Abstract
Purpose of Review
COronaVirus Disease 2019 (COVID-19) has spread at unprecedented speed and scale into a global pandemic with cardiovascular risk factors and complications emerging as important disease modifiers. We aim to review available clinical and biomedical literature on cardiovascular risks of COVID-19.
Recent Findings
SARS-CoV2, the virus responsible for COVID-19, enters the cell via ACE2 expressed in select organs. Emerging epidemiological evidence suggest cardiovascular risk factors are associated with increased disease severity and mortality in COVID-19 patients. Patients with a more severe form of COVID-19 are also more likely to develop cardiac complications such as myocardial injury and arrhythmia. The true incidence of and mechanism underlying these events remain elusive.
Summary
Cardiovascular diseases appear intricately linked with COVID-19, with cardiac complications contributing to the elevated morbidity/mortality of COVID-19. Robust epidemiologic and biologic studies are urgently needed to better understand the mechanism underlying these associations to develop better therapies.
Keywords: COVID-19, ACE2, Cardiovascular risk factors, Mortality, Myocardial injury, Arrhythmia
Introduction
Since its first documented human infection in Wuhan, China, in the winter of 2019, SARS-CoV-2, the causal agent of COronaVIrus Disease 2019 (COVID-19) that manifests as an aggressive viral pneumonia, has spread at unprecedented speed and scale resulting in a global pandemic [1]. Despite drastic interventions implemented around the world to contain its spread, COVID-19 has progressed worldwide with significant resultant morbidity and mortality while stretching medical systems to their limits. An exponential increase of COVID-19 cases has also been observed in the USA, with over 200,000 patients confirmed as of 4/1/2020 and rapid daily growth [2]. Thus, efforts are urgently needed to better understand the epidemiology and pathobiology of this illness to limit its impact.
The overall case fatality rate (CFR) of COVID-19 is estimated to be approximately 3–4%, although large variabilities exist with the highest reported in Italy (11.9%) and the lowest in Germany (1.2%) [3]. Early epidemiologic studies emerging from China point to a strong association between advanced age and severity of illness [4]. Similar observations were made in Italy, where up to 20% CFR was noted among patients greater than 80 years old [5]. Numerous important age-associated cardiovascular comorbidities, such as hypertension and coronary heart disease, have also been linked to increased risk for worse outcomes including higher rates of ICU admissions and death [6–8]. Whether these epidemiological associations are attributed to high risk of infection among the elderly or lesser ability to recover from SARS-CoV-2 infection remain to be clarified.
In this review, we aim to highlight the pathobiology of SARS-CoV-2 and discuss its potential implications in the cardiovascular system. We then summarize the available epidemiological data with particular attention paid to cardiovascular comorbidities and outcomes. Finally, we discuss various cardiac manifestations of COVID-19.
SARS-CoV-2 Biology and Clinical Implications
Coronaviridae, a family of positive strand RNA viruses causing human respiratory infections, was named for the crown-shaped outer coat seen on the electron-microscopy. First discovered in the 1960s, it received great attention during the 2003 SARS coronavirus (SARS-CoV) outbreak. There is approximately an 80% nucleotide sequence similarity [9] between SARS-CoV and SARS-CoV-2, the pathogen of COVID-19. Hence, most of our understanding of the biology of SARS-CoV-2 has been extrapolated from prior research on the original SARS virus.
The “crown” seen on electron microscopy are protruding proteins called “spike proteins” which are essential to viral entry into human cells (Fig. 1a). Studies in mice and human cells demonstrated that the SARS virus enters into the cell via contact between the spike protein and angiotensin-converting enzyme 2 (ACE2) [10], a regulator of the renin/angiotensin pathway expressed on a subset of cell surfaces. The contact of these two proteins triggers cleavage of the viral spike protein via an enzyme transmembrane protease, serine 2 (TMPRSS2), which then activates a cascade of molecular events leading to the fusion of the viral membrane envelope with the plasma membrane of the host cells and subsequent entry of viral contents into the cytoplasm [11]. The spike protein of SARS-CoV and SARS-CoV-2 shares 76% of amino acid sequence and an overall conservation of structure [12]. In vitro studies suggest SARS-CoV-2 may have an even higher affinity towards binding of ACE2 [12], which may partially explain its higher transmission rate compared to SARS-CoV. As in SARS-CoV, in vitro studies showed SARS-CoV-2 enters the cell through ACE2, and inhibitors of the protease TMPRSS2 impairs viral entry [13••]. It is most likely that ACE2 is the primary receptor by which viral entry occurs, but whether additional receptors exist for SARS-CoV-2 remains unknown.
Fig. 1.
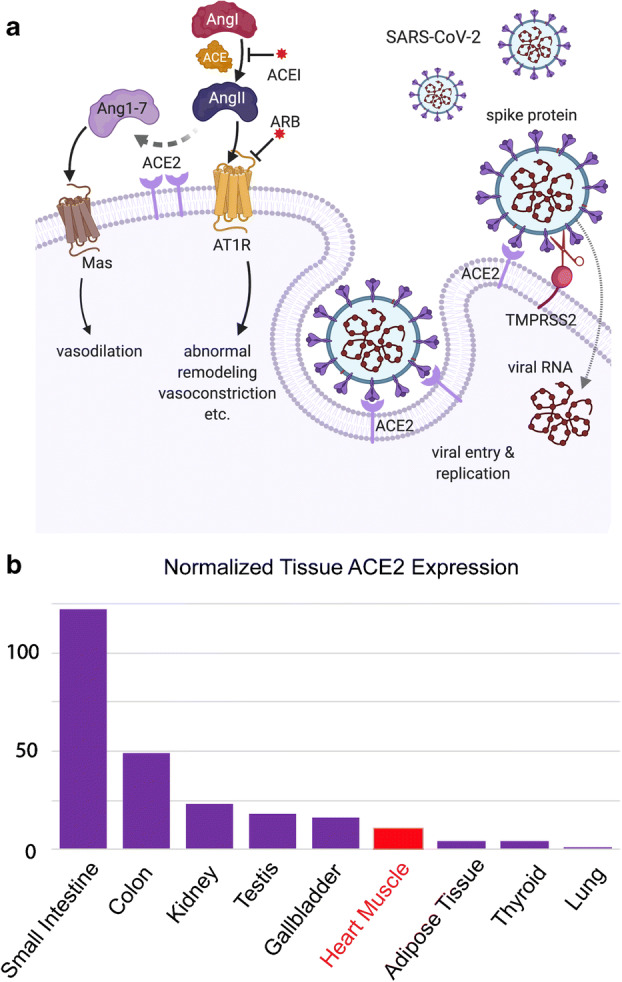
The role of ACE2 in COVID-19. a The spike protein of SARS-CoV-2 binds ACE2 on a cellular membrane, which triggers 1) endocytosis of the virus and subsequent sequestration of ACE2 or 2) cleavage of the viral spike protein via an enzyme TMPRSS2 leading to the entry of viral contents into the cytoplasm. b Normalized RNA expression of different tissue types from three transcriptomics datasets (HPA, GTEx, and FANTOM5) shows significant ACE2 expression in GI organs, the kidney, and the heart
Given the likely importance of ACE2 in pathogenesis of COVID19 and the respiratory tract being the primary site of viral entry into the body, investigators have focused on type 2 pneumocytes in alveoli as the presumed target cells of SARS-CoV-2, given that these cells express the highest level of ACE2 and TMPRSS2 in the human lung [14]. The viral infection and injury of these pneumocytes are thought to be central to the prominent diffuse alveolar damage seen on pathology of patients with COVID19. Interestingly, ACE2 expression is low in the lower airways [15], but more elevated in nasal ciliated and goblet cells, which may explain the symptom of anosmia which has been recently reported by Brann et al. [16]. At the organ level, however, respiratory tissue carries significantly less ACE2 (by 10–100-fold) than the digestive organs, kidneys, and heart (Fig. 1b) [17]. The high expression of ACE2 in the GI tract was thought to explain the frequent occurrence of GI symptoms with SARS. However, while GI symptoms are present in COVID-19 patients, they do not appear to be as frequent compared to SARS [18], suggesting key vector-specific differences in tissue tropism. There are reports, however, of detection of viral RNA in the stool of asymptomatic patients, which raises the possibility of additional routes of asymptomatic spread [19]. The relatively elevated expression of ACE2 levels in the heart compared to the lungs also lends biological plausibility for the perceived elevated incidence of cardiac injuries seen in COVID-19 patients.
The central role of ACE2 in viral entry in combination with reported worse outcomes seen in patients with hypertension and diabetes fueled much of the speculation that ACE inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), both commonly used by hypertensive or diabetic patients, may play a role in the observed increased risk. The evidence was mostly based on studies that have demonstrated a moderate increase in Ace2 expression in the mouse heart treated with ACEIs [20]. However, there is no such report of ACE2 level alterations in the lungs thus far. While theoretically, increased ACE2 expression in the lungs may lead to worsened viral entry, the potential worsening of respiratory status and progression to ARDS in hypertensive and diabetic patients taking ACE inhibitors remains speculative. In addition, ACE2 is thought to be potentially protective in acute lung injury and ARDS, as the genetic knockout of Ace2 in rodents results in worsened lung injury, and overexpression of Ace2 in the lung is protective [21]. This protective role of ACE2 is hypothesized to be due to modulation of the angiotensin response to lung, immune, and vascular cells within the pulmonary system [22]. To address the role of angiotensin in lung injury, there is an ongoing clinical trial to examine whether losartan treatment affects outcomes in COVID-19 associated ARDS (NCT04312009). Given the known benefit of ACEI/ARB treatment in patients with diabetes mellitus, heart failure, and hypertension, many societies including the American College of Cardiology, American Heart Association, Heart Failure Society of American, and the European Society of Cardiology have released statements to advise against discontinuation of these medications in COVID-19 patients until more data are available [23].
Cardiovascular Comorbidities and COVID-19 Outcomes
Recent epidemiological studies in China have reported a heightened risk of COVID-19 related complications in patients with pre-existing cardiovascular diseases and relevant risk factors (Table 1) [5, 6, 8, 24–26••]. While variabilities exist among reported studies, rates of hypertension, diabetes mellitus, and coronary heart disease appear to be higher among those with worse outcomes from COVID-19. Most notably, Guan et al. [26••] pooled data of laboratory confirmed 1099 COVID-19 patients from 552 hospitals in 30 provinces in China through January 2020 and found that rates of hypertension (23.7% vs 13.4%) and diabetes (15.2% vs 5.7%) were significantly higher among patients with severe vs non-severe pneumonia. A similar trend existed regarding primary endpoints defined as admission to an intensive care unit, the use of mechanical ventilation, or death (35.8% vs 13.7% for hypertension, 26.9% vs 6.1% for diabetes). Active smoking, which has adverse effects on both cardio and pulmonary systems, was also associated with worse composite outcomes (25.8% vs 11.8%). While overall rates were low, pre-existing coronary heart disease was also more prevalent among those with a severe form of pneumonia (5.8% vs 1.8%). These findings were replicated in several additional studies (Table 1). However, these results were not adjusted for age or other relevant variables and therefore caution is needed when interpreting these results. Additionally, it is unclear if being more ill affected the accuracy of documented risk factors, as the overall incidences of hypertension and smoking observed are significantly lower than those seen in other large general Chinese cohort studies [27]. While limited, preliminary data from the USA and Italy also suggest higher prevalence of underlying cardiovascular diseases in patients with poor outcomes [5, 25].
Table 1.
Summary of reported rates of cardiovascular comorbidities and outcomes after COVID-19
| Paper | Study population | Rates of cardiovascular comorbidities | |||
|---|---|---|---|---|---|
| Guan et al. | 1099 patients from 552 hospitals in 30 regions in China | Breakdown | All (1099) | non-severe (926) | Severe (173) |
| Age | 47yo | 45yo | 52yo | ||
| HTN | 165 (15%) | 124 (13.4%) | 41 (23.7%) | ||
| Coronary heart disease | 27 (2.5%) | 17 (1.8%) | 10 (5.8%) | ||
| Wang et al. | 138 patients in Zhongnan hosp in Wuhan | Breakdown | All (138) | no-ICU (102) | ICU (36) |
| Age | 56yo | 51yo | 66yo | ||
| HTN | 43 (31.2%) | 22 (21.6%) | 21 (58.3%) | ||
| Cardiovascular disease | 20 (14.5%) | 11 (10.8%) | 9 (25%) | ||
| Wu et al. | 201 patients in Wuhan Jinyintan hosp | Breakdown | All (201) | no-ARDS (117) | ARDS (84) |
| Age | 51yo | 48yo | 58.5yo | ||
| HTN | 39 (19.4%) | 16 (13.7%) | 23 (27.4%) | ||
| Cardiovascular disease | 8 (4%) | 3 (2.6%) | 5 (6.0%) | ||
| Zhou et al. | 191 patients in Jinyintan hosp and Wuhan Pulmonary hosp | Breakdown | All (191) | survivors (137) | non-survivors (137) |
| Age | 56yo | 52yo | 69yo | ||
| HTN | 58 (30%) | 32 (23%) | 26 (48%) | ||
| Cardiovascular disease | 15 (8%) | 2 (1%) | 13 (24%) | ||
| Onder et al. | 355 pts. died of COVID-19 in italy | mean age | 79.5yo | ||
| Ischemic heart disease | 117 (30%) | ||||
| atrial fibrillation | 87 (24.5%) | ||||
| Arentz et al. | 21 pts. in ICU, Evergreen hosp, WA, US | Congestive heart failure | 9 (42.9%) | ||
Cardiac Complications of COVID-19
Initial reports from Wuhan noted a significant association of the presence of cardiac complications with overall mortality in COVID-19 patients [7]. Notably, Ruan Q et al. showed that among those who died due to COVID-19, the cause of death was respiratory failure and myocardial injury in 33% (22/68) of the patients and primary myocardial injury and/or heart failure in 7% of the patients [7]. These observations were further corroborated in a study by Shi et al. [28•] who showed higher rates of ventilator requirement and in-hospital mortality in those with cardiac injury. In their Cox regression model, patients with cardiac injury were at a higher risk of death throughout the disease course compared to those without. Given these observations, much focus has been placed on better understanding cardiovascular sequelae of COVID19. The observed cardiovascular complications associated with COVID-19 can be roughly characterized into 1: myocardial injury and heart failure 2: arrhythmias.
Myocardial Injury and Heart Failure
Several published and unpublished case series have documented elevated serum troponin levels in a significant fraction (5–7%) of hospitalized COVID-19 patients [1, 8]. While the degree of troponin elevation was mild in the majority of cases, the presence of myocardial injury (as manifested by troponins above the upper range of normal) was associated with a significantly worse prognosis [28•]. It remains unclear whether the association with worse outcomes is simply reflective of selection of an older, sicker population more prone to demand ischemia with metabolic compromise during critical illness or direct myocardial injury caused by the virus or its inflammatory sequelae (Fig. 2). Relatively high levels of ACE2 protein expression on cardiomyocytes may theoretically lead to increased risk of viral susceptibility and virus mediated injury. However, while there are anecdotal reports of clinical presentations consistent with myocarditis [29•], significant incidence of myocarditis has not been reported in any larger case series thus far. To date, there has been very limited pathologic or radiologic proof of myocarditis as a direct sequelae of COVID-19. Determining the true prevalence of these events is critical. Alternatively, the observed incidence of myocardial injury could be due to the increased risk of myocardial ischemic insult due to the poorly understood pleiotropic pro-thrombotic inflammatory sequelae from viral infections. An increased risk of myocardial infarction as determined by serological evidence of myocardial injuries has been well-documented in influenza infections at similar prevalence [30–32]. This would suggest that the intravascular prothrombotic effect observed in COVID-19 patients is the consequence of the overall inflammatory state rather than a COVID19-specific phenomenon.
Fig. 2.
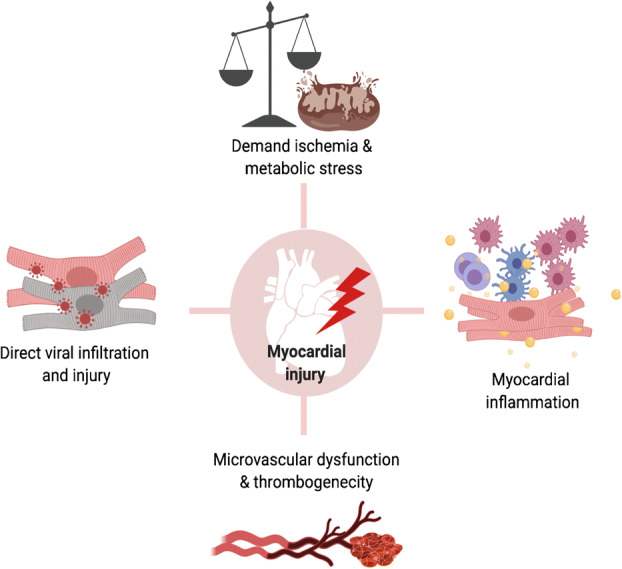
Potential mechanisms for myocardial injury caused by COVID-19
Regardless of the cause of myocardial injuries, early case reports of critically ill patients have found a significant fraction of patients developing clinical heart failure. Zhou et al. from Wuhan found that 28/54 of those who succumbed to the disease had heart failure—albeit the definition of “heart failure” employed was not stated, and a broad definition of acute cardiac injury (cardiac biomarkers > 99th percentile of the upper reference limit or new abnormalities on EKG or echocardiography) was used in this study. The case series of critically ill patients from Seattle showed cardiomyopathy in 7/21 patients, as defined by globally reduced left ventricular ejection function or decreased central venous saturation to < 70% [25]. While the frequency of patient with cardiac dysfunction is notable in these reports, some limitations such as small sample size, very high (44%) baseline history of “CHF”, and the lack of clearly defined criteria for heart failure limit the generalizability of these studies. It is worth noting that high incidence of heart failure was not mentioned in a larger case series from China [26••] nor in the Italian experience thus far [33].
Arrhythmia
A published study and additional anecdotal reports have highlighted the presence of arrhythmia and even sudden cardiac death in critically ill COVID-19 patients. The first case series out of Wuhan documented 16.7% and 44% incidence of arrhythmia in those hospitalized for COVID-19 and admitted to the ICU respectively [8]. Unfortunately, the exact nature of the arrhythmias was not detailed in this study. Interestingly, a high incidence of arrhythmias was not reported in several subsequent larger case series from China [26••]. One would expect a majority of the reported arrhythmias are atrial, as similarly elevated rates of atrial arrhythmia were seen in longitudinal studies on Medicare patients hospitalized with sepsis [34]. It remains to be determined whether a significant portion of COVID-19 patients have hemodynamically significant ventricular arrhythmias. The high prevalence of myocardial injury may itself increase life-threatening arrhythmias and contribute to worse outcomes. More definitive epidemiologic data is urgently needed. Of note, some of the therapies empirically used to treat SARS-CoV-2 infections such as chloroquine, have known effects on myocyte repolarization [35], resulting in increased risk of QT prolongation and subsequent arrhythmia. Given the high incidence of electrolyte abnormalities in ill patients, high vigilance by the treatment teams is required to avoid iatrogenic harm.
Conclusion
COVID 19, the viral illness caused by SARS-CoV2, continues to spread across the world with alarming speed and a reported case fatality rate of ~ 3–4% worldwide without any proven therapies. The virus’s port of entry into human cells, ACE2, is expressed in the myocardium, but whether direct viral damage is contributing to the disease remains unknown. Anecdotal reports and small case series have suggested an increased risk of myocardial injury, arrhythmia, and heart failure as sequelae of the disease, but more concrete epidemiological evidence is required to confirm these findings. There is strong evidence that those with underlying cardiovascular disease and risk factors are at much higher risk for worse outcomes from SARS-CoV-2 infections, but whether this is causal or simply an association remains elusive. Given that we currently have no proven effective therapy against SARS-CoV2, understanding the root cause of this association is particularly critical, as it may lead to avenues for intervention. In the meantime, keeping human-to-human transmission rates as low as possible through numerous interventions around the world is our only hope to prevent healthcare systems from being overwhelmed and to buy us time for effective therapies to be developed.
Acknowledgments
We thank all frontline healthcare workers who have been working tirelessly and courageously to care for patients with COVID-19. Part of the figures were created with the aid of BioRender.
Compliance with Ethical Standards
Conflict of Interest
June-Wha Rhee, Paul Cheng, Han Zhu, Ronald M. Witteles, Thomas Quertermous, Joseph C. Wu, and Sean M. Wu declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Paul Cheng, Email: chengpa@stanford.edu.
Han Zhu, Email: hanzhu@stanford.edu.
Ronald M. Witteles, Email: witteles@stanford.edu
Joseph C Wu, Email: joewu@stanford.edu.
Thomas Quertermous, Email: tomq1@stanford.edu.
Sean M. Wu, Email: smwu@stanford.edu
June-Wha Rhee, Email: jwrhee@stanford.edu.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC Coronavirus Disease 2019 (COVID-19) Cases in U.S. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [Accessed March 31, 2020].
- 3.Johns Hopkins University COVID-19 Map - Johns Hopkins Coronavirus Resource Center. Available at: https://coronavirus.jhu.edu/map.html [Accessed March 31, 2020].
- 4.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020. [DOI] [PubMed]
- 5.Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020. [DOI] [PubMed]
- 6.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020. [DOI] [PMC free article] [PubMed]
- 7.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020. [DOI] [PMC free article] [PubMed]
- 8.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020. [DOI] [PMC free article] [PubMed]
- 9.Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, Si H-R, Zhu Y, Li B, Huang C-L, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, Huan Y, Yang P, Zhang Y, Deng W, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsuyama S, Nagata N, Shirato K, Kawase M, Takeda M, Taguchi F. Efficient activation of the severe acute respiratory syndrome coronavirus spike protein by the transmembrane protease TMPRSS2. J Virol. 2010;84:12658–12664. doi: 10.1128/JVI.01542-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.•• Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020; In vitro study demonstrating critical roles of ACE2 MPRSS2 in SARS-CoV-2 cell entry. [DOI] [PMC free article] [PubMed]
- 14.Zhao Y, Zhao Z, Wang Y, Zhou Y, Ma Y, Zuo W. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 15.Sungnak, W., Ni, H., Bécavin, C., Berg, M., and Lung, H. C. A. (2020). Ciliated Cells within Human Airways. arXiv:2003.06122.
- 16.Brann D, Tsukahara T, Weinreb C, Logan DW, Datta SR. Non-neural expression of SARS-CoV-2 entry genes in the olfactory epithelium suggests mechanisms underlying anosmia in COVID-19 patients. BioRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 17.The Human Protein Atlas ACE2. Available at: https://www.proteinatlas.org/ENSG00000130234-ACE2/tissue [Accessed April 1, 2020].
- 18.Leung WK, To K-F, Chan PKS, Chan HLY, Wu AKL, Lee N, Yuen KY, Sung JJY. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology. 2003;125:1011–1017. doi: 10.1016/j.gastro.2003.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020. [DOI] [PMC free article] [PubMed]
- 20.Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, Diz DI, Gallagher PE. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111:2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 21.Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, Yang P, Sarao R, Wada T, Leong-Poi H, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li Y, Zeng Z, Cao Y, Liu Y, Ping F, Liang M, Xue Y, Xi C, Zhou M, Jiang W. Angiotensin-converting enzyme 2 prevents lipopolysaccharide-induced rat acute lung injury via suppressing the ERK1/2 and NF-κB signaling pathways. Sci Rep. 2016;6:27911. doi: 10.1038/srep27911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.HFSA/ACC/AHA, Joint Statement addressing concerns re: using RAAS antagonists in COVID-19. Available at: https://www.hfsa.org/patients-taking-ace-i-and-arbs-who-contract-covid-19-should-continue-treatment-unless-otherwise-advised-by-their-physician/ [Accessed April 1, 2020].
- 24.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in wuhan, china. JAMA Intern Med. 2020. [DOI] [PMC free article] [PubMed]
- 25.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA. 2020. [DOI] [PMC free article] [PubMed]
- 26.•• Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; A pooled analysis of 1000+ COVID-19 confirmed Chinese patients detailing their baseline characteristics and their association with clinical outcomes.
- 27.Liu J, Hong Y, D’Agostino RB, Wu Z, Wang W, Sun J, Wilson PWF, Kannel WB, Zhao D. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004;291:2591–2599. doi: 10.1001/jama.291.21.2591. [DOI] [PubMed] [Google Scholar]
- 28.• Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020; A first survival analysis demonstrating worse outcomes among those with cardiac injury. [DOI] [PMC free article] [PubMed]
- 29.• Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020; First case report describing fulminant viral myocarditis caused by COVID-19.
- 30.Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, Katz K, Ko DT, McGeer AJ, McNally D, et al. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection. N Engl J Med. 2018;378:345–353. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 31.Harris JE, Shah PJ, Korimilli V, Win H. Frequency of troponin elevations in patients with influenza infection during the 2017-2018 influenza season. Int J Cardiol Heart Vasc. 2019;22:145–147. doi: 10.1016/j.ijcha.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ludwig A, Lucero-Obusan C, Schirmer P, Winston C, Holodniy M. Acute cardiac injury events ≤30 days after laboratory-confirmed influenza virus infection among U.S. veterans, 2010-2012. BMC Cardiovasc Disord. 2015;15:109. doi: 10.1186/s12872-015-0095-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grasselli G, Pesenti A, Cecconi M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA. 2020. [DOI] [PubMed]
- 34.Walkey AJ, Hammill BG, Curtis LH, Benjamin EJ. Long-term outcomes following development of new-onset atrial fibrillation during sepsis. Chest. 2014;146:1187–1195. doi: 10.1378/chest.14-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Traebert M, Dumotier B, Meister L, Hoffmann P, Dominguez-Estevez M, Suter W. Inhibition of hERG K+ currents by antimalarial drugs in stably transfected HEK293 cells. Eur J Pharmacol. 2004;484:41–48. doi: 10.1016/j.ejphar.2003.11.003. [DOI] [PubMed] [Google Scholar]


