Abstract
Objectives:
Self-reported activity restriction is an established correlate of depression in dementia caregivers (dCGs). It is plausible that the daily distribution of objectively-measured activity is also altered in dCGs with depression symptoms; if so, such activity characteristics could provide a passively measurable marker of depression or specific times to target preventive interventions. We therefore investigated how levels of activity throughout the day differed in dCGs with and without depression symptoms, then tested whether any such differences predicted changes in symptoms 6-months later.
Design, setting, participants, and measurements:
We examined 56 dCGs (mean age=71, standard deviation (SD)=6.7; 68% female) and used clustering to identify subgroups who had distinct depression symptom levels, leveraging baseline Center for Epidemiologic Studies of Depression Scale–Revised Edition (CESD-R) and Patient Health Questionnaire–9 (PHQ-9) measures, as well as a PHQ-9 score from six months later. Using wrist activity (mean recording length=12.9 days, minimum=6 days), we calculated average hourly activity levels, then assessed when activity levels relate to depression symptoms and changes in symptoms 6 months later.
Results:
Clustering identified sub-groups characterized by: (1) no/minimal symptoms (36%); and (2) depression symptoms (64%). After multiple comparison correction, the group of dCG’s with depression symptoms were less active from 8–10 AM (Cohen’s d’s≤−0.9). These morning activity levels predicted the degree of symptom change on the PHQ-9 6 months later (per SD unit β=−.8, 95% confidence interval: −1.6, −0.1, p=0.03) independent of self-reported activity restriction and other key factors.
Conclusions:
These novel findings suggest that morning activity may protect dCGs from depression symptoms. Future studies should test whether helping dCGs get active in the morning addresses the other features of depression in this population (i.e., insomnia, intrusive thoughts, and perceived activity restriction).
Keywords: dementia caregiving, depression symptoms, sleep, activity restriction, physical activity
There are approximately 6.7 million family caregivers for people with dementia in the United States alone (Wolff et al., 2016). About 1.5 million of these dementia caregivers (dCGs) – over 20% – suffer from a depressive disorder (Cuijpers, 2005). Depression not only reduces the quality of daily lives, it is also associated with lower quality of caregiving (Smith et al., 2011). Preventing depression in dCGs is therefore a high priority. Major depressive episodes often do not “come out of the blue;” instead, the presence of some depressive symptoms predicts the development of more symptoms (Joling et al., 2012) and major depressive disorder (Cuijpers and Smit, 2004). The modifiable characteristics associated with subsyndromal depressive symptoms in dCGs may therefore reflect the mechanisms of depression pathogenesis and logical targets for preventive interventions.
One important and potentially modifiable contributor to depression symptoms in dCGs is activity restriction (Mausbach et al., 2011). Past research defines activity restriction as self-reports of reductions in the ability to engage in self-care and recreational activities due to the caregiving role. Given the strong relationship between the perception of activity restriction and depression in dCGs, it is plausible that differences in objectively-measurable daily activity patterns also co-travel with depression in this group. Unlike self-reported activity restriction, objective activity measures related to depression cannot be due to confounding by negative affective or recall bias. Furthermore, activity patterns can be passively measured using wearable accelerometer devices. As such, evidence for depressogenic effects of particular activity patterns could lead to clinical applications, e.g., wearable actigraphy could be used to help stratify depression risk; and preventive interventions could be delivered to alter activity during key times. However, little evidence currently exists regarding which objectively-measured activity patterns characterize depression symptoms in dCGs.
Our past study found that differences in dCGs’ daily distribution of activity correlated with subsyndromal depression severity (Smagula et al., 2017). This past work found that dCGs with more depression symptoms tended to have slower transitions between resting and active states, narrower periods of activity, and more activity during sleep. However, because these findings were based on cross-sectional data, it remains unknown whether differences in the daily distribution of activity also predict the changes in depression symptoms over time (i.e., rather than being an element or result of having depression symptoms). We therefore evaluated whether objectively-measurable differences in daily activity patterns were related to subsyndromal depression symptoms and changes in symptoms over six-months in dCGs.
