Abstract
Background:
Despite the frequent use of opioids to treat acute pain, the long-term risks and analgesic benefits of an opioid prescription for an individual emergency department (ED) patient with acute pain are still poorly understood and inadequately quantified.
Methods:
This was a prospective observational cohort study of opioid-naive patients presenting to two EDs for acute pain who were prescribed an opioid at discharge. Patients were followed by telephone six months after the ED visit. Additionally, we reviewed the statewide prescription monitoring program database. Outcomes included frequency of recurrent and persistent opioid use and frequency of persistent moderate or severe pain six months after the ED visit. Persistent opioid use was defined as filling ≥6 prescriptions during the six month study period.
Results:
During nine months beginning in November 2017, 733 patients were approached for participation. 484 met inclusion criteria and consented to participate. 410 (85%) provided six-month telephone data. The prescription monitoring database was reviewed for all 484 (100%). Most patients (317/484, 66%, 95%CI: 61, 70%) filled only the initial prescription they received in the ED. One in five patients (102/484, 21%, 95%CI: 18, 25%) filled at least 2 prescriptions within the six month period. Five patients (1% 95% CI: 0, 2%) met criteria for persistent opioid use. Of these five patients, all but one reported moderate or severe pain in the affected body part six months later.
Conclusion:
While 1 in 5 opioid naïve ED patients who received an opioid prescription for acute pain upon ED discharge filled at least two opioid prescriptions in six months, only 1% had persistent opioid use. These patients were likely to report moderate or severe pain six months after the ED visit.
Introduction
Background
Prescriptions for opioids have risen during the past two decades with a resultant increase in opioid use disorder, related ED visits, and fatal and nonfatal overdose.(1) This surge in opioid prescribing has roots in an increased awareness of undertreated pain, a problem that has yet to be solved (2) even as voluntary programs and state-based regulations have been implemented to restrict opioid prescriptions.(3, 4) While it is becoming increasingly clear that problematic opioid use is associated with the duration and quantity of initial opioid prescriptions,(5, 6) the long-term risks of an opioid prescription for an individual patient with acute pain are poorly understood and inadequately quantified.
Importance
Opioids are commonly prescribed in emergency departments. Nationally, 14% of ED patients were discharged with a prescription for an opioid.(7) In one multi-center ED-based study, 17% of discharged patients received an opioid to treat pain.(8) Prospective data about the long-term risks of an opioid prescription for ED patients with acute pain are needed to inform the decision about which analgesic to prescribe at discharge.
Goals of this investigation
The goal of this project was to quantify the risk of continued use of prescription opioids following receipt of a single opioid prescription in the ED. We therefore conducted a prospective observational cohort study to determine:
The frequency with which opioid-naive patients with acute pain who present to an ED and receive an opioid prescription go on to obtain a subsequent opioid prescription during the six months following the initial visit;
The frequency with which these patients develop new onset persistent opioid use, defined for purposes of this study as ≥6 opioid prescriptions filled during the six month study period;
Whether persistent use of opioids was associated with persistent moderate or severe pain 6 months after the ED visit
Methods
Overview.
This was a prospective observational cohort study of opioid-naive patients presenting to two EDs for acute, new-onset pain who were prescribed an opioid at discharge. Patients were enrolled at the conclusion of the ED visit, and followed by telephone six months later. Patient interviews were supplemented with a review of medical records, including the New York State prescription monitoring program database. The Albert Einstein College of Medicine IRB reviewed and approved the study. All participants provided written informed consent.
Setting.
This study was performed in two EDs of Montefiore Medical Center, the academic medical center for the Albert Einstein College of Medicine in the Bronx, New York, which combined, receive over 180,000 visits annually. Salaried, trained, bilingual (English and Spanish) technician-level research associates staff both EDs around the clock.
Subject selection.
We included adults aged 18 years and older with a chief complaint of acute pain from any cause who were discharged home from the ED and were given a prescription for an oral opioid. To participate, patients had to have pain for ≤ 10 days and could not have experienced a similar pain in the preceding six months. Individuals could only be enrolled once and were required to be opioid naïve, which we defined as no use of any opioid (including methadone and buprenorphine) or tramadol within the previous six months, as determined by patient self-report and the NY State prescription monitoring database. We excluded patients for use of any analgesic >10 days per month on average prior to the onset of acute pain, and any patients who required admission to the hospital.
Measures.
Research associates interviewed patients during the ED visit, obtaining basic socio-demographic data, information on the location and duration of pain, and completed the Opioid Risk Tool, a validated 11-item instrument that predicts opioid misuse.(9) The research associates also collected data on type of opioid prescribed at ED discharge, dose, and duration. The information on type, dose, and number of opioid pills was used to calculate the total morphine milligram equivalents (MME) of the prescription (https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf).
