Abstract
The coronavirus disease 2019 (COVID-19) has had a profound global effect. Its rapid transmissibility has forced whole countries to adopt strict measures to contain its spread. As part of necessary pandemic planning, most Canadian cardiac surgical programs have prioritized and delayed elective procedures in an effort to reduce the burden on the health care system and to mobilize resources in the event of a pandemic surge. While the number of COVID-19 cases continue to increase worldwide, new cases have begun to decline in many jurisdictions. This “flattening of the curve” has inevitably prompted discussions around reopening of the economy, relaxing some public health restrictions, and resuming nonurgent health care delivery. This document provides a template for cardiac surgical programs to begin to ramp-up the delivery of cardiac surgery in a deliberate and graded fashion as the COVID-19 pandemic burden begins to ease that is guided by 3 principles. First, all recommendations from public health authorities regarding COVID-19 containment must continue to be followed to minimize disease spread, ensure patient safety, and protect health care personnel. Second, patients awaiting elective cardiac surgery need to be proactively managed, reprioritizing those with high-risk anatomy or whose clinical status is deteriorating. Finally, case volumes should be steadily increased in a mutually agreed upon fashion and must balance the clinical needs of patients awaiting surgery against the overall requirements of the health care system.
Résumé
La maladie à coronavirus 2019 (COVID-19) a eu de profondes répercussions partout dans le monde. Sa vitesse de transmission a forcé des pays entiers à mettre en place des mesures rigoureuses pour en limiter la propagation. Conformément aux plans établis en cas de pandémie, la plupart des programmes de chirurgie cardiaque du Canada ont établi l’ordre de priorité des interventions et reporté celles qui n’étaient pas urgentes, afin de réduire les pressions sur le système de santé et de mobiliser les ressources en prévision d’une flambée pandémique. Bien que le nombre de cas de COVID-19 dans le monde ne cesse d’augmenter, les nouveaux cas ont commencé à diminuer dans beaucoup de pays. Cet « aplatissement de la courbe » a inévitablement suscité des discussions sur la réouverture de l’économie, l’assouplissement de certaines mesures de santé publique et la reprise de la prestation des soins de santé non urgents. Le présent article propose un modèle reposant sur trois principes pour aider les programmes de chirurgie cardiaque à reprendre graduellement leurs activités d’une manière ordonnée, alors que le fardeau de la pandémie de COVID-19 commence à s’alléger. D’abord, il faut continuer de suivre toutes les recommandations des autorités de santé publique visant à endiguer la COVID-19, afin de limiter le plus possible la propagation de la maladie, d’assurer la sécurité des patients et de protéger le personnel soignant. Ensuite, il faut prendre en charge de manière proactive les patients qui sont en attente d’une intervention chirurgicale cardiaque non urgente, et revoir la priorité de ceux qui présentent un problème anatomique associé à un risque élevé et de ceux dont l’état de santé se détériore. Enfin, il faut augmenter régulièrement le volume de cas traités, d’une manière approuvée par tous les intervenants, et trouver un juste équilibre entre répondre aux besoins des patients en attente d’une intervention et répondre aux besoins globaux du système de santé.
The Canadian Society of Cardiac Surgeons (CSCS) recently provided guiding statements related to the practice of cardiac surgery during the acceleration phase of the COVID-19 pandemic.1 These statements were aimed at providing cardiac surgeons across Canada with guidance on the subjects of leadership, risk reduction, and the triaging of patients on the wait list. Now, as the rate of new cases of COVID-19 begins to decline with flattening of the epidemiologic curve in certain jurisdictions, discussions to relax public health restrictions and resume nonurgent health care delivery are starting to intensify.