Methods
Sample
Participants were initially contacted through outreach to local support groups and by accessing three registries (the University of Pittsburgh Alzheimer Disease Research Center; the Pittsburgh Regional Caregiver Survey; and the University of Pittsburgh Clinical and Translational Science Institute “Pitt+Me” registry). To be included, caregivers were required to: be at least 60 years of age; provide unpaid care to someone with dementia; have experienced stress or strain, either physical or emotional, related to caregiving; live with their care recipient or provide at least 15 hours of care per week; have PHQ-9 scores less than 10 (consistent with the aim of studying subsyndromal symptoms and increases over time); and be able to undergo magnetic resonance imaging (administered for an aim of the project that is not addressed in this report). Of the 239 potential participants screened, 86 were eligible, and 66% of these eligible dCGs agreed to participate. This yielded a sample of 57 participants, of whom 56 provided adequate actigraphy data (defined below) and were included in the analysis.
Measures
Objective activity pattern:
Participants wore a Philips Spectrum Plus (Philips Respironics, Bend, OR, USA) actigraphy device on their non-dominant wrist for 14 days. Data were considered adequate if at least three days of valid wear were confirmed. Consistent with National Sleep Research Resource data processing standards (see (Dean et al., 2016) and associated website), valid days were defined as those that did not include periods of more than 4 hours of offwrist/invalid time or off wrist/invalid times during the main sleep period. Only one participant did not have adequate actigraphy data, and participants were highly compliant with the actigraphy protocol (mean recording length=12.9 days, median=14 days, range=6–15 days).
Our previous publication using cosine-based analysis methods found that differences in the distribution of activity through 24-hour periods related to depression symptoms (Smagula et al., 2017). To delineate which temporal patterns of activity relate to depression symptoms in dCGs, we defined the primary exposure variables in the current work as the average levels of actigraphy-defined activity level for each hour of the day. This set of objective measures can be passively assessed, thereby enabling potential applications tracking risk markers in interventions without active input from dCGs.
Covariates:
We included several other sleep-wake measures that are plausibly related to depression in dCGs, including: circadian preference measured with the Morningness-Eveningness Scale (Smith et al., 1989); insomnia symptom severity measured using the Insomnia Severity Index (Bastien et al., 2001); actigraphy-assessed sleep fragmentation (measured as the number of minutes awake after sleep onset, manually setting sleep intervals based on sleep diary data and then using an automated scoring system); and the Epworth Sleepiness Scale (Johns, 1991). We interviewed participants using a standardized questionnaire which asked: if they live with their care recipient; how many caregiving activities (from a list of 13 activities and instrumental activities of daily living) they provided care for; how many years they had been in the caregiving role; and the Cumulative Illness Rating Scale for Geriatrics (Miller et al., 1992) to measure medical comorbidity. Participants completed a questionnaire that included a question asking how many hours per day they provided care. Participants also completed questionnaires measuring constructs previously associated with depression: the Activity Restriction Scale (Williamson and Schulz, 1992), the Intrusive Thoughts Questionnaire adapted for caregivers (Schulz et al., 2017), and the Five Facet Mindfulness Questionnaire (Baer et al., 2006).
Depression symptoms:
Depression symptoms were measured at study baseline with the Center for Epidemiologic Studies of Depression Scale–Revised Edition (CESD-R) (Radloff, 1977) and the PHQ-9 (Kroenke et al., 2001). We re-administered the PHQ-9 six-months after baseline via phone interview.
Statistical analysis:
First, the three available depression symptom measurements were entered into a person-centered clustering approach using finite normal mixture model implemented in the R Software package ‘MClust’ (Scrucca et al., 2016). As opposed to using traditional thresholds to create subgroups in our data, this clustering approach has key advantages, namely: (1) it allows us to identify naturally occurring subgroups in the data without using an arbitrary cut-point; and (2) it allows us to leverage data from three depression symptom measurements, thereby providing a fuller picture than any single measure. We used the Bayesian Information Criterion to select the optimal model, but specified that we would reject models which included small groups defined as <10% of the sample.
Next, we characterized differences between the identified subgroups (which had distinct depression symptom levels). We compared the above-listed characteristics using independent sample T-tests and Cohen’s D (Cohen, 1988) as a measure of effect size. We applied a Benjamini-Hochberg (Benjamini and Hochberg, 1995) multiple comparison correction for the activity pattern analysis (because this analysis included 24 variables each reflecting the average activity levels for an hour of the day).
