Abstract
Objective
This study aimed to investigate the optimal level of femoral neck for measuring femoral anteversion to predict postoperative stem anteversion in Crowe type I developmental dysplasia of the hip.
Methods
This retrospective study analyzed 108 Crowe type I hips that underwent THA between January 2016 and December 2017, including 70 women and 19 men with a mean age of 63.08 ± 9.13 (range, 41–83) years. The single‐wedge stem was used in 37 hips, the double‐wedge stem was used in 71 hips. Computed tomography scans were performed pre‐ and post‐operation. Femoral anteversion at six levels of the proximal femur were measured via preoperative two‐dimensional computed tomography. Femoral anteversion at the level of the femoral neck osteotomy plane and postoperative stem anteversion were measured via three‐dimensional reconstructed models.
Results
The mean follow‐up period was 18.5 months (range, 12–27). The mean preoperative Harris Hip Score was 51.5 ± 8.7 and improved to 90.4 ± 7.8 (P < 0.001) by the last follow‐up. There were no intraoperative fractures, and no infections occurred during the follow‐up period. Two patients developed deep venous thrombosis. There was no sign of prosthetic loosening in all hips. No significant correlations were found between the height of the femoral neck osteotomy plane and postoperative stem anteversion (r = −0.119, P = 0.220). Femoral anteversion decreased gradually from 64.00° ± 10.51° at the center of lesser trochanter to 15.21° ± 13.31° at the head–neck junction, which was changed from more to less than stem anteversion (24.37° ± 13.86°). The femoral anteversion at femoral head–neck junction (15.21° ± 13.31°) was significantly less than postoperative stem anteversion (P = 0.000), with a difference of −9.16° ± 9.27°. The femoral anteversion at the level of the osteotomy plane (28.48° ± 15.34°) was significantly more than the postoperative stem anteversion (P = 0.000), with a difference of 4.11° ± 9.56°. Among all six levels and the level of osteotomy, femoral anteversion at the 10‐mm level above the proximal base of lesser trochanter (22.65 ± 12.92) displayed the smallest difference (−1.72° ± 8.90°) and a good correlation (r = 0.764) with postoperative stem anteversion for all 108 hips, with a moderate correlation of 0.465 for single‐wedge stem hips and an excellent correlation of 0.821 for double‐wedge stem hips.
Conclusion
For Crowe type I hips, femoral anteversion would be different if it was measured via different levels of the femoral neck. The 10‐mm level above the proximal base of the lesser trochanter could be an optimum choice for measuring femoral anteversion to predict postoperative stem anteversion.
Keywords: Femoral anteversion, Stem anteversion, Developmental dysplasia, Hip, Total hip arthroplasty
Introduction
Total hip arthroplasty (THA) has been an effective method to relieve pain and improve function for adult patients with developmental dysplasia of the hip (DDH)1. Compared with ordinary hip osteoarthritis patients, DDH patients have abnormal anatomies, which increases the difficulty of THA operation and the occurrence of postoperative complications2. The most notable of these morphological variants is the increased likelihood to have excessive native femoral anteversion2. Previously, we have showed that native femoral anteversion in DDH patients is significantly greater than that in normal patients3. The study by Sugano et al.4 found that patients with DDH had an average increase of 10°–14° of anteversion of the native femoral neck and the incidence of anteversion greater than 40° was 23%. Similarly, the study by Noble et al.5 found femoral anteversion was increased in patients with DDH on average by 5° to 16°. The anteversion increased with increased subluxation of the hip. However, even in mild DDH cases (Crowe I), there was a significant increase in anteversion. Hence, abnormal femoral anteversion should be considered in THA for DDH patients, even for the mild Crowe type I hips2, 6. Combined anteversion means the sum of the cup and stem anteversion in THA. The combined anteversion theory has become a popular way to avoid impingement and dislocation, and maximize hip range of motion7. Previously, we have shown that the concept of combined anteversion contributes to joint stability after THA for DDH patients8, 9. Cementless, straight, tapered femoral stems are commonly used, which depends mainly on the anatomy of the proximal femur, and in whom adjusting the anteversion of the femoral stem is difficult10. If the preoperative femoral anteversion angle is eccentric, a monoblock or modular stem with adjustable anteversion is preferable to correct excessive anteversion2, 11. Therefore, prediction of the postoperative anteversion of the femoral stem helps choose an appropriate femoral prosthesis and optimize the combined anteversion2.
