Abstract
Superior capsular reconstruction (SCR) has become an increasingly popular choice in the treatment of massive, irreparable rotator cuff tears, pseudoparalysis, and in cases in which revision of previous rotator cuff repair is indicated. The SCR procedure is intended to restore the superior stabilizing forces of a deficient rotator cuff. This technique is accomplished by substituting an autograft or allograft between the superior glenoid and the greater tuberosity of the humerus, thus keeping the humeral head centered in the glenoid during shoulder forward flexion and abduction. Since its advent, numerous techniques have been described for this procedure. A fascia lata autograft was initially described; however, many surgeons in the United States have advocated for the use of a humeral dermal allograft. Yet, biomechanical studies have demonstrated elongation and thinning of this material. Thus, the Achilles tendon allograft may be an attractive choice for SCR, given its previous success with ligamentous and tendinous reconstructions. In this article, we present our technique of SCR using an Achilles tendon allograft.
Massive, irreparable rotator cuff tears with pseudoparalysis in young patients with minimal glenohumeral arthritis represent a unique challenge to the treating physician. Patients often present with decreased range of motion, pain, and limited ability to fulfill activities of daily living.1 While partial rotator cuff repair, arthroscopic debridement and tendon transfer including latissimus dorsi, trapezius, and pectoralis major have been described, high failure rates and patient dissatisfaction are associated.2 Reverse total shoulder arthroplasty has demonstrated favorable outcomes in patients older than 60 years of age; however, variable long-term implant survivorship and limited revision options make joint-preserving alternatives ideal, especially among younger patients.3 Thus, superior capsular reconstruction (SCR) has become an increasingly popular choice and has early encouraging outcomes.4
SCR is intended to restore the superior stabilizing forces to prevent proximal migration of the humeral head due to deficient rotator cuff. This technique is accomplished by substituting an autograft or allograft between the superior glenoid and the humeral head.5 Since its advent, numerous techniques have been described for this procedure.4,6, 7, 8, 9 It was first described by Mihata et al.4 using a fascia lata autograft and later popularized in the United States with use of dermal allograft.5 Outcomes following SCR using both graft types have been satisfactory, yet graft failure and reoperative rates remain high.4,10, 11, 12, 13 The Achilles tendon allograft may be an attractive choice due to the robustness it affords and previous success in treatment of other ligamentous and tendinous reconstructions throughout the body.14, 15, 16, 17 In this article, we present our technique of SCR using an Achilles tendon allograft.
Technique (With Video Illustration)
The patient is positioned laterally on a bean bag, with the arm held at 45° of abduction and 10° of forward flexion, with 10 pounds of traction (Fig 1). A standard posterior portal is established distal and medial to the posterolateral tip of the acromion. Under spinal needle visualization, a standard anterior portal is established within the rotator cuff interval (Video 1). We also use a larger lateral portal for the purposes of graft passage. Before proceeding with SCR, concomitant pathology should be addressed and appropriate surgical management performed.
Fig 1.
During superior capsular reconstruction, the patient is positioned laterally on a bean bag, with the right arm held at 45° of abduction and 10° of forward flexion (black arrows), with 10 pounds of traction (A). The anterior (blue arrow), lateral (white arrow), and posterior portals are marked. A standard posterior portal (black arrow) is established distal and medial to the posterolateral tip of the acromion (B). Under posterior portal visualization, a standard anterior portal (black arrows) is established within the rotator cuff interval (C, *refers to posterior portal). The large lateral portal is used for the purposes of graft passage (D).
Using the posterior portal for visualization, and the anterior for instrumentation, the superior glenoid is prepared with a combination of the shaver on forward and a radioablation device. Two GRYPHON Suture Anchors (DePuy Mitek, Warsaw, IN) are placed at the 11- o’clock and 1-o’clock positions on the superior glenoid, medial to the superior labrum (Fig 2). These can either be placed through the anterior portal, or, if necessary, via percutaneous anterolateral and/or posterolateral portals. The anchors are drilled at the edge of the articular margin, at 60° to the glenoid face for good fixation.
