start of the circumferential dissection to peritoneal entry. Other operative timings for key procedural steps were similar between the two countries. The quality of the TME specimen was complete or near-complete in 81% of taTME cadaver specimens. Eighty-one percent of taTME trainees surveyed reported currently performing taTME in their clinical practice. The educators concluded that human cadaveric models provide excellent training for complex pelvic surgery such as taTME. “A structured training curriculum including reading material, dry-lab purse-string practice, and postcourse mentorship will provide surgeons with a more complete training package and ongoing support to ultimately ensure the safe introduction of taTME in the clinical setting.” 40
Wynn et al reported the outcomes of surgeons attending taTME cadaveric simulation courses as well. 41 The outcomes of 65 trainees from 12 different countries who attended 7 cadaveric simulation taTME courses revealed similar results. Maintaining distal rectal purse-string closure was the most common reported difficulty. The median time of taTME dissection was 105 (range: 60–260) minutes. The taTME specimen quality was complete or near-complete in 89% of specimens. Within 6 months after attending the taTME cadaver training course, 47% of the responding trainees were performing taTME in their clinical practice (26 out of 55 reporting surgeons). Only 8 out of these 26 surgeons had arranged mentoring for their first case. The group concluded that the human cadaveric model provides a significant level of satisfaction and information transfer in learning the technical skills necessary to start performing taTME. However, “there is still work to do to provide adequate supervision and mentorship for surgeons early on their learning curve that is essential for the safe introduction of this new technique.” 41
An Australasian (Australia and New Zealand) taTME learning pathway for the introduction of taTME has been implemented for surgeons with specialist training and baseline technical ability initiated among colon and rectal surgeons. 42 The training pathway includes an intensive training “course, a series of proctored cases, and ongoing contribution to audit.” 42 A total of 133 taTME procedures were performed following the implementation of the training program, of which 84% of cases were performed for rectal cancer. The quality of the mesorectal excision was complete or nearly complete in 98% of cases. The distal resection margin was negative in all cases. The circumferential radial margin was positive in two cases. The incidence of postoperative morbidity was 27% and there were no mortalities. The authors concluded that the taTME surgical technique can safely be introduced in a defined surgeon population in a controlled fashion using a taTME training, proctoring, and audit pathway. 42
The stepwise learning curve for participants was reported as “clearly observed” during a 2-day training course. 43 The first day consisted of supervised simulator training and taTME exercises at three cadaver workstations. Participants trained in the milestones of the taTME approach on cadavers such as distal purse-string closure and key components of the lateral, posterior, and anterior dissection pitfalls and visual cues for incorrect and correct plane identification. On the second day, participants were able to observe two live taTME cases. Participants were encouraged to report their cases in registries or registered clinical trials. 43
Application-based technology is also available for taTME modular training. 44 The iLappSurgery Foundation launched the taTME app in June of 2016. This application-based form of learning offers portable education and instant access to information regarding the taTME dissection anatomy and technique. The application has achieved a large user-base since its debut and provides useful information, videos, and diagrams for surgeons interested in mastery of the taTME technique. 44
TaTME Consensus and Collaborative Reports