Preoperative computed tomography (CT) can help assess femoral anteversion, which is thought to be the most accurate imaging method currently available12. Although several methods have been developed to predict postoperative stem anteversion, no standard predictive method has been established. Three‐dimensional CT technique can measure the native femoral anteversion more accurately than two‐dimensional CT, but it does not show an advantage in predicting the postoperative stem anteversion, and this technique is time‐consuming making it inaccessible for surgeons13. The classical method of Sugano, of measuring femoral anteversion based on two‐dimensional CT image, remains the most commonly used method because of its convenience, accuracy, and repeatability14, 15. However, whether measuring femoral anteversion via two‐dimensional CT can predict postoperative stem anteversion remains controversial. Some studies reported that postoperative stem anteversion was predictable, but the results varied widely13, 16, 17, 18, with the reported difference between preoperative femoral anteversion and postoperative stem anteversion varying from 2.3° ± 5.9° to 22.7° ± 11.6°, and the correlation coefficient varying from 0.46 to 0.93. Furthermore, some studies found that it was difficult to predict postoperative stem anteversion, especially for the single‐wedge stems16, 19. We speculated that one main reason for the controversy may lie in the inconsistency of the methods used to measure femoral anteversion for stem anteversion prediction. Because of the torsion in the proximal femur16, 17, the anteversion angle measured at different levels of the femoral neck could be different. However, at present, the optimal level of the femoral neck for measuring femoral anteversion to predict postoperative stem anteversion is not yet established.
The “acetabular first” technique remains the most commonly used in THA. Intraoperatively estimating the femoral anteversion at the level of the femoral neck osteotomy plane to predict the postoperative stem anteversion and then adjusting the cup anteversion accordingly is one method often used in the “acetabular first” technique to target combined anteversion within the safe zone. Previously, we reported the effectiveness of this method for DDH patients who underwent THA, which reduced dislocation risk and achieved better impingement‐free range of motion8, 9. However, the difference of the femoral anteversion at the level of the osteotomy plane with the postoperative stem anteversion remains to be elucidated.
To our best knowledge, there were few reports on the prediction of postoperative stem anteversion in DDH patients16. Crowe type I hips are the most common candidates for THA in the four Crowe types. Therefore, this study aimed: (i) to retrospectively analyze the characteristics of femoral anteversion in Crowe type I hips; (ii) to explore the optimal level of the femoral neck for measuring femoral anteversion to predict postoperative stem anteversion.
Materials and Methods
Inclusion and Exclusion Criteria
This was a single center retrospective study, approved by the local institutional review board. The inclusion criteria followed the P (participant), I (intervention), C (comparison), O (outcome), S (study design) principle: (i) Participant: adult Crowe type I hips according to Crowe classification20, having extreme impairment of daily activity; (ii) Intervention: underwent THA between January 2016 and December 2017; (iii) Comparison: the differences of femoral anteversion at different levels with the postoperative stem anteversion; (iv) Outcome: the optimal level of femoral neck for predicting postoperative stem anteversion; and (v) Study design: a retrospective study. The exclusion criteria were: (i) previous hip surgery; (ii) lack of integral imaging data; (iii) obvious flexion contracture of the hip; and (iv) more than 3° malalignment of the stem in the coronal and/or sagittal plane18.
Patient Data
A total of 147 consecutive THAs were performed for Crowe type I DDH patients between January 2016 and December 2017. In total, 39 hips were excluded from this study because of insufficient preoperative or postoperative CT data (27 hips), obvious flexion contracture of the hip (three hips), and more than 3° malalignment of the stem in the coronal and/or sagittal plane (nine hips). The remaining 108 hips (89 patients) were included in the study, including 70 women and 19 men with a mean age of 63.08 ± 9.13 (range, 41–83) years. The single‐wedge stem was used in 37 hips (Accolade, Stryker, Howmedica, Mahwah, NJ, USA); the double‐wedge stem was used in 71 hips (Secur‐fit, Stryker, Howmedica, Mahwah, NJ, USA).
CT Scanning
CT evaluation was performed as we previously reported21 by using the Hitachi Radix Turbo (Tokyo, Japan) (120 kVp, 200 mA, 5‐mm collimation, 5 mm/s table speed, and 5‐mm resolution index) device. By using axial sections passing from the anterior superior iliac spine to the tibial tubercle, patients underwent 1‐mm interval CT in the supine position with the hips and knees fully extended and the lower limbs as horizontal and parallel as possible. Pre‐ and postoperative CT data were stored in Digital Imaging and Communication in Medicine (DICOM) format. Femoral measurement was performed using the Radiant DICOM Viewer (version 4.6.9, 64‐bit, Medixant Company, Poland).
Surgical Procedure
All operations were performed by the same group of surgeons, with the posterolateral approach and “acetabular first” technique with the concept of combined anteversion. The procedure has been described in detail previously8, 9. Briefly, after dislocating the femoral head posteriorly, the femoral neck osteotomy was conducted (45° from the femoral anatomical axis). The assistant positioned the knee joint at a 90° angle in the flexion position with the foot arch upward, perpendicular to the horizontal plane. The femoral anteversion was evaluated by examining the axis of the femoral neck osteotomy plane and horizontal plane. Then, the acetabular cup was implanted targeting the combined anteversion of 40° ± 15°. Routine intraoperative fluoroscopy was used to verify the size and position of the final femoral broach to achieve “best‐fit”. Finally, the stem was press‐fitted according to the geometry of the native proximal femur
Follow‐up and Assessment
Outpatient follow‐ups were performed 1, 3, 6, and 12 months after surgery. Subsequently, yearly follow‐ups were performed. Clinical and imageological assessments were performed.