During the six-month telephone follow-up, research associates collected data on the following outcomes: Use of any analgesic medication during the previous week including opioids, prescription medication, and over the counter medication, and worst pain experienced in the affected site during the previous week. Pain was measured using a four-item ordinal scale with the following categorical descriptors: severe, moderate, mild, or none. We also inquired about the frequency of pain during the six months since the ED visit. Patients who reported pain on ≥50% of days since the ED visit were considered to have developed new onset chronic pain. During the six-month follow-up, we also asked patients whether they used any non-prescription opioids.
As part of a clinical program, in which individually tailored interventions were offered to ED patients prescribed an opioid who demonstrated potentially problematic usage post-discharge, we reviewed data from the NY State Prescription Monitoring Program database six months after the ED visit. All controlled substances dispensed by pharmacists in NY State are entered into the database. At six months, we abstracted the following information about dispensed opioids: type of medication dispensed, amount, and date of dispensing. For the purpose of this analysis tramadol and buprenorphine were considered opioids; cough suppressants and anti-diarrheals were not. To be considered an anti-tussive, the medication had to contain a non-analgesic component that could be used to treat cough or upper respiratory infections such as guaifenesin, an anti-histamine, or a decongestant.
Outcomes.
The primary outcome was recurrent opioid use, defined as the frequency with which patients received a second opioid prescription within six months of the ED visit. An important secondary opioid outcome was persistent opioid use, defined as ≥6 opioid prescriptions (an average of ≥1 per month) within the six month study period. Because there is no standard definition for persistent opioid use, we also present data on the following alternative definition of persistent use: a prescriptions for ≥ 10 day supply of opioids in at least three of the six months. We also report the frequency with which patients used an opioid within 30 days of the six-month follow-up (current opioid use). For all opioid outcomes, we used a composite of patients’ report plus data from the state database. If there was a discrepancy between these two sources of data, we erred on the side of over-reporting opioid use. We also report the frequency of moderate or severe pain at six months and the frequency of new-onset chronic pain.
Analysis.
We reported the frequency of all baseline variables as n/N (%), mean (SD), or median (IQR) as appropriate. We report the frequencies of primary and secondary outcomes as n/N (%) with 95%CI.
We compared baseline and pain variables among the following groups of patients: 1) those with persistent use (≥6 prescriptions); 2) those with recurrent but not persistent use (2-5 prescriptions); and 3) those with isolated or no use (0 or 1 prescriptions). Data are reported as n/N (%). Though limited by a paucity of data in the persistent use category, we report the mean difference with 95%CI or difference with 95%CI between important variables. When the 95%CI did not cross 0, we considered the difference to be statistically significant.
We did not perform regression analysis because of the paucity of patients with persistent opioid use.
Our sample size calculation was based on our wish to report the precision of the frequency of recurrent opioid use within 3%. Based on published data, we anticipated that 14% of patients would receive a subsequent opioid prescription.(10) Therefore, we needed complete data on 420 patients. We anticipated that as many as 10% of patients would have incomplete data. Thus, we intended to enroll patients until we had complete data on at least 462 patients.
Results
During a nine-month period beginning in November 2017, 733 patients were approached for participation and 484 met inclusion criteria and consented to participate (Figure 1). The most frequent reason for exclusion was use of opioids in the 6 months prior to the ED visit.
Figure 1.
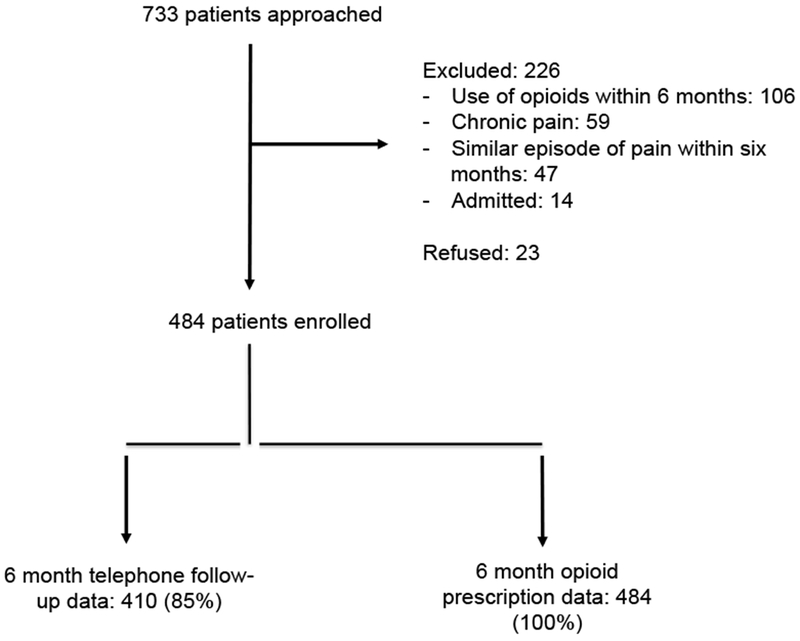
Participant flow diagram
The location of acute pain most commonly reported by patients was in the extremities, followed by back and neck, and abdomen and pelvis. Oxycodone with acetaminophen was the most frequently prescribed opioid. MMEs prescribed and other baseline variables are reported in Table 1.
Table 1.
Baseline variables
| Variable | Entire cohort (n=484) |
|---|---|
| Baseline variables | |
| Age in years, mean (SD) | 46 (16) |
| Sex | |
| Male | 215 (44%) |
| Female | 269 (56%) |
| Location of pain | |
| Extremity | 224 (46%) |
| Neck and back | 103 (21%) |
| Abdomen-pelvis | 99 (20%) |
| Face | 37 (8%) |
| Chest | 17 (4%) |
| Head | 4 (1%) |
| Diagnosed with fracture | |
| No | 405 (84%) |
| Yes | 79 (16%) |
| Pain duration in days, median (IQR) | 2 (1, 4) |
| Opioid Risk Tool score | |
| Low risk | 428 (88%) |
| Moderate risk | 38 (8%) |
| High risk | 18 (4%) |
| Opioid prescribed | |
| Oxycodone-acetaminophen | 375 (77%) |
| Codeine-acetaminophen | 105 (22%) |
| Hydrocodone-acetaminophen | 3 (1%) |
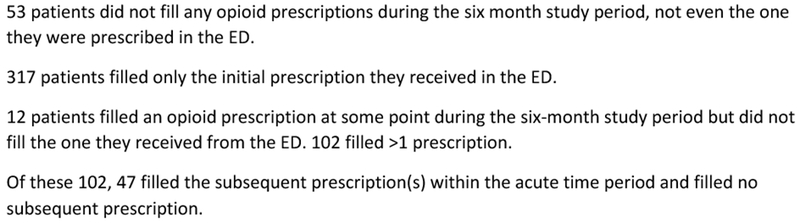
Within the six month study period, one in five patients filled at least 2 prescriptions (Table 2). Five patients filled six or more prescriptions in the 6 month period. These five patients, who filled 6, 7, 9, 11, and 15 prescriptions, are described in more detail in Figure 2. Five patients filled prescriptions for ≥ 10 day supply of opioids in at least three of the six months (All five patients who met the first persistent use criterion also met the alternative persistent use threshold). At the time of the six-month follow-up, 16/484 (3%, 95%CI: 2, 5%) had current opioid use, as determined by an opioid prescription filled within the previous 30 days or patient self-report. No patient (0/404, 0%, 95%CI: 0, 1%) reported recent use of illicit or non-prescribed opioids.
Table 2.
Usage of Prescription Opioids during the 6-Month study period among all 484 patients in the cohort
| Opioid outcome | N (%,95%CI |
|---|---|
| Recurrent opioid use: Filled 2 or more prescriptions within 6-month period | 102 (21%, 95%CI: 18, 25%) |
| Recurrent opioid use, acute time frame only: Filled two or more prescription within the first month after the ED visit, but none in the subsequent five months | 47 (10%, 95%CI: 7, 13%) |
| Persistent opioid use: Filled 6 or more prescriptions within 6-month period | 5 (1%, 95% CI: 0, 2%) |
| Persistent opioid use (alternative definition): Filled prescriptions for ≥10 day supply of opioids in at least 3 of the 6 months | 5 (1%, 95%CI: 0, 2%) |
| Current opioid use: Filled a prescription in the month before the 6- month anniversary of the initial ED visit | 16 (3%, 95% CI: 2, 5%) |
Figure 2.