The International taTME Educational Collaborative Group surveyed 207 surgeons from 18 different countries including taTME learners and 52 international experts in the field of taTME. 45 The survey results were reviewed and a final expert's consensus was published on the essential elements of a training curriculum. For patients with rectal cancers, appropriate case selection of mid and low rectal cancers, but not proximal rectal cancers, is strongly recommended. Prerequisites deemed necessary prior to learning taTME include completion of an accredited training program in laparoscopic colorectal surgery and prior experience in transanal endoscopic surgery such as TEM, transanal endoscopic operation, and TAMIS. 45
An additional publication by the International taTME Educational Collaborative Group continued to outline three key facets of taTME included technique and indications, training and adoption, and data collection in a taTME registry. 45 46 A two-team taTME approach from above and below is ideal as well as surgical practice location in an area with higher rectal cancer volume. A systematic review of published taTME outcomes confirmed higher volume surgeons (> 30 cases) were associated with higher TME quality compared with lower volume surgeons (complete TME 90% high volume vs. 81% low volume). 47 Team training of the two surgeons together is also highly recommended, as is mentorship and multidisciplinary training. 46 47 A taTME training curriculum should include progressive training modules, topographical education, as well as simulated training experience for purse-string suturing for rectal closure and creation of the anastomosis. Ongoing report of outcomes in the form of audit, proctoring, and/or participation in a registry 48 were also strong recommendations to ensure high quality of the TME specimen, perioperative morbidity, and functional outcomes. The framework for a structured taTME training program and curriculum is detailed in the publication as well. 46 47
The St.Gallen 49 multidisciplinary consensus statement on safe implementation of taTME reviewed severe elements of taTME implementation for early adopters. The group resolved seven key elements of taTME implementation: patient selection and indication, perioperative management, patient positioning and operating room set up, surgical technique, devices and instruments, pelvic anatomy, taTME training, and outcomes analysis. 49
Conclusion
The unifying international recommendation for surgeons interested in taTME is “taTME is an advanced and complex technique that requires dedicated training and experience in TME surgery.” 50 TaTME is an attractive alternative to other minimally invasive TME techniques as the number of abdominal access ports is reduced, the abdominal extraction incision can be avoided in many cases, and the technical difficulty of performing the TME is reduced. Antonio Lacy has the largest experience with taTME for rectal cancer, and has published the outcomes of the first 140 taTME cases for rectal cancer. 34 Compared with Lacy's laparoscopic experience, the taTME technique is associated with a lower conversion rate (0 vs. 20%) and shorter TME mean operative times (154 vs. 179 minutes). 35 The rate of ileus (4.1%, 1.3%), anastomotic leakage (8.2%, 7.3%), pelvic fluid collection (4.1%, 1.3%), and urinary retention (1.8%, 2.7%) were similar after taTME and laparoscopic TME, respectively.
The implementation of the taTME technique into clinical practice can be safely and effectively achieved by surgeons with expertise in the management of rectal cancer, minimally invasive TME, and transanal endoscopic surgery. Surgeons interested in learning the taTME technique should have a higher volume of experience with TME for rectal cancer in their surgical practice, expertise in achieving negative circumferential radial margins and high quality (complete) TME grade specimens after a minimally invasive approach to TME, as well as mastery of transanal endoscopic surgery. Given the relatively recent introduction of taTME and the paucity of long-term oncologic and functional outcomes, we eagerly await the results of prospective comparative trials. The key elements that should be acknowledged and emphasized in the process of learning taTME including preclinical taTME cadaver training, case observation, proctoring, ongoing mentorship, participation in a clinical registry and/or clinical, and ongoing peer review and publication of their outcomes after performing taTME.