Harris Hip Score
The Harris hip score (HHS) was used to assess the hip joint function of each patient prior to surgery and at each follow‐up examination after surgery22. The HHS score system mainly includes the four aspects of pain, function, absence of deformity, and range of motion. The score standard had a maximum of 100 points (best possible outcome). A total score < 70 is considered a poor score, 70–80 fair, 80–90 good, and 90–100 excellent.
Radiographic Assessment
A series of radiographs of the pelvis were obtained at each follow‐up visit and were carefully assessed for loosening of the prosthesis. The stability of the acetabular components was assessed radiographically using the method of DeLee and Charnley23 and that of the femoral components using the method of Gruen et al.24. Specifically, the criteria are as follows: (i) Stable fixation, no prosthesis displacement, no radiolucency or sclerotic band around the prosthesis; (ii) Fibrous stability, no prosthesis displacement, radiolucency <1mm around the prosthesis; (iii) Probable loosening, no prosthesis displacement, a discontinuous radiolucency >2 mm around the prosthesis; and (iv) Definite loosening, prosthesis displacement or breakage, screw breakage or sclerotic band around the screw, continuous radiolucency >2mm around the prosthesis.
CT Assessment
To facilitate preoperative measurement, femoral anteversion was measured at six levels (level a–f) of the proximal femur via preoperative two‐dimensional CT (Fig. 1A). The six levels were as follows: level a, center of the lesser trochanter; level b, proximal base of the lesser trochanter; level c, 5 mm above level b; level d, 10 mm above level b; level e, 15mm above level b; level f, femoral head–neck junction (just below the head). The anteversions of the anterior cortex and posterior cortex at six levels were measured respectively as the angles formed by the cortical lines and the posterior aspect of the femoral condylar line (Fig. 1B and C). The femoral anteversion at each level was calculated using the classical method as the average of the anterior cortex anteversion and posterior cortex anteversion16.
Figure 1.
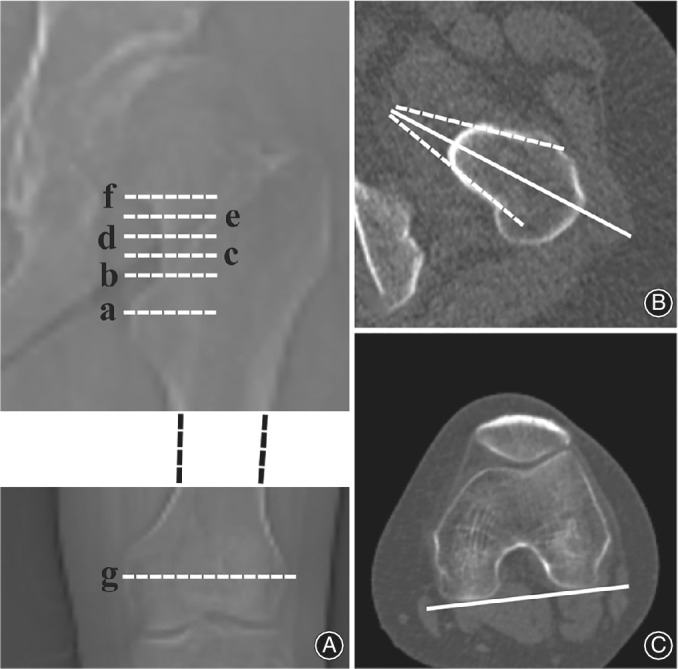
Measurement of femoral anteversion via two‐dimensional computed tomography. (A) Six measurement levels of femoral anteversion: level a, centre of the lesser trochanter; level b, proximal base of the lesser trochanter; level c, 5 mm above level b; level d, 10 mm above level b; level e, 15 mm above level b; level f, femoral head–neck junction; g, the level showed the most posterior points of the femoral condyles. (B) Anteversions of the anterior cortex and posterior cortex were measured respectively as the angles formed by the cortical lines (white dashed lines) and the posterior aspect of the femoral condylar line. Femoral anteversion was calculated as the average of the anterior cortex anteversion and posterior cortex anteversion (white solid line). (C) Posterior aspect of the femoral condylar line at level g.
The height of the femoral head–neck junction was measured as the vertical distance between the proximal base of the lesser trochanter and the medial edge of the femoral head–neck junction (just below the head). The height of the femoral neck osteotomy plane was measured as the vertical distance between the proximal base of the lesser trochanter and the medial edge of the osteotomy plane.
Femoral anteversion at the level of the femoral neck osteotomy plane and postoperative stem anteversion were measured on three‐dimensional models, which were reconstructed with Mimics software (version 15.0; Materialize, Leuven, Belgium) (Fig. 2). The femoral neck osteotomy plane for each three‐dimensional model was simulated at the height measured on postoperative two‐dimensional CT and at 45° angle from the femoral anatomical axis (the same as the with surgical operation). The femoral anteversion of each model was measured as the average of the anterior cortex anteversion and the posterior cortex anteversion (Fig. 2A). The postoperative stem anteversion of each model was measured as the angle formed by the stem neck major axis and the posterior aspect of the femoral condylar line25 (Fig. 2B). All CT measurements were performed twice over an interval of more than 2 weeks by two orthopaedic surgeons.