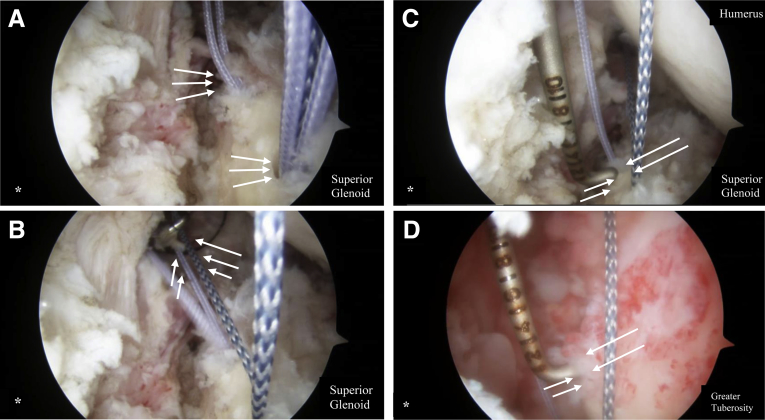
Fig 2.
Arthroscopic view of the right shoulder with the posterior viewing portal while the anterior portal is used for instrumentation during superior capsular reconstruction. Two anchors are placed at the 11- and 1-o’clock positions on the superior glenoid (white arrows), medial to the superior labrum (A). The anchors are drilled at the edge of the articular margin, at 60° to the glenoid face for good fixation. One suture from each anchor is passed out of the anterior portal (white arrows), and the other limb through the lateral portal (B). A marked probe is used to measure the glenoid footprint (white arrows) (C), the greater tuberosity footprint (white arrows) (D), and the intraarticular distance between the glenoid to the edge of the tuberosity. *Refers to posterior portal.
One suture is unloaded from each anchor. We leave the solid suture anteriorly and the striped posteriorly for identification purposes. One limb from each anchor is passed out of the anterior portal and the other limb through the lateral portal. A marked probe is used to measure the glenoid footprint, greater tuberosity footprint, and the intra-articular distance between the glenoid to the edge of the tuberosity. Next, using a shaver on forward, we prepare the greater tuberosity footprint on the humerus down to a base of bleeding bone, via the lateral portal.
Next, attention is turned to graft preparation. The narrow, or distal aspect of the Achilles tendon allograft (Medtronic, Minneapolis, MN) will be matched to the glenoid footprint. From the edge of the graft, 5 mm is marked to be the width of the glenoid footprint. From this mark, the intra-articular distance is measured and marked. This is usually between 20 and 25 mm. Finally, 15 mm is measured and marked to represent the glenoid tuberosity footprint.
On the greater tuberosity footprint, or wider side of the graft, 4 separate whip stitches are placed, using #2 ORTHOCORD suture (DePuy Mitek). Described in terms of intended future graft positioning, 2 are placed in parallel from the lateral aspect of the graft, creating one anterior and one posterior. These will correspond to the lateral row anchors. Two additional whip stitches are placed at the medial border, one on the anterior and one on the posterior aspect of the glenoid footprint. These will correspond with the medial row anchors. There are now 2 limbs anterior and posterior and 4 limbs projecting laterally from the glenoid footprint.
With graft preparation complete, attention is now turned to implantation (Fig 3). The 2 limbs of suture that were previously passed through the lateral portal are retrieved with an EXPRESSEW III Flexible Suture Passer (DePuy Mitek) simultaneously and drawn through the portal once more to confirm that there is no soft-tissue bridge. Each limb is passed through the glenoid footprint, outside of the body, in a Mason Allen fashion, and the 2 limbs are tied together.
Fig 3.
