Abstract
Background:
Increasing numbers of people with diabetes, especially those with type 1 diabetes (T1D), are using continuous glucose monitoring (CGM) systems to support their diabetes self-management, yet even so only approximately 30% of individuals with T1D meet the American Diabetes Association HbA1c target of 58 mmol/mol (7.5%) for children and 53 mmol/mol (7.0%) for adults. We aimed to produce a useful tool for people with diabetes to improve personalized understanding of CGM.
Method:
A brief leaflet titled “Guidelines to Improve Glucose Control Using CGM” was developed for people with diabetes. Semistructured interviews were held with 12 adults with T1D, focusing on their views regarding the relevance, readability, and usability of the newly revised leaflet. Participants were specifically asked to share what they would find most useful in terms of information and advice provided as well as how to make use of that in the context of their own diabetes self-management. Data were analyzed thematically and used to inform revisions of the leaflet content.
Results:
Data highlighted information and advice needs as well as personalization in terms of own diabetes management.
Conclusions:
CGM systems are associated with improved medical and psychosocial outcomes, especially when used effectively to meet the individual needs of the user. Ensuring greater understanding of the individual’s expectations when first starting CGM, matching experience and skills to meet those expectations, and tailoring use to the individual needs of each person with diabetes (PWD) are all required to achieve widespread and consistent benefit.
Keywords: engagement, type 1 diabetes, psychosocial, continuous glucose monitoring
Increasing numbers of people with diabetes, especially those with type 1 diabetes (T1D), are using continuous glucose monitoring (CGM) systems to support their diabetes self-management, yet even so only approximately 30% of individuals with T1D meet the American Diabetes Association HbA1c target of 58 mmol/mol (7.5%) for children and 53 mmol/mol (7.0%) for adults.1 Recent trials have demonstrated that CGM use contributes to improved glycemic control (including reduced glycemic variability, reduced frequency and severity of hypoglycemia and lower HbA1c) as well as enhanced quality of life.2-4 Furthermore, CGM users typically report high satisfaction with the technology, with perceived benefits outweighing perceived hassles.5,6 Still, many people find the sheer amount of data overwhelming and may find CGM use to be too stressful and/or burdensome.7 Among youths with T1D, for example, Markowitz and colleagues found that CGM use was associated with greater anxiety and depression scores than usual care.8 To be fair though, given the rapid development of different CGM systems over recent years, making meaningful comparisons across clinical trials and published research is difficult. What is clear is that CGM uptake is rapidly increasing and that effectiveness, though variable, appears to be broadly improving, especially as CGM technology has grown more reliable and accurate1,9 It is noteworthy that the increasingly simple set-up of newer CGM devices means that users do not require complex training in order to use and benefit from them; therefore, CGM uptake may increase even more substantially in the years to come. The DIAMOND trial, for example, demonstrated that simple training can be effective irrespective of education level, numeracy level or age of participants.3,4
At the present time, there are a number of different CGM systems that are available, and they differ in the degree of effort required, intrusiveness into daily life and in the degree and quality of feedback provided. In addition, some CGM systems, for example, allow CGM data to be shared with friends, families, and/or caregivers. What all of these systems have in common is the need for user engagement. More continuous wearing of CGM is—not surprisingly—associated with greater glycemic benefits.7 In addition, how frequently the individual interacts with the CGM and makes appropriate use of the data available is critical. To achieve the best from any CGM system, it is first necessary to understand what that ‘best’ looks like in the context of individualized self-management, social environment and lived experience. For some, intrusive alarms may prevent effective, long-term engagement with CGM; for others, loss of connectivity is the key frustration. Ensuring that CGM systems are initially set up for the individual and reviewed with these factors in mind, as well as exploring with the new CGM user their specific needs and how those needs will be filled are crucial to effective onboarding and use of the systems. Gehr et al10 developed a structured training program (SPECTRUM) in Germany to improve acceptance and use of CGM systems. It consists of six training modules, each approximately ninety minutes long. Our aim was to develop a brief clinical tool to assist onboarding in routine care.
Methods
A brief leaflet titled “Guidelines to Improve Glucose Control Using CGM” was developed for use by participants and healthcare professionals in the DIAMOND trial.3 The leaflet consisted of ten tips for maximizing the benefit of CGM systems. Following review after the trial, the leaflet was revised in line with feedback.
Semistructured interviews were then held with 12 adults with T1D, focusing on their views regarding the relevance, readability and usability of the newly revised leaflet. Interview scripts were piloted with potential participants prior to use and informed by current literature on the strengths and downsides of CGM systems. Participants were specifically asked to share what they would find most useful in terms of information and advice provided as well as how to make use of that in the context of their own diabetes self-management. Data were analyzed thematically and used to inform revisions of the leaflet content.
Results
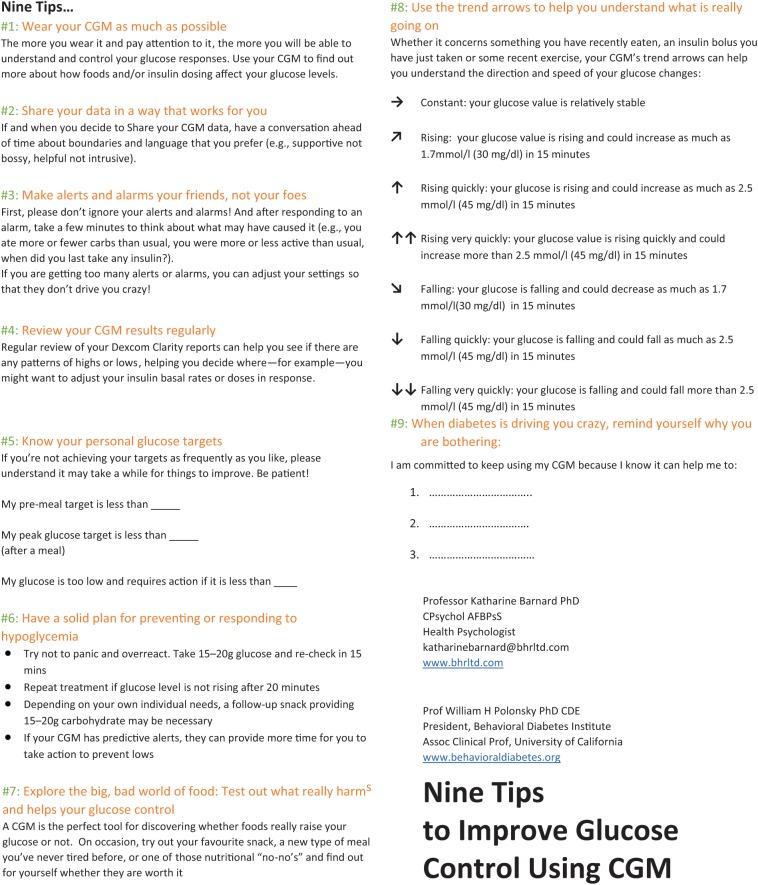
The final version of the newly revised leaflet can be found in Figure 1.
Figure 1.
Nine Tips to Improve Glucose Control Using CGM.
Following review, pilot, and rereview, the final leaflet was revised to focus on critical tips:
Tips. The number of tips or “general guidelines” was reduced to nine: (1) wear the CGM as much as possible; (2) share your data in a way that works for you; (3) make alerts and alarms your friends, not your foes; (4) review your CGM results regularly; (5) know your personal glucose targets; (6) have a solid plan for preventing or responding to hypoglycemia; (7) explore the big, bad world of food (test out what really harms and helps your glucose control); (8) use the trend arrows to help you understand what is really going on; and (9) when diabetes is driving you crazy, remind yourself why you are bothering.
Spaces are provided for recording personal glucose targets (premeal and two hours postmeal) as well as highlighting the standard suggestions for preventing or responding to low blood glucose.
Space is provided for users to identify their personal hopes and desires from using the CGM.
Trend arrows provide a visual representation of the arrows, their meaning, and how to use them alongside other relevant information.
Specific feedback from users has been that the inclusion of personalized targets and information has very much helped them reflect on current challenges and focus on use of the CGM in the context of their everyday life rather than general potential benefits of the system. The ability to include personal reasons for use and specific expectations of CGM facilitated review of those goals and whether experience matched expectation.
Conclusions
CGM systems are associated with improved biomedical and psychosocial outcomes, especially when used effectively to meet the individual needs of the user. Ensuring greater understanding of the individual’s expectations when first starting CGM, matching experience and skills to meet those expectations, and tailoring use to the individual needs of each person with diabetes (PWD) are all required to achieve widespread and consistent benefit.
Practice Implications
The Tips to Improve Glucose Control using CGM leaflet is a brief and practical tool for people with diabetes and healthcare professionals that could optimize benefit when first initiating CGM use. Critically, it can perhaps be used as a conversation starter, a useful communication tool to aid understanding of expectations of PWDs and HCPs and to target any critical skills that may need to be developed prior to onboarding CGM. It is evidence-based and freely available.
Footnotes
Abbreviations: CGM, continuous glucose monitoring; HCP, health care provider; PWD, person with diabetes; T1D, type 1 diabetes.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Katharine D. Barnard-Kelly  https://orcid.org/0000-0002-3888-3123
https://orcid.org/0000-0002-3888-3123
References
- 1. Miller KM, Foster NC, Beck RW, et al. ; T1D Exchange Clinic Network. Current state of type 1 diabetes treatment in the US: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38:971-978. [DOI] [PubMed] [Google Scholar]
- 2. Lind M, Polonsky WH, Hirsch IB, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: the GOLD randomized clinical trial. JAMA 2017;317:379-387. [DOI] [PubMed] [Google Scholar]
- 3. Beck RW, Riddlesworth T, Ruedy K, et al. Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. JAMA 2017;317:371-378. [DOI] [PubMed] [Google Scholar]
- 4. Polonsky WH, Hessler D, Ruedy KJ, Beck RW; for the DIAMOND Study Group. The impact of continuous glucose monitoring on markers of quality of life in adults with type 1 diabetes: further findings from the DIAMOND randomized clinical trial. Diabetes Care 2017;40:736–741. [DOI] [PubMed] [Google Scholar]
- 5. Polonsky WH, Hessler D. What are the quality of life-related benefits and losses associated with real-time continuous glucose monitoring? A survey of current users. Diabetes Technol Ther 2013;15:295–301. [DOI] [PubMed] [Google Scholar]
- 6. Pickup JC, Ford Holloway M, Samsi K. Real-time continuous glucose monitoring in type 1 diabetes: a qualitative framework analyses of patient narratives [published online ahead of print December 31, 2014]. Diabetes Care. doi: 10.2337/dc14-1855 [DOI] [PubMed] [Google Scholar]
- 7. Kubiak T, Mann CG, Barnard KD, Heinemann L. Psychosocial aspects of continuous glucose monitoring: connecting to the patients’ experience. J Diabetes Sci Technol. 2016:10:859-863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Markowitz JT, Pratt K, Aggarwal J, et al. Psychosocial correlates of continuous glucose monitoring use in youth and adults with type 1 diabetes and parents of youth. Diabetes Technol Ther. 2012;14:523-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Polonsky WH, Hessler D. Perceived accuracy in continuous glucose monitoring: understanding the impact on patients [published online ahead of print November 10, 2014]. J Diabetes Sci Technol. doi: 10.1177/1932296814559302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gehr B, Holder M, Kulzer B, et al. ; for the SPECTRUM Group. SPECTRUM. J Diabetes Sci Technol. 2017;11:284-289. [DOI] [PMC free article] [PubMed] [Google Scholar]