Figure 2.
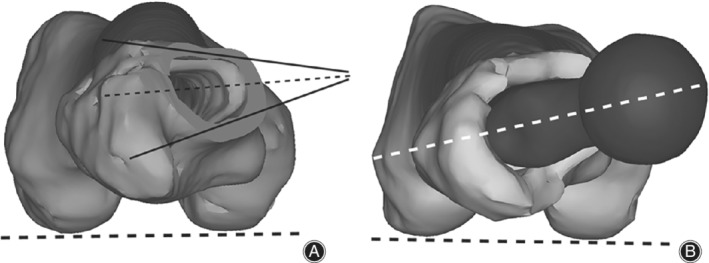
Measurement of femoral anteversion and stem anteversion via three‐dimensional reconstructed computed tomography. (A) The femoral anteversion at the level of the osteotomy plane was measured as the average (thin black dashed line) of the anterior cortex anteversion and posterior cortex anteversion (black solid lines) relative to the posterior aspect of the femoral condylar line (thick black dashed line). (B) The stem anteversion was measured as the angle formed by the stem neck major axis (white dashed line) and the posterior aspect of the femoral condylar line (black dashed line).
Statistical Analysis
Data were expressed as the mean ± standard deviation. All statistical analyses were performed using SPSS software for Windows (version 18.0; SPSS, Chicago, IL, USA). The intraclass correlation coefficients of interobserver and intraobserver reliabilities were calculated. The Shapiro–Wilk test for normal distribution was used before any statistical analysis was performed. The Wilcoxon signed rank test was used to assess the difference between preoperative femoral anteversion and postoperative stem anteversion. Spearman's correlation analysis was done to evaluate the association between each preoperative anteversion and postoperative stem anteversion. A P value <0.05 was considered to represent a significant difference. Correlation (r) was characterized as poor (0.00 to 0.20), fair (0.21 to 0.40), moderate (0.41 to 0.60), good (0.61 to 0.80), or excellent (0.81 to 1.00).
Results
Harris Hip Score
The mean follow‐up period was 18.5 months (range, 12–27). The mean preoperative Harris hip score was 51.5 ± 8.7 and improved to 90.4 ± 7.8 (P < 0.001) by the last follow‐up.
Radiographic Results
The radiological stability of the acetabular and femoral components were assessed and there was no definite sign of prosthetic loosening in all hips.
Intraobserver and Interobserver Reliabilities
The intraclass correlation coefficients for intraobserver and interobserver reliabilities were excellent (0.888–0.967 and 0.844–0.958, respectively).
Height of the Head‐Neck Junction
Generally, for all 108 hips, the mean preoperative height of the head–neck junction was 17.70 ± 2.66 mm, including five hips with head–neck junction height < 15 mm (11.00–14.50 mm) and 103 hips with ≥15 mm (15.00–25.00 mm).
Height of the Femoral Neck Osteotomy Plane
The mean height of the femoral neck osteotomy plane was 5.11 ± 2.98 mm. The mean postoperative stem anteversion was 24.37° ± 13.86°. No significant correlations were found between the height of the femoral neck osteotomy plane and postoperative stem anteversion (r = −0.119, P = 0.220).
Characteristics of Femoral Anteversion
Generally, from the center of the lesser trochanter (level a) to the head–neck junction (level f), the anterior cortex anteversion changed slightly (between 14.54° ± 13.68° and 9.08° ± 14.98°), while the posterior cortex anteversion markedly changed with a gradual decrease (from 113.46° ± 12.11° to 18.77° ± 13.66°). Accordingly, the femoral anteversion was reduced gradually from 64.00° ± 10.51° at level a to 15.21° ± 13.31° at level f, which was from more than stem anteversion to less than stem anteversion (Table 1). Hence, these results verified that femoral anteversion would be different if it is measured via different levels of the femoral neck (Fig. 3).
Table 1.