The Achilles tendon allograft is prepared for implantation during superior capsular reconstruction of the right shoulder. From the edge of the graft, 5 mm is marked to be the width of the glenoid footprint (A). From this mark, the intraarticular distance is measured, usually between 20 and 25 mm. Finally, 15 mm is marked to represent the glenoid tuberosity footprint. On the greater tuberosity footprint of the graft, 4 separate whip stitches are placed, using #2 ORTHOCORD sutures (B). Two are placed in parallel from the lateral aspect of the graft and two are placed at the medial border (red asterisks), corresponding with the lateral and medial row anchors, respectively. Each suture limb is passed through the glenoid footprint, outside of the body, in a Mason Allen fashion, and the two limbs are tied together (white arrows) (C).
Using a hemostat for assistance, and with tension on the 2 limbs of suture that have previously been passed out of the anterior portal, the graft is passed through the lateral portal, and the glenoid footprint is reduced down to the suture anchors. The 2 limbs of suture through the anterior portal are then tied down, securing the graft to the glenoid footprint via the anchors.
Next, attention is turned to securing the graft to the greater tuberosity footprint. Anterior and posterior accessory lateral portals are established for placement of the medial row anchors (Fig 4). The 2 limbs from the anterior medial row whip stitch are retrieved simultaneously from the anterior accessory lateral portal. The limbs from the posterior medial row whip stitch are retrieved via the posterior accessory lateral portal. Both limbs from the anterior medial row are loaded through a knotless anchor (Helix Advanced; DePuy Mitek).
Fig 4.
Using the posterior viewing portal during superior capsular reconstruction of the right shoulder, anterior and posterior accessory lateral portals are established for placement of the medial row anchors. The limbs from the posterior medial row whip stitch (white arrows) are retrieved via the posterior accessory lateral portal whereas the posterior portal is used for visualization (A). Both limbs from the anterior medial row are loaded through a knotless anchor (white arrows) (B). The tuberosity is tapped for anchor placement (white arrows) (C). The posterior medial row anchor is placed (white arrows) (D). It is important during this phase of the procedure to confirm that no soft tissue bridges exist, given that cannulas are not being used. The lateral row whip stitches are secured down to the footprint using the canula through the lateral portal for anchor passage. At this stage, any cuff remnant can be mobilized and tied down using extra suture from each anchor.
The tuberosity is tapped for anchor placement. With care passing through the same percutaneous path from which the sutures had passed through previously, the anchor is placed. It is important during this phase of the procedure to confirm that no soft-tissue bridges exist, given that cannulas are not being used. The graft is drawn down to bone with tension on the sutures before engaging the anchor. In the same fashion, the posterior medial row anchor is prepared and placed.
Also, using knotless anchors (Helix Advanced; DePuy Mitek), the lateral row whip stitches are secured down to the footprint using the canula through the lateral portal for anchor passage (Fig 5). At this stage, any cuff remnant can be mobilized and tied down using core suture from each anchor, closing the graft anteriorly and posteriorly to the native repaired cuff. If possible, the teres minor remnant should be tied down to the most posterior anchor. A self-retrieving EXPRESSEW III Flexible Suture Passer (DePuy Mitek) is used for this stage of the procedure.
Fig 5.
This diagram demonstrates the ideal location for anchor placement (red arrows) during superior capsular reconstruction of the right shoulder with an Achilles tendon allograft and the position of the graft relative to the glenoid and humerus once placed.
The portals are closed with a buried 3-0 MONOCRYL suture (Ethicon, Johnson & Johnson, Bridgewater, NJ) and dressed with DERMABOND (Ethicon) and a dry dressing. A sling is used for comfort for 2 weeks postoperatively, active range of motion is restricted for 6 weeks, the patient may begin immediate passive rom after surgery.