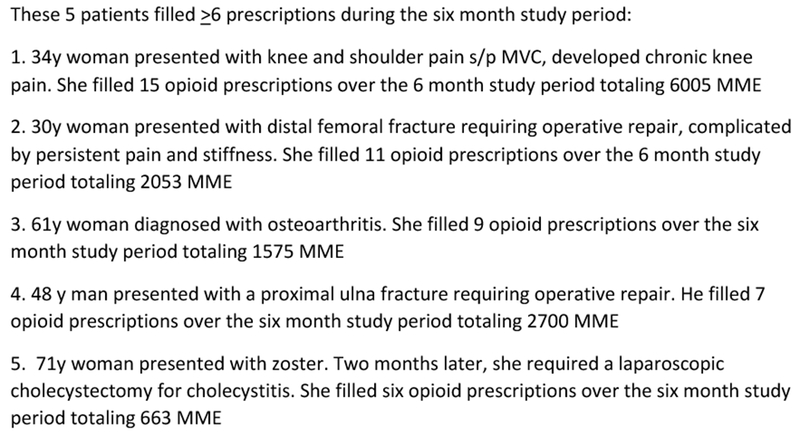
Detailed description of the five patients who filled >6 prescriptions during the six month study period
The full opioid prescription distribution is shown in Figure 3. Of note, 53/484 (11%, 95%CI: 8,14%) did not fill any opioid prescriptions during the six month study period, not even the one they were prescribed in the ED. Most patients (317/484 (66%, 95%CI: 61, 70%) filled only the initial prescription they received in the ED. 12 patients (2%, 95%CI: 1, 4%) filled an opioid prescription at some point during the six-month study period but did not fill the one they received from the ED. As depicted in Table 3, most patients who filled one, two, or three opioid prescriptions did so within the first month after the ED visit and the group with persistent opioid use exhibited declining prescription frequency over time.
Figure 3.
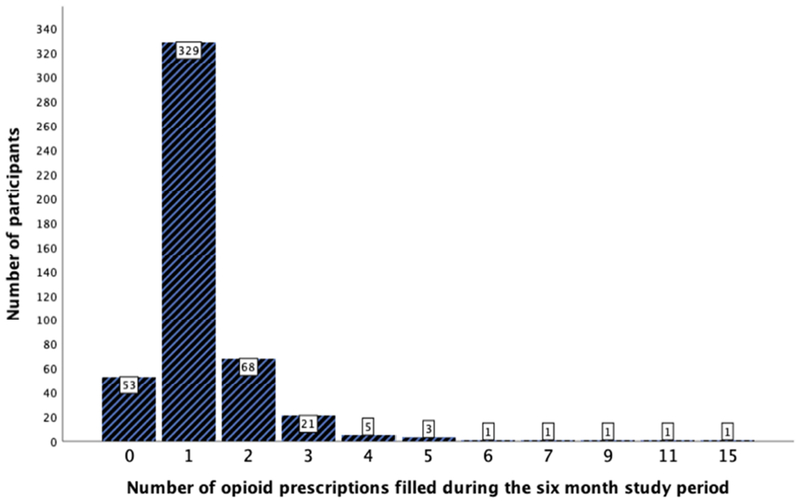
Number of prescriptions filled by each study participant
Table 3.
Total number of opioid prescriptions filled during the six month study period
| Number of opioid prescriptions filled by study participant | Number of participants in this group | Month 1 | Month 2 | Month 3 | Month 4 | Month 5 | Month 6 | Total number of opioid prescriptions filled |
|---|---|---|---|---|---|---|---|---|
| Number of opioid prescriptions filled | ||||||||
| 0 | 53 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 329 | 323 | 1 | 0 | 2 | 1 | 2 | 329 |
| 2 | 68 | 112 | 3 | 6 | 9 | 2 | 4 | 136 |
| 3 | 21 | 43 | 4 | 6 | 3 | 5 | 2 | 63 |
| 4 | 5 | 11 | 2 | 1 | 4 | 2 | 0 | 20 |
| 5 | 3 | 7 | 2 | 1 | 2 | 2 | 1 | 15 |
| >6 | 5 | 13 | 12 | 10 | 6 | 4 | 3 | 48 |
| Totals | 484 | 509 | 24 | 24 | 26 | 16 | 12 | 611 |
Table 3 compares the characteristics of the patients and their discharge medications across three groups: 1) those without recurrent use (0 or 1 prescription filled); 2) those with recurrent use but without persistent use (2 to 5 prescriptions filled); and 3) those with persistent use (6 or more prescriptions filled). The distribution of baseline characteristics was not clinically meaningfully dissimilar, though all five patients who developed persistent use were prescribed oxycodone (5/375 1% 95%CI: 0, 3%) versus none of the codeine patients (0/105 0%, 95%CI: 0, 4%). There were substantial differences among the three groups in frequency of low-risk Opioid Risk Tool scores. However, this tool misclassified as low risk the majority of patients who went on to persistent use. Poor pain outcomes were substantially more common among patients who filled ≥6 prescriptions than the patients in the other two groups. Four out of 5 (80%) patients who filled 6 or more prescriptions reported moderate or severe pain in the affected area versus 15% and 21% of patients who filled one or no prescriptions and 2-5 prescriptions respectively (Table 3). Similarly 4 of 5 (80%) patients who filled 6 or more prescriptions met the criteria for chronic pain versus 24% and 35% in the other 2 groups (Table 3).
