Following the order of the French president Emmanuel Macron on March 16, 2020, the French Military Health Service designed a 30-bed field military intensive care hospital. In an unprecedented manner, the “Élément Militaire de Réanimation du Service de Santé des Armées” (EMRSSA, Field Intensive Care Unit of the French Military Health Service) offered a full integrative intensive care system. The EMRSSA field hospital joined and supported the Émile-Muller hospital in Mulhouse, an 850-bed general hospital (Fig. 1 A). Prior to the EMRSSA field hospital deployment, the Émile-Muller hospital increased the number of its intensive care unit (ICU) beds from 36 to 62. The EMRSSA field hospital offered 30 additional ICU beds.
Fig. 1.
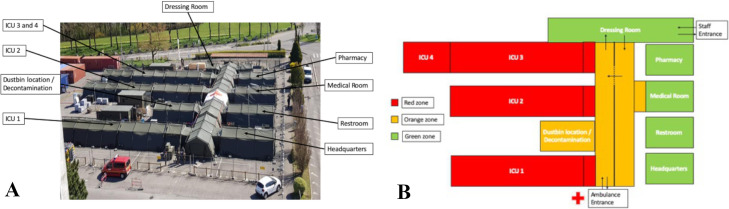
A. Aerial view of the EMRSSA. B. General organisation of the EMRSSA.
The EMRSSA team mission aimed to achieve two main objectives in strenuous conditions:
-
•
first, to treat critically ill patients with COVID-19 associated Acute Respiratory Distress Syndrome (ARDS) according to the best standards of care [1];
-
•
second, to protect caregivers [2].
The EMRSSA field hospital was built up, tested and secured from March 21 to 23, 2020. Fully equipped with critical care devices of the highest standard, three ICU wings were engaged progressively. Each ICU bed was equipped with a portable lightweight advanced, turbine-driven ventilator, a monitor, six syringe pumps, a volumetric pump, an enteral feeding pump, an alternating pressure mattress and a suction unit. Each wing was also equipped with additional devices: an ultrasound system, a portable blood analyser and a defibrillator. One oxygen concentrator provided the medical oxygen supply for each wing.
To ensure the protection of caregivers, the EMRSSA was divided into three different areas (red, orange, and green – Fig. 1B), each with specific levels of personal protective equipment (respectively wearing of full personal protective equipment: FFP2 or FFP3 mask, gown, gloves, eye protection and apron; wearing of FFP2 mask; wearing of surgical mask). Dressing and undressing procedures were conducted under the close supervision of biohazard-specialised soldiers from the “Régiment Médical” (RMED–Medical Regiment) and public health nurses.
The EMRSSA was connected to the Émile-Muller hospital's computer network to access clinical, biological, and radiological data, hospital protocols, and to easily and quickly transmit information in case of patient transfer. The EMRSSA was integrated as a new ICU of the Émile-Muller hospital, communication was permanent between the medical teams, and medical regulation ensured that each patient was at the right place to receive the adequate treatment.
From March 24 to April 17, 2020, 46 critically ill SARS-CoV-2 patients were transferred into the EMRSSA field hospital. The median age was 62 (interquartile range 53–67) years and 37 (80%) were male. The median weight was 85 (77–91) kg and median body mass index was 28 (25–32) kg/m2. The median in hospital length stay and ICU length stay before admission to EMRSSA were 4 (3–5) and 3 (1–4) days, respectively. On the day of admission in the EMRSSA, the median SAPS 2 score was 38 (27–49), the median SOFA score was 7 (6–10). All patients admitted in the EMRSSA presented with the following conditions: general anaesthesia, tracheal intubation, and mechanical ventilation.
The respiratory support strategies driven for these ARDS COVID-19 patients included protective mechanical ventilation, perfusion of neuromuscular blocking agents, prone positioning, recruitment manoeuvres, and inhalation of nitric oxide if indicated for each of these propositions. Different procedures were segmented in order to limit movements inside the EMRSSA and cross-contamination of caregivers. For example, an ears-nose-throat surgery team was deployed to perform percutaneous tracheostomies. This early tracheostomy responded to collective strategies that could allow faster weaning from mechanical ventilation, shorter length of stay in the ICU and better reorganisation of patient flows. Moreover, if the patient needed an extrarenal purification or an extracorporal oxygenation, the patient was sent back to the ICUs inside the Émile-Muller hospital.
In this military mission, several issues were resolved during the creation and even after the opening on March 24, 2020. First, we had to create ICU shift groups composed of physicians and paramedics coming from different ICUs of eight French military training hospitals. Some paramedics who did not usually work in ICU had to adapt quickly to a new and highly technical environment under challenging conditions, with the help of intensivists and experimented ICU nurses. Then, we had to be flexible and to adapt to face unexpected situations: pharmacy shortages, or unforeseen needs such as mechanical restraints for awakening patients. The access to the CT scanner was uneasy, and we had to plan intra-hospital ambulance transports carefully. Ambient temperature was also challenging, because of negative temperatures outside down to −5 °C during the nights and up to 33 °C inside the EMRSSA during the day. However, air conditioning and heating were available. None of the equipment failed in the high or low temperatures, except the portable blood analyser that did not work at temperatures above 30 °C.
Despite an austere environment and an exceptional health crisis, medical, paramedical staff, RMED soldiers and equipment performed well and approached the recommended standards of care. The EMRSSA was one of the French Military Health Service response to the COVID-19 pandemic in France, along with air evacuation of COVID-19 ICU patients with the MORPHEE module [3], and naval evacuation with Mistral-class landing helicopter deck. Not only during military operations far away from France, but also in the national territory, in an unprecedented situation, the French Military Health Service remained faithful to its motto: “Your life, our fight”.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgments
The authors thank all the teams involved in this operation: anaesthesiologists and intensivists, health caregivers, pharmacists and the RMED personals. Moreover, the authors pay a great tribute to the civilian ICU and medical teams from the Émile-Muller hospital: Dr Christian Meyer, Dr Odile Theissen, Dr Khaldoun Kuteifan, Dr Philippe Guiot, Dr Xavier Nazica, Dr Marc Noizet, and their collaborators.
References
- 1.Alhazzani W., Møller M.H., Arabi Y.M., Loeb M., Gong M.N., Fan E. Surviving Sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19) Intensive Care Med. 2020 doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verbeek J.H., Rajamaki B., Ijaz S., Sauni R., Toomey E., Blackwood B. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2020 doi: 10.1002/14651858.CD011621.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luft A., Corcostegui S.-P., Millet M., Gillard J., Boissier J., Rondy P. Aeromedical evacuations within the French armed forces: analysis of 2129 patients. Mil Med. 2020;185:468–476. doi: 10.1093/milmed/usz268. [DOI] [PubMed] [Google Scholar]