Abstract
The coronavirus disease 2019 (COVID-19) pandemic is rapidly evolving. Tan Tock Seng Hospital and the National Centre for Infectious Disease see the majority of confirmed and suspected cases in Singapore. This article describes the impact of COVID-19 on the practice of hand and reconstructive microsurgery (HRM) in our institution. It details our department’s response as the situation escalated and the impact on the HRM elective and emergency workload, including the use of personal protective equipment on the surgical practice of HRM, as well as the effects of the condition on social and academic life.
Key words: Coronavirus, COVID-19, hand, microsurgery, surgery
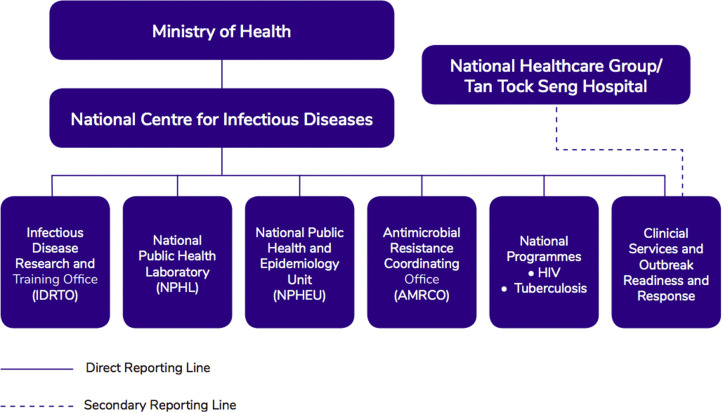
The coronavirus disease 2019 (COVID-19) pandemic has had an impact on health care systems worldwide. The disease was first detected in China in November 2019, and on January 23, 2020, Singapore confirmed the first imported case of COVID-19. Building on Singapore’s experiences with infectious disease outbreaks including severe acute respiratory syndrome in 2003, H1N1 influenza in 2009, and Zika in 2016, considerable resources, rigorous training, and planning have been put in place in preparation for new outbreaks. In September 2019, the National Center for Infectious Diseases (NCID) was established and is currently being used as a screening center and isolation facility for patients infected with COVID-19. The NCID is a 330-bed purpose-built and self-contained facility with expansion capacity close to 500 beds during an outbreak. It contains a large screening center, isolation, cohort and negative pressure wards, as well as a high-level isolation unit. Tan Tock Seng Hospital (TTSH), physically connected to the building (Fig. 1 ), is responsible for providing clinical services and is involved in outbreak readiness and response for NCID.1 As of April 2020, 56% of cases diagnosed with COVID-19 in Singapore had been admitted to TTSH-NCID.2 Because TTSH-NCID is the designated hospital for infectious diseases in Singapore, intrahospital measures and contingencies were instituted early in the course of the epidemic, ahead of nationwide recommendations.
Figure 1.
Structure of NCID.
This article describes the impact of COVID-19 on the practice of hand and reconstructive microsurgery in TTSH, whose function and staffing is intimately linked to that of NCID currently. We detail our department’s response as the situation escalated and seek to share lessons learned during this time of crisis.
Evolution of Hospital-Wide Measures
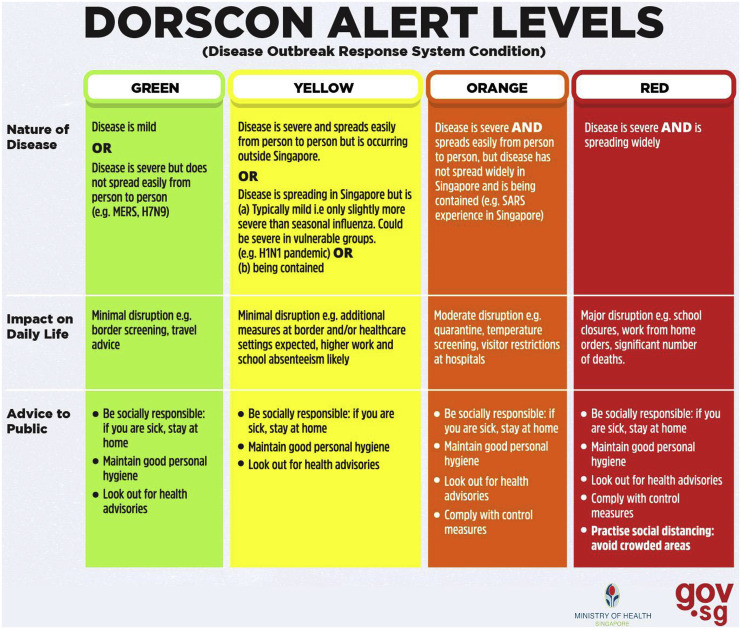
On December 31, 2019, after the World Health Organization was informed about 27 cases of pneumonia of unknown etiology detected in Wuhan City, Hubei Province of China,3 vigilance measures were carefully escalated in our institution. On January 2, 2020, our institution began to triage and isolate all suspected cases of patients with respiratory symptoms, fever, travel, or contact history. Hospital-wide N95 mask fitting and refresher training on powered air-purifying respirators was conducted in preparation for frontline duties. The use of surgical masks was enforced for health care workers in all clinical areas. Clinical heads across all departments began to plan staffing needs for the ensuing weeks to ensure their teams’ emergency readiness to be called and deployed in the event of an escalating situation; subsequently, all staff overseas and local leaves were canceled. On January 23, 2020, after Singapore confirmed the first imported case of COVID-19, nationwide contact tracing immediately commenced. On January 28, 2020, the NCID screening center was activated for all suspected cases of COVID-19, and selected clinical services were closed in our institution for diversion of staff. Singapore uses the Disease Outbreak Response System Condition (DORSCON) system,4 a color-coded framework that reflects the current disease situation (Fig. 2 ). On February 7, 2020, when 3 confirmed cases of COVID-19 were found to have no link to previous cases with travel history to China, and there was a possibility of community spread, the ministry of health raised the outbreak response to DORSCON Orange; temperature screening and visitor restrictions were enforced in all hospitals, apart from nationwide measures.
