To the Editor,
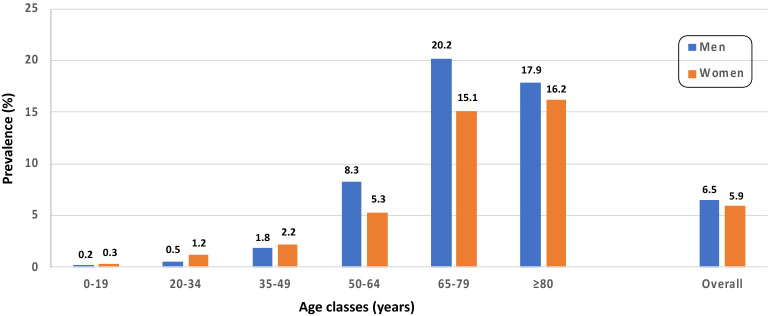
In China, among SARS-CoV-2-infected people, 12% of individuals have been reported to have diabetes mellitus (DM); this figure is quite low when comparing to reported figures in Italy [1]. In fact, as of April 2, 2020, from hospital records it has been possible to collect information on 1102 of 12,550 Italian fatalities from COVID-19 [2]. The mean number of concomitant diseases was 2.7 (median = 3): 31 patients (2.8%) were free of any other disease, 243 (22.1%) had only one, 263 (23.9%) had two, and 565 (51.3%) had at least three concomitant diseases [2]. Table 1 clearly shows that DM prevalence in deceased Italian COVID-19-positive patients was 31.5% [3]. The higher prevalence of DM in patients admitted with COVID-19 cannot be mostly a reflection of an older population known to be at higher risk for complications and mortality from COVID-19 because, while DM affects 17.9% of men and 16.2% of women over 80 years of age [4] against its overall 6.2% prevalence in the general population (Fig. 1), the over-80s accounted for 29.8% of deaths among COVID-19-positive patients (Table 2) against an overall figure of 11.8% (12,550 out of 106,399 documented infections in the hospital setting) [2].
Table 1.
Most common comorbidities observed in COVID-19-positive deceased patients.
Source: Istituto Superiore di Sanità [3] (modified)
| Disease | Number | Percentage |
|---|---|---|
| Ischemic heart disease | 302 | 27.4 |
| Atrial fibrillation | 249 | 22.6 |
| Heart failure | 186 | 16.9 |
| Stroke | 127 | 11.5 |
| Hypertension | 794 | 72.1 |
| Type 2 diabetes | 347 | 31.5 |
| Dementia | 173 | 15.7 |
| COPD | 202 | 18.3 |
| Active cancer in the past 5 years | 188 | 17.1 |
| Chronic liver disease | 45 | 4.1 |
| Chronic renal failure | 259 | 23.5 |
| Number of comorbidities | ||
| 0 | 31 | 2.8 |
| 1 | 243 | 22.1 |
| 2 | 263 | 23.9 |
| ≥ 3 | 565 | 51.3 |
Fig. 1.
DM prevalence in Italy as a function of age and gender according to the 2019 ARNO-Diabetes Report (modified) [4]
Table 2.
Mortality rate by age class in COVID-19-positive patients.
Source: Istituto Superiore di Sanità [2] (modified)
| Age groups (years) | Deceased [n (%)] | Mortality (%) |
|---|---|---|
| 0–9 | 0 (0%) | 0 |
| 10–19 | 0 (0%) | 0 |
| 20–29 | 6 (0%) | 0.1 |
| 30–39 | 29 (0.2%) | 0.4 |
| 40–49 | 110 (0.9%) | 0.8 |
| 50–59 | 479 (3.8%) | 2.3 |
| 60–69 | 1448 (11.5%) | 8.0 |
| 70–79 | 4196 (33.4%) | 21.8 |
| 80–89 | 5029 (40.1%) | 30.9 |
| ≥ 90 | 1251 (10%) | 28.7 |
| Unknown | 2 (0%) | 1.2 |
| Overall | 12,550 (100%) | 11.8 |
When putting together such a puzzle, we clearly understand why the prognosis in COVID-19-positive patients with DM can be very poor. Unfortunately, we cannot exclude that the worse prognosis in DM observed in this pandemic is not simply related to the disease itself. We must consider that in critically ill patients, treatment protocols often include extensive utilization of corticosteroids, which is known to further deteriorate infection-related hyperglycemia. It can be found in the same report from the Italian ISS (Istituto Superiore Sanità) that corticosteroids have been used in 34% of cases [2]. This is a serious situation if not well managed, because tight glucose control improves the length of hospitalization, the disease severity, and the mortality in ICU-staying patients with DM [5]. It is well known that, when facing critically ill patients with DM requiring ICU for acute respiratory failure, doctors have to progressively customize therapeutic protocols to ever-changing individual needs, comorbidities, and any symptoms of multiple organ/system involvement contributing to the clinical picture [6]. This particularly applies to the management of hyperglycemia, and particularly to its swings [1], which can increase pro-inflammatory factors and eventually prevent patients from benefiting of any otherwise well-managed treatment protocols. That is why, despite being fully aware that support of vital functions represents the primary goal for physicians taking care of COVID-19-infected patients, and that health professionals are overwhelmed by the dramatic situation, we strongly suggest the need in the presence of DM for continuous subcutaneous glucose monitoring systems to let them enhance the chance for a better prognosis.
Acknowledgements
We acknowledge the logistic support of Nefrocenter Research Network & Nyx, research start-up, Naples, Italy.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Sandro Gentile, Felice Strollo and Antonio Ceriello have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Peer Review
Please note, contrary to the journal’s standard single-blind peer review process, as a commentary this article underwent review by the journal’s Editor-in-Chief.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1.Gentile Sandro, Strollo Felice, Ceriello Antonio. COVID-19 infection in Italian people with diabetes: Lessons learned for our future (an experience to be used) Diabetes Research and Clinical Practice. 2020;162:108137. doi: 10.1016/j.diabres.2020.108137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Istituto Superiore di Sanità. Characteristics of COVID-19 patients dying in Italy: report based on available data on April 2nd. 2020 https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_2_april_2020.pdf. Accessed 3 Apr 2020.
- 3.Istituto Superiore di Sanità. Report on COVID-19 on April 2nd. 2020 https://www.epicentro.iss.it/coronavirus/bollettino/Infografica_2aprile%20ITA.pdf. Accessed 3 Apr 2020.
- 4.Rapporto ARNO-Diabete. 2019. http://www.siditalia.it/clinica/linee-guida-societari/send/80-linee-guida-documenti-societari/5025-rapporto-arno-diabete-2019. Accessed 3 Apr 2020.
- 5.Uijtendaal EV, Zwart-van Rijkom JEF, de Lange DW, Lalmohamed A, van Solinge WW, Egberts TCG. Influence of a strict glucose protocol on serum potassium and glucose concentrations and their association with mortality in intensive care patients. Crit Care. 2015;19:270. doi: 10.1186/s13054-015-0959-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kar P, Jones KL, Horowitz M, Deane AM. Management of critically ill patients with type 2 diabetes: the need for personalised therapy. World J Diabetes. 2015;6:693–706. doi: 10.4239/wjd.v6.i5.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.