Since after December 8, 2019 when the first case of coronavirus disease 2019 (COVID-19) was identified in Wuhan, China, the number of infected cases has been strikingly increased. World Health Organization (WHO) declared a “public health emergency of international concern” at January 30, 2020 and a “global pandemic” at March 11, 2020. As of April 18, 2020, confirmed cases were 2,188,936 and confirmed deaths were 152,515 across 216 countries worldwide.
Many of medical societies announced their own guidelines for management of cancer patients including gynecologic cancers in order to effectively confront this terrible situations [1,2]. However, those guidelines cannot be applied to every country across the globe because of the different situations of COVID-19. Instead, experiences from the individualized management in affected local areas are real examples that could help ascertain the best safety of both patients and health care providers. We herein present a few gynecologic cancer cases in Japan and Korea of which the management courses were affected by COVID-19. Informed consent was obtained from every patients.
OVARIAN CANCER PATIENTS UNDER NEOADJUVANT CHEMOTHERAPY WITH STRONG SUSPICION OF COVID-19
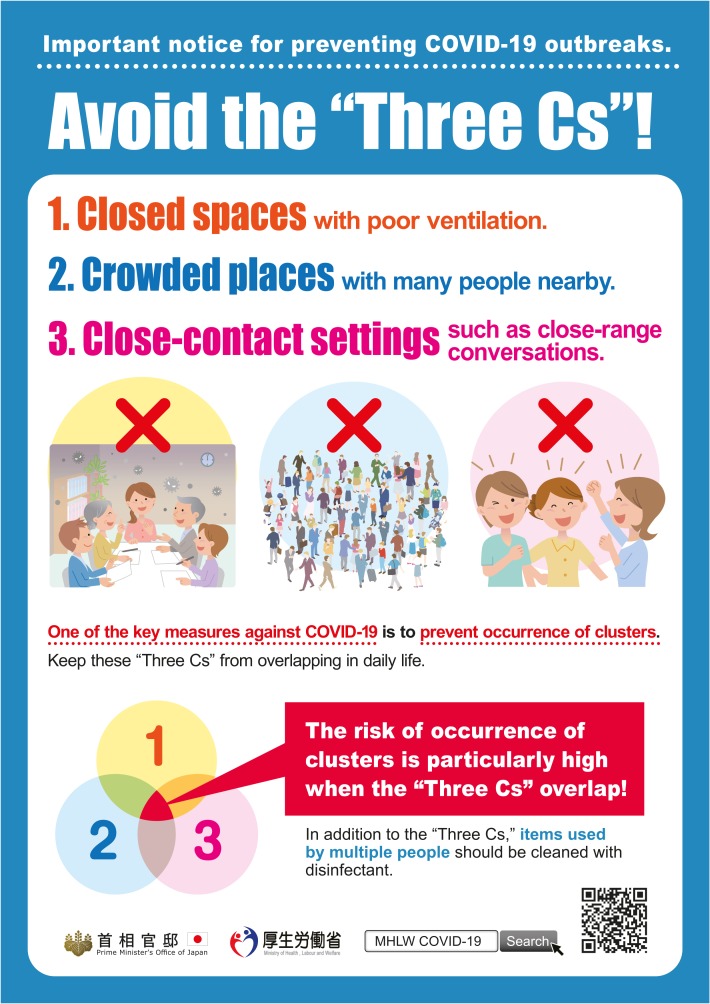
In Japan, as of April 23, there were 11,919 cases of COVID-19 infection in Japan. This included 7,315 symptomatic cases, 778 asymptomatic cases, and 3,826 cases under confirmation of the symptom. There were 287 deaths and 2,408 discharged from the hospital. On April 7, 2020, a state of emergency was declared under the Act on Special Measures for Pandemic Influenza and New Infectious Diseases Preparedness and Response. The period during which emergency measures should be taken under the declaration is 29 days from April 7 to May 6, 2020. Areas where emergency measures should be taken are Saitama, Chiba, Tokyo, Kanagawa, Osaka, Hyogo and Fukuoka Prefectures. Overall policies are being pursued to 1) slow down the speed of infection by containing clusters and reducing chances of contact, 2) minimize incidence of severe cases and death through surveillance and appropriate medical care especially for the elderly 3) minimize the impact on society and economy through pandemic prevention and economic and employment measures. Containment of the outbreak of clusters, which are patient-linked populations recognized by active epidemiological investigations, is thought to prevent the explosive spread of infection and minimize the number of infected, seriously ill, and fatalities. Therefore, there is a greater push to avoid the “Three Cs” (1. Closed spaces with insufficient ventilation, 2. Crowded conditions with people, 3. Conversations in short distance) that pose a particularly higher risk of clusters development (Fig. 1). Under the state of emergency, the public, including the government, local governments, medical personnel, experts, and businesses, have come together to implement basic infection prevention, refrain from going out of the house unnecessarily, and avoid “Three Cs,” but the clinical environment is pressing. We report on a case in our institution where COVID-19 infection was suspected during treatment of gynecological tumors, forcing a change in treatment course.