Limitations
Several factors may affect the internal and external validity of these data. First, this study was conducted in two urban EDs from the same borough of New York City. Because pain and opioid outcomes are often affected by social and cultural factors, the generalizability of these data to other settings is uncertain. Second, almost all of the patients included in this study were prescribed oxycodone-acetaminophen or codeine-acetaminophen. Thus, it is uncertain whether these data are applicable to other types of oral opioids. Third, the accuracy of the NY state prescription monitoring program has never been reported publicly. Fourth, the NY prescription monitoring program does not capture opioid prescriptions filled outside of NY state. Fifth, 6-month opioid use is a surrogate outcome; we were not able to study rare outcomes with greater clinical importance such as opioid use disorder and overdose events. Sixth, while we surveyed patients about illicit opioid use, it was not feasible to collect objective data on this outcome. Seventh, prescribing providers were aware that their patients were being enrolled in this study. This may have caused them to prescribe fewer MMEs than they otherwise would have. And finally, there is no consensus in the published literature on what threshold of number of opioid prescriptions within a time period constitute persistent use. For purposes of comparison, an Appendix table shows the number of our patients who meet several other published criteria.
Discussion
In this prospective, observational cohort study based in two EDs in the Bronx, NY, 79% of 484 opioid-naive patients who were prescribed an opioid in the ED did not receive a second opioid prescription within the following six months; 1% of these 484 opioid-naive patients transitioned to persistent opioid use. These data suggest that limited use of opioid prescriptions among opioid-naive ED patients is unlikely to lead to opioid use disorder in the vast majority of patients. Also, because the group with persistent opioid use exhibited declining prescription frequency over time, one might suspect that this persistence is not necessarily going to be chronic for many. Persistent opioid use was associated with presence of moderate or severe pain and chronic pain six months after ED discharge.
Research among opioid-naïve patients utilizing opioid prescription databases has been undertaken in other settings (Appendix Table). Investigators have generally reported one of two types of outcomes: 1) Some investigators report the frequency of an opioid prescription among a cohort of patients at one specific moment in time some number of months removed from the event that led to participation in the cohort, often one year later.(10–12) 2) Other investigators report the number of patients who meet or exceed a threshold number of prescriptions within a certain amount of time.(5) Partly because of these different methodologies, reported estimates of frequency of persistent opioid use have shown substantial variation.
In an urban ED in Colorado, 14% of patients who were prescribed an opioid in the ED between September 2011 and February 2012 were using opioids approximately one year (+/− 60 days) after their ED visit.(10) In Ontario, 10% of elderly patients who filled an opioid prescription post-operatively during the years 1997-2008 were using an opioid approximately one year (+/− 60 days) later.(11) Among older adults who were victims of a motor vehicle collision during 2011-2014, 10% transitioned from opioid naive to daily use at six months.(13) The differences in the duration of the follow-up period and the definition of persistent use seem inadequate to explain entirely the generally lower rate of use at six months (3%) and persistent opioid use (1%) we identified in this study. A better explanation for these differences may be the years in which the data were gathered, as the risks associated with opioid prescribing have only gained widespread awareness more recently. However, one study with similar results to ours used data from US ED patients prescribed an opioid for ankle sprain between 2011 and 2015. (5) This latter study used a definition of persistent opioid use similar to ours too: four or more prescriptions during the five months following the acute injury, and identified a similarly low rate of persistent opioid use of 1%.
The low rate of persistent opioid use we identified in our study is probably a result of a recent increased awareness of the potential harms of opioids. This increased awareness was manifested by the relatively low cumulative doses of the initial prescriptions (median of 75 MMEs in this study), itself associated with lower rates of long-term opioid use.(6) Similarly, as evidence about the dangers of opioid prescribing has accumulated, there may be less willingness on the part of healthcare providers to initiate opioids upon discharge from the ED and in the outpatient setting, which may also explain why persistent use of opioids in this study was uncommon. Also, in recent years, NY State has erected barriers to opioid prescribing, including limiting opioid prescriptions for acute pain to seven days, mandatory topic-specific education for providers who prescribe opioids, and requirements for physicians to obtain a unique identifier from the state prior to opioid prescribing. These public health barriers, combined with increased provider awareness of the potential harms of large volume opioid prescriptions, may be having the desired effect.(14, 15)
This study helps place at least some component of the risk of persistent opioid use in the context of the risk of persistent pain among individual ED patients with acute pain at the time of discharge from the ED. Both moderate/ severe pain at the affected site and new-onset chronic pain were much more common than persistent opioid use, affecting more than ¼ of the cohort. Whether or not opioids can impact the trajectory of acute pain in selected patients is uncertain. Multiple studies suggest that among a general population of ED patients with acute pain, oral opioids do not confer more benefit than non-opioid alternatives.(16–18) Future research is needed to identify which ED patients can achieve short or longer-term analgesic benefit from opioids.
