Abstract
Objective
To analyze the relationship between the length from injury to first debridement (LFITFD) of open tibial fractures and perioperative infection, and explore independent risk factors related to infection.
Methods
This retrospective study focused on 215 clinical patients with open tibial fractures who were admitted from January 2012 to January 2017. According to the time from injury to the operation, the patients were categorized into four groups: LFITFD ≤ 6 h, 6 < LFITFD ≤ 12 h, 12 < LFITFD≤24 h, and (LFITFD > 24 h). Infection risk factors were screened by univariate analysis, and multivariate logistic regression analysis was used to determine independent risk factors.
Results
The infection rates of four groups were 9.2%, 9.5%, 11.1%, and 10.5% with six of 65, nine of 95, four of 36, and two of 19 patients being infected, respectively. There was no statistical significance between the four groups. The infection rates among fractures of different Gustilo–Anderson classifications were as follows. Of 62 cases of type I fractures, two were infected, and the infection rate was 3.2%. Among those with type II fractures, eight were infected, and the infection rate was 8.2%. Three of 26 cases of type IIIA fracture were infected, yielding an infection rate of 11.5%, seven of 25 cases of type III B fracture were infected (28% infection rate), and one of four cases of type III C fracture was infected (25% infection rate). There was a statistically significant difference between the five groups. Multivariate regression analysis showed that smoking, combined diabetes, surgical time, and fracture Gustilo–Anderson classification were independent risk factors for perioperative infection of open tibial fractures, and the difference in time from injury to first debridement was not related to infection.
Conclusion
The incidence of perioperative infection in patients with open tibial fractures has little to do with the time of the first debridement, which is mainly related to the level of the fracture's Gustilo–Anderson classification. At the same time, smoking is prohibited before the operation, the patient's blood glucose is managed, and the debridement operation time is minimized conducive to reducing the incidence of infection.
Keywords: Debridement time, Infection rate, Gustilo–Anderson classificationTibia
Introduction
With the rapid development of society and the economies, open fractures of the limbs caused by various trauma factors are increasing, and the incidence of open tibia fractures is the highest among all open fractures1. An open fracture refers to the connection between the fracture and the external environment; open fractures are often caused by violent, high‐energy trauma, such as car accidents, falling from a significant height, bruises, or damage from farming tools. It is often accompanied by severe damage to the skin, soft tissues, muscles, blood vessels and nerves2. Injury assessment is needed, and damage control is performed in severe cases. The biggest risk of open fractures is severe tissue damage and wound contamination, which can easily cause bone and soft tissue necrosis and infection. In severe cases, it can cause limb dysfunction and multiple organ failure.
The latest data show that the infection rate after internal fixation of a closed fracture is 1%, whereas open fractures carry a risk of infection ranging from 15% to 55% in very severe cases3, 4, 5. Early debridement has been considered a key factor in preventing postoperative infections in patients with open fractures. The traditional perspective dictates that the time after injury determines whether it is feasible to debride an open fracture. In 1898, German physician Friedrich proposed the “6 h rule” for debridement based on the results of basic research. In summary, this principle claimed that it was feasible to treat an injury if the debridement occurs less than 6 h after the initial injury. If one‐stage closure of wounds occurs 6–24 h after injury, there is a risk of contracting a bacterial infection, so debridement must be deliberately used. However, if the time after injury is >24 h, debridement is not recommended due to bacterial multiplication. In a clinical setting, several objective factors will delay the timing of debridement in emergency surgery, such as the delay in delivery, the unstable condition of the patient, and urgent treatment of other combined injuries. Therefore, it is difficult to effectively debride some patients within 6 h after injury. Some other conditions unrelated to the patient's condition, such as the occupation of the operating room or time required for pre‐operative preparation, often result in the first debridement not being performed within approximately 6–8 h of the injury. According to foreign scholars, it is estimated that more than 40% of patients with open tibial fractures are delayed after the first debridement6, 7, and the time after the first debridement is more than 6 h after the injury. However, the postoperative infection rate did not significantly increase, and fractures healed better than those of patients who were treated sooner. The latest study comes from a systematic review by Schenker et al. in which a total of 16 studies including 3539 patients with open fractures and a subgroup analysis of various types of fractures were considered to have no statistically significant difference in debridement infection rates within 6 h and 6 h later (P > 0.05)8.
However, it is unknown whether delayed debridement will significantly increase the postoperative infection rate among patients with open fractures. Furthermore, the results of delayed debridement are unclear9. The purpose of this study is as follows: (i) to analyze the relationship between the timing of the first debridement of open tibial fractures and perioperative infection, and explore independent risk factors related to infection; and (ii) to contribute information and recommendations on the management of open tibial shaft fractures when the time to surgical debridement is >6 h.
Materials and Methods
Inclusion Criteria and Exclusion Criteria
Inclusion criteria included the following: (i) patients with open tibial fracture injury time, first debridement time, and complete prognosis data; (ii) hospital stay longer than 2 weeks; and (iii) patients followed for more than 10 weeks.
Exclusion criteria included: (i) patients with multiple open fractures; (ii) patients with amputated open fractures; and (iii) patients with hyperthyroidism and hematological diseases.
Surgical Methods
Emergency Treatment
Upon arrival at the emergency department, patients were treated according to the established Advanced Trauma Life Support protocol guidelines and basic orthopaedics fracture management protocol, including performing complete imaging studies. When visiting the emergency department of a patient, first observe the wound (take pictures of the wound, avoid repeated examination of the wound during treatment), cover the wound with a sterile dressing, and do not rinse the wound in the emergency room to avoid contamination of deep tissues8. Urgently improve preoperative examination and arrange emergency surgery, the initial fracture management consisted of obtaining a focused history of the patient and performing a comprehensive physical examination, hemostasis, programmed sedation and analgesia, temporary fixation of fractures, administration of intravenous antibiotics (given to all patients within 3 h of injury), and tetanus prophylaxis. All patients were kept under general anesthesia during the procedure.
Initial Debridement
During the initial debridement process, the area of injury was washed with hydrogen peroxide and physiological saline. According to the different types of wounds and degree of fracture exposure, open fractures were classified according to the Gustilo–Anderson system. At least 3 L of type I injury was washed, whereas at least 9–11 L of types II and III injuries are rinsed10, 11. Cover the open wound with sterile gauze and then soak it in Amr iodine solution for about 10 minutes. We unify the expansion and extend along the longitudinal axis of the limb to reveal deep wounds that will damage the blood supply or clean the necrotic soft tissue and remove the free bone.
Fracture Fixation
After debridement is complete, the appropriate fixation method was selected according to the classification of the patient's open fracture. Type I open fractures, in the case of adequate debridement and good soft tissue coverage, are regarded as closed fractures, are fixed for a period of time, and the wound is closed. For type II and type III open fractures, the physician selected the appropriate fixation method according to the actual situation of the patient, adopted the principle of staged treatment, and performed the external fixation after the initial debridement, or simultaneously performed limited internal fixation (open fracture of the tibia). The fibula was fixed by internal fixation to maintain the length of the limb, and the tibia was fixed by external fixation. The wound was closed with vacuum sealing drainage (VSD) negative pressure drainage. After the soft tissue of the wound was stabilized, the wound was closed as soon as possible, and the internal fixation was replaced during the second stage12.
Postoperative Treatment and Follow‐Up
Postoperative Treatment
After taking the culture in the emergency room, we routinely gave cefuroxime 1.5 g Q8 h until debridement started, and debridement started with cefuroxime 1.5 g for 72 h or until the wound was closed. Postoperative prophylactic use of antibiotics was performed according to AO “Antibiotics Guidelines.” Gustilo type I and II fractures were treated with first‐ or second‐generation cephalosporins for no more than 24 h. Gustilo type III fractures were treated with third‐generation cephalosporins, amoxicillin‐clavulanate potassium or ampicillin‐sulbactam for no more than 3 days. For the third‐generation cephalosporin plus metronidazole, acesulfame‐tazobactam or carbon blue for potential fecal contamination fractures13, 14, 15.
The wound condition was closely observed and VSD was changed in the operating room for approximately 3–5 days until the wound could be closed. The medicine was changed 3 days later, and the wound condition was observed. Abnormal secretions were immediately taken for routine bacterial culture. If the bacterial culture test yielded positive results, drug susceptibility tests were performed to determine the appropriate antibiotics for treating the infection.
The recovery of the postoperative wound was observed. If redness, swelling, or sinus secretions were observed around the wound, white blood cell, C‐reactive protein, PCT, procalcitonin, and erythrocyte sedimentation rate were measured. These factors were considered possible indicators for an infection16, 17. Furthermore, a positive bacterial culture test for secretions from the patient's wound was highly suggestive of infection. The culture test results combined with histopathological examination was used to diagnose infection.
Definition of Fracture Infection and Follow‐Up
Definition of fracture infection: bone tissue infection caused by pathogenic microbial contamination or patient's low autoimmunity after contact with implants, with or without surrounding soft tissue infection after fracture internal fixation. We counted all infections that occurred in different time periods of open tibia fractures. The follow‐up time was more than 10 weeks. There were early infections (<2 weeks), delayed infections (2–10 weeks), and chronic infections (>10 weeks). There was an incidence of nonunion in all open tibia fractures18.
Observation Indicators
Injury Severity Score (ISS) and Abbreviated Injury Scale (AIS)
ISS is the gold standard for multiple injury scoring. It can be used to evaluate the treatment effect of trauma patients, predict the recovery time, estimate the treatment cost and the length of hospital stay. There are some general principles for calculating ISS. This method divides the human body into six regions. ISS is the sum of the squares of the highest AIS values in the three most severely injured regions of the body, that is, ISS = AIS12 + AIS22 + AIS32. ISS scoring method: divide the human body into six anatomical regions, the body surface, head and neck, face, chest, abdomen, limbs, and pelvis. Take the sum of the squared AIS scores of the three most severe injuries. The higher the total score, the heavier the injury, the worse the prognosis, and the higher the mortality rate. The total score >10 points should be hospitalized19.
Debridement Time Grouping and Time to Surgery
Dividing patients into four groups based on time from initial injury to first debridement: LFITFD ≤ 6 h, 6 h < LFITFD ≤ 12 h, 12 h < LFITFD ≤ 24 h, LFITFD > 24 h. This grouping can study the relationship between the time of the first debridement and postoperative infection.
Gustilo‐Anderson Classification
Type I: skin wound <1 cm, clean, simple fracture type; Type II: skin wounds >2 cm, soft tissue damage is not extensive, no flaps and avulsions, simple fracture types; Type IIIA: bone has sufficient soft tissue coverage despite extensive soft tissue destruction; Type IIIB: extensive soft tissue injury with periosteal detachment, exposed bone tissue, severe wound contamination; Type IIIC: open fracture with arterial injury requiring repair20. It can reflect the degree of open fracture injury, provide a reference for clinical treatment, evaluate the infection risk after open fracture debridement treatment, evaluate the infection risk after open fracture debridement treatment, and facilitate academic communication.
Comorbidities
Patient's lifestyle and combined medical diseases. Poor lifestyle habits such as smoking and drinking, and medical conditions such as diabetes and malnutrition, can all lead to infections.
Transfusion
Patients with open fractures lose more blood, and hemoglobin will decrease, resulting in insufficient blood supply to local tissues, increasing the risk of postoperative infection.
Fracture Location
Tibial fractures are generally divided into upper, middle, and lower segments. The blood flow in each part of the bone tissue is different, and the occurrence of infection may also be different.
Statistical Analysis
All statistical analyses were performed using IBM SPSS statistics version 22.0 (SPSS, Chicago, IL, USA). Taking the postoperative infection as the dependent variable and each observation index as the independent variable, single‐factor and multi‐factor analyses were performed using binary logistic regression analysis. A single factor analysis was performed for each observation index, and variables with statistical significance or no statistical significance but with a significant trend (P < 0.1) were included in the multivariate logistic regression analysis model, test level α = 0.05. For categorical variables, the data between groups were compared using the χ 2‐test and Fisher's exact test. For quantitative variables, the data between groups were expressed as mean ± SD, and compared by t‐test or rank sum test for statistical analysis. A value of P < 0.05 indicated a statistically significant difference.
Results
General Results
This case study was performed in the department of orthopaedic surgery of a single institution. Data from patients with open tibial fractures who were treated from January 2012 to January 2017 were retrospectively analyzed using an electronic medical database. We identified a total of 215 patients aged ≥18 years who sustained isolated open tibial shaft fractures (Gustilo‐Anderson type I–III), including 117 men and 98 women, aged 35 to 58 years, with an average age of 48.5 ± 3.6 years. All patients were divided into four groups based on the time from injury to first debridement: LFITFD ≤ 6 h, 6 h < LFITFD ≤ 12 h, 12 h < LFITFD ≤ 24 h, LFITFD > 24 h. The basic information of the patients is shown in Tables 1 and 2.
Table 1.
Demographic characteristics of the study population by patient
| Demographic variables | Data |
|---|---|
| Number of patients | 215 |
| Age (Mean ± SD, years) | 48.5 ± 3.6 |
| Gender (Males, %) | 117 (54%) |
| Mechanism | |
| MVA (%) | 76 (35%) |
| Fall (%) | 71 (33%) |
| Industrial (%) | 33 (15%) |
| Pedestrian versus car (%) | 35 (17%) |
| Energy level | |
| Low (%) | 62 (29%) |
| Moderate (%) | 98 (46%) |
| High (%) | 55 (25%) |
|
Injury Severity Score (Mean ± SD [range]) |
16 ± 11 (4–50) |
| Comorbidities | |
| Tobacco (%) | 84 (39%) |
| Alcohol (%) | 52 (24%) |
| Diabetes (%) | 22 (10%) |
| Malnutrition, albumen ≦ 3.0 g/dL (%) | 26 (10%) |
| Debridement time grouping | |
| LFITFD ≦ 6 h (%) | 65 (30%) |
| 6 h < LFITFD ≦ 12 h (%) | 95 (44%) |
| 12 h < LFITFD ≦ 24 h (%) | 36 (17%) |
| LFITFD > 24 h (%) | 19 (9%) |
| Time to operating room (Mean ± SD [range]; hours) | 5.6 ± 7.2 (0.8–59.8) |
| Transfusions (Mean ± SD [range]; number) | 4.5 ± 3.2(0–10) |
| Follow‐up | |
| PCP (Mean ± SD [range]; days) | 486 ± 312 (97–1374) |
| Orthopedics (Mean ± SD [range]; days) | 354 ± 260 (97–1374) |
MVA, motor vehicle accident; PCP, primary care provider.
Table 2.
Demographic characteristics of the patients by fracture
| Fracture | Number |
|---|---|
| Number of fractures Gustilo classification | 215 |
| I (%) | 62 (29%) |
| II (%) | 98 (46%) |
| IIIA (%) | 26 (12%) |
| IIIB (%) | 25 (11%) |
| IIIC (%) | 4 (2%) |
| Fracture location | |
| Proximal (%) | 48 (22%) |
| Midshaft (%) | 74 (34%) |
| Distal (%) | 93 (43%) |
| Outcome | |
| Healed (%) | 143 (66%) |
| Nonunion (%) | 51 (24%) |
| Infected (%) | 21 (10%) |
Perioperative Infection Results
Of 215 patients were enrolled, 21 had postoperative infections, thus yielding an overall postoperative infection rate of 9.8%. The infection rate of LFITFD ≤ 6 h was 9.2%, with six of 65 patients being infected. The infection rate of 6 h < LFITFD ≤ 12 h was 9.5%, with nine of 95 patients being infected. In 12 h < LFITFD ≤ 24 h, the infection rate was 11.1% (four of 36 total cases), and in LFITFD > 24 h the infection rate was 10.5% (two of 19 total cases). The postoperative infection rate of the four groups showed an overall upward trend with the delay of the first time of debridement, which was consistent with the principle of early debridement of patients with open fractures. However, the increase in the rate of infection between the four groups was not statistically significant (Table 3).
Table 3.
Comparison of postoperative infections in four groups of patients
| Group | Infection | X 2/t‐value | P value | |||
|---|---|---|---|---|---|---|
| Yes | No | Overall | Ratio (%) | Fisher | ||
| LFITFD ≦ 6 h | 6 | 59 | 65 | 9.20 | 0.117 | 0.99 |
| 6 h < LFITFD ≦ 12 h | 9 | 86 | 95 | 9.50 | ||
| 12 h < LFITFD ≦ 24 h | 4 | 32 | 36 | 11.10 | ||
| LFITFD > 24 h | 2 | 17 | 19 | 10.50 | ||
| Overall | 21 | 194 | 215 | 9.80 | ||
LFITFD, Length from injury to first debridement.
Infection rates were also compared among injuries of different Gustilo‐Anderson classifications. Among type I cases, the infection rate was 3.2% (2/62 cases) and the infection rate among type II cases was 8.2% (8/98 cases). Among type IIIA cases, the infection rate was 11.5% (3/26 cases), the infection rate was 28% among type IIIB cases (7/25 cases), and it was 25% among type IIIC cases (1/4 cases). By comparing the postoperative infection rates of different Gustilo fracture types, it was determined that the postoperative infection rate significantly increased with increased severity of the fracture (Table 4).
Table 4.
Comparison of Gustilo typing infections in different fractures
| Group | Infection | X 2/t‐value | P value | |||
|---|---|---|---|---|---|---|
| Yes | No | Overall | Ratio (%) | (Fisher) | ||
| I | 2 | 60 | 62 | 3.2 | 13.872 | 0.008 |
| II | 8 | 90 | 98 | 8.2 | ||
| III A | 3 | 23 | 26 | 11.5 | ||
| III B | 7 | 18 | 25 | 28 | ||
| III C | 1 | 3 | 4 | 25 | ||
| Overall | 21 | 194 | 215 | 9.8 | ||
Results of Infection at Different Time Periods
For fractures debrided in the 0‐to‐6‐h period, the overall infection rates were 4.5%, 7.4%, and 18.8% for Gustilo‐Anderson type I, II, and III injuries, respectively. For fractures debrided in the 6‐to 12‐h period, the overall infection rates were 4.2%, 6.7%, and 19.2% for Gustilo‐Anderson type I, II, and II injuries, respectively. For fractures debrided in the 12‐to‐24‐h period, the overall infection rates were 8.3%, 7.1%, and 20% for Gustilo‐Anderson type I, II, and III injuries, respectively. For fractures debrided after 24 h, total infection rates for type I, II, and III injuries were 0%, 8.3%, and 33.3%, respectively (Figs 1, 2, 3, 4). When we compared the infection rates for patients who underwent debridement between 0 and 6 h after injury to patients who underwent debridement later (>6 h), no statistically significant differences were found (P = 0.861).
Figure 1.
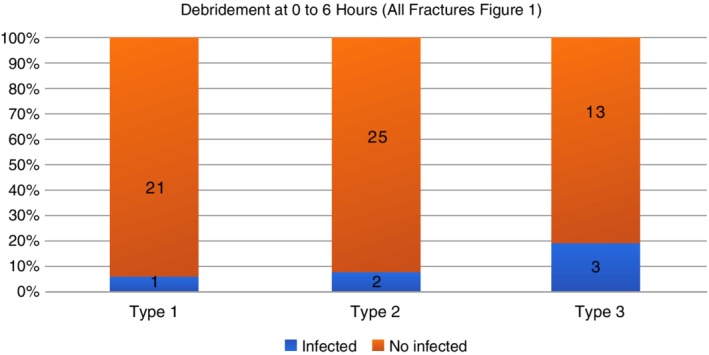
The proportion of infected and non‐infected patients with Type 1, Type 2, and Type 3 (Gustilo I, Gustilo II, and Gustilo III) fractures from 0 to 6 h from injury to first debridement.
Figure 2.
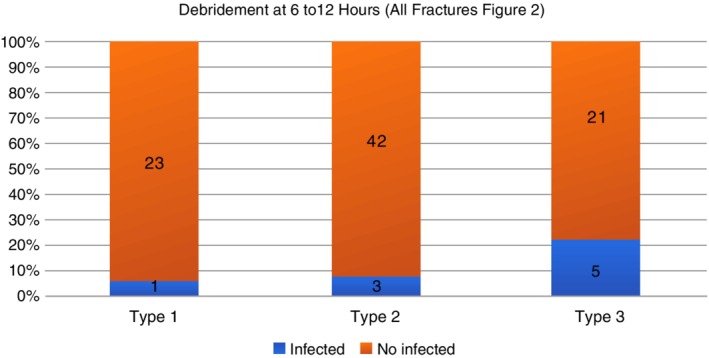
The proportion of infected and non‐infected patients with Type 1, Type 2, and Type 3 (Gustilo I, Gustilo II, and Gustilo III) fractures from 6 to 12 h from injury to first debridement.
Figure 3.
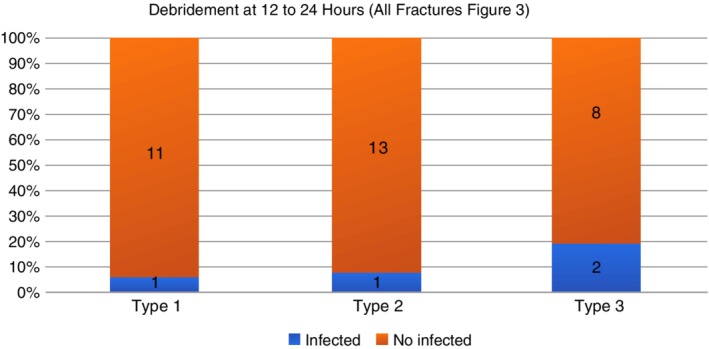
The proportion of infected and non‐infected patients with Type 1, Type 2, and Type 3 (Gustilo I, Gustilo II, and Gustilo III) fractures from 12 to 24 h from injury to first debridement.
Figure 4.
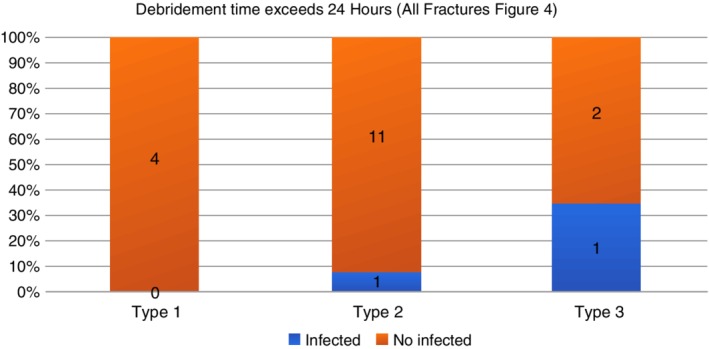
The proportion of infected and non‐infected patients with Type 1, Type 2, and Type 3 (Gustilo I, Gustilo II, and Gustilo III) fractures more than 24 h from injury to first debridement.
Risk Factors of Perioperative Infection in Patients with Open Tibial Fractures
Outcome of Univariate Analysis
Univariate analysis showed that there were no significant differences between the infected and non‐infected groups in terms of gender, age, injury severity score, drinking history, malnutrition, blood transfusion history, fracture location, and timing of first debridement (P > 0.05) (Table 5). Compared with the non‐infected group, the infected group had a history of tobacco use and diabetes, a longer operation time, and a higher Gustilo‐Anderson classification of fractures. The difference was statistically significant (P < 0.05) (Table 5).
Table 5.
Results of the univarite analysis of predictors of infection
| Variable | Infection | No infection | F value | P value |
|---|---|---|---|---|
| Number of patients | 21 | 194 | — | — |
| Age (Mean [SD]) | 49.5 (17.5) | 47.8 (18.4) | 0.960 | 0.780 |
| Gender | ||||
| Male (%) | 12 (10%) | 105 (90%) | 0.070 | 0.792 |
| Female (%) | 9 (9%) | 89 (91%) | ||
| Injury Severity Score (Mean [SD]) | 15.6 (9.1) | 16.0 (10.7) | 0.970 | 0.890 |
| Tobacco use | ||||
| Yes (%) | 13 (15%) | 71 (85%) | 5.098 | 0.024 |
| No (%) | 8 (6%) | 123 (94%) | ||
| Alcohol use | ||||
| Yes (%) | 6 (12%) | 46 (88%) | 0.244 | 0.621 |
| No (%) | 15 (9%) | 148 (91%) | ||
| Diabetes | ||||
| Yes (%) | 6 (27%) | 16 (73%) | 8.521 | 0.004 |
| No (%) | 15 (8%) | 178 (92%) | ||
| Malnutrition | ||||
| Yes (%) | 5 (19%) | 21 (81%) | 3.005 | 0.083 |
| No (%) | 16 (8%) | 173 (92%) | ||
| Time to surgery (Mean [SD]) | 11.3 (3.2) | 8.6 (4.5) | 0.780 | 0.440 |
| Transfusion | ||||
| Yes (%) | 3 (6%) | 47 (94%) | 1.049 | 0.306 |
| No (%) | 18 (11%) | 147 (89%) | ||
| Fracture location | ||||
| Proximal (%) | 3 (6%) | 45 (94%) | 1.049 | 0.306 |
| Midshaft (%) | 5 (7%) | 69 (93%) | ||
| Distal (%) | 13 (14%) | 80 (86%) | ||
| Operation time (Mean [SD]) | 139.4 (16.0) | 122.2 (16.7) | 6.985 | 0.014 |
| Gustilo classification | ||||
| I | 2 | 60 | 13.872 | 0.008 |
| II | 8 | 90 | ||
| III A | 3 | 23 | ||
| III B | 7 | 18 | ||
| III C | 1 | 3 | ||
| Debridement time grouping | ||||
| LFITFD ≦ 6 h | 6 | 59 | 0.117 | 0.990 |
| 6 h < LFITFD ≦ 12 h | 9 | 86 | ||
| 12 h < LFITFD ≦ 24 h | 4 | 32 | ||
| LFITFD > 24 h | 2 | 17 | ||
LFITFD, Length from injury to first debridement.
Outcome of Multivariate Logistic Regression Analysis
Multivariate logistic regression analysis showed that tobacco use history, combined diabetes, surgical time, and fracture Gustilo‐Anderson classification were independent risk factors for perioperative infection of open tibial fractures (Table 6).
Table 6.
Results of multivariate analysis of independent predictors of infection using the multiple GEE regression model
| Variable | Estimate | SE | OR | Wald | 95% CI | P value |
|---|---|---|---|---|---|---|
| Operation time | 0.065 | 0.026 | 1.067 | 6.425 | 1.015–1.122 | 0.011 |
| Tobacco use | 1.219 | 0.729 | 3.383 | 2.793 | 0.810–14.130 | 0.045 |
| Diabetes | 2.405 | 1.017 | 11.076 | 5.594 | 1.510–15.360 | 0.018 |
| Gustiloclassification | 2.060 | 0.600 | 7.850 | 3.605 | 2.410–25.590 | 0.001 |
Discussion
The relationship between the time of the first debridement and infection rate for open fractures has been the focus of debate among trauma specialists. Some scholars21, 22 believe that debridement within 6 h of open fractures reduces the chance of infection to a certain extent. Other reports23, 24, 25 state that debridement within 6 h is a practice that is inherited from traditional use, and delaying debridement may not increase the infection rate of open fractures. The 6‐h debridement principle is no longer followed for treating late‐stage infections in open fractures. Through this study, it was found that the occurrence of fracture infection was more related to fracture Gustilo classification, tobacco use, combined medical diseases, operation time, bacteriological factors, and antibiotic use.
There are no previously published studies showing whether there is an increase in infection if the first debridement time exceeds 24 h after the injury. We analyzed the general clinical data from 215 patients with open fractures of the tibia and included the first debridement time of more than 24 h to explore whether delayed debridement of open tibial fractures leads to an increase in infection rate. The infection rates for patients in groups A, B, C, and D were 9.2%, 9.5%, 11.1%, and 10.5%, respectively. By comparing the infection rates, it was found that with the delay of the first debridement time, the increase in infection rate was not statistically significant (P < 0.05). This finding suggests that delayed debridement does not necessarily lead to an increase in infection rate, and the time from the patient's injury to the first debridement may not be a risk factor for infection. Our research found that, in addition to thorough debridement and reasonable fixation of fractures and treatment of wounds, debridementis mainly related to the level of Gustilo's fracture of patients, the length of debridement, smoking, and whether they are associated with diabetes.
It has been reported26, 27, 28 that Gustilo‐Anderson type is significantly associated with the occurrence of open fracture infection. The higher the classification of the fracture, the higher the rate of infection and fracture nonunion. To this end, the authors studied the relationship between open fractures of the tibia and postoperative infection according to different types of fractures. According to the literature1, the infection rates of open fractures type I, II, IIIA, IIIB, and IIIC were 2%, 2%–10%, 5%–10%, 10%–50%, and 25%–50%, respectively. In our study, the overall infection rate for open tibial fractures was 9.8%. The infection rates for type I, II, IIIA, IIIB, and IIIC open tibial fractures were 3.2%, 8.2%, 11.5%, 28%, and 25%, respectively. These results were consistent with previous findings in the literature. The difference between the five groups was statistically significant, suggesting that there is a significant correlation between the postoperative infection rate and the severity of the fracture in patients with open fractures of the tibia. Because the severity of fractures is different, severity of soft tissue injury at the site of the fracture is also different. The difference in soft tissue injury can be manifested in the difference in wound size, skin, muscle damage, vascular damage, bone tissue damage, and pollution level. The conditions under which wounds invade tissues are different, and may lead to differences in postoperative infection rates. A study by Lua et al.29 show that the incidence of infection‐related complications in patients with Gustilo type III tibia open fractures is 3.72 times that of patients with Gustilo types I/II. In addition, the higher the severity of the fracture, greater is the wound damage to the surrounding soft tissue and more serious the pollution. The boundary of early necrosis of soft tissue is unclear, which may lead to incomplete debridement and increase the infection rate.
Due to the long‐term neurovascular disease in diabetic patients and the stress of surgery, the ischemia and hypoxia in the operation area are further aggravated, and the postoperative area is more likely to be unhealed and even infected. Studies30 have shown that the postoperative infection rate of patients with fractures with diabetes reaches 10%–60%. In previous studies31, 32, a long operation time indicated a slow healing of the surgical area and an increase in the infection rate. This result is consistent with the results of this study.
In the skeletal system, related studies33, 34 also found a significant increase in the incidence of delayed union and nonunion, incision infection, osteomyelitis and low functional score after fracture surgery in smoking patients35, 36.
