This systematic review and meta-analysis investigates whether internet-based self-help interventions directly targeting suicidal ideation or behavior are associated with reductions in suicidal ideation among patients in randomized clinical trials.
Key Points
Question
Is internet-based cognitive behavioral therapy directly targeting suicidal ideation or behaviors associated with reduced suicidal ideation?
Findings
In this meta-analysis including 6 unique randomized clinical trials and 1567 unique participants, internet-based cognitive behavioral therapy interventions for suicide prevention were associated with significantly reduced suicidal ideation after intervention compared with controls. First indications suggest that the treatment effect might be maintained at follow-up.
Meaning
Internet-based self-help interventions for suicide prevention based on cognitive behavioral therapy may be effective in reducing suicidal ideation and may be considered as a low-threshold treatment option, complementing current services.
Abstract
Importance
Suicidal ideation is a widespread phenomenon. However, many individuals at risk for suicide do not seek treatment, which might be addressed by providing low-threshold, internet-based self-help interventions.
Objective
To investigate whether internet-based self-help interventions directly targeting suicidal ideation or behavior are associated with reductions in suicidal ideation.
Data Sources
A systematic search of PsycINFO, MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), and the Centre for Research Excellence of Suicide Prevention (CRESP) databases for trials from inception to April 6, 2019, was performed, supplemented by reference searches. Search strings consisted of various search terms related to the concepts of internet, suicide, and randomized clinical trials.
Study Selection
Two independent researchers reviewed titles, abstracts, and full texts. Randomized clinical trials evaluating the effectiveness of internet-based self-help interventions to reduce suicidal ideation were included. Interventions were eligible if they were based on psychotherapeutic elements. Trials had to report a quantitative measure of a suicide-specific outcome. Mobile-based and gatekeeper interventions were excluded; no further restrictions were placed on participant characteristics or date of publication.
Data Extraction and Synthesis
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines. Risk of bias was evaluated using the Cochrane Risk of Bias Tool. Standardized mean differences were calculated using a random-effects model.
Main Outcomes and Measures
Suicidal ideation was the a priori primary outcome.
Results
Six unique eligible trials (1567 unique participants; 1046 [66.8%] female; pooled mean [SD] age, 36.2 [12.5] years) were included in the systematic review and meta-analysis. All identified interventions were internet-based cognitive behavioral therapy (iCBT). Participants assigned to the iCBT condition experienced a significantly reduced suicidal ideation compared with controls following intervention in all 6 trials (standardized mean difference, −0.29; 95% CI, −0.40 to −0.19; P < .001). Heterogeneity was low (I2 = 0%). The effect appeared to be maintained at follow-up in 4 trials (standardized mean difference, −0.18; 95% CI, −0.34 to −0.02; P = .03; I2 = 36%). Studies did not report sufficient data on completed suicides and suicide attempts to assess potential associations.
Conclusions and Relevance
These results show that iCBT interventions are associated with significant reductions in suicidal ideation compared with control conditions. Considering their high scalability, iCBT interventions have the potential to reduce suicide mortality. Future research should assess the effect of these digital health interventions on suicidal behavior and identify moderators and mediators to advance understanding of the mechanisms of effectiveness of these interventions.
Introduction
Suicidal ideation is a common phenomenon1,2,3,4,5 that often precedes suicide attempts and suicide deaths.1 Accordingly, suicidal ideation may be an important target for suicide prevention efforts, particularly as an indicator for early detection and intervention to avoid or reduce nonfatal and fatal outcomes.6,7 Cognitive behavioral therapy (CBT), including dialectical behavioral therapy, has been shown to be effective in the reduction of suicidal ideation and behaviors.8 Cognitive behavioral therapy is based on the assumption that cognitions play a central role in the development and maintenance of mental health issues and that emotional and behavioral problems can be resolved by modifying dysfunctional thoughts.9 Although effective treatments are available,8,10,11 many individuals at risk of suicide do not receive professional help.12 Barriers to treatment seeking in suicidal individuals include the wish to solve the problem by oneself, the belief that the problem is not that severe, stigma, limited access to treatment, and financial issues.12
There are high levels of technology use among suicidal persons.13 Moreover, suicidal persons are more likely to seek help online than in face-to-face settings,14 which might be due to the anonymity provided by digital resources.15 Thus, internet-based interventions might be an appropriate and low-threshold approach to address the barriers to treatment seeking.15,16
Growing interest in the applicability of digital technologies as scalable health solutions has seen stand-alone, internet-based self-help interventions (ISIs) become an emerging focus of health research in recent years.15 To date, most ISIs are based on CBT (internet-based CBT [iCBT]) because the highly structured and often manualized therapy elements can be transferred well into a digital format.15 The effectiveness of ISIs is well established for various mental disorders,17,18,19,20 and they have been integrated in clinical practice in several countries.15,21 However, ISIs for suicide prevention have not received the same attention. New studies using robust randomized trial designs have been published in recent years, warranting an update of the evidence.
Previous reviews in the field of digital interventions for suicide prevention have several limitations.22,23,24,25,26 First, most reviews have included a wide range of heterogeneous digital approaches for suicide prevention, such as websites, email support, online message boards, online support groups, and mobile interventions.23,25,26 The resulting statistical and clinical heterogeneity makes it difficult to draw valid conclusions on their effectiveness.27,28 Second, reviews often did not differentiate interventions directly addressing suicidality from those that focused on other conditions, such as depression.23,24,26 Third, study inclusion was often not restricted to randomized clinical trials (RCTs),22,23,25,26 which is methodologically inadequate because suicidal ideation seems to decrease even in control conditions.22 Fourth, risk of bias was not assessed in some cases.22,25 Fifth, previous reviews have typically not evaluated publication bias.22,23,24,25
The aim of this systematic review and meta-analysis is to examine whether ISIs that have been specifically designed to target suicidal ideation or behavior are associated with reductions in these outcomes. By addressing major methodological limitations of prior reviews, accurate evidence of the effects of ISIs is established in this review.