After identifying the correlates of prevalent depression symptoms sub-groups, we conducted analyses aimed at identifying factors independently associated with changes in depression symptoms over time. We used multivariable regression analyses to determine if objectively-measured activity levels (at specific times of the day) related to changes in depression symptoms independent of self-reported covariates and actigraphy-assessed sleep fragmentation. We used a linear regression model with change in PHQ-9 scores (6-month minus baseline scores) as the outcome. As predictor variables, we included age, sex, baseline PHQ-9 score, and the statistically significant correlates of depression symptom subgroups identified in the initial analysis.
Results
Clustering identified groups with distinct depression symptom levels
The Bayesian Information Criterion indicated that a two-group solution was optimal (Supplemental Table 1). This empirical solution identified a majority subgroup of participants (64%) that had depression symptoms, and a minority of dCGs that had no/minimal symptoms of depression (Table 1). Note that the typical cut-off for predicting major depressive disorder using the CES-D is ≥16 (Radloff, 1977); on the PHQ-9 ≥5 is considered mild and ≥10 is considered moderate depression symptom levels (Kroenke et al., 2001). The means and standard deviations of symptom levels in the depression symptoms subgroup indicate mild symptoms approaching the range that is traditionally considered clinically meaningful.
Table 1.
Sample characteristics by subgroups with distinct depression symptom levels identified using model-based cluster analysis (n=56)
| Caregivers with depression symptoms, 64% (n=36) | Caregivers with minimal/no depression symptoms, 36% (n=20) | Cohen’s D | p-value | |
|---|---|---|---|---|
| 69.5 (5.6) | 73.3 (8) | −0.5 | 0.06 | |
| White race, % (n) | 97 (35) | 85 (17) | - | 0.09 |
| Female sex, % (n) | 72 (26) | 60 (12) | - | 0.35 |
| Care recipient is spouse, % (n) | 72 (26) | 70 (14) | - | 0.48 |
| Caregiver lives with care recipient, % (n) | 94 (34) | 75 (15) | - | 0.08 |
| Depression symptom levels | ||||
| Baseline CES-D | 15.2 (10.6) | 2.6 (2.3) | 1.2 | <0.0001* |
| Baseline PHQ-9 | 6.6 (3.4) | 1.3 (1.0) | 1.6 | <0.0001* |
| Six-month PHQ-9 | 5.4 (3.0) | 1.1 (1.0) | 1.4 | <0.0001* |
| Caregiving characteristics | ||||
| Number of caregiving activities | 8.7 (3.5) | 9.2 (3.3) | −0.1 | 0.48 |
| Hours providing care per day | 7.5 (5.4) | 6.1 (4.9) | 0.2 | 0.39 |
| Years of in the caregiving role | 6.3 (4.6) | 4.9 (2.8) | 0.3 | 0.19* |
| Sleep-wake factors | ||||
| Morningness-Eveningness Questionnaire (higher indicates more of a preference for morning) | 39.6 (7.8) | 45.4 (5.6) | −0.7 | 0.005 |
| Insomnia Severity Index | 10.2 (5.6) | 3.8 (3.8) | 1.0 | <0.0001* |
| Sleep fragmentation (minutes awake after sleep onset) | 40.9 (16.5) | 31.0 (16.1) | 0.5 | 0.03 |
| Epworth Sleepiness Scale | 8.0 (4.7) | 5.7 (3.7) | 0.4 | 0.10 |
| Other caregiver characteristics | ||||
| Activity Restriction Scale | 20.1 (6.7) | 14.6 (6.8) | 0.7 | 0.003 |
| Intrusive Thoughts Questionnaire | 9.3 (4.1) | 6.0 (4.6) | 0.6 | 0.006 |
| Five Facet Mindfulness Questionnaire | 99.3 (12.9) | 112.5 (10.0) | −0.9 | 0.0002 |
| Cumulative Illness Rating Scale for Geriatrics | 5 (3.1) | 3.6 (1.8) | 0.4 | 0.04* |
Means (standard deviations) shown unless otherwise noted. Acronyms: CES-D, Revised Center for Epidemiologic Studies – Depression Scale; PHQ-9, nine-item Patient Health Questionnaire. P-values are from T-tests or Chi-Squared tests except for: (1) the “live-in” status and race where Fischer’s exact test were required; and (2) asterisks indicate a Satterthwaite method was used to account for the unequal variances.