In this study, all five patients who converted to persistent opioid use were prescribed oxycodone. Some data suggest that oxycodone induces more euphoria than other oral opioids and therefore is more likely to be used inappropriately.(19, 20) While our data do not exclude the possibility that oxycodone is more likely to be associated with persistent opioid use, the incidence of persistent use among patients prescribed oxycodone was only 1% (versus 0% among those prescribed codeine). Therefore, we can tentatively conclude that limited prescribing of oxycodone does not adversely impact the vast majority of patients with acute pain who receive it.
It would be useful to be able to predict which opioid-naive patients are more likely to convert to persistent use. The opioid risk tool categorized 3 of the 5 patients in this study who developed persistent opioid use as low risk and therefore, based on these limited data, does not seem to have utility for ED patients. A variety of instruments have been used to predict poor opioid outcomes in various populations.(21) The lack of utility of these tools for ED patients has been reported previously.(22) Theoretically, important drivers of the transition from opioid naive to persistent opioid use are persistent pain and opioid-induced euphoria. Instruments targeted at these latter phenomena may predict poor opioid outcomes more accurately than instruments based on an individual’s personal and family history.
Among our three groups, there was an upward trend in the mean MME prescribed during the initial ED visit: 73 MME in patients with 0-1 prescriptions; 80 MME in patients with 2-5 prescriptions; and 92 MME in patients with ≥ 6 prescriptions. An association between prescribed MMEs and persistent opioid use or opioid overdose has been documented previously (5, 6, 23). Some expert consensus guidelines suggest prescribing no more than 3 days of opioids for acute pain to minimize the risk of transition to persistent opioid use(24, 25), though lower levels of MMEs are not risk-free(5). The impact of limiting opioid prescriptions on pain trajectories is still poorly understood.
Persistent use of opioids in this study was strongly associated with persistent moderate or severe pain and with new-onset chronic pain, albeit limited by a small number of cases. Only one of the five patients with persistent opioid use reported good pain outcomes. These data suggest that, among ED patients with acute pain, persistent opioid use may be a marker for undertreated pain. In conjunction with strategies to limit opioid use, effective pain management strategies are needed urgently. The path from opioid-naive to opioid use disorder is complex, and not likely to be amenable to over simplifications. However, the putative pathway to opioid misuse almost always involves persistent pain or opioid-induced euphoria. We have demonstrated an association between persistent pain and persistent opioid use. Future research should also address the impact of opioid-induced euphoria on the transition to opioid use disorder among patients with acute pain.
In conclusion, approximately 1% of opioid naive patients presenting to an ED for acute pain who received an opioid prescription upon ED discharge used opioids persistently throughout the six-month study period. These patients were more likely to report moderate or severe pain and chronic pain six months after the ED visit.
Supplementary Material
Figure 4.
Number of study participants who met each prescription threshold during each elapsed month
Table 4.