The main focus of current open fractures is to reduce the risk of infection, and early detection of bacterial contamination is the focus of the current research. A study by Merritt37 previously questioned whether debridement at 6 h or later increased the infection rate after open fracture. The research shows that the infection rate is related to the number of bacteria after wound debridement, but it has little correlation with the number of bacteria before debridement and at the time of the first debridement. Other studies have found that open fractures are mostly nosocomial infections caused by mainly gram‐negative bacteria, which are not commonly found in bacterial cultures from the perioperative wound. Even if the tissue culture is negative after intraoperative debridement, the postoperative infection cannot be avoided. Therefore, whether debridement is performed early on or later, some cases will still have infection after the operation. This suggests that the risk for postoperative infection depends upon how well the patient is managed after being hospitalized and has little to do with the length of time of injury to the first debridement.
Some scholars15, 38 analyzed the relationship between the timing of antibiotic injection and the time from the initial injury to the operation. The infection rate was significantly increased when antibiotics were administered after 3 h. Antibiotics should be administered as soon as possible (within 3 h) after the injury, but the long‐term use of antibiotics may increase bacterial resistance.
The “6 h debridement principle” may have played an important role in preventing infections in the past; however, the wide applications of antibiotics and advancements in medical technologies have decreased its utility in reducing the rate of infections for open fractures. The rates of infection for fractures are more dependent upon the severity of the fracture, tobacco use, operation time, early coverage of the wound after injury, timely administration of antibiotics (within 3 h after injury), and strict hospital management. However, this does not mean that debridement should be deliberately delayed. Open fracture treatment should still follow the basic principles of early debridement. It is recommended to complete this procedure within 24 h of the injury, but the “6 h principle” should be broken when formulating the debridement plan. This may allow more experienced doctors to participate in the operation. Careful and thorough debridement, a reasonable choice of fracture fixation, and early application of antibiotics should improve prognosis among fracture patients.
This study is a single‐center retrospective study with certain biases. The doctors on duty who perform emergency debridement after admission are uneven in age, and all surgeries are not performed by the same group of doctors, which causes some interference with the analysis results. The study sample size is small, and there may be bias in the statistical analysis results; the research results need to be further confirmed by multi‐center large‐sample studies.
Grant Sources: This study was supported by the Key Social Development Projects of Shaanxi Science and Technology Administration (2016SF‐340).
Disclosure: Each author certifies that he has no commercial or any other associations that might pose a conflict of interest in connection with the submitted article.
References
- 1. Court‐Brown CM, Mcbirnie J. The epidemiology of tibial fractures. J Bone Joint Surg Am, 1995, 77: 417–421. [PubMed] [Google Scholar]
- 2. Court‐Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM. The epidemiology of open fractures in adults. A 15‐year review. Injury, 2012, 43: 891–897. [DOI] [PubMed] [Google Scholar]
- 3. Morgenstern M, Kühl R, Eckardt H, et al Diagnostic challenges and future perspectives in fracture‐related infection. Injury, 2018, 49: S83–S90. [DOI] [PubMed] [Google Scholar]
- 4. Trampuz A, Zimmerli W. Diagnosis and treatment of infections associated with fracture‐fixation devices. Injury, 2006, 37: S59–S66. [DOI] [PubMed] [Google Scholar]
- 5. Shivapo SK, Jackson ND, Schleining JA, Kreuder AJ, Miles KG, Jeffery ND. Surgical intervention for vertebral osteomyelitis in a calf. Vet Surg, 2019, 48: 1064–1070. [DOI] [PubMed] [Google Scholar]
- 6. Spencer J, Smith A, Woods D. The effect of time delay on infection in open long‐bone fractures: a 5‐year prospective audit from a district general hospital. Ann R Coll Surg Engl, 2004, 86: 108–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Namdari S, Baldwin KD, Matuszewski P, Esterhai JL, Mehta S. Delay in surgical debridement of open tibia fractures: an analysis of national practice trends. J Orthop Trauma, 2011, 25: 140–144. [DOI] [PubMed] [Google Scholar]
- 8. Schenker ML, Yannascoli S, Baldwin KD, Ahn J, Mehta S. Does timing to operative debridement affect infectious complications in open long‐bone fractures? A systematic review. J Bone Joint Surg Am, 2012, 94: 1057–1064. [DOI] [PubMed] [Google Scholar]
- 9. Lee C, Porter KM. Prehospital management of lower limb fractures. Emerg Med J, 2005, 22: 660–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jedlicka N, Summers NJ, Murdoch MM. Overview of concepts and treatments in open fractures. Clin Podiatr Med Surg, 2012, 29: 279–290. [DOI] [PubMed] [Google Scholar]
- 11. Sprague S, Petrisor B, Jeray K, et al Wound irrigation does not affect health‐related quality of life after open fractures: results of a randomized controlled trial. Bone Joint J, 2018, 100: 88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sirkin M, Sanders R, Dipasquale T, Herscovici D. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma, 2004, 18: 32–38. [DOI] [PubMed] [Google Scholar]
- 13. Helfet DL, Haas NP, Schatzker J, Matter P, Moser R, Hanson B. AO philosophy and principles of fracture management—its evolution and evaluation. J Bone Joint Surg Am, 2003, 85: 1156–1160. [PubMed] [Google Scholar]
- 14. Patzakis MJ, Wilkins J, Moore TM. Considerations in deducing the infection rate in open tibial fractures. Clin Orthop Relat Res, 1983, 178: 36–41. [PubMed] [Google Scholar]
- 15. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res, 1989, 243: 36–40. [PubMed] [Google Scholar]
- 16. Wang S, Yin P, Quan C, et al Evaluating the use of serum inflammatory markers for preoperative diagnosis of infection in patients with nonunions. Biomed Res Int, 2017, 2017: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jiang N, Qin C, Hou Y, Yao Z, Yu B. Serum TNF‐α, erythrocyte sedimentation rate and IL‐6 are more valuable biomarkers for assisted diagnosis of extremity chronic osteomyelitis. Biomark Med, 2017, 11: 597–605. [DOI] [PubMed] [Google Scholar]
- 18. Metsemakers WJ, Kuehl R, Moriarty TF, et al Infection after fracture fixation: current surgical and microbiological concepts. Injury, 2016, 49: 511–522. [DOI] [PubMed] [Google Scholar]
- 19. Linn S. The injury severity score—Importance and uses. Ann Epidemiol, 1995, 5: 440–446. [DOI] [PubMed] [Google Scholar]
- 20. Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures. A new classification of type III open fractures. J Trauma, 1984, 24: 742–746. [DOI] [PubMed] [Google Scholar]
- 21. Kindsfater K, Jonassen EA. Osteomyelitis in grade II and III open tibia fractures with late debridement. J Orthop Trauma, 1995, 9: 121–127. [DOI] [PubMed] [Google Scholar]
- 22. Kreder HJ, Armstrong P. A review of open tibia fractures in children. J Pediatr Orthop, 1995, 15: 482–488. [DOI] [PubMed] [Google Scholar]
- 23. Pollak AN, Jones AL, Castillo RC, Bosse MJ, MacKenzie EJ, LEAP Study Group . The relationship between time to surgical debridement and incidence of infection after open high‐energy lower extremity trauma. J Bone Joint Surg Am, 2010, 92: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ibrahim T, Riaz M, Hegazy A, Erwin PJ, Tleyjeh IM. Delayed surgical debridement in pediatric open fractures: a systematic review and meta‐analysis. J Child Orthop, 2014, 8: 135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Charalambous CP, Siddique I, Zenios M, et al Early versus delayed surgical treatment of open tibial fractures: effect on the rates of infection and need of secondary surgical procedures to promote bone union. Injury, 2005, 36: 656–661. [DOI] [PubMed] [Google Scholar]
- 26. Reuss BL, Cole JD. Effect of delayed treatment on open tibial shaft fractures. Am J Orthop, 2007, 36: 215–220. [PubMed] [Google Scholar]
- 27. Chua W, Murphy D, Siow W, Kagda F, Thambiah J. Epidemiological analysis of outcomes in 323 open tibial diaphyseal fractures: a nine‐year experience. Singapore Med J, 2012, 53: 385–389. [PubMed] [Google Scholar]
- 28. Malhotra AK, Goldberg S, Graham J, et al Open extremity fractures: impact of delay in operative debridement and irrigation. J Trauma Acute Care Surg, 2014, 76: 1201–1207. [DOI] [PubMed] [Google Scholar]
- 29. Lua J, Tan VH, Sivasubramanian H, Kwek E. Complications of open tibial fracture management: risk factors and treatment. Malays Orthop J, 2017, 11: 18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stark E, Stucken C, Trainer G, Tornetta P. Compartment syndrome in Schatzker type VI plateau fractures and medial condylar fracture‐dislocations treated with temporary external fixation. J Orthop Trauma, 2009, 23: 502–506. [DOI] [PubMed] [Google Scholar]
- 31. Ren T, Ding L, Xue F, He Z, Xiao H. Risk factors for surgical site infection of pilon fractures. Clinics, 2015, 6: 419–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Colman M, Wright A, Gruen G, Siska P, Pape HC, Tarkin I. Prolonged operative time increases infection rate in tibial plateau fractures. Injury, 2013, 44: 249–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Porter SE, Hanley EN. The musculoskeletal effects of smoking. J Am Acad Orthop Surg, 2001, 9: 9–17. [DOI] [PubMed] [Google Scholar]
- 34. Gaston MS, Simpson AHRW. Inhibition of fracture healing. J Bone Joint Surg Br, 2007, 89: 1553–1560. [DOI] [PubMed] [Google Scholar]
- 35. Guan R, Wang J, Li Z, et al Sodium tanshinone IIA sulfonate decreases cigarette smoke‐induced inflammation and oxidative stress via blocking the activation of MAPK/HIF‐1α signaling pathway. Front Pharmacol, 2018, 9: 263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. de Oliveira Ramos C, Campos KKD, de Paula Costa G, Cangussú SD, Talvani A, Bezerra FS. Taurine treatment decreases inflammation and oxidative stress in lungs of adult mice exposed to cigarette smoke. Regul Toxicol Pharmacol, 2018, 98: 50–57. [DOI] [PubMed] [Google Scholar]
- 37. Merritt K. Factors increasing the risk of infection in patients with open fractures. J Trauma, 1988, 28: 823–827. [DOI] [PubMed] [Google Scholar]
- 38. Fletcher N, Sofianos D, Berkes MB, Obremskey WT. Prevention of perioperative infection. J Bone Joint Surg Am, 2007, 89: 1605–1618. [DOI] [PubMed] [Google Scholar]