Femoral anteversion measured at different levels
| Level | No. | Anterior cortex anteversion (°) | Posterior cortex anteversion (°) | Femoral anteversion (°) | Stem anteversion (°) | Difference (°) | P | r(P) |
|---|---|---|---|---|---|---|---|---|
| a | 108 | 14.54 ± 13.68 | 113.46 ± 12.11 | 64.00 ± 10.51 | 24.37 ± 13.86 | 39.63 ± 10.89 | 0.000 | 0.602 (0.000) |
| b | 108 | 13.60 ± 13.56 | 52.61 ± 19.06 | 33.10 ± 15.33 | 24.37 ± 13.86 | 8.73 ± 9.16 | 0.000 | 0.793 (0.000) |
| c | 108 | 12.07 ± 14.00 | 45.49 ± 16.80 | 28.78 ± 14.52 | 24.37 ± 13.86 | 4.41 ± 9.70 | 0.000 | 0.751 (0.000) |
| d | 108 | 9.08 ± 14.98 | 36.22 ± 12.46 | 22.65 ± 12.92 | 24.37 ± 13.86 | −1.72 ± 8.90 | 0.402 | 0.764 (0.000) |
| e | 103 | 9.43 ± 15.27 | 25.64 ± 12.85 | 17.53 ± 12.76 | 24.40 ± 14.00 | −6.87 ± 8.73 | 0.000 | 0.787 (0.000) |
| f | 108 | 11.64 ± 14.15 | 18.77 ± 13.66 | 15.21 ± 13.31 | 24.37 ± 13.86 | −9.16 ± 9.27 | 0.000 | 0.764 (0.000) |
| Osteotomy plane | 108 | 11.48 ± 14.01 | 45.47 ± 18.74 | 28.48 ± 15.34 | 24.37 ± 13.86 | 4.11 ± 9.56 | 0.000 | 0.767 (0.000) |
Level, refer to Fig. 1; Difference = femoral anteversion − stem anteversion
Figure 3.
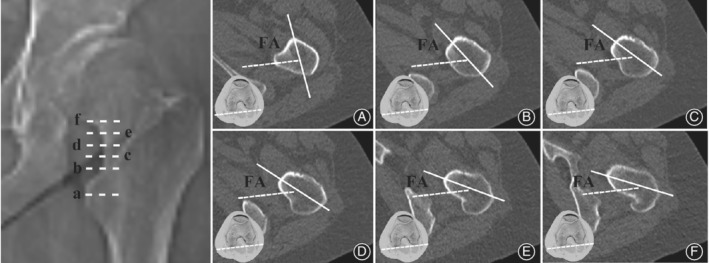
Change in femoral anteversion measured at different levels. From level a to f, the femoral anteversion (FA) was reduced gradually. Level a‐f, refer to Fig. 1. White dashed line: the posterior aspect of the femoral condylar line; white solid line: the middle line of the anterior cortex and posterior cortex.
Difference Between Femoral Anteversion and Postoperative Stem Anteversion
For all 108 hips (Table 1), good correlations were shown between femoral anteversion at all measurement levels and postoperative stem anteversion (r = 0.602–0.793); however, only the femoral anteversion at level d (22.65° ± 12.92°) showed no statistical difference with postoperative stem anteversion (P = 0.402), with a difference of −1.72° ± 8.90° and a correlation of 0.764 (Fig. 4). Level f (head–neck junction) was often used for measuring femoral anteversion in previous studies15, 16. Our results showed that the femoral anteversion at level f (15.21° ± 13.31°) was significantly less than postoperative stem anteversion (P = 0.000), with a difference of −9.16° ± 9.27°. In addition, as an intraoperative reference 8, the femoral anteversion at the level of the osteotomy plane (28.48° ± 15.34°) was significantly more than the postoperative stem anteversion (P = 0.000), with a difference of 4.11° ± 9.56°. Hence, our results showed that femoral anteversion at level d (10‐mm level above the proximal base of the lesser trochanter) displayed minimum difference with postoperative stem anteversion, with a good correlation.
Figure 4.
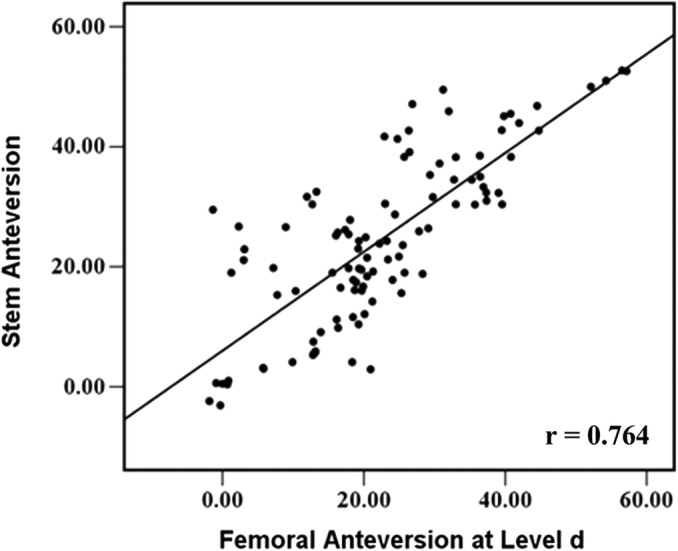
Correlation of femoral anteversion measured at level d with stem anteversion for all 108 hips.
Anteversion Prediction for Single‐Wedge and Double‐Wedge Stems
We further analyzed whether femoral anteversion measured at level d could be used as a predictor for postoperative stem anteversion for both single‐wedge and double‐wedge stems (Table 2). For single‐wedge stems, moderate correlations were shown between femoral anteversion at all measurement levels and stem anteversion (r = 0.417–0.578). The femoral anteversion at level c, level d, and osteotomy plane showed no statistical difference with postoperative stem anteversion (P = 0.081, 0.597, and 0.131, respectively), while the femoral anteversion at level d showed the smallest difference of −0.23° ± 9.54° in the stem anteversion, with a correlation of 0.465 (Fig. 5A). For double‐wedge stems, good to excellent correlations were found between femoral anteversion at all measurement levels and stem anteversion (r = 0.637–0.874), while only the femoral anteversion at level d showed no statistical difference in stem anteversion (P = 0.123), with a difference of −2.50° ± 8.52° and an excellent correlation of 0.821 (Fig. 5B).