Discussion
In the young, active patient with massive, irreparable rotator cuff tear and minimal glenohumeral arthritis, SCR has become a valuable treatment option for those with a functional deltoid and intact subscapularis.7,13 Several small case studies have demonstrated significant improvement in active range of motion, increase in acromiohumeral distance, and improvement American Shoulder and Elbow Surgeons score.10, 11, 12, 13,18 Nonetheless, SCR is considered a technically challenging procedure that is constantly evolving. The technique presented here uses several unique features from graft selection to passage and final fixation to provide a robust, secure fixation (Table 1).
Table 1.
Key Points of Superior Capsular Reconstruction with Achilles Tendon Allograft
| Key Points | Achilles Tendon Allograft |
|---|---|
| Graft selection | Thicker and more robust Naturally tapered to provide greater humeral head coverage |
| Fixation technique | Modified Mason Allen on glenoid side Intercrossing whip stitches on tuberosity side |
| Cannula placement | No cannula laterally to avoid disruption of the graft |
Traditionally, SCR has been described in the literature as being performed using a folded fascia lata autograft or an acellular dermal allograft, with a minimum graft thickness of 3 mm recommended to decrease failure.18 Although satisfaction rates have been reported as high as 90% at 1-year postoperatively, graft failure rates range from 4.5% to 18.6% in case series using these graft options.4,10, 11, 12, 13 Graft thickness plays a key role in maintenance of glenohumeral stability following SCR. In biomechanical studies, Mihata et al.18, 19, 20 demonstrated that the fascia lata autograft, typically 6- to 8-mm thick, undergoes less elongation and provides better stability and thinning compared with dermal allografts, typically- 3 to 4-mm thick. Nonetheless, fascia lata autograft comes with increased risks of donor-site morbidity and increased operative time. The technique describe here uses an Achilles tendon allograft (Medtronic) to perform SCR that has a max thickness of ≥8 mm and tapers to 3 to 4 mm, broadening out to appropriately cover the humeral head.
To the authors’ knowledge, implementation of an Achilles tendon allograft for SCR has not been previously described. Nonetheless, the natural flared shape of an Achilles tendon allograft owes to an ideal graft for SCR. The tapered, flared aspect of the graft attaches to the tuberosity side of the reconstruction allowing for greater humeral head coverage, while thicker, narrow side is fixated to the glenoid. With an average graft thickness of ≥8 mm, it is conceivable that it is as robust as the fascia lata autograft without creating donor site morbidity or increased operative time. Furthermore, Achilles tendon allografts have been successfully used in tendon and ligamentous reconstructions throughout the body, including anterior cruciate ligament, posterior cruciate ligament reconstruction, and distal biceps repair.14, 15, 16,21,22 Unlike dermal patches, Achilles tendon allografts provide the opportunity for graft incorporation.
Unlike previously published techniques, the Achilles tendon allograft is introduced into the joint via a percutaneous pathway. By passing the graft by way of percutaneous path, we decrease the risk of graft disruption, as well as eliminate concerns about graft to cannula size. Once the graft is appropriately positioned, we use intercrossing whip stitches on the tuberosity side and modified Mason Allen sutures on the glenoid side to provide superior fixation.
Allograft use, however, has its own inherent limitations. When compared with fresh autografts, allograft tissue can be associated with lower biological activity.23 In addition, disease transmission, infection, and possible immune reaction may occur with the incorporation of allograft tissue.24 Finally, this technique does not restore shoulder, specifically supraspinatus and infraspinatus, strength and is more so intended to position and center the humeral head within the glenoid, especially while ranging the shoulder. The pearls and pitfalls, and advantages and disadvantages, of this technique are described in Tables 2 and 3, respectively.
Table 2.