Fig. 1. Three Cs (1. Closed spaces with insufficient ventilation, 2. Crowded conditions with people, 3. Conversations in short distance).
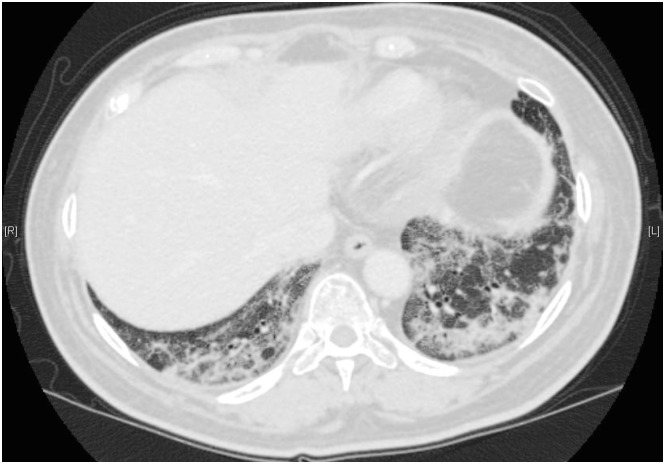
The case is a 49-year-old woman, presented in January 2020 mainly for abdominal distention, who was diagnosed with ovarian serous carcinoma after imaging and scrutiny of ascites. She underwent neoadjuvant chemotherapy because of para-aortic and closed lymph node metastasis and peritoneal dissemination, which was considered to be stage IIIC. She had diabetes mellitus, hypertension, and glaucoma. Neoadjuvant paclitaxel and carboplatin were started on February 18, the second cycle of paclitaxel and carboplatin with the addition of bevacizumab was started on March 10, and the third cycle of paclitaxel and carboplatin with bevacizumab was also given on April 2. On April 15, contrast computed tomography (CT) scan for therapeutic evaluation showed bilateral and peripheral dominant, heterogeneous ground-glass opacities and consolidation in the lower lobes of both lungs, which have been reported as images of COVID-19 pneumonia (Fig. 2). The polymerase chain reaction (PCR) testing performed the next day was negative, but considering the possibility of a false negative PCR result, we decided to take the case as COVID-19 pneumonia, although it was necessary to differentiate the drug-induced pneumonia. Because of the absence of fever and respiratory symptoms, it was decided to keep her in isolation at home, but the planned fourth cycle of paclitaxel and carboplatin therapy was postponed. We are now closely monitoring the changes in her general condition.
Fig. 2. Bilateral and peripheral dominant, ground-glass opacities and consolidation on chest computed tomography.
In this case, although there were no physical findings, a CT scan of the patient for treatment evaluation showed pneumonia with strong suspicion of COVID-19. In a report of 101 cases from China, imaging findings in COVID-19 pneumonia included ground-glass opacities (GGO) (86.1%), a mixture of GGO and consolidation (64.4%), and reticulation (48.5%), similar to typical findings in other viral pneumonias such as severe acute respiratory syndrome and Middle East respiratory syndrome [3]. Many patients also noted vascular enlargement of the lesion (71.3%), which may have been caused by acute inflammation. The lesions presented a peripheral (87.1%), bilateral (82.2%), lower lung predominant (54.5%), and multifocal (54.5%) distribution. In another report of 81 cases from China, the predominant pattern of abnormality observed was bilateral (79%), peripheral (54%), ill-defined (81%), and GGO (65%), mainly involving the right lower lobes (27%) [4]. When categorized according to the time since symptom onset, unilateral (60%), multifocal (53%), and GGO (93%) were seen in asymptomatic cases. Bilateral (90%), diffuse (52%) and GGO predominance (81%) were seen in cases within 1 week of symptom onset, while prevalence of GGO were reduced and consolidation and mixed patterns were more prevalent in cases more than one week after onset. On the other hand, the above findings are generally those of viral pneumonia and are not unique to COVID-19. Whether a patient has COVID-19 should be determined comprehensively by interview, general condition, oxygen saturation, blood test, chest CT scan, and if in doubt, by PCR testing. This case has CT findings suspicious for COVID-19 pneumonia, as described above, but the first PCR testing was negative. The pooled sensitivity was 89% for PCR [5], and the possibility of false negatives should be kept in mind. CT scan is regarded more sensitive than PCR because imaging changes can be seen even in mild cases, including asymptomatic ones [6,7].
This patient has advanced cancer and needs timely anticancer treatment, but we had to postpone treatment because of the strong suspicion of COVID-19. In particular, severe cases of COVID-19 often have underlying diseases such as hypertension, cardiovascular disease, cerebrovascular disease, and diabetes mellitus [8]. This case also had underlying disease, and more careful management was needed. We must choose a balanced cancer treatment with a strong awareness of COVID-19 by trial and error.