Table 2.
Comparison between the femoral anteversion (°) at each level and the anteversion (°) of single‐wedge and double‐wedge stems
| Single wedge stems | Double wedge stems | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level | No. | Femoral anteversion | Stem anteversion | Difference (°) | P | r (P) | No. | Femoral anteversion | Stem anteversion | Difference (°) | P | r (P) |
| a | 37 | 62.46 ± 7.75 | 20.64 ± 11.17 | 41.82 ± 10.22 | 0.000 | 0.417 (0.01) | 71 | 64.80 ± 11.66 | 26.32 ± 14.78 | 38.48 ± 11.13 | 0.000 | 0.637 (0.000) |
| b | 37 | 28.26 ± 12.92 | 20.64 ± 11.17 | 7.61 ± 12.01 | 0.000 | 0.541 (0.001) | 71 | 35.63 ± 15.96 | 26.32 ± 14.78 | 9.31 ± 7.28 | 0.000 | 0.874 (0.000) |
| c | 37 | 23.90 ± 12.68 | 20.64 ± 11.17 | 3.26 ± 11.79 | 0.081 | 0.460 (0.004) | 71 | 31.33 ± 14.84 | 26.32 ± 14.78 | 5.01 ± 8.44 | 0.000 | 0.822 (0.000) |
| d | 37 | 20.41 ± 8.60 | 20.64 ± 11.17 | −0.23 ± 9.54 | 0.597 | 0.465 (0.004) | 71 | 23.82 ± 14.60 | 26.32 ± 14.78 | −2.50 ± 8.52 | 0.123 | 0.821 (0.000) |
| e | 36 | 14.73 ± 8.93 | 20.98 ± 11.14 | −6.25 ± 9.69 | 0.001 | 0.578 (0.000) | 67 | 19.04 ± 14.24 | 26.24 ± 15.08 | −7.20 ± 8.22 | 0.000 | 0.832 (0.000) |
| f | 37 | 12.58 ± 10.95 | 20.64 ± 11.17 | −8.06 ± 10.81 | 0.000 | 0.536 (0.001) | 71 | 16.59 ± 14.27 | 26.32 ± 14.78 | −9.72 ± 8.38 | 0.000 | 0.820 (0.000) |
| Osteotomy plane | 37 | 23.03 ± 12.85 | 20.64 ± 11.17 | 2.39 ± 11.13 | 0.131 | 0.557 (0.000) | 71 | 31.32 ± 15.83 | 26.32 ± 14.78 | 5.00 ± 8.58 | 0.000 | 0.820 (0.000) |
Level, refer to Fig. 1; Difference = femoral anteversion − stem anteversion
Figure 5.
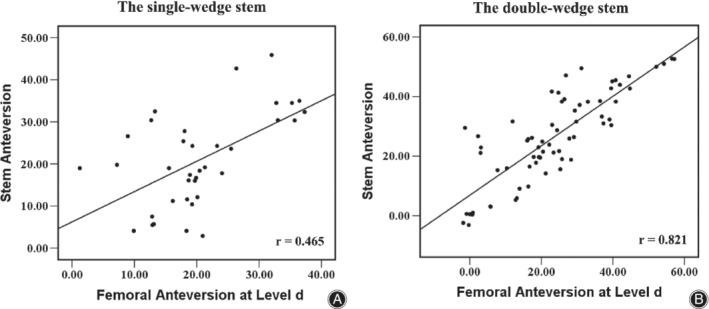
Correlations of femoral anteversion measured at level d with stem anteversion for single‐wedge stems (A) and double‐wedge stems (B).
Hence, the 10‐mm level above the proximal base of the lesser trochanter could be chosen as the optimal level for measuring femoral anteversion to predict postoperative stem anteversion in Crowe type I DDH hips, which is applicable for both single‐wedge and double‐wedge stems.
Complications
There were no intraoperative fractures, and no infections occurred during the follow‐up period. Two patients developed deep venous thrombosis; this condition resolved after anticoagulation treatment with low molecular‐weight heparin. No patients required revision during the follow‐up period.
Discussion
Prediction of Stem Anteversion for DDH
As for the prediction of postoperative stem anteversion via preoperative two‐dimensional CT, few studies were conducted for DDH patients. The study by Taniguchi et al.16 showed that for the double‐wedge stem, the difference between femoral anteversion and stem anteversion was 17.2° ± 8.3°, the correlation coefficient was 0.78; for the single‐wedge stem, the difference was 22.7° ± 11.6°, the correlation coefficient was 0.46. Compared with their findings, the current study showed similar correlations, but smaller differences. In their study, patients with Crowe types were not listed, which demonstrates different femoral anteversion26, and larger differences than that of other previous studies were shown16.