Methods
Search Strategy and Selection Criteria
This systematic review and meta-analysis was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.29 We searched the following databases from inception to April 6, 2019: PsycINFO, MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), and the Centre for Research Excellence of Suicide Prevention (CRESP). Search strings combined a variety of search terms related to the concepts of internet, suicide, and RCT and can be viewed in the study protocol.30 We conducted a pilot testing of the search strategy using a validation set of 5 eligible RCTs. All of these trials were identified using the search strategy. In addition, we screened the reference lists of all included studies and relevant review articles for additional studies (backward search), and we screened studies that cited the included studies and relevant reviews (forward search).28 Following this, we conducted a search on ClinicalTrials.gov on June 19, 2019, to examine publication bias and identify ongoing trials that are presented to give an overview of current developments in the field, but these results were not included in the meta-analysis. We did not search for gray literature.
Studies were eligible, first, if they used ISIs that directly targeted suicidal ideation or behaviors, were delivered predominantly in an online setting, and were based on psychological elements. Second, control groups could receive treatment as usual, another active or passive treatment, placebo, or no intervention or consist of a wait-list group. Third, studies had to report a quantitative measure of a suicide-specific outcome (ie, suicidal ideation, completed suicide, or suicide attempt). Fourth, eligible RCTs were provided in English or German and available in full text. Studies were excluded if they used mobile-based interventions or interventions that targeted gatekeepers (eg, teachers). We did not place any restrictions on sociodemographic characteristics of participants or date of publication.
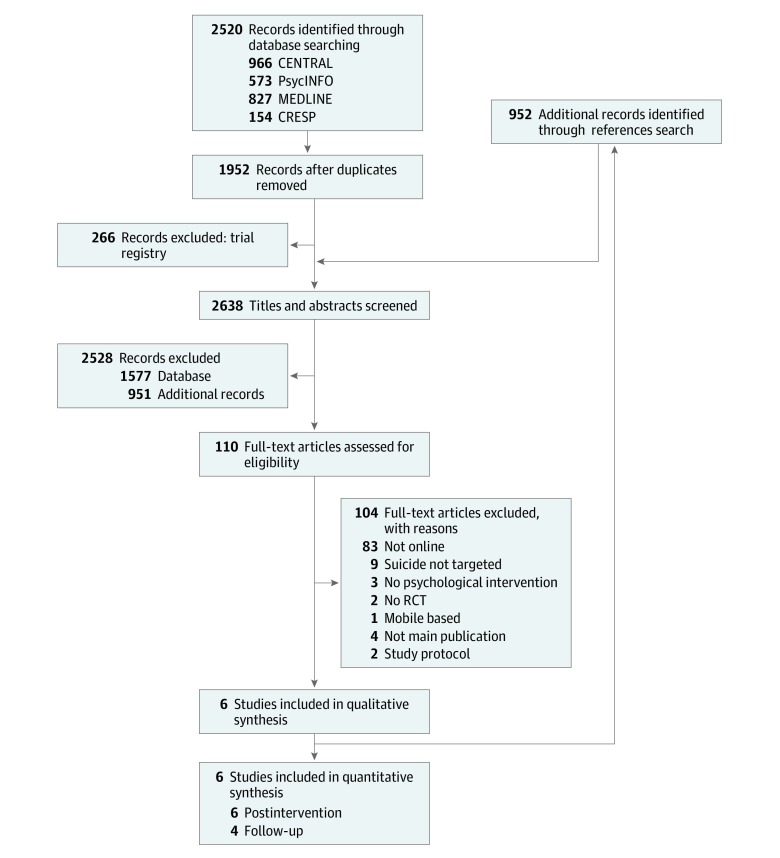
We analyzed summary data that were reported in the study or provided by authors. Two reviewers (R.B. and M.T.) independently screened the studies for eligibility in a hierarchical approach: in a first step, they screened titles and abstracts identified in the databases. In a second step, they screened full-text articles. Discrepancies were resolved in discussion with a third researcher (L.S.). The selection process is displayed in the PRISMA flowchart (Figure 1).
Figure 1. PRISMA Flowchart of Included Studies.
CENTRAL indicates Cochrane Central Register of Controlled Trials; CRESP, Centre for Research Excellence of Suicide Prevention; and RCTs, randomized clinical trials.
The procedure was predefined and described in detail in a study protocol.30 We registered the study with the International Prospective Register of Systematic Reviews (CRD42019130253). Amendments to the protocol are displayed in the eMethods in the Supplement.
Data Extraction
We used an investigator-developed data extraction form. Data were extracted by 1 researcher (R.B.) and double-checked by a second researcher (M.T. or Y.T.). The following data were extracted from the included studies: study identification items, study design, description of the intervention and control conditions, technical characteristics, population, setting, treatment adherence, study dropout, outcome variables, and results. If relevant data were not reported, we contacted corresponding authors via email to provide them. Authors of 2 eligible studies were asked to provide data that we received for 1 study. Where available, we used intent-to-treat data, including data from all randomized participants. To avoid bias through missing data, we extracted data from imputation models or estimated in robust multilevel analyses. The effect measures included in the meta-analysis were unadjusted. Suicidal ideation was the primary outcome. The following variables were included as secondary outcomes: suicide and suicide attempt, depressiveness, anxiety, and hopelessness. If multiple measures were used, we prioritized data extraction as follows: (1) validated questionnaires, (2) clinician ratings, and (3) single-item analysis of other rating scales.
Risk of Bias and Quality of Evidence
The risk of bias was evaluated with the Cochrane Risk of Bias tool that assesses risk of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias.31 The quality of evidence for the primary outcome was evaluated according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE).32 The GRADE assessments include the domains risk of bias, inconsistency, indirectness of evidence, imprecision of the estimate, and publication bias on outcome level. Both risk of bias and the quality of evidence were assessed by 2 independent researchers (R.B. and M.T.). Potential discrepancies were resolved in discussion with a third researcher (L.S.).
To determine whether publication bias was likely, we inspected an international trial registry (ClinicalTrials.gov) and used the systematic database searches to identify relevant trial protocols. Afterwards, we checked for subsequent publications.
Statistical Analysis
We conducted a random-effects meta-analysis for the primary outcome post intervention and at medium-term follow-up. We estimated standardized mean differences (SMDs) using Hedges g28 and respective 95% CIs; it was a between-group effect of mean changes from baseline, standardized by the pooled SD at baseline. Statistical heterogeneity was analyzed using I2 statistics. According to the GRADE handbook, an I2 statistic of less than 40% indicates low heterogeneity; 30% to 60%, moderate; 50% to 90%, substantial; and 75% to 100%, considerable.32 We conducted a preplanned subgroup analysis for different types of control groups (active vs wait-list controls). We conducted predefined sensitivity analyses by only including interventions for adults and by only including unguided interventions. Unguided ISIs were defined as interventions that do not involve any human support, whereas in guided ISI, a therapist provides feedback and guidance in addition to the self-help material that can be used independently.15 Another predefined sensitivity analysis was conducted by excluding trials at high risk of bias (ie, >2 items of the Cochrane Risk of Bias Tool31 rated at high risk). We performed a post hoc sensitivity analysis by excluding a trial that had a high weight (43.3%) on the pooled effect size. All subgroup and sensitivity analyses were only performed for the effects post intervention.
Effects on secondary outcomes were reported narratively. The Cochrane Collaboration’s Review Manager (RevMan, version 5.3) was used for calculation. We used R, version 3.6.1 (R Project for Statistical Computing), for preparatory analyses. Two-sided P < .05 indicated statistical significance.
Results
Selection, Inclusion, and Study Characteristics
We identified 2638 records for screening. A total of 6 unique studies33,34,35,36,37,38 (1567 unique baseline participants; 1046 [66.8%] female; pooled mean [SD] age, 36.2 [12.5] years) were included in the systematic review and meta-analysis. The study selection process is displayed along with reasons for exclusion in Figure 1.
A summary of included studies is provided in the Table. All studies were published from 2014 to 2019. Two interventions34,35 were designed for youth (mean [SD] age, 16.9 [1.7] and 14.7 [1.4] years), whereas 4 interventions33,36,37,38 were designed for adults (mean [SD] age range, 14.7 [1.4] to 40.9 [13.7] years). The proportion of female participants ranged from 59.4% to 82.0%. All interventions were developed for the reduction of preexisting suicidal ideation or behaviors and were based on iCBT, including third-wave therapies such as dialectical behavioral therapy. Five studies33,34,36,37,38 reported using homework or exercises in their programs; only 2 interventions were guided.35,37 Exposure time ranged from 2 weeks34 to 10 weeks.35 Most of the trials33,35,36,37,38 reported safety procedures for enrolled participants. This involved contacting participants who reported suicidal ideation above a predefined threshold, and in 2 trials,33,38 the participant’s psychiatrist or general clinician was called when the risk threshold defined in the duty of care protocol was reached.
Table. Study Characteristics.
| Source | Country | Population | Age at baseline, mean (SD), y | Total No. at baseline (female, %) | Intervention type (No. of modules) [duration] | Control condition | Measure of suicidal ideation | Dropout rate, %a | |
|---|---|---|---|---|---|---|---|---|---|
| Intervention group | Control group | ||||||||
| van Spijker et at,33 2014 | The Netherlands | Adults with suicidal thoughts | 40.9 (13.7) | 236 (66.1) | CBT, DBT problem-solving therapy, mindfulness-based therapy; unguided (6) [6 wk] | Wait-list | Beck Scale for Suicidal Ideation | 9.5 | 8.3 |
| Hill and Pettit,34 2016 | United States | School students with perceived burdensomeness | 16.9 (1.7) | 80 (68.8) | CBT; unguided (2) [2 wk] plus psychoeducational emails | Attention-control (emails with psychoeducational information) | Beck Scale for Suicidal Ideation | 12.2 | 10.03 |
| Hetrick et at,35 2017 | Australia | School students with suicidal ideation | 14.7 (1.4) | 50 (82.0) | CBT; guided (8) [10 wk] plus TAU | TAU (contact with the school well-being staff) | Suicidal Ideation Questionnaire | 30.8 | 12.5 |
| van Spijker et al,36 2018 | Australia | Adults with suicidal thoughts | 40.6 (11.9) | 418 (77.3) | CBT, DBT, problem-solving therapy, mindfulness-based therapy; unguided (6) [6 wk] | Attention-control (6-wk online modular lifestyle information program) | Intensity of Suicidal Ideation subscale of the Columbia Suicide Severity Rating Scale | 43.5 | 48.3 |
| Wilks et al,37 2018 | United States | Suicidal individuals with heavy episodic drinking and emotion dysregulation | 38.0 (10.4) | 59 (69.5) | DBT; guided (8) [8 wk] | Wait-list | Beck Scale for Suicidal Ideation | 26.7 | 3.4 |
| de Jaegere et al,38 2019 | Belgium | Adults with suicidal thoughts | 35.7 (13.6) | 724 (59.4) | CBT, DBT, problem-solving therapy, mindfulness-based therapy; unguided (6) [6 wk] | Wait-list | Beck Scale for Suicidal Ideation | 74.0 | 52.1 |
Abbreviations: CBT, cognitive behavioral therapy; DBT, dialectical behavioral therapy; TAU, treatment as usual.
Rates shown are for participants who dropped out after the intervention was completed.
Three studies33,36,38 used the same intervention (“Living with deadly thoughts”) developed by van Spijker et al39 or an adapted version of it. This unguided intervention consisted of 6 modules, and participants were instructed to work for 30 minutes a day on each module during a 6-week period. The intervention had a strong focus on worry scheduling, aiming to help suicidal individuals to gain more control over their suicidal ideation. In addition, the intervention consisted of learning exercises and psychoeducation on emotion regulation, the identification and modification of automatic thoughts, and relapse prevention.39 Two interventions34,35 were designed for secondary school students. The 8 modules in the intervention by Hetrick et al35 included CBT elements such as behavioral activation, identification of automatic thoughts, problem solving, and cognitive restructuring. The intervention by Hill and Pettit34 consisted of 2 modules and included psychoeducation, exploration of situations in which adolescents perceive themselves as a burden, reality checking, and activity scheduling. One intervention37 was a dialectical behavioral therapy skills training consisting of 8 modules designed for heavy episodic drinkers experiencing suicidal ideation. The intervention focused especially on emotion dysregulation, which is associated with both suicide risk and binge drinking.40
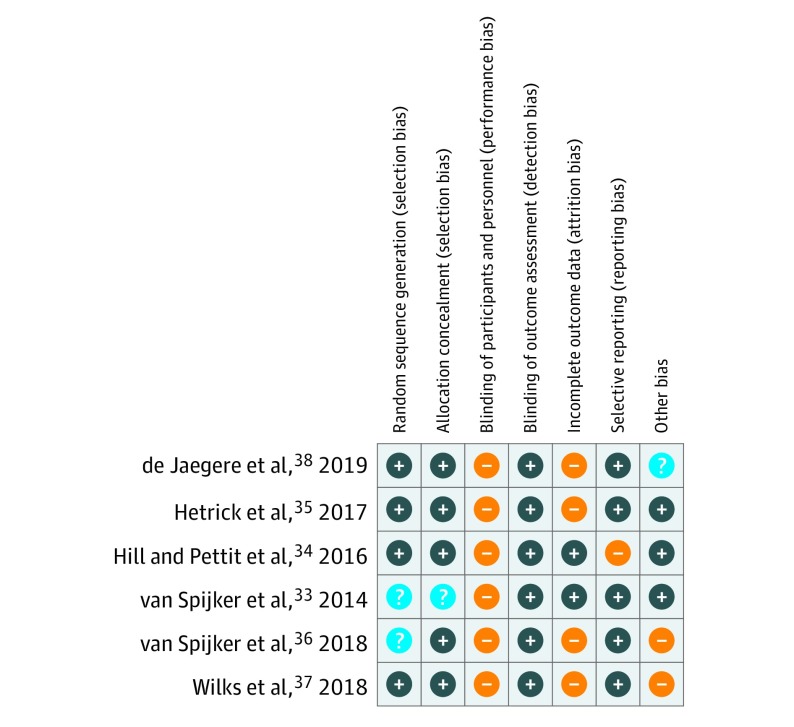
Risk of Bias
An overview of the risk of bias assessment is presented in Figure 2. The largest source of potential bias resulted from the failure to blind participants. As is the case for most psychological intervention trials, blinding of participants was not possible. This is a potential risk of bias, in particular because all outcomes were self-reported. Substantial risk of bias was introduced by incomplete outcome data. Risk of attrition bias was high in 4 studies.35,36,37,38 One study did not provide robust estimates based on an imputation model or multilevel analysis for the meta-analysis37; 3 studies35,36,38 reported more than 20% dropout (up to 63.1%38) following the intervention, and in 2 of these,35,38 dropout was higher in the intervention group than in the control condition. Risk of bias was mostly low in the other evaluated categories.
Figure 2. Risk of Bias Summary.
Ratings were performed using the Cochrane Risk of Bias Tool. Plus sign indicates low risk of bias; minus sign, high risk; and question mark, unclear.
Meta-analysis
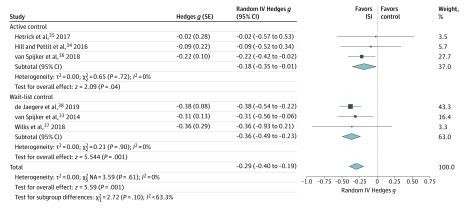
All 6 studies reported effects on suicidal ideation and were included in the meta-analysis. The meta-analysis revealed a statistically significant effect following the intervention favoring ISI over controls (SMD, −0.29; 95% CI, −0.40 to −0.19; P < .001). Postintervention times ranged from 2 to 10 weeks after baseline. The forest plot is displayed in Figure 3. The overall level of heterogeneity was low (I2 = 0%).32
Figure 3. Between-Group Effects of Internet-Based Self-help Interventions (ISIs) on Suicidal Ideation Post Intervention.
Negative values indicate lower suicidal ideation in the intervention group compared with controls. Size of markers indicates weight. IV indicates inverse variance; and NA, not applicable.
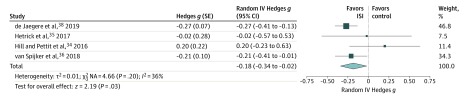
A follow-up comparison of suicidal ideation to 6 months post intervention was available from 4 studies,33,34,35,36,38 with assessment times ranging from 6 to 26 weeks after the postintervention period. At follow-up, the reduction of suicidal ideation was significant (SMD, −0.18; 95% CI, −0.34 to −0.02; P = .03) (Figure 4), and statistical heterogeneity was moderate (I2 = 36%).32
Figure 4. Between-Group Effects of Internet-Based Self-help Interventions (ISIs) on Suicidal Ideation at Follow-up.
Follow-up occurred 6 to 26 weeks after the postintervention period. Negative values indicate lower suicidal ideation in the intervention group compared with controls. Size of markers indicates weight. IV indicates inverse variance; NA, not applicable; and SE, standard error.
Subgroup and Sensitivity Analyses
Subgroup and sensitivity analyses were performed for the effects post intervention. The subgroup analysis (Figure 3) for different types of control groups revealed an SMD of ISI compared with active controls of −0.18 (95% CI, −0.35 to −0.01; P = .04), whereas the SMD of ISI compared with wait-list controls was −0.36 (95% CI, −0.49 to −0.23; P < .001). Active controls received emails with psychoeducational content, were in contact with the school well-being staff, or received a modular lifestyle program that was matched to the ISI for suicide prevention. The variability between subgroups was I2 = 63.3. Sensitivity analyses showed a significant effect for ISI for adults in 4 studies33,36,37,38 (SMD, −0.32; 95% CI, −0.43 to −0.21; P < .001) and a significant effect for unguided ISI in 4 studies33,34,36,38 (SMD, −0.30; 95% CI, −0.41 to −0.20; P < .001).
An additional sensitivity analysis revealed that when the study by de Jaegere et al38 that had a weight of 43.3% in the meta-analysis post intervention was excluded, there was still a significant effect on suicidal ideation33,34,35,36,37 (SMD, −0.23; 95% CI, −0.37 to −0.09; P = .001). Furthermore, when trials at high risk of bias (ie, >2 items of the Cochrane Risk of Bias Tool rated at high risk of bias) were excluded,36,37 a comparable effect size to the overall effect post intervention was found33,34,35,38 (SMD, −0.32; 95% CI, −0.45 to −0.20; P < .001).
Secondary Outcomes
Regarding completed suicides, 2 studies33,38 included anecdotal reports that no suicide death occurred during the study. However, both studies did not include assessment of suicide deaths in the methods section and did not specifically declared it as an outcome, so how they ensured that suicide deaths could be detected remains unclear. Two studies35,36 reported on suicide attempts, and both trials did not find an effect. A total of 5 studies33,34,35,36,38 reported data on depressive symptoms, whereas 4 studies33,35,36,38 reported data on anxiety and hopelessness symptoms. Effect sizes and 95% CIs for depressiveness, anxiety, and hopelessness are displayed in eTable 1 in the Supplement. Most of the trials found almost no significant effects, with the exception of 1 study38 that found significant reductions of depressive symptoms, anxiety, and hopelessness across all time points with small to medium effect sizes.
Adherence to the intervention was reported in 5 studies,33,34,35,36,37 using a variety of definitions, so that we could only summarize data from 3 trials.33,34,37 A total of 45.2% to 92.7% of participants completed at least half of the modules, with a mean of 64.6%. The percentage of participants completing no modules ranged from 6.5% to 22.4%, with a mean of 12.1%.
Unpublished Studies
We searched for registered trials and study protocols to check for potential publication bias, because unpublished trials might be different from published trials, and to give an overview of ongoing trials. The search of ongoing trials in ClinicalTrials.gov yielded 313 records. No completed but unpublished trials were identified. In addition, we identified 9 relevant study protocols in the database searches. For 4 protocols, subsequent publications were identified and included in this review.33,35,36,37 For 5 protocols, we could not identify any publication of results; however, it could be presumed that trials or publication processes were still ongoing, because the identified protocols were published from 2016 to 2018.41,42,43,44,45 Thus, we did not find any evidence of publication bias. The database and clinical trial register searches revealed a total of 7 potentially relevant ongoing trials that are reviewed in eResults in the Supplement.
Quality of Evidence
The quality of evidence was rated for the effect on suicidal ideation post intervention and at follow-up by using the GRADE procedure32 (eTable 2 in the Supplement). Ratings indicated a moderate quality of evidence for the reduction in suicidal ideation scores post intervention. The main reason for downgrading was risk of bias resulting from high attrition rates, the failure to blind participants, and the use of wait-list controls. Quality of evidence was rated very low at follow-up because only 4 trials34,35,36,38 provided follow-up data. The confidence in the effect estimate was additionally limited by exceedingly high dropout rates (>50% overall), by 1 trial finding an effect in favor of the control condition,34 because of variance in assessment timing, and because of wide 95% CIs (−0.34 to −0.02) indicating a high degree of uncertainty.
Discussion
This report is, to our knowledge, the first systematic review and meta-analysis to evaluate whether iCBT interventions that directly target suicidality are associated with reductions in suicidal ideation. Six RCTs were identified and included in this meta-analysis, of which 1 was a pilot trial.34 Available data suggest that ISIs significantly reduced suicidal ideation post intervention and provide preliminary evidence that this effect can be maintained at follow-up. Statistical and clinical heterogeneity was low. The identified effect size post intervention is similar to those found in meta-analyses for face-to-face CBT for suicidal ideation24 and for interventions for youth that directly target suicidality,46 suggesting that iCBT may be a useful alternative to traditional therapies.
The GRADE rating indicated a moderate quality of evidence for the effect post intervention. Subgroup analysis revealed higher effect sizes in wait-list–controlled compared with actively controlled study designs, which is a common finding in meta-analyses.47,48 Wait-list controls might introduce a nocebo effect, leading to a possible overestimation of effects due to a worsening of symptoms in the control condition.49
Taking into account that ISIs are highly scalable15,50 and that suicidal ideation is a major risk factor for suicide,1 even small effects on suicidal ideation might have substantial effects when implemented at scale. Ideally, in addition to ISIs being made available online, they could be integrated into health services, such as through prescription by clinicians as standalone or adjunctive therapies.51 Moreover, crisis services, such as the National Suicide Prevention Lifeline, could be complemented by iCBT. Above that, multiple implementation pathways, such as search engine–based approaches, should be explored to identify optimal distribution channels to reach individuals at risk of suicide.52
The participants of the studies in this meta-analysis were predominantly female, which is in line with the higher prevalence of suicidal ideation1,4 and help-seeking behavior in women.53 Rates of suicide have been higher in men than in women; however, this gender gap is narrowing.54 The field should move forward by developing tailored interventions to address the specific needs of individual users, instead of distributing one-size-fits-all interventions. Using machine-learning algorithms might be a viable way to reach this goal.55 New technological opportunities, such as digital phenotyping, could be used to perform risk assessments and to personalize interventions to the current needs of individuals at risk of suicide.55,56,57,58
Furthermore, future research could strengthen the evidence base of ISIs for suicide prevention by conducting larger-scale effectiveness trials with active controls or noninferiority trials and by including longer follow-up measurement occasions. These approaches are not only needed to increase confidence in the effectiveness of ISIs but also to examine the potential effect of these interventions on suicide behavioral outcomes.59,60 Fortunately, the field appears to be moving in this direction, with 2 large-scale, ongoing trials planned to evaluate the effectiveness of internet-based interventions on suicidal behavior.41,45 A possible way to strengthen the effects of ISI could be to undertake implementation trials of strategies to improve uptake and adherence, which has been suboptimal in previous studies.38 Adding human support could contribute to achieve this goal, because guided interventions typically demonstrate larger effects than unguided interventions and might increase adherence.61,62 However, adding guidance limits the scalability and anonymity to some extent. To make full use of the existing date and to identify moderators and mediators of effects, an individual patient data meta-analysis could also be a fruitful next step.
Limitations
This systematic review and meta-analysis has some limitations. First, subgroup and sensitivity analyses need to be interpreted with caution, because they rely on observational data. Owing to the low number of included studies (n = 6), results of subgroup and sensitivity analyses are likely to be confounded with other variables.28 Second, although statistical heterogeneity was low (I2 = 0%), there are most likely differential effects for different interventions, populations, or designs that could not be detected owing to the imprecision of effect estimates. Third, it remains largely unclear whether reductions in suicidal ideation can be maintained. The GRADE rating indicated a very low quality of evidence at follow-up, because the estimate is based on data from only 4 studies with high dropout rates, and follow-up assessment times ranged from 6 to 26 weeks. Finally, publication bias could not be ruled out.28 However, we did not find any evidence for the presence of publication bias by screening the trial register and study protocols. Furthermore, included studies consist not only of studies with significant effects but also small trials with nonsignificant results, which might be less likely to be published.63
Conclusions
The current body of research suggests that iCBT may be an important part of future suicide prevention efforts. Owing to their high scalability, the implementation of iCBT interventions into health systems and communities might translate to a substantial effect on reducing the disease burden of suicidal ideation. However, the field is still in its infancy, and continued robust research efforts are needed to confidently establish the effectiveness of interventions, identify moderators and mediators, and explore pathways to deliver tailored interventions for individuals at risk of suicide.
eMethods. Amendments to the Study Protocol
eTable 1. Between-Groups Effect Sizes of Secondary Outcomes
eTable 2. GRADE Ratings for Suicidal Ideation
eResults. Results of Ongoing Trials
eReferences.
References
- 1.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):-. doi: 10.1192/bjp.bp.107.040113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uddin R, Burton NW, Maple M, Khan SR, Khan A. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. Lancet Child Adolesc Health. 2019;3(4):223-233. doi: 10.1016/S2352-4642(18)30403-6 [DOI] [PubMed] [Google Scholar]
- 3.Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214-2236. doi: 10.1001/jama.2016.17324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300-310. doi: 10.1001/2013.jamapsychiatry.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Voss C, Ollmann TM, Miché M, et al. Prevalence, onset, and course of suicidal behavior among adolescents and young adults in Germany. JAMA Netw Open. 2019;2(10):e1914386. doi: 10.1001/jamanetworkopen.2019.14386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73-85. doi: 10.1016/S2215-0366(14)70222-6 [DOI] [PubMed] [Google Scholar]
- 7.Hawton K. Suicide prevention: a complex global challenge. Lancet Psychiatry. 2014;1(1):2-3. doi: 10.1016/S2215-0366(14)70240-8 [DOI] [PubMed] [Google Scholar]
- 8.Zalsman G, Hawton K, Wasserman D, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. 2016;3(7):646-659. doi: 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- 9.Kazantzis N, Luong HK, Usatoff AS, Impala T, Yew RY, Hofmann SG. The processes of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2018;42(4):349-357. doi: 10.1007/s10608-018-9920-y [DOI] [Google Scholar]
- 10.Calati R, Courtet P. Is psychotherapy effective for reducing suicide attempt and non-suicidal self-injury rates? Meta-analysis and meta-regression of literature data. J Psychiatr Res. 2016;79:8-20. doi: 10.1016/j.jpsychires.2016.04.003 [DOI] [PubMed] [Google Scholar]
- 11.Hogan MF. Better suicide screening and prevention are possible. JAMA Psychiatry. 2016;73(11):1111-1112. doi: 10.1001/jamapsychiatry.2016.2411 [DOI] [PubMed] [Google Scholar]
- 12.Bruffaerts R, Demyttenaere K, Hwang I, et al. Treatment of suicidal people around the world. Br J Psychiatry. 2011;199(1):64-70. doi: 10.1192/bjp.bp.110.084129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris KM, McLean JP, Sheffield J. Suicidal and online: how do online behaviors inform us of this high-risk population? Death Stud. 2014;38(6-10):387-394. doi: 10.1080/07481187.2013.768313 [DOI] [PubMed] [Google Scholar]
- 14.Wilks CR, Coyle TN, Krek M, Lungu A, Andriani K. Suicide ideation and acceptability toward online help-seeking. Suicide Life Threat Behav. 2018;48(4):379-385. doi: 10.1111/sltb.12356 [DOI] [PubMed] [Google Scholar]
- 15.Ebert DD, van Daele T, Nordgreen T, et al. Internet- and mobile-based psychological interventions: applications, efficacy, and potential for improving mental health. Eur Psychol. 2018;23(2):167-187. doi: 10.1027/1016-9040/a000318 [DOI] [Google Scholar]
- 16.Andersson G, Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4-11. doi: 10.1002/wps.20083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andrews G, Basu A, Cuijpers P, et al. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. J Anxiety Disord. 2018;55:70-78. doi: 10.1016/j.janxdis.2018.01.001 [DOI] [PubMed] [Google Scholar]
- 18.Sijbrandij M, Kunovski I, Cuijpers P. Effectiveness of internet-delivered cognitive behavioral therapy for posttraumatic stress disorder: a systematic review and meta-analysis. Depress Anxiety. 2016;33(9):783-791. doi: 10.1002/da.22533 [DOI] [PubMed] [Google Scholar]
- 19.Karyotaki E, Riper H, Twisk J, et al. Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms: a meta-analysis of individual participant data. JAMA Psychiatry. 2017;74(4):351-359. doi: 10.1001/jamapsychiatry.2017.0044 [DOI] [PubMed] [Google Scholar]
- 20.Josephine K, Josefine L, Philipp D, David E, Harald B. Internet- and mobile-based depression interventions for people with diagnosed depression: a systematic review and meta-analysis. J Affect Disord. 2017;223:28-40. doi: 10.1016/j.jad.2017.07.021 [DOI] [PubMed] [Google Scholar]
- 21.Titov N, Hadjistavropoulos HD, Nielssen O, Mohr DC, Andersson G, Dear BF. From research to practice: ten lessons in delivering digital mental health services. J Clin Med. 2019;8(8):E1239. doi: 10.3390/jcm8081239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christensen H, Batterham PJ, O’Dea B. E-health interventions for suicide prevention. Int J Environ Res Public Health. 2014;11(8):8193-8212. doi: 10.3390/ijerph110808193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lai MH, Maniam T, Chan LF, Ravindran AV. Caught in the web: a review of web-based suicide prevention. J Med internet Res. 2014;16(1):e30. doi: 10.2196/jmir.2973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leavey K, Hawkins R. Is cognitive behavioural therapy effective in reducing suicidal ideation and behaviour when delivered face-to-face or via e-health? a systematic review and meta-analysis. Cogn Behav Ther. 2017;46(5):353-374. doi: 10.1080/16506073.2017.1332095 [DOI] [PubMed] [Google Scholar]
- 25.Perry Y, Werner-Seidler A, Calear AL, Christensen H. Web-based and mobile suicide prevention interventions for young people: a systematic review. J Can Acad Child Adolesc Psychiatry. 2016;25(2):73-79. [PMC free article] [PubMed] [Google Scholar]
- 26.Witt K, Spittal MJ, Carter G, et al. Effectiveness of online and mobile telephone applications (“apps”) for the self-management of suicidal ideation and self-harm: a systematic review and meta-analysis. BMC Psychiatry. 2017;17(1):297. doi: 10.1186/s12888-017-1458-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kriston L. Dealing with clinical heterogeneity in meta-analysis. Assumptions, methods, interpretation. Int J Methods Psychiatr Res. 2013;22(1):1-15. doi: 10.1002/mpr.1377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higgins JPT, Green S, e.s Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. Accessed October 30, 2019. https://training.cochrane.org/handbook/archive/v5.1/
- 29.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65-W94. doi: 10.7326/0003-4819-151-4-200908180-00136 [DOI] [PubMed] [Google Scholar]
- 30.Büscher R, Torok M, Sander L. The effectiveness of internet-based self-help interventions to reduce suicidal ideation: protocol for a systematic review and meta-analysis. JMIR Res Protoc. 2019;8(7):e14174. doi: 10.2196/14174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JPT, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schünemann H, Brożek J, Guyatt G, Oxman A Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach GRADE Working Group. Updated October 2013. Accessed October 30, 2019. https://gdt.gradepro.org/app/handbook/handbook.html#h.svwngs6pm0f2
- 33.van Spijker BA, van Straten A, Kerkhof AJFM. Effectiveness of online self-help for suicidal thoughts: results of a randomised controlled trial. PLoS One. 2014;9(2):e90118. doi: 10.1371/journal.pone.0090118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hill RM, Pettit JW. Pilot randomized controlled trial of LEAP: a selective preventive intervention to reduce adolescents’ perceived burdensomeness. J Clin Child Adolesc Psychol. 2016;00(00):1-12. doi: 10.1080/15374416.2016.1188705 [DOI] [PubMed] [Google Scholar]
- 35.Hetrick SE, Yuen HP, Bailey E, et al. Internet-based cognitive behavioural therapy for young people with suicide-related behaviour (Reframe-IT): a randomised controlled trial. Evid Based Ment Health. 2017;20(3):76-82. doi: 10.1136/eb-2017-102719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Spijker BA, Werner-Seidler A, Batterham PJ, et al. Effectiveness of a web-based self-help program for suicidal thinking in an Australian community sample: randomized controlled trial. J Med internet Res. 2018;20(2):e15. doi: 10.2196/jmir.8595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilks CR, Lungu A, Ang SY, Matsumiya B, Yin Q, Linehan MM. A randomized controlled trial of an internet delivered dialectical behavior therapy skills training for suicidal and heavy episodic drinkers. J Affect Disord. 2018;232:219-228. doi: 10.1016/j.jad.2018.02.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Jaegere E, van Landschoot R, van Heeringen K, et al. The online treatment of suicidal ideation: a randomised controlled trial of an unguided web-based intervention. Behav Res Ther. 2019;119:103406. doi: 10.1016/j.brat.2019.05.003 [DOI] [PubMed] [Google Scholar]
- 39.van Spijker BAJ, van Straten A, Kerkhof AJFM. The effectiveness of a web-based self-help intervention to reduce suicidal thoughts: a randomized controlled trial. Trials. 2010;11:25. doi: 10.1186/1745-6215-11-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilks C, Yin Q, Ang SY, Matsumiya B, Lungu A, Linehan M. Internet-delivered dialectical behavioral therapy skills training for suicidal and heavy episodic drinkers: protocol and preliminary results of a randomized controlled trial. JMIR Res Protoc. 2017;6(10):e207. doi: 10.2196/resprot.7767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coralie G, Kathleen T, Marie-Amelie V, Anais LJ, Hazo JB, Karine C. Printemps project: e-health intervention for suicide prevention and mental health promotion in the French general population. Eur Psychiatry. 2018;48:S222-S223. doi: 10.1016/j.eurpsy.2017.12.016 [DOI] [Google Scholar]
- 42.Eylem O, van Straten A, Bhui K, Kerkhof AJFM. Protocol: reducing suicidal ideation among Turkish migrants in the Netherlands and in the UK: effectiveness of an online intervention. Int Rev Psychiatry. 2015;27(1):72-81. doi: 10.3109/09540261.2014.996121 [DOI] [PubMed] [Google Scholar]
- 43.Mascayano F, Schilling S, Tapia E, et al. Using information and communication technologies to prevent suicide among secondary school students in two regions of Chile: a randomized controlled trial. Front Psychiatry. 2018;9(236):236. doi: 10.3389/fpsyt.2018.00236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mühlmann C, Madsen T, Hjorthøj C, Kerkhof A, Nordentoft M, Erlangsen A. The Self-help Online Against Suicidal Thoughts (SOS) trial: study protocol for a randomized controlled trial. Trials. 2017;18(1):45. doi: 10.1186/s13063-017-1794-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simon GE, Beck A, Rossom R, et al. Population-based outreach versus care as usual to prevent suicide attempt: study protocol for a randomized controlled trial. Trials. 2016;17(1):452. doi: 10.1186/s13063-016-1566-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robinson J, Bailey E, Witt K, et al. What works in youth suicide prevention? a systematic review and meta-analysis. EClinicalMedicine. 2018;4-5:52-91. doi: 10.1016/j.eclinm.2018.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cuijpers P, van Straten A, Bohlmeijer E, Hollon SD, Andersson G. The effects of psychotherapy for adult depression are overestimated: a meta-analysis of study quality and effect size. Psychol Med. 2010;40(2):211-223. doi: 10.1017/S0033291709006114 [DOI] [PubMed] [Google Scholar]
- 48.Hempel S, Suttorp MJ, Miles JN, et al. Empirical Evidence of Associations Between Trial Quality and Effect Size. Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 49.Gold SM, Enck P, Hasselmann H, et al. Control conditions for randomised trials of behavioural interventions in psychiatry: a decision framework. Lancet Psychiatry. 2017;4(9):725-732. doi: 10.1016/S2215-0366(17)30153-0 [DOI] [PubMed] [Google Scholar]
- 50.Singla DR, Raviola G, Patel V. Scaling up psychological treatments for common mental disorders: a call to action. World Psychiatry. 2018;17(2):226-227. doi: 10.1002/wps.20532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Andrews G, Hobbs MJ. Pragmatic treatment options for depression and anxiety disorders are needed. World Psychiatry. 2016;15(3):241-242. doi: 10.1002/wps.20364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sueki H, Ito J. Appropriate targets for search advertising as part of online gatekeeping for suicide prevention. Crisis. 2018;39(3):197-204. doi: 10.1027/0227-5910/a000486 [DOI] [PubMed] [Google Scholar]
- 53.Oliver MI, Pearson N, Coe N, Gunnell D. Help-seeking behaviour in men and women with common mental health problems: cross-sectional study. Br J Psychiatry. 2005;186(4):297-301. doi: 10.1192/bjp.186.4.297 [DOI] [PubMed] [Google Scholar]
- 54.Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in suicide among youth aged 10 to 19 years in the United States, 1975 to 2016. JAMA Netw Open. 2019;2(5):e193886. doi: 10.1001/jamanetworkopen.2019.3886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stanley B, Mann JJ. The need for innovation in health care systems to improve suicide prevention. JAMA Psychiatry. 2019;1-3. doi: 10.1001/jamapsychiatry.2019.2769 [DOI] [PubMed] [Google Scholar]
- 56.Kleiman EM, Turner BJ, Fedor S, et al. Digital phenotyping of suicidal thoughts. Depress Anxiety. 2018;35(7):601-608. doi: 10.1002/da.22730 [DOI] [PubMed] [Google Scholar]
- 57.Torous J, Walker R. Leveraging digital health and machine learning toward reducing suicide—from panacea to practical tool. JAMA Psychiatry. 2019;76(10):999-1000. doi: 10.1001/jamapsychiatry.2019.1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Insel TR. Digital phenotyping: technology for a new science of behavior. JAMA. 2017;318(13):1215-1216. doi: 10.1001/jama.2017.11295 [DOI] [PubMed] [Google Scholar]
- 59.Holmes EA, Ghaderi A, Harmer CJ, et al. The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry. 2018;5(3):237-286. doi: 10.1016/S2215-0366(17)30513-8 [DOI] [PubMed] [Google Scholar]
- 60.Sisti DA, Joffe S. Implications of zero suicide for suicide prevention research. JAMA. 2018;320(16):1633-1634. doi: 10.1001/jama.2018.13083 [DOI] [PubMed] [Google Scholar]
- 61.Domhardt M, Geßlein H, von Rezori RE, Baumeister H. Internet- and mobile-based interventions for anxiety disorders: a meta-analytic review of intervention components. Depress Anxiety. 2019;36(3):213-224. doi: 10.1002/da.22860 [DOI] [PubMed] [Google Scholar]
- 62.Titov N. Internet-delivered psychotherapy for depression in adults. Curr Opin Psychiatry. 2011;24(1):18-23. doi: 10.1097/YCO.0b013e32833ed18f [DOI] [PubMed] [Google Scholar]
- 63.Sterne JAC, Sutton AJ, Ioannidis JPA, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Amendments to the Study Protocol
eTable 1. Between-Groups Effect Sizes of Secondary Outcomes
eTable 2. GRADE Ratings for Suicidal Ideation
eResults. Results of Ongoing Trials
eReferences.