Pearls and Pitfalls
| Step | Pearls | Pitfalls |
|---|---|---|
| Positioning and Preparation | The surgeon should ensure the patient is positioned laterally at 45° of abduction and 10° of forward flexion with 10 lb of traction. | Inadequate abduction and flexion lead to difficulty visualizing the intraarticular anatomy of the shoulder. |
| Portal creation | Establishing the anterior portal becomes important as this will be the working portal for the procedure. | The surgeon should ensure visualization of the spinal needle within the rotator cuff interval as lateral as possible before proceeding. |
| Superior glenoid footprint | Use the shaver on forward and use a radioablation device. | Compromised implantation may occur if an adequate base of bleeding bone is not achieved. |
| Placement of the suture anchors on the superior glenoid | The surgeon should ensure 2 anchors (DePuy Mitek) are placed at the 11- and 1-o’ clock positions, medial to the superior labrum. | If the anchors are not drilled at the edge of the articular margin at 60° to the glenoid face, there is risk for poor fixation. |
| Greater tuberosity footprint | Use the shaver on forward. | Compromised healing may occur if an adequate base of bleeding bone is not achieved. |
| Graft preparation | Use the narrow, thicker portion of the graft for the glenoid footprint and the wide, thinner portion for the glenoid tuberosity footprint. | Two medial and 2 lateral anchor rows using 4 separate whip stitches are necessary to fully secure the graft onto the glenoid tuberosity. |
| Implantation | Pass 2 limbs of suture through the glenoid footprint of the graft outside the body in a Mason Allen fashion and using the lateral portal, first secure the graft to the glenoid footprint. | Anterior and posterior accessory lateral portals are necessary for placement of the medial row anchors of the greater tuberosity footprint. |
| Wound closure | Use 3-0 MONOCRYL (Johnson & Johnson) to close the epidermal layer. | Bury MONOCRYL (Johnson & Johnson) to prevent stitch abscess |
Table 3.
Advantages and Disadvantages of Superior Capsular Reconstruction with Various Grafts
| Graft | Advantages | Disadvantages |
|---|---|---|
| Fascia lata autograft |
|
|
| Acellular dermal allograft |
|
|
| Achilles tendon allograft |
|
|
SCR using an Achilles tendon allograft may provide robust stability in young, active patients in whom reverse total shoulder arthroplasty is not a viable option. Unique features of the Achilles graft coupled with ease of graft passage and secure fixation provide an innovate approach to SCR.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.J.S. reports other from ISO-biologics, personal fees from Mitek, and other from New Jersey Orthopaedic Society, outside the submitted work. E.S.S. reports other from Johnson & Johnson and other from Merck, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
During superior capsular reconstruction of the right shoulder, the patient is positioned laterally on a bean bag, with the arm held at 45° of abduction and 10° of forward flexion, with ten pounds of traction. A standard posterior portal is established distal and medial to the posterolateral tip of the acromion. Under spinal needle visualization, a standard anterior portal is established within the rotator cuff interval. We also use a larger lateral portal for the purposes of graft passage. Using the posterior portal for visualization, and the anterior for instrumentation, the superior glenoid is prepared with a combination of the shaver on forward and a radioablation device. Two suture anchors are placed at the 11-o’clock and 1-o’clock positions on the superior glenoid, medial to the superior labrum via the anterior portal, or if necessary, via percutaneous anterolateral and/or posterolateral portals. The anchors are drilled at the edge of the articular margin, at 60° to the glenoid face for good fixation. One suture is unloaded from each anchor. We leave the solid suture anteriorly, and the striped posteriorly for identification purposes. One limb from each anchor is passed out of the anterior portal, and the other limb through the lateral portal. A marked probe is used to measure the glenoid footprint, greater tuberosity footprint, and the intraarticular distance between the glenoid to the edge of the tuberosity. Next, using a shaver on forward the greater tuberosity footprint on the humerus is prepared down to a