Conflict of Interest None declared.
Disclosures
Dr. McLemore, Dr. Lavi, and Dr. Attaluri have no financial disclosures to report.
References
- 1.Heald R J. The ‘Holy Plane’ of rectal surgery. J R Soc Med. 1988;81(09):503–508. doi: 10.1177/014107688808100904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rea J D, Cone M M, Diggs B S, Deveney K E, Lu K C, Herzig D O. Utilization of laparoscopic colectomy in the United States before and after the clinical outcomes of surgical therapy study group trial. Ann Surg. 2011;254(02):281–288. doi: 10.1097/SLA.0b013e3182251aa3. [DOI] [PubMed] [Google Scholar]
- 3.Marks G J, Marks J H, Mohiuddin M, Brady L. Radical Sphincter preservation surgery with coloanal anastomosis following high-dose external irradiation for the very low lying rectal cancer. Recent Results Cancer Res. 1998;146:161–174. doi: 10.1007/978-3-642-71967-7_15. [DOI] [PubMed] [Google Scholar]
- 4.Marks J, Mizrahi B, Dalane S, Nweze I, Marks G. Laparoscopic transanal abdominal transanal resection with sphincter preservation for rectal cancer in the distal 3 cm of the rectum after neoadjuvant therapy. Surg Endosc. 2010;24(11):2700–2707. doi: 10.1007/s00464-010-1028-8. [DOI] [PubMed] [Google Scholar]
- 5.Buess G, Theiss R, Hutterer F et al. Die transanale endoskopische Rektumoperation - Erprobung einer neuen Methode im Tierversuch. Leber Magen Darm. 1983;13(02):73–77. [PubMed] [Google Scholar]
- 6.Buess G. Review: transanal endoscopic microsurgery (TEM) J R Coll Surg Edinb. 1993;38(04):239–245. [PubMed] [Google Scholar]
- 7.Middleton P F, Sutherland L M, Maddern G J. Transanal endoscopic microsurgery: a systematic review. Dis Colon Rectum. 2005;48(02):270–284. doi: 10.1007/s10350-004-0804-8. [DOI] [PubMed] [Google Scholar]
- 8.Moore J S, Cataldo P A, Osler T, Hyman N H.Transanal endoscopic microsurgery is more effective than traditional transanal excision for resection of rectal masses Dis Colon Rectum 200851071026–1030., discussion 1030–1031 [DOI] [PubMed] [Google Scholar]
- 9.Barendse R M, van den Broek F J, Dekker E et al. Systematic review of endoscopic mucosal resection versus transanal endoscopic microsurgery for large rectal adenomas. Endoscopy. 2011;43(11):941–949. doi: 10.1055/s-0030-1256765. [DOI] [PubMed] [Google Scholar]
- 10.Allaix M E, Arezzo A, Caldart M, Festa F, Morino M. Transanal endoscopic microsurgery for rectal neoplasms: experience of 300 consecutive cases. Dis Colon Rectum. 2009;52(11):1831–1836. doi: 10.1007/DCR.0b013e3181b14d2d. [DOI] [PubMed] [Google Scholar]
- 11.Guerrieri M, Baldarelli M, de Sanctis A, Campagnacci R, Rimini M, Lezoche E. Treatment of rectal adenomas by transanal endoscopic microsurgery: 15 years' experience. Surg Endosc. 2010;24(02):445–449. doi: 10.1007/s00464-009-0585-1. [DOI] [PubMed] [Google Scholar]
- 12.Lacy A M, Adelsdorfer C. Totally transrectal endoscopic total mesorectal excision (TME) Colorectal Dis. 2011;13 07:43–46. doi: 10.1111/j.1463-1318.2011.02781.x. [DOI] [PubMed] [Google Scholar]
- 13.Gaujoux S, Bretagnol F, Au J, Ferron M, Panis Y. Single port access proctectomy with total mesorectal excision and intersphincteric resection with a primary transanal approach. Colorectal Dis. 2011;13(09):e305–e307. doi: 10.1111/j.1463-1318.2011.02676.x. [DOI] [PubMed] [Google Scholar]
- 14.Zhang H, Zhang Y S, Jin X W, Li M Z, Fan J S, Yang Z H. Transanal single-port laparoscopic total mesorectal excision in the treatment of rectal cancer. Tech Coloproctol. 2013;17(01):117–123. doi: 10.1007/s10151-012-0882-x. [DOI] [PubMed] [Google Scholar]
- 15.Sylla P. Current experience and future directions of completely NOTES colorectal resection. World J Gastrointest Surg. 2010;2(06):193–198. doi: 10.4240/wjgs.v2.i6.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whiteford M H, Denk P M, Swanström L L. Feasibility of radical sigmoid colectomy performed as natural orifice translumenal endoscopic surgery (NOTES) using transanal endoscopic microsurgery. Surg Endosc. 2007;21(10):1870–1874. doi: 10.1007/s00464-007-9552-x. [DOI] [PubMed] [Google Scholar]