Baseline differences associated with membership in depression symptom groups
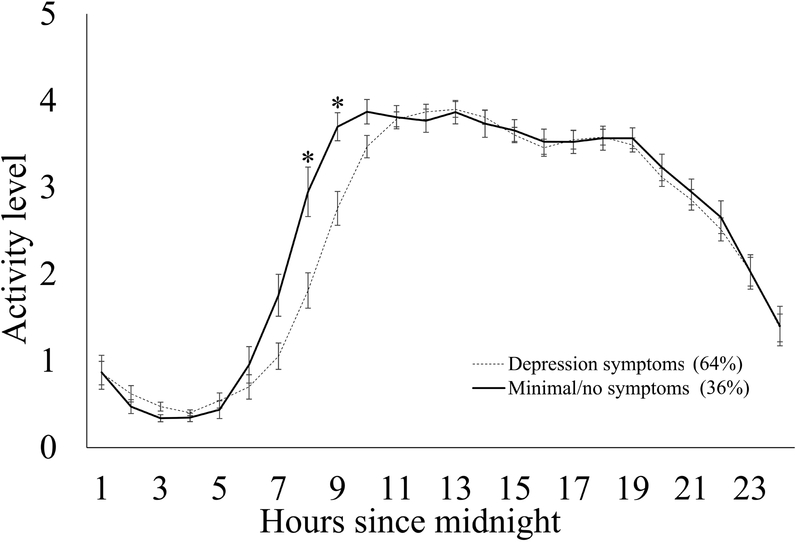
There were large differences in two specific hourly measures of activity between the groups that survived multiple comparison correction (Figure 1 and Supplemental Table 2). Dementia caregivers with depression symptoms had significantly less actigraphy-assessed activity in the hours from 8–10 AM (Cohen’s d’s≤−0.9); given that associations of these adjacent hourly bins were in the same direction, we summed activity levels in these hours to simplify subsequent modeling. Dementia caregivers with depression symptoms also had more activity in the 3 AM bin, though this association was not statistically significant after correcting for multiple comparisons.
Figure 1.
Activity levels in each hour since midnight in subgroups of dementia caregivers with distinct depression symptom levels. Asterisks indicates False Discovery Rates of less than 0.05 (see Supplemental Table 2).
There were also large differences in self-reported measures of potential risk factors for depression between the groups. The group with depression symptoms had relatively more insomnia symptoms (d=1.0), more actigraphy-assessed sleep fragmentation (d=0.5), less preference for morningness (d=−0.7), more activity restriction (d=0.7), more intrusive thoughts (d=0.6), lower mindfulness scores (d=−0.9), and a greater medical comorbidity (d=0.4).
Associations with changes in PHQ-9 scores over time
Only activity levels in the 8–10 AM period were associated with the degree of change in depression symptom levels over time (Table 2). For every standard deviation unit higher activity level in the 8–10 AM period, the PHQ-9 score decreased by 0.8 more units over 6 months. Because morning activity plausibly can be affected by alcohol consumption, we further adjusted for the frequency of alcohol use, which did not alter these estimates.
Table 2.
Associations of selected potential risk factors with six-month changes in PHQ-9 scores (n=56)
| β (95% confidence interval) | p-value | |
|---|---|---|
| −0.8 (−1.6, −0.1) | 0.03 | |
| Insomnia Severity Index | 0.4 (−0.5, 1.3) | 0.36 |
| Sleep fragmentation (minutes awake after sleep onset) | −0.1 (−0.8, 0.6) | 0.79 |
| Activity Restriction Scale | 0.5 (−0.4, 1.3) | 0.30 |
| Intrusive Thoughts Questionnaire | 0.4 (−0.5, 1.3) | 0.42 |
| Five Facets Mindfulness Questionnaire | 0.2 (−0.7, 1.1) | 0.64 |
| Cumulative Illness Rating Scale for Geriatrics | 0.01 (−0.3, 0.3) | 0.98 |
Linear regression model shown predicting PHQ-9 changes scores (six-month minus baseline score). The predictor variables listed were standardized to a mean of zero and a standard deviation of one to facilitate effect size comparison. All factors are included in a single model that also includes baseline PHQ-9 scores, age, and sex.