The notion of ramping-up, though, is a sensitive subject. Although there is a desire to reestablish what society once knew as being normal, there is a reluctance to return to “business as usual.” Cardiac surgical programs face a similar predicament. Significant efforts have been made by cardiac surgery teams to prioritize and delay elective cardiac surgery cases so that health care resources, in particular critical care resources, may be liberated to treat those most severely affected by COVID-19. However, there is growing concern about the increased risk that patients with surgical cardiac disease face by being asked to wait indefinitely for their life-saving procedure.
As such, decisions to reexpand surgical case volume will require thoughtful and appropriate caution as we navigate through this global pandemic. There will be a need to make collaborative decisions, all the while maintaining the awareness and flexibility needed to readjust our escalation strategy in response to new and emerging data. It is with this in mind that the CSCS has proposed the following guiding statements. On the basis of the expert opinions of cardiac surgical and critical care leaders from across Canada, these guiding statements provide a template for cardiac surgical programs to increase cardiac care in a deliberate and graded fashion as the COVID-19 pandemic burden begins to ease (Fig. 1 ).
-
1.
As cardiac surgical programs begin to ramp-up, care must be taken to instill confidence among patients and health care providers that their safety remains a priority. To this effect, cardiac surgical programs must continue to respect and enforce the precautions and guidelines that have been put in place by their respective institutions and by the public health authorities at all levels of government to manage and contain COVID-19, limit the risk of nosocomial infection, ensure patient safety, and protect health care personnel. These include, but are not limited to, hand hygiene, the use of personal protective equipment, the creation of COVID-19-free units, social distancing, self-isolation, and travel restrictions.
-
2.Comprehensive screening procedures to identify patients at increased risk for COVID-19 should continue to be respected and enforced as cardiac surgical programs begin to ramp-up. These include the following:
-
A.Standardized clinical screening questionnaires before admission to the hospital, ideally via telephone, focusing on the clinical history of patients and their cohabitants (including viral-like symptoms compatible with COVID-19).
-
B.Initial admission to an isolation room within the hospital where additional screening and/or testing is performed as needed.
-
C.When admitted to the ward, daily clinical screening of patients to elicit signs and symptoms of viral illness and identify patients who might have been in the incubation or presymptomatic phase of infection on admission.
-
A.
-
3.The validity of COVID-19 testing has been the source of significant debate, and there is presently no test available that can reliably rule out COVID-19, particularly in the absence of symptoms. Despite this, nasopharyngeal swab testing for COVID-19, including rapid molecular tests, are being performed routinely across Canada with many centres having the ability to obtain test results within hours. To this effect, the CSCS provides the following guidance to COVID-19 test interpretation in the ramp-up phase on the basis of best available evidence at time of writing.
-
A.Nasopharyngeal swab testing for COVID-19 has a diminished sensitivity with false negative rates between 26% and 100%.2 Clinical sensitivity is reduced because of poor-quality specimen collection,3 timing of collection as it relates to an exposure or the onset of symptoms (higher false negative rates have been noted in the asymptomatic or preclinical period),2 or the presence of more advanced disease at which time the virus might be more localized to the lung as opposed to the nasopharynx.4
-
B.Patients with negative molecular testing in whom the clinical suspicion of COVID-19 infection remains high should stay in isolation per the guidance of institutional infection control practitioners. Additional investigative tools that might be considered to help confirm the diagnosis of COVID-19 in the appropriate setting include repeating nasopharyngeal specimen collection, endotracheal aspirates for molecular testing, and/or computed tomography imaging.
-
C.As testing for serologic immunity becomes more readily available, patients should be screened for antibodies, if possible, to assess for immunity secondary to previous natural infection.
-
A.
-
4.Given the protracted nature of this pandemic, cardiac surgery programs must continue to proactively manage every patient on their wait list despite reexpansion of case volumes. Aspects of this management might include, but are not limited to, the following:
-
A.All wait list patients must be contacted via telephone, teleconference, or videoconference at least every 2-4 weeks so that their clinical status might be assessed and reassessed on a regular basis.
