Abstract
The Trillat procedure is a surgical treatment for recurrent anterior shoulder instability in the setting of significant or irreparable rotator cuff tears in elderly patients. The procedure comprises an inferior closing wedge partial osteotomy of the coracoid process with fixation to the glenoid neck. This results in a lowered and medialized coracoid process that acts as a bone block and the conjoint tendon is brought closer to the glenohumeral joint, thus closing the subcoracoid space, which blocks humeral dislocation. We describe an arthroscopic step-by-step guided Trillat technique that is simple, efficient, and reproducible, while minimizing risk in the extra-articular subcoracoid space. Our technique does not require the release of the pectoralis minor tendon from the coracoid process, which reduces the risk of damaging the brachial plexus. We use a tight-rope fixation construct that allows progressive transfer of the coracoid process, limiting fracture risk and the risk of overtightening of the subscapularis muscle. Because there is a trend for more complex procedures being performed arthroscopically, it is important to develop and simplify operative techniques, aiding surgeons in achieving reproducible and reliable patient outcomes.
There are many described arthroscopic techniques for the management of recurrent anterior-inferior shoulder instability. In our practice, the choice of stabilization technique depends on the instability severity index score,1 the age, and the presence of rotator cuff tears. Recurrent anterior instability in the setting of significant or irreparable rotator cuff tears is not uncommon, with incidence reported by Walch et al.2 as 5% of anterior instability cases. Elderly patients with massive irreparable posterosuperior rotator cuff tears can become secondarily unstable because of the lack of a posterior checkrein.3 The Latarjet procedure is contraindicated in elderly patients because of the risk of coracoid fracture, avulsion fracture, and nonunion.
The Trillat procedure was first published in 19544 for the management of anteroinferior glenohumeral instability, and it brought satisfactory results in older patients with irreparable rotator cuff tears.2,5,6 The procedure requires the presence of a subscapularis tendon still attached to the humeral lesser tuberosity. The procedure comprises an inferior closing wedge partial osteotomy of the coracoid process with transfer and screw fixation to the glenoid neck. This results in a coracoid process that is lowered and medialized, and this acts as a bone block. The conjoint tendon is brought closer to the glenohumeral joint, thus closing the subcoracoid space, and it lowers the subscapularis, which combined, creates the “sling effect,” with the humeral head being pushed posteriorly in humeral abduction. The principles of our arthroscopic Trillat technique are the same. Our aim was to describe an arthroscopic surgical technique for the Trillat procedure in patients with anterior shoulder instability in the setting of irreparable rotator cuff tears.
Patient Positioning
General anesthesia and an interscalene nerve block are routinely used. We recommend performing this procedure with the patient in a semi-beach chair position with the arm placed freely on a moveable support (Trimano Fortis; Arthrex Inc., Naples, FL) without traction. The head is secured in a head rest with a slight tilt away from the operative side. At commencement of the procedure, the arm is placed 30° flexed and in neutral rotation.
Portals
The bone landmarks are drawn on the skin before commencement. In addition to the standard posterior viewing portals, 3 other portals are used for this procedure (Fig 1). First, the standard posterior portal is created in the palpable soft spot, 2 cm inferior and 1 cm medial to the posterolateral corner of the acromion. The anterolateral portal is located at the anterolateral corner of the acromion. The medial portal is 1 finger-breadth medial and proximal to the tip of the coracoid process. The inferolateral portal is 2 finger-breadths lateral to the tip of the coracoid process. Further details of portal placement will follow in the text. We use a 70° scope for the entire procedure because it allows superior visualization of the coracoid process with the scope positioned through the rotator interval while using the posterior portal. The advantage of viewing “around the corner” with a 70° scope obviates the need for extra portals.
Fig 1.

Photograph of a right shoulder showing the portals used during the arthroscopic Trillat procedure. NW = Anterolateral (“North-West” for a right shoulder), N = Medial (“North”), W = Inferolateral (“West” for a right shoulder). The fourth portal is the standard posterior portal (not visualized in this photograph).
Arthroscopic Diagnosis
The scope is introduced through the posterior portal. We routinely perform a systematic inspection of the joint and any associated intra-articular pathology is treated as appropriate. We perform a simulation of anterior dislocation for assessment for an engaging Hill-Sachs lesion. This is done under arthroscopic visualization with the arm placed in 90° of abduction and 90° of external rotation. During this maneuver, a humeral head dislocation can be seen and an engaging Hill-Sachs lesion identified. The procedure comprises 5 main steps, which are all performed arthroscopically (as shown in the procedural video 1). The instruments used have been designed and developed by one of our senior authors (P.B.) for the arthroscopic Latarjet7 and Trillat procedures (Latarjet Guiding System; Smith & Nephew Inc., Andover, MA).
Step 1: Extra-articular Coracoid Dissection
The anterolateral portal is created (Table 1). A radiofrequency electrocautery device (Super TurboVac 90; ArthroCare, Austin, TX) is best used to widely open the rotator interval and subcoracoid space because any bleeding should be efficiently coagulated. The rotator interval is dissected with release of the superior and middle glenohumeral ligaments. The arm is then placed into internal rotation across the patient’s thorax to relax the subscapularis and open the subcoracoid space.
Table 1.
Technical tips and tricks for portal positioning
| Posterior |
| Parallel to the glenoid, to ease passing of the glenoid drill guide. Use a needle first to confirm this |
| Anterolateral |
| A needle is used to ensure that instrumentation will be tangential to the under-surface of the coracoid. |
| As a guide, a good position is when the needle is generally parallel to the superior round tendinous portion of the subscapularis muscle. |
| If the portal is made too superior, it will be difficult to complete the most medial portion of the coracoid osteotomy later on. |
| Anteroinferior |
| Pass a needle under vision through the anterior deltoid muscle fibers two finger-breadths lateral to the coracoid process tip |
| Medial |
| Use 2 needles |
| Place the first needle at the tip of the coracoid process under vision |
| Place the second needle 1 finger-breadth proximal and medial to the first needle, which corresponds with the tip of the needle arriving just proximal to the pectoralis minor tendon insertion |
| This allows for the coracoid drill guide to arrive at a 45° angle and 5 mm from all sides of the coracoid process tip |
Releasing along the superior border of subscapularis leads to the base of the coracoid process. Dissection is then performed inferior to the arch of the coracoid process towards the tip. The coracoacromial and coracohumeral ligaments are detached from the coracoid process. The conjoint tendon is identified, and dissection is performed laterally only (Fig 2). Care should be taken to avoid dissection medial to the conjoint tendon and coracoid process because the brachial plexus and great vessels lie within the fat in this region. The arm is now flexed to 45° so that the supracoracoid space is opened by reducing the deltoid muscle tension. Dissection is performed superior to the coracoid process with care not to dissect too medially into the fat at this level because there are multiple small blood vessels that can bleed. The pectoralis minor is not detached from the medial border of the coracoid process to maintain coracoid stability and aid medialization.
Fig 2.
(A) Arthroscopic view from the posterior portal of a right shoulder showing the coracoid process (C) once dissection is complete. Note the plexus fat (PF) inferomedial to the coracoid process. (B) Arthroscopic view from the posterior portal of a right shoulder showing the conjoint tendon (CT) origin from the coracoid process (C) tip and the pectoralis minor (PM) tendon insertion left intact.
Next, the other 2 portals are made (Table 1). The inferolateral portal is made using a standard technique. To make the medial portal, 2 needles are placed. The first is placed at the tip of the coracoid process under vision, and the second needle is placed 1 finger-breadth proximal and medial to the first needle, which corresponds with the tip of the needle arriving just proximal to the pectoralis minor tendon insertion on the coracoid process.
Step 2: Coracoid Osteotomy
A switching stick is passed though the inferolateral portal into the subcoracoid space for the assistant to retract the subscapularis away from the coracoid process. The coracoid osteotomy is then performed through the anterolateral portal. We find that this is best performed using a combination of devices. We commence the osteotomy on the flat cortical under-surface using a motorized rasp (Smith & Nephew Inc.), which gives the exact inferior cortical resection width required. This is performed just distal to the angle of the coracoid or approximately 25 mm from the tip (Fig 3). In patients with good quality bone, we find a 5.5-mm motorized burr (Stryker, Kalamazoo, MI) to be maximally efficient in completing the osteotomy through the middle section of the coracoid process to osteotomize approximately 80% of the coracoid process, leaving the superior cortex intact. Our preference is to complete the most medial and superior portion of the osteotomy using a large Kerrison rongeur in a controlled manner with minimal risk to medial neurovascular structures. In our experience, it is important not to make the osteotomy too narrow in the superior portion, because in patients with good bone quality, it will require more force and be difficult to close the wedge and transfer the coracoid process without fracturing. A broader osteotomy superiorly allows for easier plastic deformation of the superior cortex during transfer with less force required and lower fracture risk.
Fig 3.
(A) Arthroscopic view from the posterior portal of a right shoulder showing the correct position for commencement of the coracoid (C) osteotomy using a motorized rasp. (B) Arthroscopic view from the posterior portal of a right shoulder showing the finished partial coracoid process (C) osteotomy of approximately 80% of the coracoid thickness.
Step 3: Coracoid Drilling and Suture Management
For this step, the switching stick, which is still present in the inferolateral portal, is switched from below to above the coracoid to retract the deltoid fibers superiorly, thus opening the space for coracoid process drilling. Still using the 70° scope from posteriorly, the coracoid guide (Smith & Nephew Inc.) is introduced through the medial portal to grasp the coracoid perpendicular to its surface. Usually the guide handle is angled 45° medially, with the patient’s head being tilted slightly away to allow this. This grasper guides the position of the drill hole to be 5-mm from the coracoid process tip. This is important in aiding distalization and medialization of the coracoid transfer. A first drill tipped K-wire housed inside an outer 2.8mm sleeve (RCG Drill; Smith & Nephew Inc.) is advanced through the guide and drilled until it exits the inferior surface of the coracoid process. The K-wire is then removed and replaced with a polydioxanone (PDS) suture, which after being passed though the sleeve and hole in the coracoid is retrieved with a suture grasper through the inferolateral portal. A pin puller is used to remove the drill sleeve from the coracoid process. The PDS is used to shuttle the Bone-Link button and sutures (Smith & Nephew Inc.) through the coracoid drill hole until the button is seated on the coracoid process superior cortex. The Bone-Link sutures are then moved to the medial portal for safe keeping.
Step 4: Glenoid Drilling and passing the Bone-Link
With the 70° scope still in the posterior viewing portal, the anterior capsule and labrum, if present, are elevated off the anterior rim of the glenoid at the level of the superior edge of subscapularis using electrocautery through the anterolateral portal. The anterior glenoid is then debrided to allow passage of the glenoid drill from posterior to anterior. This is best achieved with the arm in internal rotation to relax the subscapularis and using a switching stick though the inferolateral portal to depress the subscapularis anteroinferiorly creating space. A second switching stick is placed into the antero-lateral portal and the scope is now switched, for the first time, to the anterolateral portal after a third switching stick is placed in the posterior portal.
The scope is now rotated to view the posterior capsule, while a half-pipe cannula is slid along the posterior switching stick. Once the half-pipe is in place the switching stick is removed and electrocautery is used to open the posterior capsule around the half-pipe. This is important to facilitate the easy passing of the glenoid drill guide (Smith & Nephew Inc.) from posteriorly across the face of the glenoid to the anterior glenoid. This guide should be placed parallel to the glenoid and this ensures the drill tunnel exits 5 mm medial to the anterior glenoid rim. It should be placed level to the top of the subscapularis (or at the base of the coracoid, which corresponds to the 1 or 11 o’clock position on the glenoid for right and left shoulders) and not inferiorly because this will cause subscapularis impingement during arm rotation. The guide also serves to protect the subscapularis and the brachial plexus from injury from the drill tip. A cannula is passed percutaneously medially through the guide and pushed onto the posterior glenoid. The same K-wire housed inside an outer 2.8-mm drill sleeve used to drill the coracoid process is then drilled through the glenoid and visualized at its anterior exit point. Once the K-wire tip is identified, the guide is pushed 10 mm anteriorly against the subscapularis, and the drill is advanced until the drill sleeve is visualized. The K-wire is removed, and a PDS is passed from posteriorly into the drill sleeve.
The PDS is retrieved from the inferolateral portal using a suture grasper along with the 2 suture loops of the Bone-Link. A pin puller is used to remove the drill sleeve from the glenoid. The PDS is used to shuttle the Bone-Link strands though the glenoid and exit posteriorly. The half-pipe cannula is then replaced along the glenoid drill guide to facilitate its removal from the joint.
Step 5: Coracoid Mobilization and Final Fixation
The 2 loops of the Bone-Link are adjusted until they are of even length. A suture passer is used to aid passing the loops through the hole in the button, which is then pushed down the suture loops to the level of the skin. The 2 Bone-Link loops are then liberated, and a Nice Knot is made and gently tensioned to pass the button through the soft tissues and onto the posterior cortex of the glenoid.7 A suture tensioner (Smith & Nephew Inc.) is used to progressively tension the Bone-Link construct. This can be done under direct vision with the scope still positioned in the anterolateral portal and allow for gradual and controlled closure of the osteotomy with the coracoid moving downward and medially toward the glenoid neck (Fig 4). This can be done with the assistant testing internal and external rotation of the humerus after progressive tensioning of the Bone-Link to avoid overtightening and subscapularis subcoracoid impingement. Once the desired degree of coracoid transfer is achieved, the stabilizing conjoint tendon sling effect can be easily visualized under dynamic humeral external rotation (Fig 4). It is important to avoid over-tensioning and to leave enough space for the subscapularis to slide. The remaining protruding posterior suture loop can be cut, and the Nice-knot can be definitively locked with surgeon’s knots. An arthroscopic suture cutter is used to remove the excess suture.
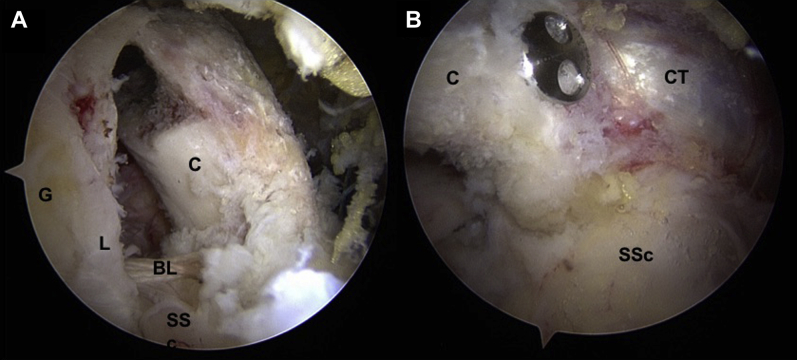
Fig 4.
(A) Arthroscopic view from the posterior portal of a right shoulder showing the completed coracoid process (C) transfer inferomedially after tensioning of the Bone-Link (BL). The subscapularis tendon (SSC) can be seen between the glenoid (G) and labrum (L) posteriorly and the coracoid process anteriorly. Care is taken not to over-tension the Bone-Link and cause subscapularis impingement. (B) Arthroscopic view from the North-West portal of a right shoulder showing the position of the low-profile coracoid button and the conjoint tendon (CT) sitting against the anterior surface of the subscapularis (SSc).
The scope can be switched back to the posterior portal at this stage using a switching stick placed into the half pipe cannula. At this point, the assistant can once again test the stability of the joint with humeral abduction and external rotation. If desired, the surgeon has the option to perform a soft tissue Bankart capsular-labral repair using the anterolateral portal and suture anchors.
Postoperative Care
Postoperative radiographs are obtained to verify correct coracoid process positioning and implant button positioning (Fig 5). A computed tomography scan is obtained 3 months after surgery to assess healing of the coracoid osteotomy. The patient is discharged from the hospital on the same day with the arm in a neutral rotation sling for 2 weeks. The patient starts a physiotherapy and hydrotherapy rehabilitation program after 2 weeks as per the Liotard Protocol to regain shoulder range of motion. Sling usage is ceased after 4 weeks. No heavy lifting is allowed within the first 3 months; however, return to sports or vigorous work activity is allowed after 3 months.
Fig 5.
(A) Preoperative radiograph showing the anatomical coracoid process position. (B) Postoperative radiograph showing the button fixation and the new inferior and medialized position of the coracoid process. (C) Scapula-Y radiograph showing the position of the buttons and the closer proximity of the coracoid process to the anterior glenoid.
Discussion
The technique initially described by Trillat4 has been a treatment for recurrent anterior shoulder instability with good long term results in often difficult to manage patients. Walch et al.2 reported 96% patient satisfaction with more than 10 years of follow up in patients with anterior instability with massive irreparable cuff tears. Ongoing instability has been reported as 16% by Walch et al.2, by Gerber et al.5 as 4% recurrent dislocation but 18% recurrent apprehension, and recently by Labattut et al.8 as 5.5% in a short-term follow-up of arthroscopically assisted open Trillat procedures. In both articles by Walch et al.2 and Gerber et al.,5 they reported glenohumeral osteoarthritis at final follow-up of 64.3% and 62%, respectively. This is expected because the patient cohorts had irreparable rotator cuff tears, and the natural history of cuff tear arthropathy is well documented. However, the Trillat procedure may delay the onset of cuff tear arthropathy by the double benefits of stabilizing the shoulder and preventing humeral head superior migration by lowering the subscapularis.
We prefer to treat patients with recurrent anterior shoulder instability and irreparable rotator cuff tears with the Trillat procedure because in such patients, often the only functional cuff remaining is the subscapularis and teres minor. In such patients, performing a Latarjet coracoid transfer via a subscapularis split may cause subscapularis injury and potentially result in a pseudoparalytic shoulder and also risk coracoid fracture or nonconsolidation because of poor bone quality in elderly patients (Table 2). The Trillat procedure avoids these potential complications and, furthermore, performed arthroscopically has the added benefits of allowing rotator cuff repair and Bankart capsular repair.
Table 2.
Decision-making: indications and contraindications for the Latarjet and Trillat procedures
| Latarjet procedure |
| Indications |
| Young patients with recurrent anterior instability |
| Significant glenoid bone loss |
| Engaging Hill-Sachs lesion |
| High level contact sport players |
| Failed soft tissue stabilization |
| Contraindications |
| Subscapularis tear |
| Elderly patients |
| Glenoid bone loss or fracture > 30%. (Relative contraindication) |
| Multidirectional instability |
| Voluntary anterior instability |
| Trillat procedure |
| Indications |
| Elderly patients with anterior instability and irreparable posterosuperior RCT |
| Young patients with hyperlaxity and anterior instability |
| Contraindications |
| Subscapularis tear |
| Shoulder pseudoparalysis |
| Loss of active external rotation |
| Engaging Hill-Sachs lesion |
| Glenoid bone loss |
Our arthroscopic Trillat technique is simpler and less technically demanding than arthroscopic Latarjet procedures, making it a good initial procedure for surgeons wanting to transition to extra-articular arthroscopic stabilization procedures (Table 3). An important advantage of this technique, compared with other open or arthroscopic Trillat techniques,8,9 is the lack of release of the pectoralis minor tendon from the coracoid process. This negates the need for dissection medial to the coracoid process and thus reduces the risk of serious intraoperative bleeding and damage to the musculocutaneous and axillary nerves. These complications are most surgeons’ greatest concern or indeed a barrier to performing arthroscopic procedures within the anterior extra-articular space.
Table 3.
Key points in performing the arthroscopic Trillat procedure
| Pearls |
| Use a 70° scope |
| Place the coracoid tunnel 5 mm from the coracoid tip to aid distalization and medialization of the coracoid transfer |
| Perform a partial inferior coracoid osteotomy of at least 80%. If the patient is male and the bone is of good quality, a more aggressive osteotomy is required to allow coracoid transfer |
| Progressive closure of the osteotomy is performed under vision with progressive tensioning of the tightrope while an assistant dynamically rotates the humerus, thus avoiding overtightening and sub-coracoid subscapularis impingement |
| Pitfalls |
| Leave the pectoralis minor tendon intact and avoid medial conjoint tendon dissection and in so doing reduce the risk of bleeding and musculocutaneous and axillary nerve injuries |
| Slow and controlled transfer of the osteotomy is performed to avoid coracoid fracture and over tightening of the |
| Bone-Link |
Another advantage of our technique, along with that of Valenti et al.9, who described an arthroscopic technique with a similar fixation device, is that the use of double-button tension fixation potentially reduces hardware complications10 and removal. Use of this fixation type may limit coracoid fractures and overtightening of the subscapularis between the glenoid neck and the conjoint tendon. Furthermore, the use of guided instrumentation greatly facilitates the ease with which the surgery can be performed. The specific instrumentation has proven reliable and reproducible in the arthroscopic Latarjet procedure, and it has been designed to specifically improve the safety of coracoid and glenoid drilling. The tensioner avoids the risk of over-tensioning and thus complete coracoid fracture.
With regard to potential limitations of this technique, the use of a 70° arthroscope and working in the anterior extra-articular space has a significant learning curve and is still considered technically demanding. The procedural duration is potentially longer than that of an open technique, therefore prolonging anesthetic time and the potential associated risks. Although the risk of complete coracoid osteotomy (fracture) is avoided with careful operative technique, if this does occur during coracoid transfer, then the salvage options for coracoid stabilization are best performed by conversion to an open technique. The cost of the specific instrumentation and implant is higher than that for an open technique with screw fixation.
In conclusion, this step-by-step guided Trillat technique has been developed to be simple, efficient, and reproducible, while minimizing risk in the extra-articular subcoracoid space. Because there is a trend for more complex procedures being performed all arthroscopically, it is important to develop and simplify operative techniques, aiding surgeons in achieving reproducible and reliable patient outcomes.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: Pascal Boileau has received financial remuneration from Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video is of an arthroscopic Trillat procedure performed on the right shoulder. This elderly patient with recurrent right anterior shoulder dislocation has an irreparable rotator cuff tear with a degenerate, but intact subscapularis tendon on preoperative CT arthrography. The patient is positioned in the beach chair position, and the portals are marked on the skin according to the anatomic landmarks. (NW, antero-lateral portal; N, medial portal; W, inferolateral portal.) Arthroscopy via the posterior portal confirms anteroinferior shoulder dislocation with manipulation. It was also confirmed that the patient had an irreparable posterosuperior rotator cuff tear. The decision is made to perform a Trillat coracoid transfer procedure. The video demonstrates the important procedural aspects with audio describing each step. At completion of the procedure, the bone block and conjoint tendon sling effect of the coracoid transfer can be seen arthroscopically, and the shoulder is clinically assessed to be stable.
References
- 1.Balg F., Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89:1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 2.Walch G., Dejour H., Trillat A.G. [Recurrent anterior luxation of the shoulder occurring after the age of 40] Rev Chir Orthop Reparatrice Appar Mot. 1987;73:609–616. [PubMed] [Google Scholar]
- 3.Craig E.V. The posterior mechanism of acute anterior shoulder dislocations. Clin Orthop Relat Res. 1984:212–216. [PubMed] [Google Scholar]
- 4.Trillat A. [Treatment of recurrent dislocation of the shoulder; technical considerations] Lyon Chir. 1954;49:986–993. [PubMed] [Google Scholar]
- 5.Gerber C., Terrier F., Ganz R. The Trillat procedure for recurrent anterior instability of the shoulder. J Bone Joint Surg Br. 1988;70:130–134. doi: 10.1302/0301-620X.70B1.3339045. [DOI] [PubMed] [Google Scholar]
- 6.Jouve F., Graveleau N., Nove-Josserand L., Walch G. [Recurrent anterior instability of the shoulder associated with full thickness rotator cuff tear: results of surgical treatment] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:659–669. doi: 10.1016/j.rco.2008.03.032. [DOI] [PubMed] [Google Scholar]
- 7.Boileau P., Gendre P., Baba M. A guided surgical approach and novel fixation method for arthroscopic Latarjet. J Shoulder Elbow Surg. 2016;25:78–89. doi: 10.1016/j.jse.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Labattut L., Bertrand V., Reybet Degat P.Y. Arthroscopy-assisted Trillat procedure for anterior shoulder instability: surgical technique and preliminary clinical results. Orthop Traumatol Surg Res. 2018;104:811–816. doi: 10.1016/j.otsr.2017.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Valenti P.M.C., Schoch B., Arango S., Werthel J. Arthroscopic Trillat corocoid transfer procedure using a cortical button for chronic anterior shoulder instability. Arthrosc Techn. 2019;8:e199–e204. doi: 10.1016/j.eats.2018.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butt U., Charalambous C.P. Complications associated with open coracoid transfer procedures for shoulder instability. J Shoulder Elbow Surg. 2012;21:1110–1119. doi: 10.1016/j.jse.2012.02.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video is of an arthroscopic Trillat procedure performed on the right shoulder. This elderly patient with recurrent right anterior shoulder dislocation has an irreparable rotator cuff tear with a degenerate, but intact subscapularis tendon on preoperative CT arthrography. The patient is positioned in the beach chair position, and the portals are marked on the skin according to the anatomic landmarks. (NW, antero-lateral portal; N, medial portal; W, inferolateral portal.) Arthroscopy via the posterior portal confirms anteroinferior shoulder dislocation with manipulation. It was also confirmed that the patient had an irreparable posterosuperior rotator cuff tear. The decision is made to perform a Trillat coracoid transfer procedure. The video demonstrates the important procedural aspects with audio describing each step. At completion of the procedure, the bone block and conjoint tendon sling effect of the coracoid transfer can be seen arthroscopically, and the shoulder is clinically assessed to be stable.