Figure 2.
Definition of DORSCON levels.
By March 2020, up to 50% of our institution’s workforce had been deployed to outbreak duties across TTSH and NCID to ensure sufficient rest days and reduced stress for all deployed staff. Doctors from medical departments have been deployed to run the outbreak wards in NCID, whereas those from surgical departments have been deployed to the NCID screening center. Almost all doctors from the Hand and Reconstructive Microsurgery (HRM) Department, from junior medical officers to senior consultants, have performed deployment duties at the NCID screening center.
The NCID screening center is the primary designated location in Singapore for screening suspected cases of COVID-19. The sources of these suspect cases range from primary health care physicians’ referrals, ambulance conveyances, passengers arriving from airports and seaports, unwell hospital staff, and walk-in patients. Surgical division doctors, including those from our department, work alongside emergency physicians in assessing patients clinically, and with investigations such as chest radiographs and nasopharyngeal swabs for COVID-19 testing. At the screening center, strict infection control measures are enforced; every health care worker is required to wear an N95 mask, goggles, a shower cap, a long-sleeved gown, and 2 pairs of gloves. Before deployment, an orientation lecture and walkabout of the screening center is performed to familiarize all doctors with the workflow and reinforce the procedures of donning and removal of personal protective equipment (PPE).
Impact on HRM Elective Workload
As of March 2020, 31% of HRM operations have been postponed. Elective workload has been reduced for 3 reasons.
Reduced anaesthesia support
This is the primary reason: anesthetists have been deployed to the NCID intensive care unit (ICU). Accordingly, we have reduced our elective general anesthesia cases; examples of such cases include surgeries for thumb carpometacarpal joint osteoarthritis, wrist arthroscopies, tendon transfers, and arthrodesis procedures. When possible, certain operations, such as the removal of implants and fixation of simple fractures, have been converted from general anesthesia to be done under local anesthesia. Time-dependent general anesthesia operations such as nerve transfers and fracture fixations proceed as usual. Our department is fortunate to have a separate local anesthesia theater; this theater is also lead-lined; therefore, surgeries requiring fluoroscopic assistance are able to proceed without anesthesia support.
Reduced number of HRM doctors owing to redeployment to NCID
As a result, the number of surgeons per surgery have been reduced as well. Fortunately, most HRM surgeries can be performed by 1 or 2 surgeons.
Reduced beds available for inpatient stay
This is another important reason for reducing the elective workload for disciplines such as general surgery and orthopedic surgery, for which postoperative patients may require inpatient hospitalization for a few days. Because most HRM procedures can be performed as day surgery, this has not been a major factor in reducing our elective workload.
As of April 2020, workload in the specialist outpatient setting has been scaled down to 34% compared with the 2019 monthly average. Patients per clinic session have been reduced by postponing nonurgent appointments; each patient is individually called and case notes are reviewed to determine which cases are nonurgent and can be postponed. Where appropriate, telemedicine is utilised for clinical consultation. The reduction in clinic load resulted in minimizing patient congregation in the clinics as well as shortened waiting time from registration to consultation. For stable patients whose appointments were postponed, the outpatient pharmacist team is mobilized to dispense medications by telecounseling and home delivery services if necessary.
