Highlights
-
•
Countries need to develop well-planned exit strategies when the COVID-19 pandemic subsides.
Abstract
Aim
The purpose of this perspective is to review the options countries have to exit the draconian “lockdowns” in a carefully staged manner.
Methods
Experts from different countries experiencing Corona Virus Infectious Disease 2019 (COVID-19) reviewed evidence and country-specific approaches and the results of their interventions.
Results
Three factors are essential: 1. Reintroduction from countries with ongoing community transmission; 2. The need for extensive testing capacity and widespread community testing, and 3. An adequate supply of personal protective equipment, PPE, to protect health care workers. Discussed at length are lifting physical distancing, how to open manufacturing and construction, logistics, and the opening of higher educational institutions and schools. The use of electronic surveillance is considered.
Conclusion
Each country should decide on the best path forward. However, we can learn from each other, and the approaches are, in reality, very similar.
1. Introduction
With the SARS-CoV-2 pandemic passing one million ill people (1,521,252 confirmed cases and 92 798 reported deaths (WHO Sit Rep 10 April), most countries are occupied with controlling the outbreak. The economic consequences are enormous. The World Trade Organization (WTO) estimates that “commerce could shrink up to 32% and warns against 30s-style protectionism” [WTO, 2020].
With no vaccine and no proven effective treatment, the tools available are limited to physical distancing, which includes quarantine and travel restrictions. These tools are the same as were available during the black death due to plague in Europe in the 13th century, although modern molecular diagnostics and electronic surveillance have modified them slightly.
With no manual to follow, most countries have taken a broad approach to slow down the spread of the infection, trying to “flatten the curve” to prevent overwhelming health care systems by enforcing tight restrictions on population movements. This strategy has largely shut down society and reduced economic activity by closing offices and manufacturing plants, closing schools, restricting mobility in public places, closing non-essential shops, restricting traffic (road, air, and sea), and closing borders.
This comes with a heavy socio-economic price, particularly in low-and-middle-income countries with limited capacity to absorb prolonged national lockdowns. Many companies have or will request government support or file for bankruptcy. Unemployment is rapidly increasing, with devastating consequences on the lives of vulnerable populations, particularly in low- and middle-income countries (LMIC).
It is critical to plan for the reactivation of society, restarting work and production, opening up travel and education. Although no one knows the future, there have been speculations of a second wave that, so far, is conjectural but may well happen. A strategy or "roadmap" for de-escalating the enforced physical distancing, based on epidemiological indicators, is needed to inform citizens and policymakers.
From an epidemiological and medical point of view, this review discusses how strict isolation measures could gradually be lifted. The medical profession must lead the way out of the pandemic just as we shaped the response at the beginning.
2. The post-peak period–the “opening phase”
What is the "post-peak period“? There is no clear definition but most experts providing opinions to the media agree that having a plateau of cases or hospital admissions for two weeks signals that transmission has stabilized and hospitals are then able to treat all patients requiring hospitalization for COVID-19 without resorting to crisis standards of care [Zhang J et al., 2020].
This is the time when opening up a society should be considered. However, because most of the population has not yet been exposed, there are concerns that, with minimal but ongoing local transmission, new clusters might escape into the community, triggering a second wave of infections [Leung et al., 2020]. In the post-peak period, it will be important to classify the epidemiological situation to increase the understanding of and target transmission; we suggest the following, adapted from the WHO [WHO 19 March 2020] (Table 1 ).
Table 1.
Classification of new cases during surveillance in the “post-peak period adapted from the WHO (WHO 19 March 2020)
| A. Imported, i.e., likely infections from abroad |
| B. Part of a known cluster, or contact with a known case |
| C. Source unknown. |
Table 2.
A reopening of society should be staged according to the local situation
| Stage 1 | Restrictions lifted for a specific sector of the community, that could be schools, could be specific manufacturing industies, e.g., the construction industry, or could be limited to low endemic areas only. |
| Observe for two weeks, monitor hospital admissions, perform testing at key sites of all persons with upper and lower respiratory tract infections. | |
| Stage 2 | If the situation is stable, |
| Extend opening of manufacturing and construction industries | |
| Open public transport but request face mask in public spaces | |
| Open schools in more areas | |
| Open international travel from selected countries, quarantine arrivals from high endemic | |
| countries or perform a rapid DNA test on arrival or ask for pre-departure test | |
| Observe for two weeks, monitor hospital admissions, perform testing at key sites of all persons with upper and lower respiratory tract infections. | |
| Stage 3 | If the situation is stable, open all workplaces and open small shops and restaurants |
| provided physical distancing is maintained. Open international travels from selected countries, | |
| quarantine arrivals from high endemic countries, or perform a rapid DNA test on arrival or ask for pre-departure test | |
| Observe for two weeks, monitor hospital admissions, perform testing at key sites of all persons with upper and lower respiratory tract infections. | |
| Stage 4 | Open up for mass gatherings like football matches, religious meetings, etc. .. |
There are important lessons from countries such as China and Korea that managed to control the outbreak after experiencing a peak in the first-wave epidemic; Taiwan [Wang et al., 2020] and Macau [Lo et al., 2020] which managed to keep case counts low; and places where despite initial control there has been a resurgence such as Singapore and Hong Kong. The experience from these countries point to three main challenges:
-
1.
Reintroduction from countries with ongoing community transmission (still in the outbreak phase) may initiate a new outbreak in the susceptible population.
-
2.
The need for extensive testing capacity and widespread community testing to identify new cases as early as possible, coupled with effective contact tracing and isolation ability.
-
3.
The importance of an adequate supply of personal protective equipment, PPE, to protect health care workers.
3. Risk of introduction by travelers
The outbreak has demonstrated how easily a respiratory infection can spread across borders. If countries open up for travel before widespread SARS-CoV-2 immunity, there need to be interventions to reduce the risk of transmission from travelers who have few or no symptoms. Post-arrival quarantine has been applied effectively by South Korea, but this is impractical and cannot be implemented in most countries.
We believe that the International Health Regulation, IHR, an agreement between 196 countries including all WHO Member States to work together for global health security, has a vital role to play in the enforcement of more targeted travel restrictions [IHR 2005]. Under the IHR, using a mechanism similar to the Yellow fever immunization certificate requirement, travelers could be asked to provide proof of a previous infection, and therefore immunity, by having SARS-CoV-2 specific IgG antibodies [Petersen et al., 2020]. Seronegative travelers could be asked to undergo rapid testing (antigen or PCR in the airport or pre-departure). However, rapid testing technologies are not yet available for routine implementation [Petherick A et al., 2020].
In Hong Kong, truck drivers are required from the end of this week (9 April 2020) to produce evidence of a “SARS-Cov-2 negative medical certificate” when they cross the Hong Kong–Mainland border, as required by the Chinese government; these ∼10,000 drivers ensure that Hong Kong has food and commodities during the lockdown.“
South Korea imposed a two weeks mandatory quarantine on all travelers entering the country from 1 April; persons with a previous infection as documented by positive serology are exempt. This is analogous to healthcare workers who are required to document immunity to varicella, measles, mumps, rubella, and hepatitis B before working in most healthcare institutions.
Risk-based approaches to travel restrictions could also be considered. For example, travel restrictions could be eased between countries “past the peak” with local transmission at low levels. For instance, travels between Germany and China could be opened under certain conditions that persons from third countries with high transmission rates would not be eligible for. Another approach could be to open travel from countries with appropriate and efficient surveillance systems, transparent reporting, and few local cases where the risk of importing infected cases would be low. Opening aviation routes would require agreement between the two countries for direct flights.
4. The need for extensive test capacity
Lifting the general restrictions on mobility and physical distancing, allowing businesses to open, opening schools and higher education institutions, restarting manufacturing and allowing travel should only be done after peak incidence. However, the circulating virus has not disappeared, and resurgence remains a possibility. Determining the rate at which mild disease is spreading in the community is critically important to inform shifts between containment and mitigation strategies.
After de-escalation of enforced physical distancing by closing shops and workplaces, community-based symptom screening and testing must be made widely available to allow early identification of new cases. This will only be effective if supported by contact tracing, quarantine, and isolation of cases that need supervision by public health authorities. In low-and-middle-income countries, it will be essential to provide facilities for quarantine and isolation for people unable to safely do so in their homes.
In the opening phase, access to testing must be available to all people to allow identification of new cases and clusters as early as possible. This would ideally be supported by point-of-care tests that are accurate and reliable. There should also be effective surveillance systems for influenza-like illnesses, mortality rates, and sick leave.
Public health authorities must be appropriately staffed and equipped. A recent study from California, testing patients with respiratory symptoms, found that 11% of influenza-negative were SARS-CoV-2 PCR positive [Zwald ML 2020]; such testing at sentinel sites is an essential tool to keep track of community transmission.
Thus, public health capabilities for case identification and isolation must be expanded, probably permanently; tools can include physical inspection or use of electronic devices, such as mobile phone-based surveillance and point-of-care tests as used in Taiwan, Korea, and Oman, summarized in Table 3 .
Table 3.
Generic electronic surveillance system.
| The system use information from mobile phones or bracelets. The system is linked to a national electronic surveillance system and to the civil identification number and can be shared with other stakeholders, such as police or public prosecution. |
| An “Isolation Enforcement System” can provide supervision of the location of persons in isolation or quarantine outside institutions. |
| Isolation Tracking App |
| Isolation Compliance |
| Crowdsensing when people in quarantine move out of the isolation facility |
| Mobile phone and/or bracelet App |
| Self Reporting and symptoms analysis |
| Self Reporting Questionnaires |
| Translation and language support |
| The bracelet is for a single-use purpose that makes it very cost-effective and will be |
| able to measure the body temperature. |
| The system will allow authorities to supervise compliance with quarantine and isolation |
| - |
| 12-month battery life |
| Perform contact history by linking geographical location of SIM card or bracelet risk assessment according to the number of people quarantined or isolated in a specific geographic location. |
5. Lifting physical distancing
The examples from Korea, Singapore, and Hong Kong show that the virus will re-emerge if strict control measures are relaxed. The closure of all social activities and confining people at home has a profound effect on the economy and should only be maintained until other, more targeted measures of disease control are established. There are several approaches available to policymakers.
Containment efforts could be focussed on populations at the highest risk from infection, including people over 65 years old, people living in care institutions, and those with chronic medical conditions. These groups would need to be identified and supported to restrict their movements and practice physical distancing for a more extended period than the rest of society. Communications about such an approach will be critical as the public currently has a pronounced negative attitude towards any mention of herd immunity. During times of eased restrictions working from home - “teleworking” - should still be encouraged, and social gatherings discouraged.
Strategies to reduce workplace transmission include daily declarations of being symptom-free by all staff members and, where feasible, screening of staff by RT-PCR or even serology immediately after lifting of enforced quarantine; however, the need to screen everyone at a workplace before it opens up must be determined individually. This may be particularly important in higher-risk industries such as the hospitality sector (tourists and hotels) and aviation or others with high degrees of interaction with vulnerable populations. The occupational health service will be valuable when manufacturing and construction industries open to keep very close surveillance on employees and quarantine anyone with symptoms pending test results.
Similarly to targeted travel restrictions, opening up shops, offices, schools, and factories could be preceded by RT-PCR testing of asymptomatic or oligosymptomatic persons and/or the introduction of widespread serological testing to confirm immunity before removal of individual quarantine. This would require a massive mobilization of resources and is unlikely to be feasible in LMICs in the short term.
It is critical to have communities as partners understanding the need for restriction even while some parts of society start working again. The higher the buy-in and quality of response in every locality, the better the outcome.
Universal masking has been proposed as an additional strategy for reducing community transmission. Surgical masks may minimize the risk of community transmission from infected people [Leung et al., 2020; Chan and Yuen, 2020]. This appears to have been effective in countries such as Taiwan and South Korea and parts of Italy where mandatory mask-wearing was implemented, although an independent impact is difficult to assess. The WHO has recently stated that “the use of a medical mask can prevent the spread of infectious droplets from an infected person to someone else and potential contamination of the environment by these droplets” [WHO, 2020c, WHO, 2020d, WHO, 2020e 6 April]; opening workplaces and asking employees to wear a face mask–surgical mask or equivalent–for two weeks after opening is an option which must be discussed with the occupational health service. Lombardy in Italy imposed mandatory face masks in public places [The Guardian, 2020].
We do not know if this will prevent person-to-person spread to the same extent as the closure of shops, factories, educational institutions, and offices, but it makes sense that masks (including non-medical) will reduce expulsion of large infectious droplets as stated by the WHO, thus reducing the risk of transmission in public spaces.
In China, shops, restaurants, bars, and offices are opening; manufacturing activity is picking up, and traffic is starting to flow. Three-quarters of China's workforce was back on the job as of 24 March, according to one company's estimate. Wuhan, where the COVID-19 pandemic originated, is lagging, as is the rest of Hubei province—but even there, the lockdown was lifted on 8 April [Normille D 2020]. The impact of this has yet to be determined.
6. Surveillance identifying cases in society
COVID-19 clusters much more in families and households and social contacts of those households (Fan J et al., 2020). More granular geographical information is needed for effective contact tracing, for instance, using Geographical Information Systems (GIS). The lesson from South Korea is that tracking of cases and contacts via modern digital technology to apply focused testing can control community transmission without enforced distancing [Korean CDC 2020]. After identifying a case, contacts will be asked to self-quarantine and monitored by appropriate digital technology. Random sampling would help to estimate the number of mild or asymptomatic cases and inform about the actual attack rate in the population.