We did not include objectively-measured morning activity levels and the Morningness-Eveningness Scale in the same model because these two measures tap similar constructs and their correlation were high (Spearman r=0.6). Similar results were obtained when altering the model shown in Table 2 using the Morningness-Eveningness Scale in place of objectively-measured morning activity levels (per SD unit Morningness-Eveningness scale, β=−.8, 95% confidence interval: −1.6, 0.0, p=0.05). Race and live-in status were not initially included as covariates due to concerns that there were very few non-white and non-live-in dCGs in our sample (Table 1) but further adjusting for these factors did not alter our findings.
Given these findings, we also examined whether diary-assessed morning wake and rise times (time the individual gets out of bed in the morning) were also related to changes in depression symptoms over time. Later wake and rise times were similarly associated with the degree of symptom changes (per SD unit wake time, β=1.0, 95% confidence interval: 0.2, 1.8, p=0.01; per SD unit time out-of-bed, β=1.1, 95% confidence interval: 0.3, 1.9, p=0.006).
To further illustrate these results, we also report PHQ-9 scores at baseline and the six-month follow-up stratified by whether dCGs were above and below the median morning (8–10 AM) activity level (Table 3). Unlike dCGs above the median morning activity level, dCG’s below the median morning activity level maintained symptom levels in the mild range at the six-month follow-up.
Table 3.
Baseline and 6-month PHQ-9 scores by quartile of activity levels from 8–10 AM
| Baseline PHQ-9 | 6-month PHQ-9 | ||||
|---|---|---|---|---|---|
| Activity level from 8–10 AM | Mean | (95% confidence interval) | Mean | (95% confidence interval) | |
| Above the median (more morning activity) | 4.0 | (2.6, 5.4) | 2.6 | (1.5, 3.8) | |
| Below the median (less morning activity) | 5.3 | (3.9, 6.7) | 5.0 | (3.9, 6.1) | |
Discussion
Using data-driven clustering, we identified two distinct subgroups of dCGs: a minority who had minimal/no depression symptoms, and a majority who had a considerable symptom burden. Because the subgroups were similar on several markers of caregiving intensity, the group with minimal/no symptoms might be considered resilient to the stressors of dementia caregiving. In contrast, the group that had depression symptoms was characterized by insomnia symptoms, sleep fragmentation, reports of activity restriction, intrusive thoughts, lower levels of self-reported mindfulness, and a greater burden of medical comorbidity. These factors are all potentially modifiable and had similarly large associations with prevalent depression symptoms, suggesting multiple important features of prevalent symptomology (i.e., the qualities of depression in dCGs) that should be considered in interventions. But among these correlates of depression symptoms, only markers of morning activity independently predicted the degree of change in depression symptoms over time; these associations were independent of baseline symptom levels, actigraphy-assessed sleep fragmentation, and the self-reported correlates of prevalent depression listed above.
Measures related to morning activity (i.e., self-reported preferences, morning wake times, and times out-of-bed) were also associated with changes in depression symptoms over time. This suggests that, rather than being a characteristic of prevalent depression, staying in bed and not being active in the morning may shape the trajectory of depression symptoms in dCGs. Specifically, dCG’s with higher morning activity levels had lower levels of depression symptoms six-months later (Table 3); in contrast, dCG’s with lower morning activity levels maintained their mild depression symptoms (indexed by the PHQ-9) six-months later. Thus, low levels of morning activity may perpetuate depression symptoms, potentially impairing quality of life, and increasing the risk of future conversion to major depression.
These observations are consistent with prior evidence that a preference for “morningness” is associated with lower rates of depression (Taylor and Hasler, 2018). While the mechanisms behind these associations are not clear, more “eveningness” is associated with several known neurobiological correlates of depression: default mode network connectivity (Facer-Childs et al., 2019; Horne and Norbury, 2018), activation of frontal networks in the morning (Schmidt et al., 2015), and grey matter density in these regions (Takeuchi et al., 2015). It is plausible that morning inactivity reflects and/or leads to a lack of engagement in key circuits, e.g., those responsible for motivating action and deliberately regulating behavior. Our findings and this interpretation are consistent with evidence that negative mood is associated with a lower morning cortisol awakening response in caregivers (Leggett et al., 2014). Future work is needed to understand how these hormonal and neurobiological factors inter-relate in determining morning activity and its relationship with depression symptom.