Optimal Femoral Neck Level for the Prediction of Stem Anteversion
This study demonstrated that the femoral anteversion value may be different if it is measured at different levels of the femoral neck for Crowe type I DDH hips. From the center of lesser trochanter to head–neck junction, femoral anteversion reduced gradually from more to less than postoperative stem anteversion. Although several methods of measuring the femoral anteversion via two‐dimensional CT have been reported16, 18, 19, 27, 28, there is no report on the optimal level of the femoral neck recommended to measure preoperative femoral anteversion for the prediction of postoperative stem anteversion. The study by Kwan et al.13 reported that femoral anteversion measured via the middle level of the femoral neck could predict postoperative stem anteversion better than that measured at the head–neck junction level. The current study clearly showed that, for Crowe type I DDH hips, femoral anteversion at the 10‐mm level above the proximal base of the lesser trochanter showed the smallest difference with the stem anteversion among different levels of femoral neck, including the level of the head–neck junction and the level of the osteotomy plane, which were often used for the prediction of postoperative stem anteversion in clinical practice8, 9, 16.
Prediction of Stem Anteversion for Hips with Different Femoral Stems
Similar to the study by Taniguchi et al.16, the double‐wedge stem showed a better correlation with femoral anteversion than the single‐wedge stem in the current study. It has been believed that the difference is related to the stem design. Compared with the double‐wedge stem, the single‐wedge stem is relatively thin29, has more freedom in the horizontal plane7, and is prone to tilting17, which could change the stem anteversion. However, only one measurement method was used in the current study and the study by Taniguchi et al.16. The femoral anteversion value measured by different methods is different even for the same patient13, 15. There may be one measurement method that could be more suitable for predicting the anteversion of a specific stem than other methods. Hence, further studies are needed to compare the difference between the femoral neck and stem anteversion in a single‐wedge stem compared to a double‐wedge stem.
Limitations of the Study
One limitation to this study is that the femoral neck osteotomy plane for each three‐dimensional model was simulated at the level measured via postoperative two‐dimensional CT and at 45° angle from the femoral anatomical axis used intraoperatively. There may be some difference in the actual situation. The point‐to‐point match technique of preoperative and postoperative models30 may provide more accuracy, but it is more complicated. However, to our knowledge, this is the first study on the prediction of postoperative stem anteversion in Crowe type I DDH patients.
Conclusion
This study demonstrated that femoral anteversion is different if it is measured via different levels of the femoral neck in Crowe type I DDH patients. The 10‐mm level above the proximal base of the lesser trochanter displayed the smallest difference with postoperative stem anteversion, with moderate correlations with single‐wedge stems, and excellent correlations with double‐wedge stems, which would be an optimum choice for measuring femoral anteversion to predict postoperative stem anteversion in Crowe type I hips.
Authorship declaration
Zhenan Zhu, Mengning Yan, and Yuanqing Mao contributed to the study design; Degang Yu and Zanjing Zhai performed the data collection and drafted the manuscript, Jingwei Zhang and Huiwu Li contributed to the statistical data analyses. All authors contributed to interpretation of results, and critical revisions of the manuscript; and they all agreed on its final appearance.
Conflict of interest
There are no conflicts of interest to declare.
Co‐first authorship: The first two authors contributed equally to this manuscript.
Co‐corresponding authorship: The last two authors contributed equally to this manuscript.
Grant Sources This work was supported by grants from the National Natural Science Foundation of China (No. 81572158 and 81772361), Shanghai Clinical Medical Center (Grant Number 2017ZZ01023), and Shanghai Municipal Key Clinical Specialty.
Disclosure The authors declare that they have no competing interests. All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors; all authors are in agreement with the manuscript.