7. Infection control in the health care system
A well-established and robust core program of infection prevention and control within the healthcare system is central to preparedness and responsiveness. It will also need to be maintained as a priority in the recovery phase of healthcare systems and national exit strategies. As the number of COVID-19 inpatients diminishes and the proportion of inpatients that are COVID-19 naïve rises again, the likelihood of potential nosocomial infection may increase. There must be established hospital surveillance systems that can capture nosocomial infections rapidly and prevent the generation of hospital outbreaks and further waves of transmission.
Hand hygiene and environmental hygiene must be considered as underpinning priorities in protecting healthcare staff, and efforts must be made to promote physical distancing in health care settings. The SARS epidemic in Hong Kong demonstrated the vulnerability of front line health care workers (HCWs). Protecting HCWs is a major task, and sufficient personal protective equipment (PPE) must be available [Cheng VCC et al., 2020]. The protection of HCWs and support staff is critical, and the resilience of healthcare systems is dependent on sustaining their safety and their trust. For COVID-19 in comparison to SARS, particular attention is needed to ensure that HCWs who see individuals at the earliest stages in the disease, are well protected; this would include those working in the community and in residential and nursing care homes.
PPE guidelines for healthcare systems need to be clearly communicated, understood, supported by staff, and based on the best evidence. However, the PPEs recommended in any guidance must have the necessary supporting supply chains well defined and clearly mapped, along with the appropriate logistics and the capacity to maintain it. Without continuous adequate, appropriate PPE provision for HCWs and support staff, their sustained commitment and their trust, required for a successful exit strategy, may be lost [Cheng VCC et al., 2020; WHO IPC 2020].
8. Country specific experiences
Korea, Republic of
South Korea experienced the Middle East Respiratory Syndrome coronavirus (MERS-CoV) outbreak in 2015 with 186 confirmed cases, 38 fatalities, and a 20.4% case fatality rate [Korean CDC 2015]. Key lessons learned were the impact of a single missed case, which resulted in a nationwide outbreak and the importance of early detection and isolation of cases [Oh MD et al., 2018].
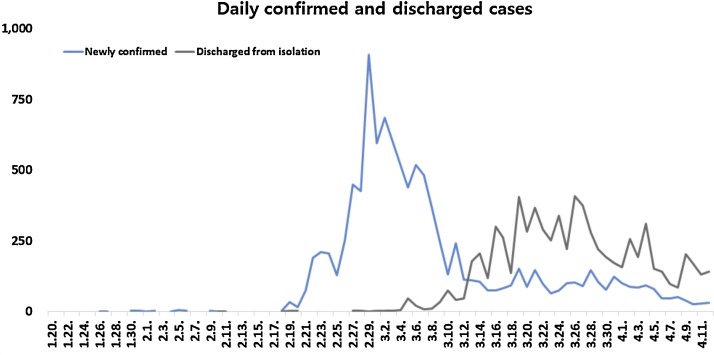
The development of a SARS-CoV-2 infection illustrates how rapidly the numbers increase (Fig. 1 ). The numbers went from two daily cases to 909 from 18 February to 29 February. As of 11 April 2020, a total of 10,480 confirmed cases and 211 deaths with a fatality rate of 2.0%, were reported. Extensive testing was applied to cases and contacts and a total of 510,479 tests or up to 18,000 per day were run to identify cases and contacts and quarantine them [Korean CDC 2020].
Fig. 1.
Korea. From Korean CDC (see KCDC, 2020a).
Based on the lessons learned from the MERS-CoV outbreak in 2015, Korea's Centers for Disease Control and Prevention (KCDC) intensified contact investigation and management of contacts with following measures: 1) interviewing patients and determining the location of contacts (patient route) with complementary methods including checking medical records, phone-based global positioning system (GPS), credit card transaction records and closed-circuit television (CCTV); 2) evaluation of the risk of exposure; 3) classification of contacts based on risk analysis and 4) management of contacts (Korean CDC 2020). KCDC shared the epidemiologic information with the public in a transparent manner. In order to effectively utilize health care resources, health authorities classified patients based on the severity using the categories of mild, moderate, severe and extremely severe. Mild cases were isolated and monitored in living quarters and treatment support centers. Moderate, severe and extremely severe cases were immediately hospitalized for treatment. Korea expanded special procedures to all travelers since 19 March and is requiring a 14-day self-quarantine or isolation in facilities for all travelers entering Korea from 1 April with symptom screening at point of entry and laboratory testing at point of entry or within three days upon arrival.
A public awareness campaign has been implemented, including personal hygiene practices such as hand washing and wearing a mask when visiting clinics or hospitals. In order to minimize the dense working environment, measures such as telecommuting, flexible work, monitoring of fever or respiratory symptoms for employees were implemented. On 21 March 2020, physical distancing measures were recommended up to 19 April, including limiting the operation of facilities of indoor sports and entertainment and replacement of religious gatherings with online ceremonies. School opening has been postponed and replaced by online education. Furthermore, in order to minimize the infection in the community, a collective quarantine system was established to prevent the spread of infection by early detection of patients in nursing homes and mental hospitals.
As of 11 April, Korea has flattened the epidemic curve without shutting down the country nor the cities at the epicenter of the outbreak, without imposing extreme personal travel or movement restrictions and without closing airports or taking other authoritarian actions [The Government of the Republic of Korea, 2020].
9. Singapore
Singapore was one of the most affected areas in the 2003 SARS outbreak. Since then, Singapore has steadily built up its outbreak preparedness, including developing a national pandemic preparedness plan based on risk assessment and calibration of response measures that are proportionate to the risk [Lee VJ et al., 2020]. This includes holding regular exercises as well as building the National Centre for Infectious Diseases (NCID), a 330-bed purpose-built infectious diseases management facility with integrated clinical, laboratory, and epidemiological functions.
Up to 27 March, Singapore had reported a total of 683 cases with 2 deaths. The ministry of health (MOH) had already developed a local case definition by 2 January 2020, and SARS-CoV-2 real-time polymerase chain reaction (RT-PCR) laboratory testing capacity was scaled up rapidly in all public hospitals in Singapore to handle 2,200 tests a day. All contacts were assessed by telephone for fever or respiratory symptoms by public health officials during the quarantine or monitoring period, thrice daily for close contacts and once daily for contacts at lower risk.
In late January 2020 the following groups were tested for SARS-CoV-2: 1) all hospitalized patients with pneumonia (later expanded to include patients with pneumonia evaluated in primary care settings); 2) ICU patients with possible infectious causes as determined by the physician; 3) patients with influenza-like illness at sentinel government and private primary care clinics included in the routine influenza surveillance network; and 4) deaths from possible infectious causes [Ng Y et al., 2020].
Despite the city-state's strict contact-tracing, quarantining, and travel restrictions, a second wave of infections, from returning residents and local transmission, saw cases spike from 100 to 10,000 in one month (South China Morning Post 3 April). The initial part of the second wave of infections involved Singapore residents returning from countries such as the United States and Britain. The second wave also includes an increasing number of locally transmitted infections and cases with no known links to confirmed patients. However, many cases were found to be linked to transmission among migrant workers living in crowded dormitories. In response to the second wave, the city-state introduced stricter physical distancing measures, barring the entry of all travelers, closing bars and nightlife, and eventually launching a strict lockdown in early April 2020 of schools, non-essential shops, places of worship, etc., all closed for a month because the number of locally transmitted cases routinely exceeded a hundred a day.
10. Hong Kong
In Hong Kong, the first imported case of COVID-19 was reported on 23 January 2020, two days before the Lunar New Year. From the last week of January 2020, the Government had ordered the closure of schools; most borders with Mainland China were closed from the first week of February. Between February and April, control measures were stepped up. Through new regulations introduced under the Prevention and Control of Diseases Ordinance (Cap 599), compulsory quarantine and physical distancing orders became enforced. The quarantine applies to all people, including local citizens entering Hong Kong. Physical distancing regulations include the prohibition of a gathering of more than four persons in public areas, restriction of the number of customers and the occupancy of food-catering premises, and closure of amusement game centers, bathhouses, fitness centers, bars, and other entertainment places. There is no legal restriction on workplaces, but the Government has, since late January, mandated work-from-home arrangements for civil servants. Of note, the vacating of workplaces affected not only the 170,000-member government staff-force but also employees of statutory bodies, non-government organizations as well as major businesses. As of 9 April, 974 confirmed cases of SARS-CoV-2 infection were reported in the 7-million population city, with four deaths [Government of Hong Kong, 2020]. About 60% were imported cases or their contacts while local transmission, especially the dormitories of migrant workers, accounted for the rest. Over half of the non-imported cases could be traced back to close contacts with reported local cases. There was a marked increase of daily reports from less than ten in January/February to 20-60 since the second half of March, which was attributed to the return of local citizens following the acceleration of the European outbreaks, and the scaling up of testing. The main local transmission clusters had occurred in a religious worship area and in social activities, including dinner gatherings and entertainment bars. Transmission linked to contacts in the workplace has so far been uncommon. Universal masking in public areas and on public transport is a common sighting, and in fact, forms part of their general hygiene advice. Such practice is required by law for staff and people patronizing catering premises, as stipulated in the newly enacted legal regulation. While the epidemic appeared to be less severe than in other cities/countries in the region, restrictions have continued to be tightened to guard against major outbreaks.
11. Taiwan
Taiwan enhanced its COVID-19 case discovery by proactively locating patients with severe respiratory symptoms (based on information from the National Health Insurance (NHI) database who had tested negative for influenza) and retesting them for COVID-19; they found 113 more cases. The toll-free number 1922 served as a hotline for citizens to report persons with suspicious symptoms or for possible cases to report themselves; as the disease progressed, this hotline has reached full capacity, so each major city was asked to create its own hotline as an alternative. At this time, it is not known how often this hotline has been used. The government addressed the issue of disease stigma and compassion for those affected by providing food, frequent health checks, and encouragement for those under quarantine. This rapid response included hundreds of action items.
Taiwan citizens’ household registration system and the foreigners’ entry card allowed the government to track individuals at high risk because of a recent travel history in affected areas. Those identified as high risk (under home quarantine) were monitored electronically through their mobile phones. On 30 January, the NHA database was expanded to cover the past 14-day travel history for patients from China, Hong Kong, and Macau. On 14 February, the Entry Quarantine System was launched, so travelers may complete a health declaration form by scanning a QR code that leads to an online form, either before departure from or upon arrival at a Taiwan airport. A mobile health declaration pass was then sent via SMS to phones using a local telecom operator, which allowed for faster immigration clearance for those with minimal risk. This system was created inside a 72-hour period. On 18 February, the government announced that all hospitals, clinics, and pharmacies in Taiwan would have access to patients’ travel histories.
12. South Africa
South Africa is an upper-middle-income economy with a population of approximately 59 million people and one of the highest inequality rates in the world. Critical concerns are the large population of people living in densely populated peri-urban areas under difficult social circumstances plus the high national prevalence of HIV and TB, which may interact with SARS-CoV-2 to cause more severe disease. Also, South Africa's health services are already overburdened with limited capacity to absorb a massive influx of COVID-19 patients.
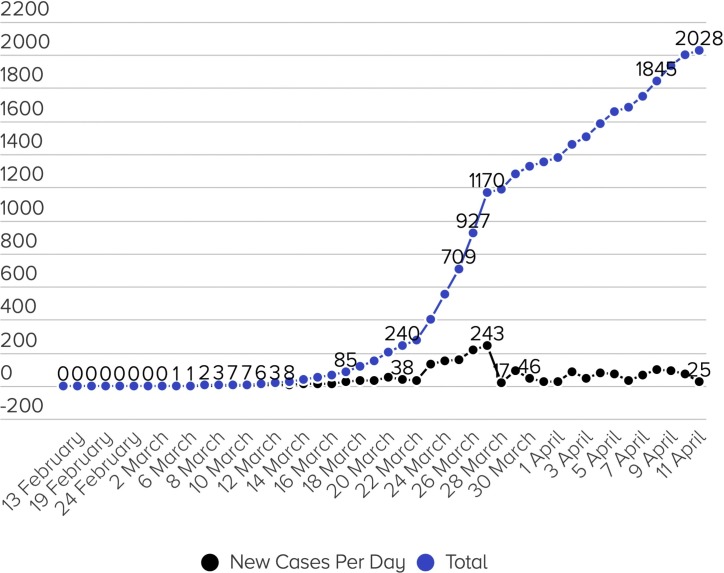
The first case of COVID-19 was detected on 5 March 2020 in a group of travelers from Italy, and the initial period of the epidemic was limited to imported cases and their contacts, occurring within a specific demographic of middle-class and relatively younger people. The Government responded rapidly, announcing a national state of disaster on 15 March after 61 confirmed cases had been reported with evidence of local transmission (Fig. 2 ). This initial public health response included travel bans from countries with high levels of community transmission and a 14-day mandatory quarantine for all returning travelers from those countries, school closures, cancellation of gatherings of more than 100 people, and expanding testing and quarantine capacity. One week after these measures were implemented, and after case numbers had grown six-fold to 402 cases, a strict national 3-week lockdown was initiated on 26 March, which prohibited all movement for citizens not involved in designated essential services except under strictly controlled circumstances, such as to seek medical care, buy food, medicine, and other supplies or collect a social grant. Despite the profound impact of the lockdown on an already tenuous economy - estimated reduction in growth by 2.6% translating into ∼9% contraction of national GDP - the President announced a 2-week extension on 9 April, following an apparent decrease in the average daily infection rate from 42% to 4%. Critical challenges for transitioning to a risk-based containment strategy in South Africa include limited testing capacity - currently, 75,000 tests have been performed; to match the per-capita testing of South Korea would require 400,000 tests - and a lack of infrastructure to implement contact tracing and isolation for people living in dense peri-urban environments.
Fig. 2.
Daily number of new cases in South Africa and cumulated number of cases. Confirmed COVID-19 cases in South Africa (12 April 2020). Source: https://www.coronapp.co.za/.
13. Conclusion
Each country has to decide how to open up its society for work and social activities. A study comparing health care systems in Hong Kong, Singapore, and Japan had three important conclusions [Legido-Quigley et al., 2020]. The first is that “integration of services in the health system and across other sectors amplifies the ability to absorb and adapt to shock.” The second is that “the spread of fake news and misinformation constitutes a major unresolved challenge. Finally, “the trust of patients, healthcare professionals, and society as a whole in the government is of paramount importance for meeting health crises.” While the surge of cases in these three countries may have altered the analysis somewhat, the general principles still apply.
This is a new infection spreading in a nonimmune population, and we have no reference manual–still, we have to make decisions. Measures that can be used are summarized in Table 4 . As each country chooses its own path, we can learn from each other to determine the optimum approach that works in our setting.
Table 4.
Principles can help countries to plot a way out of the shutdown.
| 1. | Consider easing restrictions when the case count has decreased after the peak, has been stable for two weeks, and the hospitals can cope with the number of severe cases. Cases must be staged into imported, linked to known clusters and cases and unknown sources. |
| 2. | Expand testing for new and past infections by setting up strategic testing sites, introduce testing stations in the community providing diagnostic tests to everyone with compatible symptoms and serological testing for surveillance of population immunity. Introduce point-of-care (POC) testing when validated tests become available. |
| 3. | Consider testing employees with nucleic acid tests and/or antibody tests before returning to work to find silent cases and recovered persons. This can also be applied to schools. In collaboration with the occupational health service, establish sustainable workplace policies emphasizing infection control. |
| 4. | Consider imposing the use of surgical or non-medical face masks whenever outside the household to reduce the risk that those persons with an unrecognized infection will contribute to transmission. This must be an adjunct to other ongoing physical distancing interventions and hand hygiene. |
| 5. | Continue to impose quarantine on arriving passengers from countries with active outbreaks. Aim to develop a travel certificate for people with documented immunity with SARS-CoV-2-specific antibodies to be exempt from quarantine rules. |
| 6. | Maintain strong infection prevention measures in all health care institutions. |
| 7. | The SARS-CoV-2 virus will most probably be in our societies for a long time until we have a vaccine. Flare-ups, small outbreaks, and clusters are expected, and thus public health care system must be refurbished to take care of new cases, rapidly perform contact follow-up, and ensure quarantine. Therefore, a permanent upgrade of the public system is needed. |
Funding
The study received no funding
All authors contributed equally to the text.
References
- Chan K.H., Yuen K.Y. COVID-19 epidemic: disentangling the re-emerging controversy about medical facemasks from an epidemiological perspective. Int J Epidemiol. 2020:31. doi: 10.1093/ije/dyaa044. March [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y., Sridhar S., Chan J.F.W., Ho P.L., Yuen K.Y. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020:5. doi: 10.1017/ice.2020.58. March [ePub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan J., Liu X., Pan W., Douglas M.W., Bao S. Epidemiology of 2019 Novel Coronavirus Disease-19 in Gansu Province. China, 2020. Emerg Infect Dis. 2020;26:6. doi: 10.3201/eid2606.200251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Hong Kong. https://chp-dashboard.geodata.gov.hk/covid-19/en.html (Accessed 12 April 2020).
- Guardian The Lombardy insists on face masks outside homes to stop Covid-19. Angela Giuffrida in Orvieto and Peter Beaumont. https://www.theguardian.com/world/2020/apr/05/lombardy-insists-on-face-masks-outside-homes-to-stop-covid-19 (Accessed 8 April 2020).
- Korea Centers for Disease Control and Prevention. Middle East Respiratory Syndrome Coronavirus Outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect 2015; 6:269-278. [DOI] [PMC free article] [PubMed]
- Korea Center for Disease Control and Prevention. The updates of the COVID-19 in the Republic of Korea. 11 April 2020a. https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 (Accessed 12 April 2020).
- Korea Center for Disease Control and Prevention. COVID-19 National Emergency Response Center, Epidemiology and Case Management Team. Contact Transmission of COVID-19 in South Korea: Novel Investigation Techniques for Tracing Contacts. Osong Public Health Res Perspect 2020b; 11(1):60-63. [DOI] [PMC free article] [PubMed]
- Korea Center for Disease Control and Prevention. Guideline for COVID-19 Response. 2 April 2020a.
- Lee V.J., Chiew C.J., Khong W.X. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. Journal of Travel Medicine. 2020 doi: 10.1093/jtm/taaa039. 13 March. pii: taaa039. doi: 10.1093/jtm/taaa039. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legido-Quigley H., Asgari N., Teo Y.Y., Leung G.M., Oshitani H., Fukuda K., Cook A.R., Hsu L.Y., Shibuya K., Heymann D. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395:848–850. doi: 10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung C.C., Lam T.H., Cheng K.K. Mass masking in the COVID-19 epidemic: people need guidance. Lancet. 2020;395:945–950. doi: 10.1016/S0140-6736(20)30520-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung K., Wu J.T., Liu D., Leung G.M. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. 2020 doi: 10.1016/S0140-6736(20)30746-7. Apr 8. pii: S0140-6736(20)30746-7. doi: 10.1016/S0140-6736(20)30746-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo I.L., Lio C.F., Cheong H.H., Lei C.I., Cheong T.H., Zhong X. Evaluation of SARS-CoV-2 RNA shedding in clinical specimens and clinical characteristics of 10 patients with COVID-19 in Macau. Int J Biol Sci. 2020;16:1698–1707. doi: 10.7150/ijbs.45357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng Y., Li Z., Chua Y.X., Chaw W.L., Zhao Z. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore — 2 January–29 February 2020. Morbidity and Mortality Weekly Report. 2020;69(11):307–311. doi: 10.15585/mmwr.mm6911e1. doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh M.D., Park W.B., Park S.W., Choe P.G., Bang J.H., Song K.H., Kim E.S., Kim H.B., Kim N.J. The Korean Middle East Respiratory Syndrome Coronavirus outbreak and our responsibility to the global scientific community. Korean J Intern Med. 2018;33:233–246. doi: 10.3904/kjim.2018.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen E., McCloskey B., Hui D.S., Kock R., Ntoumi F., Memish Z.A. COVID-19 travel restrictions and the International Health Regulations–call for an open debate on easing of travel restrictions. Intl J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.04.029. 13 April in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petherick A. Developing antibody tests for SARS-CoV-2. Lancet. 2020;395:1101–1102. doi: 10.1016/S0140-6736(20)30788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Government of the Republic of Korea. Tackling COVID-19. Health, Quarantine and Economic Measures: Korean Experience. 31 March 2020. http://english.moef.go.kr/pc/selectTbPressCenterDtl.do?boardCd = N0001&seq = 4868.
- Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA. 2020:3151. doi: 10.1001/jama.2020.3151. 3 March. doi: 10.1001/jama.2020. [DOI] [PubMed] [Google Scholar]
- WHO. International Health Regulation. Geneva 2005. https://www.who.int/ihr/about/en/(Accessed 2 April 2020).
- WHO. Operational considerations for case management of COVID-19 in health facility and community. Interim guidance. Geneva. 19 March 2020a. https://apps.who.int/iris/bitstream/handle/10665/331492/WHO-2019-nCoV-HCF_operations-2020.1-eng.pdf (Accessed 10 April 2020).
- WHO . 2020. Situation Report-72. 1 April 2020b. (https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200401-sitrep-72-covid-19.pdf?.sfvrsn=3dd8971b_2. (Accessed 2 April) [Google Scholar]
- WHO. Advice on the use of masks in the context of COVID-19. Interim guidance. Geneva, 6 April 2020c. https://apps.who.int/iris/bitstream/handle/10665/331693/WHO-2019-nCov-IPC_Masks-2020.3-eng.pdf?sequence=1&isAllowed=y (Accessed 12 April 2020).
- WHO. Coronavirus disease (COVID-19) technical guidance: Infection prevention and control/WASH. Collection of documents. Geneva 2020d. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control (Accessed 12 April 2020).
- World Trade Organization, WTO. Trade set to plunge as COVID-19 pandemic upends global economy. https://www.wto.org/english/news_e/pres20_e/pr855_e.htm. 8 April 2020 (Accessed 8 April 2020).
- Zhang J., Litvinova M., Wang W., Wang Y., Deng W., Cen X. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modeling study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30230-9. online 2 April. DOI:https://doi.org/10.1016/S1473-3099(20)30230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwald M.L., Lin W., Sondermeyer Cooksey G.L., Weiss C., Suarez A., Fischer M. Rapid Sentinel Surveillance for COVID-19 — Santa Clara County. California. 2020;69:3. doi: 10.15585/mmwr.mm6914e3. March MMWR2020April–early release. [DOI] [PMC free article] [PubMed] [Google Scholar]