Impact on HRM Emergency Workload
The emergency workload of the HRM department remained constant despite a reduction in staffing by up to 33%. Beginning late March 2020, our ministry directed the national ambulance services to divert non–COVID-related emergency conveyances to other hospitals owing to increased COVID-related workload in our institution. Although this measure reduced the emergency workload for certain clinical disciplines, the hand surgery emergency workload remained relatively constant for 2 reasons: (1) most patients are not conveyed by ambulance; they are often stable enough to come to the hospital without emergency services support; and (2) severe hand injury was an exclusion criterion for the national ambulance services diversion, because our institution is the only one with a 24-hour dedicated hand unit in the northern and central regions of Singapore.
Because our emergency workload did not decrease, consultants and senior residents had to perform step-down call duties.
Impact on HRM Surgical Practice
Corona virus 2019 has had a major impact on the practice of HRM. Table 1 lists guidelines for the types of PPE required for various cases in our operating room (OR). Operations for patients with positive contact or travel history are performed in a dedicated OR with one-way human traffic and strictly supervised donning and removal of PPE. Surgical procedures for patients diagnosed with COVID-19 are performed exclusively in the NCID OR.
Table 1.
Types of PPE Required for Various Cases in OR
| Type of Case | Goggles | Surgical Mask | N95 Mask | Gown | Powered Air-Purifying Respirator |
|---|---|---|---|---|---|
| Non-suspect | ✓ | ✓ | |||
| COVID-19 symptoms or diagnosed pneumonia | ✓ | ✓ | ✓ | ||
| Positive contact or travel history | ✓ | ✓ | |||
| Diagnosed COVID-19 | ✓ | ✓ |
Our approach to performing surgeries on COVID-19 patients is to delay the surgery whenever clinically feasible, until the patient is stable and the COVID-19 swab is negative.
The comfort of PPE is an issue with prolonged surgeries. An N95 mask has not been shown to cause a statistically significant physiological burden during 1 hour of use; however, continuous use of the N95 exceeding 4 hours is associated with the development of headaches.5 , 6 Because the surgeon’s comfort is vital, in the setting of a possibly long surgery in a COVID-diagnosed or suspected patient, we recommend a break every 2 hours, which can be aligned with tourniquet breaks.
Besides the N95 mask, thick goggles pose additional difficulties during surgery. Based on our department’s experience, thick goggles create an additional barrier to microscope use and an even greater challenge when used over surgical loupes.
In the setting of a need for flap reconstruction in a COVID-19 confirmed or suspected patient, considerations are to postpone the surgery when possible. In the unlikely situation in which early flap coverage is essential, we aim to perform a pedicled flap to avoid a longer free flap procedure. Instead of using surgical loupes for dissection, we use the microscope. If a free flap is necessary, it is essential to plan the timings carefully: flap ischemic time, time taken to perform microanastomoses, and N95 comfort time.
Impact on Social and Academic Life
Although all interhospital and intrahospital teaching meetings have been canceled, doctors in our department have been using time allocated for education, for self-directed studying, and to write academic papers and read journals. Because we have started to become accustomed to the new norm in the setting of this outbreak, since April 2020, we have resumed small-group continuing medical education meetings and large-group continuing medical education meetings with the assistance of teleconferencing. We are also reinstating small-group microsurgery workshops for residents in our microsurgery laboratory.
Social distancing is constantly reinforced among health care workers. The department is currently functioning based on team-based rounds and calls; interactions among teams or other health care workers are strongly discouraged within and beyond the hospital. From April 7, residents in Singapore were no longer allowed to dine in at food and beverage outlets and only takeaways and deliveries are allowed; staff either eat at their own workstations or allocated seats. All health care workers have been issued oral thermometers and are tracked closely by our institution through self-reporting of temperature. Health care workers are also advised to have a low threshold for reporting sick and are referred to the NCID screening center, if necessary.
Moving Forward and Lessons Learned
The COVID-19 outbreak is expected to last for a substantial period. The prime minister of Singapore, during his national address on COVID-19,7 and Dale Fisher, chair of the Global Outbreak Alert and Response Network steering committee for the World Health Organization, expect the COVID-19 crisis to continue for at least a year.8 With ongoing plans to increase the number of ICU beds in the NCID, a group of intensivists has been appointed to train more staff to be equipped with basic intensive care knowledge and skills. If there is a further escalation to DORSCON Red4 status, a further drastic reduction in elective workload is expected.
With further reduction in operating room availability, we have planned some strategies.