base of bleeding bone, via the lateral portal. Graft preparation: The narrow, or distal aspect of the Achilles tendon autograft will be matched to the glenoid footprint. From the edge of the graft, 5 mm is marked to be the width of the glenoid footprint. From this mark, the intraarticular distance is measured and marked. This is usually between 20 and 25 mm. Finally, 15 mm is measured and marked to represent the glenoid tuberosity footprint. On the greater tuberosity footprint, or wider side of the graft, 4 separate whip stitches are placed, using a #2 ORTHOCORD suture. Described in terms of intended future graft positioning, two are placed in parallel, from the lateral aspect of the graft creating one anterior and one posterior. These will correspond to the lateral row anchors. Two additional whip stitches are placed at the medial border, one on the anterior and one on the posterior aspect of the glenoid footprint. These will correspond with the medial row anchors. There are now 2 limbs anterior and posterior and 4 limbs projecting laterally from the glenoid footprint. Graft implantation: The 2 limbs of suture that were previously passed through the lateral portal are retrieved with a flexible suture passer. simultaneously and drawn through the portal once more to confirm that there is no soft tissue bridge. Each limb is passed through the glenoid footprint, outside of the body, in a Mason Allen fashion, and the 2 limbs are tied together. Using a hemostat for assistance, and with tension on the 2 limbs of suture that have previously been passed out of the anterior portal, the graft is passed through the lateral portal, and the glenoid footprint is reduced down to the suture anchors. The 2 limbs of suture through the anterior portal are then tied down, securing the graft to the glenoid footprint via the anchors. Next, attention is turned to securing the graft to the greater tuberosity footprint. Anterior and posterior accessory lateral portals are established for placement of the medial row anchors. The 2 limbs from the anterior medial row whip stitch are retrieved simultaneously from the anterior accessory lateral portal. The limbs from the posterior medial row whip stitch are retrieved via the posterior accessory lateral portal. Both limbs from the anterior medial row are loaded through a knotless anchor. The tuberosity is tapped for anchor placement. With care passing through the same percutaneous path from which the sutures had passed through previously, the anchor is placed. It is important during this phase of the procedure to confirm that no soft tissue bridges exist, given that cannulas are not being used. The graft is drawn down to bone with tension on the sutures prior to engaging the anchor. In the same fashion the posterior medial row anchor is prepared and placed. Using knotless anchors (Helix Advanced; DePuy Mitek), the lateral row whip stitches are secured down to the footprint using the canula through the lateral portal for anchor passage. At this stage, any cuff remnant can be mobilized and tied down using core suture from each anchor, closing the graft anteriorly and posteriorly to the native repaired cuff. If possible, the teres minor remnant should be tied down to the most posterior anchor.
References
- 1.Sochacki K.R., McCulloch P.C., Lintner D.M., Harris J.D. Superior capsular reconstruction for massive rotator cuff tear leads to significant improvement in range of motion and clinical outcomes: A systematic review. Arthroscopy. 2019;35:1269–1277. doi: 10.1016/j.arthro.2018.10.129. [DOI] [PubMed] [Google Scholar]
- 2.Galvin J.W., Kenney R., Curry E.J. Superior capsular reconstruction for massive rotator cuff tears: A critical analysis review. JBJS Rev. 2019;7:e1. doi: 10.2106/JBJS.RVW.18.00072. [DOI] [PubMed] [Google Scholar]
- 3.Adams C.R., Denard P.J., Brady P.C., Hartzler R.U., Burkhart S.S. The arthroscopic superior capsular reconstruction. Am J Orthop (Belle Mead NJ) 2016;45:320–324. [PubMed] [Google Scholar]