A comparison of socio-demographic, prescription, and pain variables by number of prescriptions filled during the six month study period
| Variable | Filled 0-1 prescriptions in 6 months (n=382) | Filled 2-5 prescriptions in 6 months (n=97) | Filled ≥6 prescriptions in 6 months (n=5) | Between-group differences | |||
|---|---|---|---|---|---|---|---|
| Filled 2-5 versus 0-1 Difference (95% CI) | Filled ≥6 versus 0-1 Difference (95% CI) | Filled ≥6 versus 2-5 Difference (95%CI) | |||||
| Age in years, mean (SD) | 46 (16) | 47 (17) | 49 (17) | 2 years* (−2, 5 years) | 3 years (−11, 17 years) | 1 year* (−14, 17 years) | |
| Sex | |||||||
| Male | 168 (44%) | 46 (47%) | 1 (20%) | 3% (−8, 15%) | 24% (−11, 59%) | 27% (−9, 64%) | |
| Female | 214 (56%) | 51 (53%) | 4 (80%) | ||||
| Location of pain | |||||||
| Extremity | 166 (43%) | 54 (56%) | 4 (80%) | 12%* (1, 23%) | 37% (1, 72%) | 24% (−12, 61%) | |
| Other** | 216 (57%) | 43 (44%) | 1 (20%) | ||||
| Pain duration before ED visit, mean number of days (SD) | 3 (2) | 3 (3) | 3 (2) | 0 days (−0.2, 1.0 days) | 0 days (−2, 2 days) | 0 days (−2, 3 days) | |
| Opioid risk tool score | |||||||
| Low risk | 341 (89%) | 84 (87%) | 3 (60%) | 3%* (−5, 10%) | 29% (−14, 72%) | 27% (−17, 70%) | |
| Moderate risk/High risk | 41 (11%) | 13 (13%) | 2 (40%) | ||||
| Opioid prescribed | |||||||
| Oxycodone-acetaminophen | 295 (77%) | 75 (77%) | 5 (100%) | 0% (−9, 9%) | 23% (19, 72%) | 23% (14, 31%) | |
| Other opioids** | 87 (23%) | 22 (23%) | 0 (0%) | ||||
| Morphine milligrams equivalents (MME) dispensed, mean (SD) | 73 (32) | 80 (43) | 92 (77) | 7 MME (−1, 15 MME) | 19 MME (−10, 48 MME) | 12 MME (−29, 53 MME) | |
| Worst pain in affected area at 6-month follow-up | |||||||
| Mild/ none | 273 (85%) | 65 (79%) | 1 (20%) | 5% (−4, 15%) | 65% (29, 100%) | 59% (23, 95%) | |
| Moderate/ Severe | 50 (15%) | 17 (21%) | 4 (80%) | ||||
| Missing | 59 | 15 | 0 | ||||
| Chronic pain | |||||||
| No | 244 (76%) | 53 (65%) | 1 (20%) | 11% (0, 23%) | 56% (21, 91%) | 45% (8, 81%) | |
| Yes | 77 (24%) | 29 (35%) | 4 (80%) | ||||
| Missing | 61 | 15 | 0 | ||||
Rounded
Please see Table 1 for the categories comprising “other”.
Acknowledgments
This publication was supported in part by the Harold and Muriel Block Institute for Clinical and Translational Research at Einstein and Montefiore grant support (UL1TR001073)
Appendix Table.
How other investigators defined persistent opioid use + our results using their definition
| Author | Condition | Years and geographic source of data | Definition of Opioid Use | Their findings | Our findings using their definitions |
|---|---|---|---|---|---|
| Delgado(5) | ED ankle sprains | 2011-2015, US | Persistent use: 4 or more prescriptions 30-180 days after index visit | 0.73% (95%CI: 0.63% to 0.84%) | 5/484 (1%, 95%CI: 0, 2%) |
| Clarke(12) | Major surgery | 2003-2010, Ontario | Persistent use: one or more opioid prescriptions within 1 to 90 days after surgery along with one or more prescriptions for opioids within 91 to 180 days after surgery. | 3% | 31/484 (6%, 95%CI: 5, 9%) |
| Platts-Mills(13) | Elderly adults s/p motor vehicle collision | June 2011-June 2014 Florida, Massachusetts, Michigan, and New York |
New daily opioid use | 14/143 (10%) | 0/484 (0%, 95%CI: 0, 1%) |
| Alam (11) | Low-risk surgery | 1997-2008, Ontario | Opioid use, moment in time: An additional opioid claim within 60 days of 1 year anniversary of the surgery | 10% | Unable to compare |
| Hoppe(10) | ED | September 2011 and February 2012, Colorado | Opioid use, moment in time: Filled an opioid within 60 days of 1 year anniversary of ED visit | 153/ 1079 (14%) | Unable to compare |
| Shah(6) | Commercially insured, cancer-free adults | 2006-2015, USA | Did not discontinue opioids: Discontinuation is ≥180 days without opioid use | 33,548/1,294,247 (2.6%) | Unable to compare |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
We have no conflicts of interest to report.
References
- 1.CDC December 19, 2018;Pageshttps://www.cdc.gov/drugoverdose/data/prescribing.html on April 1, 2019.