MANAGEMENT OF OVARIAN CANCER PATIENTS AFFECTED BY LOCAL COVID-19 STATUS
Of total 10,653 confirmed cases in Korea as of April 18, 2020, 6,830 (64.1%) were diagnosed in Daegu where the biggest clusters were reported in Korea. The number of daily new confirmed cases dropped below 20 again for the first time in 58 days after February 20 in Korea. We present two ovarian cancer patients whose treatment courses were affected by the local circumstances of COVID-19 in Daegu.
The first case was a 56-year old woman who had a diagnosis of high-grade serous ovarian cancer IIa after primary debulking surgery on October 17, 2019. There was no residual tumor after the surgery. She received the fifth cycle of adjuvant paclitaxel-carboplatin on February 2, 2020. Because of her exposure to COVID-19 confirmed patient at a nursing home in Daegu where one of the significant COVID-19 clusters occurred, she got confirmatory testing for COVID-19 and chest CT scan. Fortunately, PCR test result was reported negative and she had no relevant symptoms. However, the physician decided to postpone the sixth cycle of paclitaxel-carboplatin not only because chest CT showed abnormal finding of early atypical pneumonia (Fig. 3), but also because she visited another nursing home in Daegu against the advice of her oncologist which also had significant COVID-19 cluster. She did not resume her adjuvant chemotherapy schedule although COVID-19 was negative. Watchful monitoring and follow-up started.
Fig. 3. Early finding of atypical pneumonia, viral pneumonia on chest computed tomography.
The second case was a 65-year old woman with advanced stage ovarian cancer with peritoneal carcinomatosis and liver metastasis. At December 2, 2019, results of biopsy at seeding nodules reported malignant neoplasm, possibly low-grade serous carcinoma. She received three cycles of neoadjuvant paclitaxel-carboplatin from December 12, 2019 to January 28, 2020. Initially she was scheduled to undergo interval debulking surgery after three cycles of neoadjuvant chemotherapy. Because, however, she had close-contact with a COVID-19 confirmed patient at a nursing home in Daegu and therefore needed to enter quarantine and self-monitor for symptoms for 14 days, surgery was delayed after the completion of quarantine and continued to receive subsequent cycles (4th to 6th) of chemotherapy based on good response to chemotherapy.
Guidelines allow to consider extending the chemotherapy plan to 6 cycles before the interval cytoreductive surgery in women who have already started neoadjuvant chemotherapy despite no high-level evidence supporting this. Five cycles of adjuvant chemotherapy after optimal cytoreductive surgery without residual tumor might not damage the survival outcomes expected for this stage. Patients with most solid tumor including gynecologic cancers belong to priority B according to pandemic planning clinical guideline for patients with cancer [9]. Patients in priority B were those for whom a delay of <4 weeks from target would not be anticipated to impact significantly on survival outcomes. Patients sometimes would not listen to medical advice, especially when it is about unscheduled delay of cancer treatment. Patients' concealment or even fabrication about their history of travel and exposure brings about moral issues. These may endanger the whole medical system including patients and health care workers. Main challenges of cancer care in COVID-19 pandemic period include not only continuing the possible best treatment as long as essential precautions are undertaken but also educating patients about moral issues.
ACKNOWLEDGMENTS
We would like to thank Dr. Kosuke Tsuji (Department of Obstetrics and Gynecology) from Keio University School of Medicine, Dr. Jin Young Kim (Department of Internal Medicine) and Dr. Sojin Shin (Department of Obstetrics and Gynecology) from Keimyung University Dongsan Medical Center in Daegu, Korea, for providing cases.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: K.J.W.
- Data curation: K.Y., S.D.H.
- Methodology: K.Y., D.A., K.J.W.
- Project administration: D.A., K.J.W.
- Supervision: D.A., K.J.W.
- Writing - original draft: K.Y., S.D.H.
- Writing - review & editing: K.Y., S.D.H., D.A., K.J.W.
References
- 1.Ramirez PT, Chiva L, Eriksson AG, Frumovitz M, Fagotti A, Gonzalez Martin A, et al. COVID-19 global pandemic: options for management of gynecologic cancers. Int J Gynecol Cancer. 2020 doi: 10.1136/ijgc-2020-001419. [DOI] [PubMed] [Google Scholar]
- 2.Kimmig R, Verheijen RH, Rudnicki M, SERGS Council Robot assisted surgery during the COVID-19 pandemic, especially for gynecological cancer: a statement of the Society of European Robotic Gynaecological Surgery (SERGS) J Gynecol Oncol. 2020;31:e59. doi: 10.3802/jgo.2020.31.e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol. 2020;214:1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 4.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020 doi: 10.1148/radiol.2020201343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020:200432. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ontario Health (Cancer Care Ontario) Pandemic planning clinical guideline for patients with cancer [Internet] Toronto: Ontario Health; 2020. Mar 10, [cited 2020 Apr 23]. Available from: https://www.accc-cancer.org/docs/documents/cancer-program-fundamentals/oh-cco-pandemic-planning-clinical-guideline_final_2020-03-10.pdf. [Google Scholar]