Several limitations of this work should be noted. Because the follow-up period was relatively short and severe depression was not observed, we cannot be certain that these observations generalize to severe depression. Our finding that morning activity temporally precedes the degree of depression symptom change, independent of other factors, is consistent with a causal effect; but analyses were correlational in design and we cannot ascertain causality due to the potential of unmeasured (residual) confounding. Residual confounding, e.g., if morning activity marks an unmeasured pre-existing aspect of depression, could account for the longitudinal association of morning activity with the degree of symptom change. Additional limitations of the current work include a relatively small, older, and racially homogeneous sample, so these findings do not necessarily generalize to caregivers in different groups.
In conclusion, we have extended the existing literature on activity restriction and depression in caregivers (Mausbach et al., 2011) by examining objectively-measured 24-hour activity patterns in relation to depression symptoms and their persistence six-months later. The findings and limitations of the current work indicate that randomized experiments are needed to test whether modification of morning activity patterns has a causal and clinically meaningful effect on dCG’s mood. Existing interventions targeting psychosocial factors in dCGs (e.g., Cheng et al. (2016); Collins and Kishita (2018); Liu et al. (2017)) may yield additional benefits if they were to address the potential perpetuating effects of morning inactivity on depression. This proposal is consistent with the important role of behavioral activation in Cognitive Behavioral Therapy for depression (Beck, 1979). Behavioral activation aims to increase the frequency of active, positive, engagement by expanding exposures to potentially rewarding activities (Kanter et al., 2010; Lewinsohn et al., 1980). Our data specify that depression-vulnerable dCGs may be in particular need of help being active in the morning, e.g., by planning morning activities or respite services. Future studies are needed to test whether interventions that increase morning activity help mitigate subsyndromal symptoms and reduce the likelihood they progression to major depression. In addition, studies with longer follow-up periods and experimental designs are needed to determine whether passive monitoring of morning activity may be developed to achieve precision medicine risk stratification approaches.
Supplementary Material
Acknowledgements:
The funders had no role in the development or submission of this manuscript. SFS, BH, RS, CFR, DJB, HJA, and MHH designed the study. All authors conceptualized the analysis. JLG, RTK, and SFS designed the analytic pipeline. SFS executed the analysis and drafted the paper. All authors critically revised the paper and approved the final submission.
Funding: This study is supported by K01MH112683 to SFS and R01GM113243 to RTK. Recruitment support was provided through the University of Pittsburgh Alzheimer Disease Research Center (NIA #AG005133-28), the Pittsburgh Regional Caregiving Survey (funded by the Stern Family Foundation and the Emily Kelly Roseburgh Memorial Fund of The Pittsburgh Foundation), and the University of Pittsburgh Clinical and Translational Sciences Institute (UL1TR000005).
Footnotes
Declaration of interest: None.
References
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L, 2006. Using self-report assessment methods to explore facets of mindfulness. Assessment 13(1), 27–45. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallieres A, Morin CM, 2001. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep medicine 2(4), 297–307. [DOI] [PubMed] [Google Scholar]
- Beck AT, 1979. Cognitive Thearpy for Depression. Guilford Press, New York, NY. [Google Scholar]
- Benjamini Y, Hochberg Y, 1995. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society. Series B (Methodological) 57(1), 289–300. [Google Scholar]
- Cheng ST, Fung HH, Chan WC, Lam LC, 2016. Short-Term Effects of a Gain-Focused Reappraisal Intervention for Dementia Caregivers: A Double-Blind Cluster-Randomized Controlled Trial. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry 24(9), 740–750. [DOI] [PubMed] [Google Scholar]
- Cohen J, 1988. Statistical Power Analysis for the Behavioral Sciences. Routledge Academic; New York, NY. [Google Scholar]
- Collins RN, Kishita N, 2018. The Effectiveness of Mindfulness- and Acceptance-Based Interventions for Informal Caregivers of People With Dementia: A Meta-Analysis. The Gerontologist. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, 2005. Depressive disorders in caregivers of dementia patients: a systematic review. Aging & mental health 9(4), 325–330. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Smit F, 2004. Subthreshold depression as a risk indicator for major depressive disorder: a systematic review of prospective studies. Acta Psychiatr Scand 109(5), 325–331. [DOI] [PubMed] [Google Scholar]
- Dean DA II, Goldberger AL, Mueller R, Kim M, Rueschman M, Mobley D, Sahoo SS, Jayapandian CP, Cui L, Morrical MG, Surovec S, Zhang G-Q, Redline S, 2016. Scaling Up Scientific Discovery in Sleep Medicine: The National Sleep Research Resource. Sleep 39(5), 1151–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facer-Childs ER, Campos BM, Middleton B, Skene DJ, Bagshaw AP, 2019. Circadian phenotype impacts the brain’s resting-state functional connectivity, attentional performance, and sleepiness. Sleep 42(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne CM, Norbury R, 2018. Altered resting-state connectivity within default mode network associated with late chronotype. Journal of Psychiatric Research 102, 223–229. [DOI] [PubMed] [Google Scholar]
- Johns MW, 1991. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6), 540–545. [DOI] [PubMed] [Google Scholar]
- Joling KJ, Smit F, van Marwijk HW, van der Horst HE, Scheltens P, Schulz R, van Hout HP, 2012. Identifying target groups for the prevention of depression among caregivers of dementia patients. International psychogeriatrics 24(2), 298–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, Rusch LC, 2010. What is behavioral activation?: A review of the empirical literature. Clinical psychology review 30(6), 608–620. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, 2001. The PHQ-9: Validity of a Brief Depression Severity Measure. Journal of General Internal Medicine 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leggett AN, Zarit SH, Kim K, Almeida DM, Klein LC, 2014. Depressive Mood, Anger, and Daily Cortisol of Caregivers on High- and Low-Stress Days. The Journals of Gerontology: Series B 70(6), 820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Sullivan JM, Grosscup SJ, 1980. Changing reinforcing events: An approach to the treatment of depression. Division of Psychotherapy (29), American Psychological Association, US, pp. 322–334. [Google Scholar]
- Liu Z, Chen QL, Sun YY, 2017. Mindfulness training for psychological stress in family caregivers of persons with dementia: a systematic review and meta-analysis of randomized controlled trials. Clin Interv Aging 12, 1521–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Chattillion EA, Moore RC, Roepke SK, Depp CA, Roesch S, 2011. Activity restriction and depression in medical patients and their caregivers: a meta-analysis. Clinical psychology review 31(6), 900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, Mulsant B, Reynolds CF 3rd, 1992. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry research 41(3), 237–248. [DOI] [PubMed] [Google Scholar]
- Radloff LS, 1977. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement 1(3), 385–401. [Google Scholar]
- Schmidt C, Collette F, Reichert CF, Maire M, Vandewalle G, Peigneux P, Cajochen C, 2015. Pushing the Limits: Chronotype and Time of Day Modulate Working Memory-Dependent Cerebral Activity. Front Neurol 6, 199–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Savla J, Czaja SJ, Monin J, 2017. The role of compassion, suffering, and intrusive thoughts in dementia caregiver depression. Aging & mental health 21(9), 997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scrucca L, Fop M, Murphy TB, Raftery AE, 2016. mclust 5: Clustering, Classification and Density Estimation Using Gaussian Finite Mixture Models. The R journal 8(1), 289–317. [PMC free article] [PubMed] [Google Scholar]
- Smagula SF, Krafty RT, Taylor BJ, Martire LM, Schulz R, Hall MH, 2017. Rest–activity rhythm and sleep characteristics associated with depression symptom severity in strained dementia caregivers. Journal of sleep research 26(6), 718–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CS, Reilly C, Midkiff K, 1989. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. The Journal of applied psychology 74(5), 728–738. [DOI] [PubMed] [Google Scholar]
- Smith GR, Williamson GM, Miller LS, Schulz R, 2011. Depression and Quality of Informal Care: A Longitudinal Investigation of Caregiving Stressors. Psychology and aging 26(3), 584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi H, Taki Y, Sekiguchi A, Nouchi R, Kotozaki Y, Nakagawa S, Miyauchi CM, Iizuka K, Yokoyama R, Shinada T, Yamamoto Y, Hanawa S, Araki T, Hashizume H, Kunitoki K, Sassa Y, Kawashima R, 2015. Regional gray matter density is associated with morningness-eveningness: Evidence from voxel-based morphometry. NeuroImage 117, 294–304. [DOI] [PubMed] [Google Scholar]
- Taylor BJ, Hasler BP, 2018. Chronotype and mental health: recent advances. Current psychiatry reports 20(8), 59. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Schulz R, 1992. Pain, activity restriction, and symptoms of depression among community-residing elderly adults. Journal of gerontology 47(6), P367–372. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Spillman BC, Freedman VA, Kasper JD, 2016. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA internal medicine 176(3), 372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.