- 2.Todd K, Crandall C, Choiniere M, Ducharme J. Pain in the Emergency Department: A multicenter study (Abstract). Academic Emergency Medicine Journal. 2006;13(5S). [DOI] [PubMed] [Google Scholar]
- 3.Broida RI, Gronowski T, Kalnow AF, Little AG, Lloyd CM. State Emergency Department Opioid Guidelines: Current Status. West J Emerg Med. 2017;18(3):340–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Juurlink DN, Dhalla IA, Nelson LS. Improving opioid prescribing: the New York City recommendations. JAMA. 2013;309(9):879–80. [DOI] [PubMed] [Google Scholar]
- 5.Delgado MK, Huang Y, Meisel Z, Hennessy S, Yokell M, Polsky D, et al. National Variation in Opioid Prescribing and Risk of Prolonged Use for Opioid-Naive Patients Treated in the Emergency Department for Ankle Sprains. Ann Emerg Med. 2018;72(4):389–400 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah A, Hayes CJ, Martin BC. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use - United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mazer-Amirshahi M, Mullins PM, Rasooly I, van den Anker J, Pines JM. Rising opioid prescribing in adult U.S. emergency department visits: 2001-2010. Acad Emerg Med. 2014;21(3):236–43. [DOI] [PubMed] [Google Scholar]
- 8.Hoppe JA, Nelson LS, Perrone J, Weiner SG, Prescribing Opioids Safely in the Emergency Department Study I, Prescribing Opioids Safely in the Emergency Department PSI. Opioid Prescribing in a Cross Section of US Emergency Departments. Ann Emerg Med. 2015;66(3):253–9 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6(6):432–42. [DOI] [PubMed] [Google Scholar]
- 10.Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. 2015;65(5):493–9 e4. [DOI] [PubMed] [Google Scholar]
- 11.Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–30. [DOI] [PubMed] [Google Scholar]
- 12.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Platts-Mills TF, Flannigan SA, Bortsov AV, Smith S, Domeier RM, Swor RA, et al. Persistent Pain Among Older Adults Discharged Home From the Emergency Department After Motor Vehicle Crash: A Prospective Cohort Study. Ann Emerg Med. 2016;67(2):166–76 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rasubala L, Pernapati L, Velasquez X, Burk J, Ren YF. Impact of a Mandatory Prescription Drug Monitoring Program on Prescription of Opioid Analgesics by Dentists. PLoS One. 2015;10(8):e0135957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wen H, Schackman BR, Aden B, Bao Y. States With Prescription Drug Monitoring Mandates Saw A Reduction In Opioids Prescribed To Medicaid Enrollees. Health Aff (Millwood). 2017;36(4):733–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beaudoin FL, Gutman R, Merchant RC, Clark MA, Swor RA, Jones JS, et al. Persistent pain after motor vehicle collision: comparative effectiveness of opioids vs nonsteroidal antiinflammatory drugs prescribed from the emergency department-a propensity matched analysis. Pain. 2017;158(2):289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang AK, Bijur PE, Esses D, Barnaby DP, Baer J. Effect of a Single Dose of Oral Opioid and Nonopioid Analgesics on Acute Extremity Pain in the Emergency Department: A Randomized Clinical Trial. JAMA. 2017;318(17):1661–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedman BW, Dym AA, Davitt M, Holden L, Solorzano C, Esses D, et al. Naproxen With Cyclobenzaprine, Oxycodone/Acetaminophen, or Placebo for Treating Acute Low Back Pain: A Randomized Clinical Trial. JAMA. 2015;314(15):1572–80. [DOI] [PubMed] [Google Scholar]
- 19.Wightman R, Perrone J, Portelli I, Nelson L. Likeability and abuse liability of commonly prescribed opioids. J Med Toxicol. 2012;8(4):335–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zacny JP, Gutierrez S. Subjective, psychomotor, and physiological effects profile of hydrocodone/acetaminophen and oxycodone/acetaminophen combination products. Pain Med. 2008;9(4):433–43. [DOI] [PubMed] [Google Scholar]
- 21.Chou R, Fanciullo GJ, Fine PG, Miaskowski C, Passik SD, Portenoy RK. Opioids for chronic noncancer pain: prediction and identification of aberrant drug-related behaviors: a review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guideline. J Pain. 2009;10(2):131–46. [DOI] [PubMed] [Google Scholar]
- 22.Chalmers CE, Mullinax S, Brennan J, Vilke GM, Oliveto AH, Wilson MP. Screening Tools Validated in the Outpatient Pain Management Setting Poorly Predict Opioid Misuse in the Emergency Department: A Pilot Study. J Emerg Med. 2019. [DOI] [PubMed] [Google Scholar]
- 23.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686–91. [DOI] [PubMed] [Google Scholar]
- 24.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016;315(15):1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chu J, Farmer B, Ginsburg BY, Hernandez SH, Kenny JF, Majlesi N, et al. ;Pageshttps://www1.nyc.gov/assets/doh/downloads/pdf/basas/opioid-prescribing-guidelines.pdf on June 17 2019. 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