- 4.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Cvetanovich G.L., Waterman B.R., Verma N.N., Romeo A.A. Management of the irreparable rotator cuff tear. J Am Acad Orthop Surg. 2019;27:909–917. doi: 10.5435/JAAOS-D-18-00199. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart S.S., Denard P.J., Adams C.R., Brady P.C., Hartzler R.U. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. doi: 10.1016/j.eats.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hirahara A.M., Adams C.R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e637–e641. doi: 10.1016/j.eats.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petri M., Greenspoon J.A., Millett P.J. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e751–e755. doi: 10.1016/j.eats.2015.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sutter E.G., Godin J.A., Garrigues G.E. All-arthroscopic superior shoulder capsule reconstruction with partial rotator cuff repair. Orthopedics. 2017;40:e735–e738. doi: 10.3928/01477447-20170615-01. [DOI] [PubMed] [Google Scholar]
- 10.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 11.Hirahara A.M., Andersen W.J., Panero A.J. Superior capsular reconstruction: Clinical outcomes after minimum 2-year follow-up. Am J Orthop (Belle Mead NJ) 2017;46:266–278. [PubMed] [Google Scholar]
- 12.Mihata T., Lee T.Q., Fukunishi K. Return to sports and physical work after arthroscopic superior capsule reconstruction among patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:1077–1083. doi: 10.1177/0363546517753387. [DOI] [PubMed] [Google Scholar]
- 13.Pennington W.T., Bartz B.A., Pauli J.M., Walker C.E., Schmidt W. Arthroscopic superior capsular reconstruction with acellular dermal allograft for the treatment of massive irreparable rotator cuff tears: Short-term clinical outcomes and the radiographic parameter of superior capsular distance. Arthroscopy. 2018;34:1764–1773. doi: 10.1016/j.arthro.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Ding D.Y., Ryan W.E., Strauss E.J., Jazrawi L.M. Chronic distal biceps repair with an achilles allograft. Arthrosc Tech. 2016;5:e525–e529. doi: 10.1016/j.eats.2016.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forsythe B., Haro M.S., Bogunovic L. Biomechanical evaluation of posterior cruciate ligament reconstruction with quadriceps versus Achilles tendon bone block allograft. Orthop J Sport Med. 2016;4 doi: 10.1177/2325967116660068. 2325967116660068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mabe I., Hunter S. Quadriceps tendon allografts as an alternative to Achilles tendon allografts: A biomechanical comparison. Cell Tissue Bank. 2014;15:523–529. doi: 10.1007/s10561-014-9421-5. [DOI] [PubMed] [Google Scholar]
- 17.Murthi A.M., Ramirez M.A., Parks B.G., Carpenter S.R. Lacertus fibrosus versus Achilles allograft reconstruction for distal biceps tears: A biomechanical study. Am J Sports Med. 2017;45:3340–3344. doi: 10.1177/0363546517727511. [DOI] [PubMed] [Google Scholar]
- 18.Mihata T., Bui C.N.H., Akeda M. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elb Surg. 2017;26:2158–2166. doi: 10.1016/j.jse.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44:1423–1430. doi: 10.1177/0363546516631751. [DOI] [PubMed] [Google Scholar]
- 20.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical effect of thickness and tension of fascia lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy. 2016;32:418–426. doi: 10.1016/j.arthro.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Lädermann A., Denard P.J., Abrassart S., Schwitzguébel A.J.-P. Achilles tendon allograft for an irreparable massive rotator cuff tear with bony deficiency of the greater tuberosity. Knee Surg Sports Traumatol Arthrosc. 2017;25:2147–2150. doi: 10.1007/s00167-016-3989-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weber A.E., Mayer E.N., Nathani A. How variable are Achilles allografts used for anterior cruciate ligament reconstruction? A biomechanical study. Am J Sports Med. 2018;46:1870–1876. doi: 10.1177/0363546518768780. [DOI] [PubMed] [Google Scholar]
- 23.Diniz P., Pacheco J., Flora M. Clinical applications of allografts in foot and ankle surgery. Knee Surg Sports Traumatol Arthrosc. 2019;27:1847–1872. doi: 10.1007/s00167-019-05362-0. [DOI] [PubMed] [Google Scholar]
- 24.Chaudhury S., Wanivenhaus F., Fox A.J., Warren R.F., Doyle M., Rodeo S.A. Allograft replacement for absent native tissue. Sports Health. 2013;5:175–182. doi: 10.1177/1941738112456668. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