References
- 1. Ferguson RJ, Palmer AJR, Taylor A, Porter ML, Malchau H, Glyn‐Jones S. Hip replacement. Lancet, 2018, 392: 1662–1671. [DOI] [PubMed] [Google Scholar]
- 2. Greber EM, Pelt CE, Gililland JM, Anderson MB, Erickson JA, Peters CL. Challenges in total hip arthroplasty in the setting of developmental dysplasia of the hip. J Arthroplasty, 2017, 32: S38–S44. [DOI] [PubMed] [Google Scholar]
- 3. Li H, Wang Y, Oni JK, et al The role of femoral neck anteversion in the development of osteoarthritis in dysplastic hips. Bone Joint J, 2014, 96‐b: 1586–1593. [DOI] [PubMed] [Google Scholar]
- 4. Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br, 1998, 80: 711–719. [DOI] [PubMed] [Google Scholar]
- 5. Noble PC, Kamaric E, Sugano N, et al Three‐dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res, 2003, 417: 27–40. [PubMed] [Google Scholar]
- 6. Perry KI, Berry DJ, Perry KI, Berry DJ. Femoral considerations for total hip replacement in hip dysplasia. Orthop Clin North Am, 2012, 43: 377–386. [DOI] [PubMed] [Google Scholar]
- 7. Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res, 2009, 467: 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang J, Wang L, Mao Y, Li H, Ding H, Zhu Z. The use of combined anteversion in total hip arthroplasty for patients with developmental dysplasia of the hip. J Arthroplasty, 2014, 29: 621–625. [DOI] [PubMed] [Google Scholar]
- 9. Zhang J, Wei J, Mao Y, Li H, Xie Y, Zhu Z. Range of hip joint motion in developmental dysplasia of the hip patients following total hip arthroplasty with the surgical technique using the concept of combined Anteversion: a study of Crowe I and II patients. J Arthroplasty, 2015, 30: 2248–2255. [DOI] [PubMed] [Google Scholar]
- 10. Dorr LD, Zhinian W, Aamer M, Jinjun Z, Manish D, Prashant D. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am, 2009, 91: 2598–2604. [DOI] [PubMed] [Google Scholar]
- 11. Peters CL, Chrastil J, Stoddard GJ, Erickson JA, Anderson MB, Pelt CE. Can radiographs predict the use of modular stems in developmental dysplasia of the hip? Clin Orthop Relat Res, 2016, 474: 423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Botser IB, Ozoude GC, Martin DE, Siddiqi AJ, Kuppuswami S, Domb BG. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Art Ther, 2012, 28: 619–627. [DOI] [PubMed] [Google Scholar]
- 13. Kwan Kyu P, Tsung‐Yuan T, Dimitris D, Young‐Min K. Utility of preoperative femoral neck geometry in predicting femoral stem Anteversion. J Arthroplasty, 2015, 30: 1079–1084. [DOI] [PubMed] [Google Scholar]
- 14. Georgiadis AG, Siegal DS, Scher CE, Zaltz I. Can femoral rotation be localized and quantified using standard CT measures? Clin Orthop Relat Res, 2015, 473: 1309–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr, 1998, 22: 610–614. [DOI] [PubMed] [Google Scholar]
- 16. Taniguchi N, Jinno T, Koga D, Hagino T, Okawa A, Haro H. Cementless hip stem Anteversion in the dysplastic hip: a comparison of tapered wedge vs metaphyseal filling. J Arthroplasty, 2016, 32: 1547. [DOI] [PubMed] [Google Scholar]
- 17. Hirata M, Nakashima Y, Itokawa T, et al Influencing factors for the increased stem version compared to the native femur in cementless total hip arthroplasty. Int Orthop, 2014, 38: 1341–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Abe H, Sakai T, Takao M, Nishii T, Nakamura N, Sugano N. Difference in stem alignment between the direct anterior approach and the posterolateral approach in Total hip arthroplasty. J Arthroplasty, 2015, 30: 1761–1766. [DOI] [PubMed] [Google Scholar]
- 19. Worlicek M, Weber M, Craiovan B, et al Native femoral anteversion should not be used as reference in cementless total hip arthroplasty with a straight, tapered stem: a retrospective clinical study. BMC Musculoskelet Dis, 2016, 17: 399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Banaszkiewicz PA. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am, 1979, 61: 15. [PubMed] [Google Scholar]
- 21. Yu DG, Zhang JW, Xu C, et al Changes in alignment of ipsilateral knee on computed tomography after total hip arthroplasty for developmental dysplasia of the hip. Orthop Surg, 2019, 11: 397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end‐result study using a new method of result evaluation. J Bone Joint Surg Am, 1969, 51: 737–755. [PubMed] [Google Scholar]
- 23. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res, 1976, 121: 20–32. [PubMed] [Google Scholar]
- 24. Banaszkiewicz PA. “Modes of failure” of cemented stem‐type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res, 1979, 141: 17. [PubMed] [Google Scholar]
- 25. Dimitriou D, Tsai TY, Kwon YM. The effect of femoral neck osteotomy on femoral component position of a primary cementless total hip arthroplasty. Int Orthop, 2015, 39: 2315–2321. [DOI] [PubMed] [Google Scholar]
- 26. Boughton OR, Uemura K, Tamura K, et al Gender and disease severity determine proximal femoral morphology in developmental dysplasia of the hip. J Orthop Res, 2019, 37: 1123–1132. [DOI] [PubMed] [Google Scholar]
- 27. Emerson RH. Increased anteversion of press‐fit femoral stems compared with anatomic femur. Clin Orthop Relat Res, 2012, 470: 477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Suh KT, Kang JH, Roh HL, Moon KP, Kim HJ. True femoral anteversion during primary Total hip arthroplasty. J Arthroplasty, 2006, 21: 599–605. [DOI] [PubMed] [Google Scholar]
- 29. Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am, 2011, 93: 500–509. [DOI] [PubMed] [Google Scholar]
- 30. Xu J, Qu X, Li H, Mao Y, Yu D, Zhu Z. Three‐dimensional host bone coverage in Total hip arthroplasty for Crowe types II and III developmental dysplasia of the hip. J Arthroplasty, 2017, 32: 1374–1380. [DOI] [PubMed] [Google Scholar]