- 17.Denk P M, Swanström L L, Whiteford M H. Transanal endoscopic microsurgical platform for natural orifice surgery. Gastrointest Endosc. 2008;68(05):954–959. doi: 10.1016/j.gie.2008.03.1115. [DOI] [PubMed] [Google Scholar]
- 18.Fajardo A D, Hunt S R, Fleshman J W, Mutch M G. Video. Transanal single-port low anterior resection in a cadaver model. Surg Endosc. 2010;24(07):1765. doi: 10.1007/s00464-009-0838-z. [DOI] [PubMed] [Google Scholar]
- 19.Trunzo J A, Delaney C P. Natural orifice proctectomy using a transanal endoscopic microsurgical technique in a porcine model. Surg Innov. 2010;17(01):48–52. doi: 10.1177/1553350609359516. [DOI] [PubMed] [Google Scholar]
- 20.Sylla P, Sohn D K, Cizginer S et al. Survival study of natural orifice translumenal endoscopic surgery for rectosigmoid resection using transanal endoscopic microsurgery with or without transgastric endoscopic assistance in a swine model. Surg Endosc. 2010;24(08):2022–2030. doi: 10.1007/s00464-010-0898-0. [DOI] [PubMed] [Google Scholar]
- 21.Sylla P, Willingham F F, Sohn D K, Gee D, Brugge W R, Rattner D W. NOTES rectosigmoid resection using transanal endoscopic microsurgery (TEM) with transgastric endoscopic assistance: a pilot study in swine. J Gastrointest Surg. 2008;12(10):1717–1723. doi: 10.1007/s11605-008-0637-1. [DOI] [PubMed] [Google Scholar]
- 22.Han Y, He Y G, Zhang H B et al. Total laparoscopic sigmoid and rectal surgery in combination with transanal endoscopic microsurgery: a preliminary evaluation in China. Surg Endosc. 2013;27(02):518–524. doi: 10.1007/s00464-012-2471-5. [DOI] [PubMed] [Google Scholar]
- 23.Bhattacharjee H K, Kirschniak A, Storz P, Wilhelm P, Kunert W. Transanal endoscopic microsurgery-based transanal access for colorectal surgery: experience on human cadavers. J Laparoendosc Adv Surg Tech A. 2011;21(09):835–840. doi: 10.1089/lap.2011.0045. [DOI] [PubMed] [Google Scholar]
- 24.Sohn D K, Jeong S Y, Park J W et al. Comparative study of NOTES rectosigmoidectomy in a swine model: E-NOTES vs. P-NOTES. Endoscopy. 2011;43(06):526–532. doi: 10.1055/s-0030-1256239. [DOI] [PubMed] [Google Scholar]
- 25.Telem D A, Han K S, Kim M C et al. Transanal rectosigmoid resection via natural orifice translumenal endoscopic surgery (NOTES) with total mesorectal excision in a large human cadaver series. Surg Endosc. 2013;27(01):74–80. doi: 10.1007/s00464-012-2409-y. [DOI] [PubMed] [Google Scholar]
- 26.Atallah S, Albert M, Larach S. Transanal minimally invasive surgery: a giant leap forward. Surg Endosc. 2010;24(09):2200–2205. doi: 10.1007/s00464-010-0927-z. [DOI] [PubMed] [Google Scholar]
- 27.Cid R C, Pérez J C, Elosua T G et al. Transanal resection using a single port trocar: a new approach to NOTES [in Spanish] Cir Esp. 2011;89(01):20–23. doi: 10.1016/j.ciresp.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 28.Dumont F, Goéré D, Honoré C, Elias D. Transanal endoscopic total mesorectal excision combined with single-port laparoscopy. Dis Colon Rectum. 2012;55(09):996–1001. doi: 10.1097/DCR.0b013e318260d3a0. [DOI] [PubMed] [Google Scholar]
- 29.McLemore E C, Coker A, Jacobsen G, Talamini M A, Horgan S. eTAMIS: endoscopic visualization for transanal minimally invasive surgery. Surg Endosc. 2013;27(05):1842–1845. doi: 10.1007/s00464-012-2652-2. [DOI] [PubMed] [Google Scholar]
- 30.McLemore E C, Coker A, Leland H et al. New disposable transanal endoscopic surgery platform: longer channel, longer reach. Global J Gastroenterol Hepatol. 2013;1:46–50. [Google Scholar]
- 31.McLemore E C, Weston L A, Coker A M et al. Transanal minimally invasive surgery for benign and malignant rectal neoplasia. Am J Surg. 2014;208(03):372–381. doi: 10.1016/j.amjsurg.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 32.McLemore E C, Leland H, Devaraj B et al. Transanal endoscopic surgical proctectomy for proctitis case series report: diversion, radiation, ulcerative colitis, and Crohn's disease. Global J Gastroenterol Hepatol. 2013;1:41–47. [Google Scholar]
- 33.McLemore E C, Coker A M, Devaraj B et al. TAMIS-assisted laparoscopic low anterior resection with total mesorectal excision in a cadaveric series. Surg Endosc. 2013;27(09):3478–3484. doi: 10.1007/s00464-013-2889-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lacy A M, Tasende M M, Delgado S et al. Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg. 2015;221(02):415–423. doi: 10.1016/j.jamcollsurg.2015.03.046. [DOI] [PubMed] [Google Scholar]
- 35.Sylla P, Rattner D W, Delgado S, Lacy A M. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc. 2010;24(05):1205–1210. doi: 10.1007/s00464-010-0965-6. [DOI] [PubMed] [Google Scholar]
- 36.McLemore E C, Harnsberger C R, Broderick R C et al. Transanal total mesorectal excision (taTME) for rectal cancer: a training pathway. Surg Endosc. 2016;30(09):4130–4135. doi: 10.1007/s00464-015-4680-1. [DOI] [PubMed] [Google Scholar]
- 37.Hohenberger W, Merkel S, Hermanek P. Volume and outcome in rectal cancer surgery: the importance of quality management. Int J Colorectal Dis. 2013;28(02):197–206. doi: 10.1007/s00384-012-1596-2. [DOI] [PubMed] [Google Scholar]
- 38.Wexner S D, Rotholtz N A. Surgeon influenced variables in resectional rectal cancer surgery. Dis Colon Rectum. 2000;43(11):1606–1627. doi: 10.1007/BF02236751. [DOI] [PubMed] [Google Scholar]
- 39.Hompes R, Arnold S, Warusavitarne J. Towards the safe introduction of transanal total mesorectal excision: the role of a clinical registry. Colorectal Dis. 2014;16(07):498–501. doi: 10.1111/codi.12661. [DOI] [PubMed] [Google Scholar]
- 40.Penna M, Whiteford M, Hompes R, Sylla P. Developing and assessing a cadaveric training model for transanal total mesorectal excision: initial experience in the UK and USA. Colorectal Dis. 2017;19(05):476–484. doi: 10.1111/codi.13525. [DOI] [PubMed] [Google Scholar]
- 41.Wynn G R, Austin R CT, Motson R WU. Using cadaveric simulation to introduce the concept and skills required to start performing transanal total mesorectal excision. Colorectal Dis. 2018;20(06):496–501. doi: 10.1111/codi.14034. [DOI] [PubMed] [Google Scholar]
- 42.Abbott S C, Stevenson A RL, Bell S W et al. An assessment of an Australasian pathway for the introduction of transanal total mesorectal excision (taTME) Colorectal Dis. 2018;20(01):O1–O6. doi: 10.1111/codi.13964. [DOI] [PubMed] [Google Scholar]
- 43.Aigner F, Biebl M, Fürst A, Jöns T, Pratschke J, Kneist W. Training course transanal total mesorectal excision (TaTME): concept and establishment of a training course for safe application [in German] Chirurg. 2017;88(02):147–154. doi: 10.1007/s00104-016-0295-x. [DOI] [PubMed] [Google Scholar]
- 44.Atallah S, Brady R R. The iLappSurgery taTME app: a modern adjunct to the teaching of surgical techniques. Tech Coloproctol. 2016;20(09):665–666. doi: 10.1007/s10151-016-1509-4. [DOI] [PubMed] [Google Scholar]
- 45.Motson R W, Whiteford M H, Hompes R, Albert M, Miles W F; Expert Group.Current status of trans-anal total mesorectal excision (TaTME) following the Second International Consensus Conference Colorectal Dis 2016180113–18. [DOI] [PubMed] [Google Scholar]
- 46.Francis N, Penna M, Mackenzie H, Carter F, Hompes R; International TaTME Educational Collaborative Group.Consensus on structured training curriculum for transanal total mesorectal excision (TaTME) Surg Endosc 201731072711–2719. [DOI] [PubMed] [Google Scholar]
- 47.Deijen C L, Tsai A, Koedam T W et al. Clinical outcomes and case volume effect of transanal total mesorectal excision for rectal cancer: a systematic review. Tech Coloproctol. 2016;20(12):811–824. doi: 10.1007/s10151-016-1545-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Penna M, Hompes R, Arnold S et al. Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg. 2017;266(01):111–117. doi: 10.1097/SLA.0000000000001948. [DOI] [PubMed] [Google Scholar]
- 49.Adamina M, Buchs N C, Penna M, Hompes R; St.Gallen Colorectal Consensus Expert Group.St.Gallen consensus on safe implementation of transanal total mesorectal excision Surg Endosc 201832031091–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Penna M, Cunningham C, Hompes R. Transanal total mesorectal excision: why, when, and how. Clin Colon Rectal Surg. 2017;30(05):339–345. doi: 10.1055/s-0037-1606111. [DOI] [PMC free article] [PubMed] [Google Scholar]


