To the Editor,
The emergence of the novel coronavirus disease-19 (COVID-19) in December 2019 resulted in a significant number of cases as reported by the World Health Organization (WHO) and was subsequently declared by the WHO as a pandemic on Mar 11, 2020. The review of the WHO data reveals some perplexing facts.
There was a genetic variation of SARS-CoV-2, the etiologic agent of COVID-19 [1]. In addition, there were three genomic variants, termed A, B, and C, based on amino acid changes. COVID-19 variant A is the ancestral type, and both A and C types are found in significant proportions in Europe and America [2]. In the absence of a documented difference in the virulence of these COVID-19 variants, it is challenging to explain the wild differences in prevalence and mortality rates in the different countries affected by COVID-19. Differences in the diagnostic efforts, or differences in the definition or reporting cannot, in our opinion, explain the wide variation of the data.
Climactic conditions have been postulated as a potential explanation for heightened transmission of COVID-19 and the occurrence of community outbreaks in countries with temperature of 5–11 °C and low humidity resembles seasonal influenza [3]. However, other factors, such as greater number of commercial or tourist travel might independently influence the spread of COVID-19.
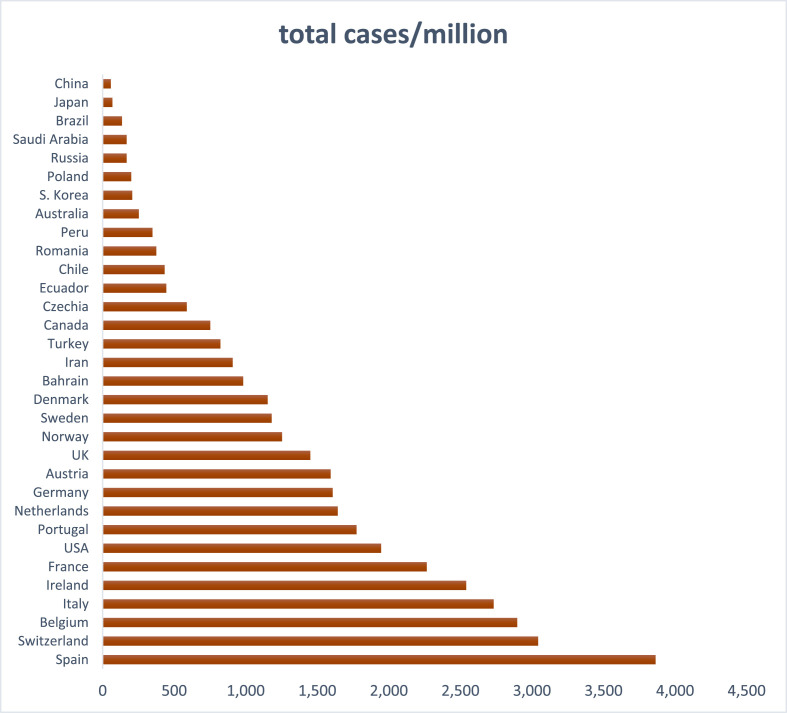
Specifically, when we examined the reported data, we were struck by the great variability of the number of confirmed cases per million. According to the available data as of April 16, 2020, the number of confirmed cases/million is 2732 in Italy, 207 in Korea, 909 in Iran, 982 in Bahrain, 3864 in Spain, 57 in China, 68 in Japan, and 168 in the Kingdom of Saudi Arabia (KSA) (Fig. 1 ).
Fig. 1.
Country-specific estimates of COVID-19 cases per million inhabitants (From https://www.worldometers.info/coronavirus/).
The orders of magnitude difference between Italy (2732/MM) and the KSA (168/MM) speak of an enormous difference in the propagation of COVID-19. This gigantic gap is dwarfed by the three order of magnitude difference between the KSA (168/MM) and the Italian epicenter in the province of Bergamo (>3000/MM).
When we examined the mortality rates reported by various countries, the mortality again varies greatly. Italy is reporting the highest mortality (13.1% on April 16, 2020), whereas, Iran (6.3%), China (4%), Spain (10.4%), France (11.6%) and Korea (2.1%) described lower mortality rates. At the bottom of the countries with low mortality are Bahrain and Singapore (with 0.3–0.4% mortality). Are there plausible explanations for the great variability in disease prevalence within the different countries? Social habits (greetings customs, ease to touch another person, kissing etc.) could possibly play a role, as could a greater susceptibility of the population, the presence of “super-spreaders” [4] or a delayed implementation of measures intended to stop the spread of infectious disease such as social distancing and closure of public areas. One study indicated that variation in prevalence could be due to differences in transmission and migration rates [3]. What enabled China to contain the spread of the epidemic was most certainly the coordinated effort of the central government to shut down Wuhan on January 23rd, followed on January 24th by the shutdown of another 15 cities: since then the number of new cases began to go down. This extremely successful endeavor is the result of draconian measures implemented with military discipline, and thus this measure maybe difficult to implement in western countries.
Are there plausible explanations for the great variability in mortality rate? There was a variation in the risk of death in a study from China. -The estimates of the risk for death was 12% in the epicenter of Wuhan and 1% in other, more mildly affected areas [5]. A higher average age of the population, (particularly in Italy with a median age of (47.4 years), accompanying higher percentage of comorbidities, most likely play a significant role in death rates. In one study, older age and higher Sequential Organ Failure Assessment (SOFA) score were associated with increased mortality [6]. Sadly, in certain instances, it appears that the underlying cause of dramatically higher mortality, to this date, was a drastic decrease in availability of critical resources. This decrease in resources leads to a functional collapse of the healthcare system and an overwhelmingly and unmanageable surge of people needing assistance in the intensive care units.
In the absence of a single plausible explanation for the existence of such dramatic disparities, we feel that home quarantine and isolation of the vulnerable populations (such as the elderly and the frail) along with the draconian measures being implemented in many countries are justified in order to successfully contain and eventually overcome the current pandemic due to COVID-19.
Funding source
None.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Shen Z., Xiao Y., Kang L., Ma W., Shi L., Zhang L. Genomic diversity of SARS-CoV-2 in coronavirus disease 2019 patients. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Forster P., Forster L., Renfrew C., Forster M. Phylogenetic network analysis of SARS-CoV-2 genomes. Proc Natl Acad Sci U S A. 2020 doi: 10.1073/pnas.2004999117. 202004999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neher R.A., Dyrdak R., Druelle V., Hodcroft E.B., Albert J. Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Med Wkly. 2020;150 doi: 10.4414/smw.2020.20224. w20224. [DOI] [PubMed] [Google Scholar]
- 4.Al-Tawfiq J.A., Rodriguez-Morales A.J. Super-spreading events and contribution to transmission of MERS, SARS, and COVID-19. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mizumoto K., Chowell G. Estimating risk for death from 2019 novel coronavirus disease, China, January-February 2020. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2606.200233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;6736:1–9. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]