Abstract
Acute respiratory distress syndrome (ARDS) is a devastating clinical manifestation of COVID-19 pneumonia and is mainly based on an immune-driven pathology. Mounting evidence suggests that COVID-19 is fueled by a maladaptive host inflammatory response that involves excessive activation of innate immune pathways. While a “cytokine storm” involving IL-6 and other cytokines has been documented, complement C3 activation has been implicated as an initial effector mechanism that exacerbates lung injury in preclinical models of SARS-CoV infection. C3-targeted intervention may provide broader therapeutic control of complement-mediated inflammatory damage in COVID-19 patients. Herein, we report the clinical course of a patient with severe ARDS due to COVID-19 pneumonia who was safely and successfully treated with the compstatin-based complement C3 inhibitor AMY-101.
1. Introduction
The recently declared global emergency following the outbreak of SARS-CoV-2 has raised awareness about tackling COVID-19, the disease caused by SARS-CoV-2, with more effective therapeutic means. While complement is considered a first-line defense against invading pathogens [1], including viral infections, recent evidence has strikingly suggested that complement activation can promote severe acute respiratory syndrome (SARS) coronavirus pathogenesis [2,3]. Indeed, blocking C3 activation or downstream effector generation can significantly attenuate the lung-directed proinflammatory sequelae of coronavirus (CoV) infections, including MERS-CoV or SARS-CoV, limiting the pathological changes that impose a high burden on CoV-infected patients [2,4]. Both the genetic absence of C3 and blockade of downstream complement effectors, such as C5a/C5aR1, have shown therapeutic promise by containing the detrimental proinflammatory consequences of viral spread mainly via inhibition of monocyte/neutrophil activation and immune cell infiltration into the lungs [2,4].
Acute respiratory distress syndrome (ARDS) is mainly based on an immune-driven pathology that is observed in severe cases of COVID-19 [5]. The deregulated activation of multiple innate immune pathways, including the complement system, the cytokine circuitry, and several procoagulant and thrombogenic pathways, is believed to fuel a hyper-inflammatory state that drives ARDS and may lead to multiple organ injury in COVID-19 [3,6,7].
C3 activation is positioned upstream of these proinflammatory innate immune circuits that contribute to thromboinflammation and organ damage in COVID-19 [3]. Therefore, C3 interception could be a promising approach to broadly inhibit complement activation and contain systemic, complement-mediated inflammatory reactions that may fuel tissue destructive inflammation in COVID-19 patients.
A new generation of highly selective and potent C3 inhibitors, termed compstatins Cp40/AMY-101, are clinically developed by Amyndas Pharmaceuticals for various complement-mediated indications [[8], [9], [10], [11], [12], [13], [14]]. These small-sized peptidic C3 inhibitors are primate/human-specific and display more favorable pharmacological profiles and a greater tissue-penetrating capacity than larger biologics, such as the complement inhibitor TP-10, previously evaluated as a treatment option for ARDS [15]. The C3-targeted therapeutic AMY-101 is currently in Phase II clinical trials having shown good safety and tolerability in human volunteers in a Phase I study [11] [16,17]. In light of the recent evidence linking C3 activation to a systemic proinflammatory response in SARS-CoV infection, AMY-101 could form a unique base for developing adjunctive anti-inflammatory therapies to counteract the emerging COVID-19 outbreak [3].
Recent clinical developments further supporting the therapeutic merit of complement inhibition as a potential anti-inflammatory therapy in COVID-19 include the report of five cases of COVID-19 patients associated with pronounced systemic complement activation, complement-mediated microvascular injury and coagulopathy [18], and a recent preprint reporting complement activation in lung biopsies and serum from COVID19 patients hospitalized during the recent SARS-CoV-2 outbreak in China [19]. While this is only a preliminary analysis that remains to be confirmed by larger studies, the immediate clinical improvement resulting from anti-C5a blockade in two COVID-19 patients has prompted the further investigation of this route of complement therapeutic targeting [19]. In this regard, clinical trials aiming to evaluate the safety and efficacy of various complement targeting approaches in COVID-19 patients are now listed in international registries (clinicaltrials.gov).
Given that C3 interception with compstatin-based inhibitors (such as AMY-101) may offer broader therapeutic coverage than anti-C5 or anti-C5a agents by blocking simultaneously generation of all downstream proinflammatory mediators involved in SARS-CoV-2-induced ARDS and thrombotic microangiopathies, AMY-101 is well poised for clinical evaluation as an anti-inflammatory agent in severe cases of COVID-19 infection [3].
2. Case presentation
Patient #1 is a 71-year-old Caucasian male, who was admitted in the hospital for critical limb ischemia of the right leg requiring surgery. He had a meaningful past medical history, due to history of atrial fibrillation (resolved at the time of hospitalization), hypercholesterolemia and hypertension, associated with multiple arterial complications and mild kidney failure. Indeed, the patient had coronary artery disease requiring 5 stents, and then the recent peripheral arterial disease treated with embolectomy by Fogarty catheter. During the hospitalization, on April 6th the patient was diagnosed with bilateral interstitial pneumonia (see chest X-ray, Fig. 1 ), that was eventually demonstrated to have been caused by SARS-CoV-2 infection. Because of severe hypoxia irrespective of oxygen support through standard Ventimask, the patient had to start non-invasive mechanical ventilation (NIV) with Continuous Positive Air-Pressure (C-PAP) with 60% of Fraction of Inspired Oxygen (FIO2) given in 2 h cycles every 12 h. At this time, his arterial oxygen pressure (PaO2) and his blood oxygen saturation (SpO2) were 65 mmHg and 93%, respectively; the patient had increased C-reactive protein (CRP, 63 mg/L), increased lactate de‑hydrogenase (LDH, 466 UI/L), leukocytosis (16.9 g/L) and lymphocytopenia. Patient's performance status (PS, using the Eastern Cooperative Oncology Group [ECOG] scale) was 3. In consideration of the Acute Respiratory Distress Syndrome (ARDS) due to SARS-CoV-2, the patient was considered a candidate for experimental treatments for Coronavirus Disease 2019 (COVID-19), including the complement C3 inhibitor AMY-101, available at the San Raffaele Hospital. AMY-101 is available at the San Raffaele Hospital within a compassionate use program sponsored by Amyndas Pharmaceuticals S.A, which was approved by the Institutional Review Board (IRB) of San Raffaele Hospital on March 25th.
Fig. 1.
A. Chest X-ray at enrollment. The X-ray demonstrates the bilateral infiltration of the lungs leading to the diagnosis of bilateral interstitial pneumonia. B. Chest X-ray on day 19. The X-ray demonstrates a marked improvement of pneumonia with re-expansion of the lungs, bilaterally.
On April 8th, the AMY-101 compassionate use was discussed with the patient, who expressed his willingness to be included in the program. After having signed the IRB approved informed consent, the patient was enrolled in the AMY-101 compassionate use program. The patient was not treated with specific antiviral therapy, whereas antibacterial prophylaxis with piperacilline/tazobactam was added 2 days before the start of AMY-101 administration and continued for the entire treatment period. April 10th was the day that the AMY-101 treatment started; at baseline, the patient was in poor general clinical conditions, with severe fatigue, severe tachypnea (>35 respiratory acts per minute), and persistent dry cough. Pulmonary auscultation revealed mid-inspiratory and expiratory coarse crackles, bilateral. He was in severe ARDS, requiring C-PAP cycles (2 h every 12 h) alternating to oxygen support through Ventimask with 60% FIO2. His lung parameters at baseline, with FIO2 60%, were as follows: PaO2 89 mmHg, PaCO2 36 mmHg, SpO2 96%, pH 7,5, PaO2/FIO2 148 mmHg. Blood tests were as follows: white blood cells (WBC) 11.6 × 109/L, absolute neutrophil count (ANC) 8.6 × 109/L, absolute lymphocyte count (ALC) 1.6 × 109/L, CRP 94.2 mg/L, LDH 306 UI/l, C3 plasma level 1.81 g/L. Additional lab testing demonstrated mild renal function impairment and grade I transaminase elevation. Glasgow Coma Scale (GCS) and quick Sequential Organ Failure Assessment (qSOFA) score were 15 and 1 (for respiratory rate > 22/min), respectively.
AMY-101 was given intravenously (IV) through a peripheral vein infusion at dose of 5 mg/kg mg/Kg/day, given as initial loading dose administered in 6 h; no side effects were recorded after the loading dose. Immediately after the completion of the loading dose, 13 maintenance doses were administered as 24-h continuous infusions, for a 14-day treatment period. No infusion reactions were reported during the whole duration of the therapy; notably, the experimental treatment did not worsen renal and hepatic function.
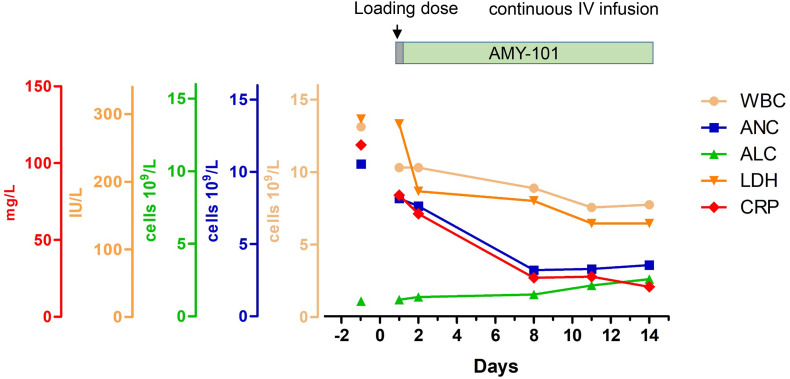
After 48 h from the initiation of AMY-101 treatment, the patient showed a dramatic improvement of all parameters that were abnormal at baseline, resulting in the quick resolution of the broad inflammatory response associated with COVID-19. In particular, CRP and LDH progressively normalized, while leukocytosis and lymphocytopenia improved more slowly but progressively (Fig. 2 ). These laboratory findings were associated with a significant improvement of respiratory performance with a gradual decrease of oxygen requirement (Fig. 3 ). Starting from April 18th (Day 9) a progressive weaning from oxygen supplementation was allowed. C-PAP was initially reduced to alternate day cycles, and then discontinued on April 20th (Day 11 of AMY 101 treatment). Similarly to the progressive and continuous improvement of blood tests, the lung function also continued to improve: indeed, the day after C-PAP discontinuation the patient's oxygen requirement diminished, with FIO2 reducing from 40% to 31% and then 28%, without desaturation (Fig. 3). Interestingly, lung functional improvement was not associated with major changes by imaging: indeed, the bilateral interstitial pneumonia was still observed by a chest X-ray performed on April 16th (Day 7), and by a subsequent CT scan performed on April 20th (Day 11), that showed also a mild right pleural effusion.
Fig. 2.
Biomarkers of systemic inflammation during AMY-101 treatment. Changes of biomarkers of systemic inflammation during the 14-day treatment period; WBC: white blood cells; ANC: absolute neutrophil count; ALC: absolute lymphocyte count; LDH: lactate de‑hydrogenase; CRP: C-reactive protein.
Fig. 3.
Changes of lung function during the 14-day treatment period, displayed as need of oxygen support; Panel A: Continuous Positive Air-Pressure, measured as hours of C-PAP per 12 h; Panel B: % pf Fraction of Inspired Oxygen in Ventimask.
At the end of AMY-101 treatment on April 23rd (day 14), with Ventimask at 28% FIO2, the patient had SpO2 98%, normal respiratory rate and normal lung auscultation, in absence of any respiratory symptom. Blood tests were as follows (Fig. 2): WBC 8.7 × 109/L, ANC 4.0 × 109/L, ALC 2.9 × 109/L, CRP 23.4 mg/L, LDH 145 U/L, C3 1.74 g/L. The patient had just mild fatigue, with ECOG performance status improved to 1, overall demonstrating a significant clinical improvement which is anticipated to result to the quick resolution of COVID without any further complications. Notably, the concomitant critical limb ischemia of both legs has not worsened (no abnormalities reported at arterial and venous ultrasound imaging performed on April 25th), and no clinical or laboratory signs of cardiovascular complication occurred, including thrombotic microangiopathy. At the latest follow up on April 28th (day 19) general conditions are further improved: the patient is afebrile, without any need of oxygen support (withdrawn on day 18). Indeed, his SpO2 in room air is 94%, with normal respiratory rate and no respiratory symptom; at this time the chest X-ray shows a marked improvement of pneumonia with re-expansion of the lungs, bilaterally (Fig. 1B).
3. Conclusions
Treatment with the compstatin-based C3 inhibitor AMY-101 is safe, and associated with a favorable course in a patient with COVID-19 severe pneumonia with systemic hyper inflammation. These early clinical results indicate that C3 inhibition holds potential as a novel anti-inflammatory therapy in COVID-19 and pave the way for systematic prospective trials.
Disclosure statement
J.D.L. is the founder of Amyndas Pharmaceuticals, which is developing complement inhibitors for therapeutic purposes and is the inventor of patents or patent applications that describe the use of complement inhibitors for therapeutic purposes some of which are developed by Amyndas. J.D.L. is also the inventor of the compstatin technology licensed to Apellis Pharmaceuticals (i.e., 4(1MeW)7W/POT-4/APL-1 and PEGylated derivatives such as APL-2/pegcetacoplan). A.M.R. has received research support from Alexion, Novartis, Alnylam and Rapharma, lecture fees from Alexion, Novartis, Pfizer and Apellis, served as member of advisory/investigator board for Alexion, Achillion, Apellis, Biocryst, Novartis, Roche, Samsung and Sanofi, and served as consultant for Amyndas, Novartis and Omeros. D.Y. is the Managing Director of Amyndas Pharmaceuticals which is developing complement inhibitors for therapeutic purposes. The other authors declare no competing interests.
Acknowledgements
This work was supported by grants from the US National Institutes of Health (AI068730; to J.D.L.), grant No DFG SFB1149 A01 (to M.H-L.), the Institutional National 5x1000 Grant (to F.C.) and the Dolce&Gabbana Fashion Firm (to C.G.). J.D.L. also thanks R. and S. Weaver for the generous endowment of his professorship.
References
- 1.Reis E.S., Mastellos D.C., Yancopoulou D., Risitano A.M., Ricklin D., Lambris J.D. Applying complement therapeutics to rare diseases. Clin. Immunol. 2015;161:225–240. doi: 10.1016/j.clim.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gralinski L.E., Sheahan T.P., Morrison T.E., Menachery V.D., Jensen K., Leist S.R., Whitmore A., Heise M.T., Baric R.S. Complement activation contributes to severe acute respiratory syndrome coronavirus pathogenesis. MBio. 2018;9 doi: 10.1128/mBio.01753-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Risitano A.M., Mastellos D.C., Huber-Lang M., Yancopoulou D., Garlanda C., Ciceri F., Lambris J.D. Complement as a target in COVID-19? Nat. Rev. Immunol. 2020;2020:1–2. doi: 10.1038/s41577-020-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiang Y., Zhao G., Song N., Li P., Chen Y., Guo Y., Li J., Du L., Jiang S., Guo R., Sun S., Zhou Y. Blockade of the C5a-C5aR axis alleviates lung damage in hDPP4-transgenic mice infected with MERS-CoV article. Emerg. Microbes Infect. 2018;7 doi: 10.1038/s41426-018-0063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thompson B.T., Chambers R.C., Liu K.D. Acute respiratory distress syndrome. N. Engl. J. Med. 2017;377:562–572. doi: 10.1056/NEJMra1608077. [DOI] [PubMed] [Google Scholar]
- 6.Campbell C.M., Kahwash R. Will complement inhibition be the new target in treating COVID-19 related systemic thrombosis? Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047419. [DOI] [PubMed] [Google Scholar]
- 7.Ciceri F., Beretta L., Scandroglio A.M., Colombo S., Landoni G., Ruggeri A., Peccatori J., D’Angelo A., De Cobelli F., Rovere-Querini P., Tresoldi M., Dagna L., Zangrillo A. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit. Care Resusc. 2020 doi: 10.51893/2020.2.pov2. http://www.ncbi.nlm.nih.gov/pubmed/32294809 (accessed April 27, 2020), Ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mastellos D.C., Yancopoulou D., Kokkinos P., Huber-Lang M., Hajishengallis G., Biglarnia A.R., Lupu F., Nilsson B., Risitano A.M., Ricklin D., Lambris J.D. Compstatin: a C3-targeted complement inhibitor reaching its prime for bedside intervention. Eur. J. Clin. Investig. 2015;45:423–440. doi: 10.1111/eci.12419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindorfer M.A., Cook E.M., Reis E.S., Ricklin D., Risitano A.M., Lambris J.D., Taylor R.P. Compstatin Cp40 blocks hematin-mediated deposition of C3b fragments on erythrocytes: implications for treatment of malarial anemia. Clin. Immunol. 2016;171:32–35. doi: 10.1016/j.clim.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berger N., Alayi T.D., Resuello R.R.G., Tuplano J.V., Reis E.S., Lambris J.D. New Analogs of the complement C3 inhibitor compstatin with increased solubility and improved pharmacokinetic profile. J. Med. Chem. 2018;61:6153–6162. doi: 10.1021/acs.jmedchem.8b00560. [DOI] [PubMed] [Google Scholar]
- 11.Mastellos D.C., Ricklin D., Lambris J.D. Clinical promise of next-generation complement therapeutics. Nat. Rev. Drug Discov. 2019;18:707–729. doi: 10.1038/s41573-019-0031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mastellos D.C., Reis E.S., Biglarnia A.-R., Waldman M., Quigg R.J., Huber-Lang M., Seelen M.A., Daha M.R., Lambris J.D. Taming hemodialysis-induced inflammation: are complement C3 inhibitors a viable option? Clin. Immunol. 2019;198:102–105. doi: 10.1016/j.clim.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silasi-Mansat R., Zhu H., Georgescu C., Popescu N., Keshari R.S., Peer G., Lupu C., Taylor F.B., Pereira H.A., Kinasewitz G., Lambris J.D., Lupu F. Complement inhibition decreases early fibrogenic events in the lung of septic baboons. J. Cell. Mol. Med. 2015;19:2549–2563. doi: 10.1111/jcmm.12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Griensven M., Ricklin D., Denk S., Halbgebauer R., Braun C.K., Schultze A., Hönes F., Koutsogiannaki S., Primikyri A., Reis E., Messerer D., Hafner S., Radermacher P., Biglarnia A.R., Resuello R.R.G., Tuplano J.V., Mayer B., Nilsson K., Nilsson B., Lambris J.D., Huber-Lang M. Protective effects of the complement inhibitor compstatin CP40 in hemorrhagic shock. Shock. 2019;51:78–87. doi: 10.1097/SHK.0000000000001127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zimmerman J.L., Dellinger R.P., Straube R.C., Levin J.L. Phase I trial of the recombinant soluble complement receptor 1 in acute lung injury and acute respiratory distress syndrome. Crit. Care Med. 2000;28:3149–3154. doi: 10.1097/00003246-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Reis E.S., Berger N., Wang X., Koutsogiannaki S., Doot R.K., Gumas J.T., Foukas P.G., Resuello R.R.G., Tuplano J.V., Kukis D., Tarantal A.F., Young A.J., Kajikawa T., Soulika A.M., Mastellos D.C., Yancopoulou D., Biglarnia A.-R., Huber-Lang M., Hajishengallis G., Nilsson B., Lambris J.D. Safety profile after prolonged C3 inhibition. Clin. Immunol. 2018;197:96–106. doi: 10.1016/j.clim.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hajishengallis G., Kajikawa T., Hajishengallis E., Maekawa T., Reis E.S., Mastellos D.C., Yancopoulou D., Hasturk H., Lambris J.D. Complement-dependent mechanisms and interventions in periodontal disease. Front. Immunol. 2019;10:406. doi: 10.3389/fimmu.2019.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Magro C., Mulvey J.J., Berlin D., Nuovo G., Salvatore S., Harp J., Baxter-Stoltzfus A., Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl. Res. 2020 doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao T., Hu M., Zhang X., Li H., Zhu L., Liu H., Dong Q., Zhang Z., Wang Z., Hu Y., Fu Y., Jin Y., Li K., Zhao S., Xiao Y., Luo S., Li L., Zhao L., Liu J., Zhao H., Liu Y., Yang W., Peng J., Chen X., Li P., Liu Y., Xie Y., Song J., Zhang L., Ma Q., Bian X., Chen W., Liu X., Mao Q., Cao C. Highly pathogenic coronavirus N protein aggravates lung injury by MASP-2-mediated complement over-activation. MedRxiv. 2020 doi: 10.1101/2020.03.29.20041962. [DOI] [Google Scholar]