During superior capsular reconstruction of the right shoulder, the patient is positioned laterally on a bean bag, with the arm held at 45° of abduction and 10° of forward flexion, with ten pounds of traction. A standard posterior portal is established distal and medial to the posterolateral tip of the acromion. Under spinal needle visualization, a standard anterior portal is established within the rotator cuff interval. We also use a larger lateral portal for the purposes of graft passage. Using the posterior portal for visualization, and the anterior for instrumentation, the superior glenoid is prepared with a combination of the shaver on forward and a radioablation device. Two suture anchors are placed at the 11-o’clock and 1-o’clock positions on the superior glenoid, medial to the superior labrum via the anterior portal, or if necessary, via percutaneous anterolateral and/or posterolateral portals. The anchors are drilled at the edge of the articular margin, at 60° to the glenoid face for good fixation. One suture is unloaded from each anchor. We leave the solid suture anteriorly, and the striped posteriorly for identification purposes. One limb from each anchor is passed out of the anterior portal, and the other limb through the lateral portal. A marked probe is used to measure the glenoid footprint, greater tuberosity footprint, and the intraarticular distance between the glenoid to the edge of the tuberosity. Next, using a shaver on forward the greater tuberosity footprint on the humerus is prepared down to a base of bleeding bone, via the lateral portal. Graft preparation: The narrow, or distal aspect of the Achilles tendon autograft will be matched to the glenoid footprint. From the edge of the graft, 5 mm is marked to be the width of the glenoid footprint. From this mark, the intraarticular distance is measured and marked. This is usually between 20 and 25 mm. Finally, 15 mm is measured and marked to represent the glenoid tuberosity footprint. On the greater tuberosity footprint, or wider side of the graft, 4 separate whip stitches are placed, using a #2 ORTHOCORD suture. Described in terms of intended future graft positioning, two are placed in parallel, from the lateral aspect of the graft creating one anterior and one posterior. These will correspond to the lateral row anchors. Two additional whip stitches are placed at the medial border, one on the anterior and one on the posterior aspect of the glenoid footprint. These will correspond with the medial row anchors. There are now 2 limbs anterior and posterior and 4 limbs projecting laterally from the glenoid footprint. Graft implantation: The 2 limbs of suture that were previously passed through the lateral portal are retrieved with a flexible suture passer. simultaneously and drawn through the portal once more to confirm that there is no soft tissue bridge. Each limb is passed through the glenoid footprint, outside of the body, in a Mason Allen fashion, and the 2 limbs are tied together. Using a hemostat for assistance, and with tension on the 2 limbs of suture that have previously been passed out of the anterior portal, the graft is passed through the lateral portal, and the glenoid footprint is reduced down to the suture anchors. The 2 limbs of suture through the anterior portal are then tied down, securing the graft to the glenoid footprint via the anchors. Next, attention is turned to securing the graft to the greater tuberosity footprint. Anterior and posterior accessory lateral portals are established for placement of the medial row anchors. The 2 limbs from the anterior medial row whip stitch are retrieved simultaneously from the anterior accessory lateral portal. The limbs from the posterior medial row whip stitch are retrieved via the posterior accessory lateral portal. Both limbs from the anterior medial row are loaded through a knotless anchor. The tuberosity is tapped for anchor placement. With care passing through the same percutaneous path from which the sutures had passed through previously, the anchor is placed. It is important during this phase of the procedure to confirm that no soft tissue bridges exist, given that cannulas are not being used. The graft is drawn down to bone with tension on the sutures prior to engaging the anchor. In the same fashion the posterior medial row anchor is prepared and placed. Using knotless anchors (Helix Advanced; DePuy Mitek), the lateral row whip stitches are secured down to the footprint using the canula through the lateral portal for anchor passage. At this stage, any cuff remnant can be mobilized and tied down using core suture from each anchor, closing the graft anteriorly and posteriorly to the native repaired cuff. If possible, the teres minor remnant should be tied down to the most posterior anchor.