-
B.Each centre must have a clear mechanism in place to formally assess patients with deteriorating symptoms, unstable clinical characteristics, or high-risk anatomy and to order any noninvasive tests as needed.
-
C.Peer review with other members of the heart team is highly encouraged for complex patients.
-
A.
-
5.
Efforts to ramp-up must be done within the local context of the pandemic, as a careful balance must be struck between the clinical needs of patients awaiting cardiac surgery, risk of nosocomial infection, and the overall resource requirements of the health care system. Any intention to escalate or reescalate cardiac surgical volumes requires regular communication between members of the heart team, intensive care units, hospital administration, provincial department of health, and/or public health officials. This communication should occur frequently, with consideration given to daily meetings if feasible. Ideally, a provincial dashboard that provides a real-time trend of resource utilization (eg, hospital admissions, intensive care unit admissions, ventilator use, personal protective equipment availability) should be created to facilitate forecasting, communication, and rapid decision-making.
-
6.
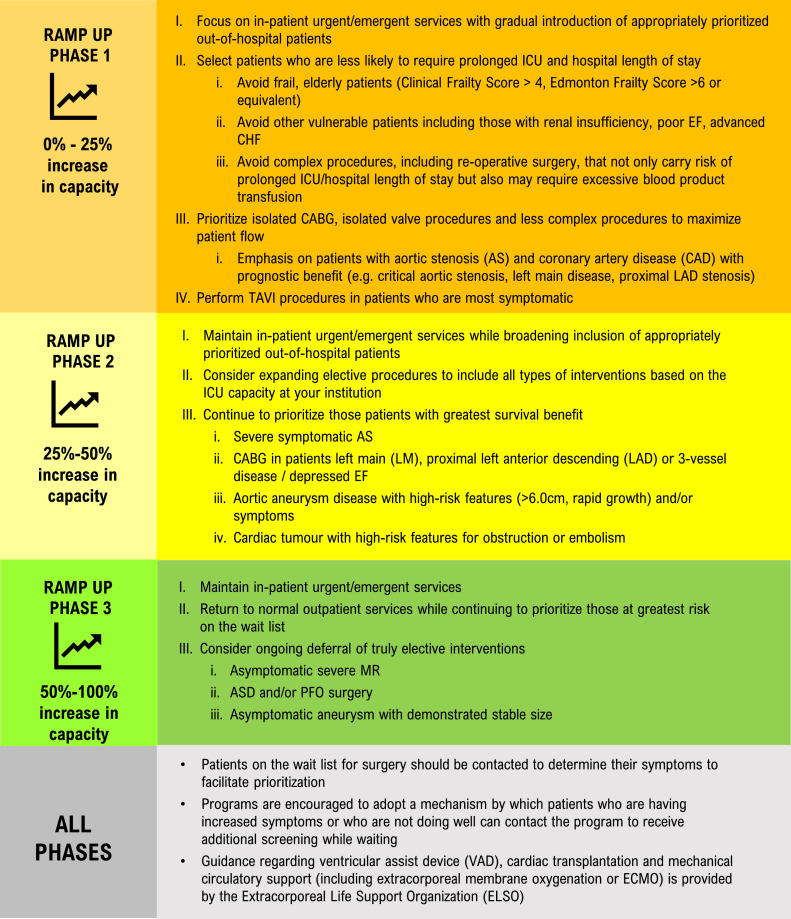
When ramping-up, the CSCS proposes a phased implementation approach that is on the basis of what phase your hospital is at with respect to its reexpansion or increase in hospital capacity (Fig. 2). We have defined increase in hospital capacity as the percentage of resources previously allocated to the COVID-19 pandemic that have now been reallocated to the management of non-COVID-19 patients. Phase 1 reflects a 0-25% increase in capacity, phase 2 a 25%-50% increase, and phase 3 a 50%-100% increase, or a return to normal or near-normal institutional activity. Depending on which phase of reexpansion your institution is currently in, your cardiac surgical program will have a defined approach to which elective cases will be given priority during the ramp-up (Fig. 2). As far as the number of electives cases by which your program might ramp-up are concerned, this will depend upon the urgent case demands at your institution and your overall institutional capacity. It should be noted that the recently published International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) trial5 supports the role of optimal medical therapy as first-line therapy in appropriately selected patients with stable coronary artery disease, thus allowing for the deferral of surgical revascularization in this patient population. It should also be noted that urgent case demands might increase as the result of having reduced or eliminated elective cardiac care services during the COVID-19 pandemic at your institution, which, in turn, could potentially lead to patients presenting with more unstable symptoms or complications of missed or delayed treatment of myocardial infarction.
-
7.
Cardiac surgical programs must be prepared to immediately stop ramping-up or to even deescalate cardiac surgical volumes should there be a resurgence in the number of COVID-19 cases or COVID-19-related admissions and deaths.
Figure 1.
Visual abstract of the guiding principles for the ramping-up of cardiac surgery during the coronavirus disease 2019 (COVID-19) pandemic.
Figure 2.
Phased implementation approach to cardiac surgery ramp-up on the basis of increase in hospital capacity. AS, aortic stenosis; ASD, atrial septal defect; CABG, coronary artery bypass grafting; CHF, congestive heart failure; EF, ejection fraction; ICU, intensive care unit; LAD, left anterior descending artery; LM, left main; MR, mitral regurgitation; PFO, patent foramen ovale; TAVI, transcatheter aortic valve implantation; VAD, ventricular assist device. Modified and reproduced with permission from the Canadian Society of Cardiac Surgeons.
Summary
The COVID-19 pandemic has introduced challenges that cardiac surgical programs have never experienced. Elective cases have been scaled back, restricting programs to urgent and emergent cases so that resources might be mobilized to care for patients with COVID-19. Wait lists have grown, and those being asked to wait for surgery might be forced to experience excessively prolonged wait times. In an effort to mitigate this, patients who were once deemed surgical candidates have increasingly been referred for medical management or alternative percutaneous therapies. Despite this, there remains a significant number of patients in whom timely surgical intervention, even if during a global pandemic, outweighs the risk of further delay.
It is with this in mind that the CSCS has postulated the aforementioned guiding statements in an effort to support cardiac surgical programs across Canada and to provide them with a template on which to formulate their plans to ramp-up. As new data emerge, these guiding statements might change over time because of the fluidity and scope of the current pandemic. Geographic differences in epidemiology and practice patterns across Canada must be acknowledged, and we hope that these guiding statements will allow for the deliberate and graded increase in cardiac surgical care as the COVID-19 pandemic burden begins to ease.
Funding Sources
The authors report no funding sources.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 1143 for disclosure information.
References
- 1.Hassan A., Arora R.C., Adams C., et al. Cardiac surgery in Canada during the COVID-19 pandemic: a guidance statement from the Canadian Society of Cardiac Surgeons. Can J of Cardiol. 2020;36:952–955. doi: 10.1016/j.cjca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure [e-pub ahead of print]. Ann Intern Med 10.7326/M20-1495, accessed June 6, 2020. [DOI] [PMC free article] [PubMed]
- 3.Cheng MP, Papenburg J, Desjardinset M, et al. Diagnostic testing for severe acute respiratory syndrome-related coronavirus-2. Ann Intern Med. 2020;172:726-34. [DOI] [PMC free article] [PubMed]
- 4.Guo L, Ren L, Yang S, et al. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19) [e-pub ahead of print]. Clin Infect Dis 10.1093/cid/ciaa310, accessed June 6, 2020. [DOI] [PMC free article] [PubMed]
- 5.Maron D.J., Hochman J.S., Reynolds H.R., et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382:1395–1407. doi: 10.1056/NEJMoa1915922. [DOI] [PMC free article] [PubMed] [Google Scholar]