Surgical fixation of fractures
Although arguments for and against plate osteosynthesis are beyond the scope of this article, with less OR space and general anesthesia support, it is essential to consider techniques that are quicker to perform, despite fixation that could possibly be less stable. This would include Kirschner wire fixation techniques for finger fractures, as well as interfocal and intrafocal pinning of distal radius fractures.9
Nonsurgical management of fractures
With reduced operating room space, there may be consideration for managing certain fractures that would have been normally managed surgically, through nonsurgical techniques instead. As an example, a distal radius fracture in a young patient, with a dorsal tilt of 30° and radiological predictors of instability,10 would normally be considered for surgery in our institution. However, when there is limited operating room availability, we would consider repeated manipulations during the first week to achieve as best a reduction as possible. If the malunion results, there is the option of performing a corrective osteotomy once the COVID-19 crisis settles.
Resurfacing procedures
When resurfacing is required, it is perhaps necessary to look away from the reconstructive elevator11 and look back at the reconstructive ladder12 and consider, when possible, simpler resurfacing options. These include split-thickness skin grafting, healing by secondary intention, or the use of negative pressure therapy. Although we would still endeavor not to compromise functional outcome, cosmetic outcome may be of a lower priority in this crisis situation. Secondary cosmetic procedures can always be considered at a later date.
Brachial plexus blocks
Although our department is currently not trained in regional anesthesia techniques, this crisis has made us consider being trained in brachial plexus blocks for future similar scenarios. We are well-versed with the wide-awake local anesthesia no tourniquet technique (WALANT)13 and will use the technique more frequently in the setting of reduced anesthetic support.
Our Role as Hand Surgeons
During this time of crisis, we are reminded once again of our calling as physicians as we work alongside our medical and emergency department colleagues to support the frontline battle against COVID-19. The HRM Department has in place emergency contingencies for staff diversion to support the NCID. The drain on health care resources and hospital beds has been reduced by scaling down elective operative and outpatient loads and recruiting more help from our allied health colleagues, physical and occupational therapists. We have further embraced technology in the form of teleconferencing, for purposes of information dissemination and continued learning. Encouraged by support from the public for health care workers,14 and under the strong leadership of our hospital, the HRM Department, together with the rest of Singapore’s health care community is committed to fight alongside fellow Singaporeans in the battle to overcome this pandemic.
Footnotes
No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.National Centre for Infectious Diseases NCID corporate brochure. https://www.ncid.sg/About-NCID/Documents/NCID%20Corporate%20Brochure.pdf Available at:
- 2.Singapore Ministry of Health COVID-19: Cases in Singapore. https://www.gov.sg/article/covid-19-cases-in-singapore Available at:
- 3.World Health Organization Novel coronavirus (2019-nCoV). Situation report 1. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf Available at:
- 4.Singapore Ministry of Health What do the different DORSCON levels mean? https://www.gov.sg/article/what-do-the-different-dorscon-levels-mean Available at:
- 5.Roberge R.J., Coca A., Williams W.J. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010;55(5):569–577. [PubMed] [Google Scholar]
- 6.Lim E.C., Seet R.C., Lee K.H. Headaches and the N95 face-mask amongst healthcare providers. Acta Neurol Scand. 2006;113(3):199–202. doi: 10.1111/j.1600-0404.2005.00560.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee H.L. Coronavirus: Full speech by PM Lee Hsien Loong on the COVID-19 outbreak. https://www.straitstimes.com/singapore/coronavirus-full-text-of-speech-by-pm-lee-hsien-loong-on-the-covid-19-outbreak Available at:
- 8.Fisher D. The current and future COVID-19 situation. https://news.nus.edu.sg/research/prof-dale-fisher-current-and-future-covid-19-situation Available at:
- 9.Greatting M.D., Bishop A.T. Intrafocal (Kapandji) pinning of unstable fractures of the distal radius. Orthop Clin North Am. 1993;24(2):301–307. [PubMed] [Google Scholar]
- 10.Mackenney P.J., McQueen M.M., Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am Vol. 2006;88(9):1944–1951. doi: 10.2106/JBJS.D.02520. [DOI] [PubMed] [Google Scholar]
- 11.Gottlieb L.J., Krieger L.M. From the reconstructive ladder to the reconstructive elevator. Plast Reconstr Surg. 1994;93(7):1503–1504. doi: 10.1097/00006534-199406000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Mathes S., Nahai F. Mosby; St Louis, MO: 1982. Clinical Application for Muscle and Musculocutaneous Flaps. 3. [Google Scholar]
- 13.Lalonde D. Wide awake local anaesthesia no tourniquet technique (WALANT) Biomed Central. 2015;9(3 suppl):A81. [Google Scholar]
- 14.Ho O. Singapore gives those on coronavirus front lines a round of applause. https://www.straitstimes.com/singapore/singapore-gives-coronavirus-frontliners-a-round-of-applause Available at: