The outbreak and spread of coronavirus disease 2019 (COVID-19) are not only a disaster of people's life and health over the world,[1]–[3] but also the challenge for medical practitioner in clinical management. Owing to many diagnostic instruments are not suitable or convenient to use any more in contagious ward considering the risk of cross infections, such as traditional stethoscope or electrocardiogram (ECG). In this scenarios, wireless and digital equipment are optimal choices for epidemic management in order to exert rapid diagnosis and disease evaluation. Herein, we reported a case of the patient suffering both COVID-19 and myocardial infarction, for which the tele-ECG and wireless stethoscope facilitated the accurate diagnosis and instant management.
The patient was a 60-year-old male with prior history of hypertension and recently elevated blood glucose. One month ago, he presented with dry cough and low-grade fever at 37.5 °C, so quarantined and rest at home considering the occupied hospitals in Wuhan in early February, as the timeline depicted in Figure 1. Then sudden onset of drastic vomiting and long duration of chest discomfort tortured him a whole night without obvious relief, then he was sent to the Wuhan Asia Heart Hospital by family in the next day. Markers of myocardial injury were significantly elevated, such as troponin T was 11,500 ng/L, natriuretic peptide was up to 4,121 ng/L, and nucleic acid test of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was positive. The ECG showed ST-segments were elevated significantly in inferior wall leads and mildly elevated in posterior wall leads, whereas depressed in anterior wall. Following chest computed tomography showed both signs of ground glass opacity (GGO) as viral pneumonia and pulmonary edema indicating heart failure (Figure 2). The diagnosis was ST-segment elevated acute myocardial infarction concomitant with COVID-19. Since the percutaneous coronary intervention was not available during the epidemic, while thrombolysis was not applicable due to the delay time more than 12 h, only intra-aortic balloon pump (IABP) and noninvasive ventilator were implemented for nearly three weeks. Meanwhile, the antiviral drugs and traditional Chinese medicine were prescribed considering the concomitant COVID-19. After the vital signs of the patient were prone to be stable, the instruments were weaning and then the patient was transferred to Infectious Diseases Department of Huoshenshan Hospital. However, the patient felt short of breath immediately after the admission and accompanied by drastic cough. Since either COVID-19 or angina post myocardial infarction was possible pathogenesis of these symptoms, how to evaluate and manage such tough scenario is critical. Considering the convenience and rapidness of wireless equipment, we performed auscultation with wireless stethoscope first and heard the gallop rhythm and reflex murmur in mitral valve zone. Then we performed ECG using waistband-shaped tele-ECG, which indicated severe ischemia in inferior wall as II, III, and aVF leads, and it also reflected by the mirror leads (Figure 3). We judged that the patient suffered angina post infarction and congestive heart failure during the long way transport, and then immediately prescribed nitroglycerine and furosemide for vasodilation as well as preload reduction. Thereafter, the symptoms of the patient relieved in ten minutes. Then second chest computed tomography proved aforementioned diagnosis and showed gradual absorption of GGO of the patient. Following echocardiography also showed decreased left ventricular ejection fraction as 43% and observed severe mitral regurgitation found by wireless stethoscope. The serum brain natriuretic peptide level was still elevated at 800 ng/L in supporting the diagnosis of heart failure. After that, dual anti-platelet drugs, anti-ischemia agents, and diuretics as optimal medication of acute myocardial infarction were given, as well as the COVID-19 treatment according to the guideline.[4] After a period of treatment, the patient recovered well without the symptom of shortness of breath or cough during supine. In order to improve the prognosis furtherly, the revascularization should be performed only after the epidemic controlled.
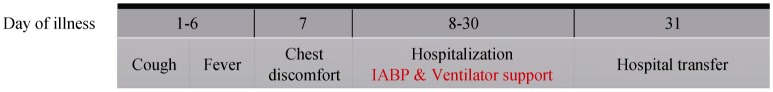
Figure 1. Timeline of disease course according to days from initial presentation of illness.
IABP: intra-aortic balloon pump.
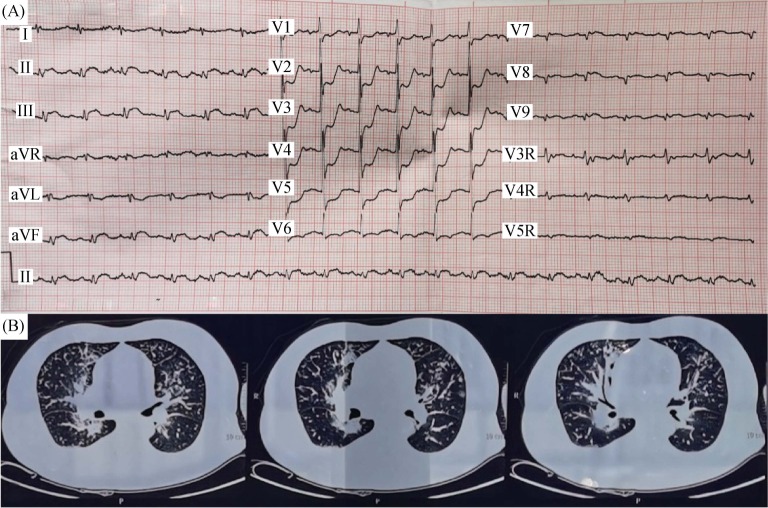
Figure 2. ECG and CT during chest discomfort in emergency department of Wuhan Asia Heart Hospital.
(A): ECG showed elevated ST-segment in II, III, and aVF leads, whereas depressed in V1-V6 leads; and (B): CT scanning showed both signs of viral pneumonia and pulmonary edema indicating heart failure. CT: computed tomography; ECG: electrocardiogram.
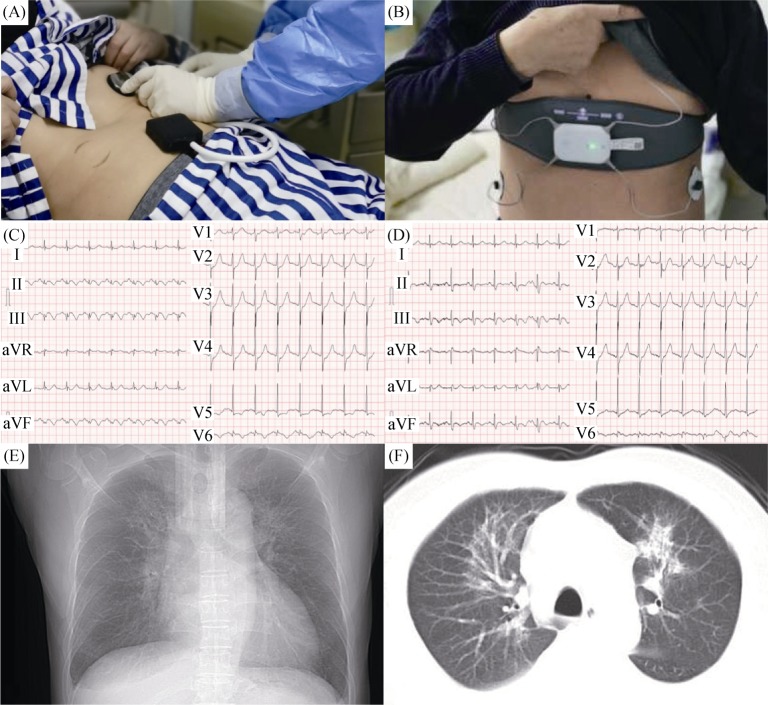
Figure 3. Role of wireless equipment in angina management post myocardial infarction in Wuhan Huoshenshan Hospital.
(A): Wireless stethoscope equipment; (B): tele-ECG equipment; (C): ECG showed ischemia in inferior wall during the patient admission; (D): ECG after medication; and (E & F): X-ray chest film and CT showed gradual absorption of ground glass opacity. CT: computed tomography; ECG: electrocardiogram.
COVID-19, also known as the global pandemic, has caused nearly 630,000 confirmed cases infected and more than 30,000 deaths according to the latest WHO report.[5] Although lung is acknowledged as the primary target organ attacked by the pathogen named SARS-CoV-2, the cardiovascular system is also severely affected due to mononuclear inflammatory infiltrates, microvessel thromboembolism, hypoxia and turbulent hemodynamics.[6],[7] In such state of COVID-19, the coronary plaques are unstable and fragile to rupture or erosion, causing following cascade of acute coronary syndrome. In our case, the patient initially presented with symptom of COVID-19, then suffered acute myocardial infarction suddenly due to abrupt blocking of the coronary flow. After that, the occurrence of concomitant acute myocardial infarction are adding injury to insult of COVID-19, aggravating the lung edema and debilitating the hemodynamics. Moreover, the concurrent cardiogenic and infectious shock are tough problems to tackle. Since the patient were initially rescued in the Wuhan Asia Heart Hospital, we have no clue of vital details concerning the successful emergency treatment except for the usage of both IABP and ventilator. However, owing to the revascularization were not performed considering insecure condition, the patient was still at high risk of myocardial ischemia and congestive heart failure after the hospital transfer. In such circumstance, how to make sure the continuity and concordance of the treatment, then differentiate and tackle similar symptoms caused by different pathogenesis are critical, which determined the effect of the patient's prognosis.
The contagious ward and isolation gown greatly restrain the usage of conventional medical instruments, such as stethoscope or ECG machine. In such scenarios, advanced medical equipment will be alternative and sometimes even the optimal choices. In this case, the usage of wireless stethoscope designed by military engineering broke out the restraint of isolation gown, through which we recognized the sign of congestive heart failure, rather than aggravated pneumonia infiltration or effusion. Moreover, the tele-ECG systems are both convenient and practical for usage. After the patient wearing the belt band, the ECG can be shown in app of mobile phone. Meanwhile, the tele analysis and conclusion made by the First Medical Center of Chinese PLA General Hospital at distance can be transferred to the front line of medical relief in minutes, assisting doctors in both diagnostics and management. Through usage and analysis of the tele-ECG and wireless stethoscope, we confirmed the angina diagnosis of this patient, which greatly helped to save precious time and finally assisted the rescue.
With the development of science and technology, new medical equipment is used to promote the evolution of medical practice. Owing to escort and assistance of novel equipment, such severe case with concurrent myocardial infarction and COVID-19 may have opportunity to wait for complete revascularization as early as possible.
Acknowledgments
All authors had no conflicts of interest to disclose. In the manuscript, we had the written informed consent of our patient to publish this case (including publication of images).
References
- 1.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. doi: 10.1056/NEJMoa2002032. Published Online First: 28 February 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. doi: 10.1001/jama.2020.4031. Published Online First: 13 March 2020. [DOI] [PubMed] [Google Scholar]
- 4.National Health Commission & National Administration of Traditional Chinese Medicine. Diagnosis and treatment plan for COVID-19 (trial version 6) Chin Med J (Engl) doi: 10.1097/CM9.0000000000000819. Published Online First: 17 March 2020. [DOI] [Google Scholar]
- 5.World Health Organization. About coronavirus disease 2019 (COVID-19). World Health Organization of coronavirus disease Web site. [(accessed Mar 30, 2020)]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/
- 6.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. doi: 10.1016/S2213-2600(20)30076-X. Published Online First: 18 February 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Restrepo MI, Reyes LF. Pneumonia as a cardiovascular disease. Respirology. 2018;23:250–259. doi: 10.1111/resp.13233. [DOI] [PubMed] [Google Scholar]