Abstract
Objective:
The objective of the study was to investigate the causative factors and complications attributable to obesity in children living in Jeddah, Saudi Arabia.
Methods:
This is a retrospective study encompassing a sample size of 151 children and adolescents between the ages of 4 and 20 years. Data were collected through reviewing medical records, medical files on the hospital electronic system, and clinical interviews conducted with legal guardians. The date of the study was from January to June 2018, and the study was carried out in Jeddah, Western Region, Saudi Arabia.
Results:
Data were entered, coded, cleaned, and analyzed using the Statistical Package for the Social Sciences (IBM SPSS), version 22. The analysis was done by assessing the significance of various risk factors and sequelae in their contribution to pediatric obesity by one-way ANOVA for nominal variables of more than two categories and independent-samples t-test for the nominal variables with two categories. The sample was 47% of the male gender, whereas females made for the remaining 53%. The causation of obesity was distributed among the following factors: an unhealthy diet, a sedentary lifestyle, medications such as glucocorticoids, and complications attributed to obesity including gastroesophageal reflux, hypertension, precocious puberty, sleep apnea, psychological disturbances, and fatty liver diseases.
Conclusion:
Environmental factors were found to be the most predominant cause, where the majority of children were found to be leading a sedentary lifestyle, following an unhealthy diet, and skipping meals. The most recurring complications involved psychosocial and behavioral abnormalities, and among the medical consequences, gastroesophageal reflux and obstructive sleep apnea were the most prevalent.
Keywords: Childhood, complications, factors, obesity, risk, Enfance, complications, facteurs, obésité, risque
Résumé
Objectif:
Étudier les facteurs de causalité et les complications imputables à l’obésité chez les enfants vivant à Djedda, en Arabie saoudite.
Matériels et Méthodes:
Il s’agit d’une étude rétrospective couvrant un échantillon de 151 enfants et adolescents âgés de 4 à 20 ans. Les données ont été collectées à travers l’examen des dossiers médicaux, des fichiers médicaux sur le système électronique de l’hôpital et des entretiens cliniques menés avec des tuteurs légaux. La date d’étude était de janvier à juin 2018 et a été réalisée à Djeddah, dans l’ouest de l’Arabie saoudite.
Résultats:
Les données ont été entrées, codées, nettoyées et analysées à l’aide d’un logiciel de statistiques sociales (IBM SPSS), version 22. L’analyse a été réalisée en évaluant l’importance de divers facteurs de risque et de leurs conséquences dans leur contribution à l’obésité pédiatrique par une ANOVA à un facteur pour les variables nominales de plus de deux catégories et Test t de l’échantillon indépendant pour les variables nominales à deux catégories. L’échantillon comprenait 47% du sexe masculin alors que les femmes représentaient les 53% restants. La cause de l’obésité a été répartie entre les facteurs suivants: une alimentation malsaine, un style de vie sédentaire, des médicaments tels que les glucocorticoïdes, et les complications attribuées à l’obésité comprennent le reflux gastro-oesophagien, l’hypertension, la puberté précoce, l’apnée du sommeil, des troubles psychologiques et des maladies de foie grasses.
Conclusions:
Les facteurs environnementaux ont été la principale cause, la majorité des enfants menant une vie sédentaire, suivant un régime alimentaire malsain et sautant des repas. Les complications les plus récurrentes concernaient des anomalies psychosociales et comportementales, et parmi les conséquences médicales, le reflux gastro-oesophagien et l’apnée obstructive du sommeil étaient les plus répandus.
INTRODUCTION
Childhood obesity is a global health concern on the rise as children who suffer from obesity are more likely to grow into obese adults, increasing not only their current but also their lifelong risk of metabolic dysfunction and cardiovascular morbidity. Furthermore, it has been proven that treating obesity after its establishment poses a more difficult challenge than efforts directed toward its prevention.[1]
The World Health Organization (WHO) defines being overweight and obese, respectively, as having a weight of more than 2 and 3 standard deviations (SDs) above the mean.[2] The worldwide prevalence of overweight and obesity in the pediatric population alone had increased in a 20-year duration from 4.2% to 6.7% in 2010.[2] In Saudi Arabia, the National Growth Study reported the prevalence of obesity in children between the ages of 5 and 18 years in nearly half the population at a percentage of 44.7%. Therefore, in order to limit and decrease the incidence of obesity, a more secured understanding of the risk factors contributing to its onset is required, and in order to effectively bring about a more serious awareness into the community of the burden it entails, a thorough account of associated complications must be reported into evidence.
Environmental factors play a prominent role in the development of obesity; with the improvement in Saudi Arabia’s economy over the past 3 decades following the discovery of oil, access to video-games, television, junk food and private cars for transportation has become more readily available for Saudi children, allowing them to lead a more sedentary lifestyle.[3] Other identified causes of obesity that are popular in childhood include syndromic disorders, such as Prader–Willi and Bardet–Biedl syndromes, and endocrinopathies, of which the most recurring are hypothyroidism, growth hormone deficiency, and cortisol excess.[2]
In consequence, medical morbidities priorly recognizable only in adults are now extremely prevalent in children; these include but are not limited to fatty liver disease, type 2 diabetes, obstructive sleep apnea (OSA), dyslipidemia, and menstrual abnormalities.[4] Childhood obesity is furthermore implicated in psychosocial ramifications, as children who are overweight/obese are more liable to bullying from their peers, discrimination, and social marginalization. This, in turn, leads to a negative body image, low self-esteem, and low self-confidence that all contribute to a poorer academic performance.[5]
The aim of this study was to investigate the causative factors and complications attributable to obesity in children living in Jeddah, Western Region, Saudi Arabia.
METHODS
This study is of a cross-sectional design and had included three outpatient endocrinology clinics across the city of Jeddah in Saudi Arabia. It was carried throughout the months of January–June 2018. Ethical approval from the ethical committee of scientific research in King Abdulaziz University was obtained prior to the commencement of this study and has detailed permission for reviewing electronically documented medical records, conducting clinical interviews, and performing physical examination. A sample size of 151 participants was selected through vetting children visiting pediatric endocrinology clinics across Jeddah, Saudi Arabia. The selection was based on primary exclusion of children below the age of 4 years and above the age of 20 years and those of a body mass index (BMI) below 25. Therefore, all children included were either overweight, obese, or morbidly obese.
Data variables included lifestyle factors such as eating habits, diet, and level of activity; medical history of metabolic dysfunction, endocrinopathies, syndromic disorders, psychosocial abnormalities, heartburn, and sleep apnea; medication history including glucocorticoids; family history of obesity; and anthropometric measures of height and weight with consequent calculation of BMI and relative SD. An unhealthy diet was defined as one that included an unsupervised availability of chips, sweets, soft drinks, and fried foods in the child diet, which were identified as major contributors to energy, fat, and high-calorie intake. The activity level was assessed through evaluating both duration and frequency of indulging activities that prompted cardiovascular effort; this included swimming, cycling, dancing, martial arts, and running sports such as football, baseball, and basketball. In line with the WHO guidelines for adequate physical activity in children, 60 min of moderate-to-vigorous intensity per day was considered sufficient to classify the child as physically active.
When evaluating Vitamin D status, values of serum 25-hydroxycholecalciferol below 25 nmol/l were interpreted as Vitamin D deficiency, whereas values between 50 and 25 nmol/l were considered indicative of a Vitamin D insufficiency. Growth hormone status was evaluated through growth hormone stimulation tests using both provocative agents, clonidine and glucagon. Serum values of growth hormone were then evaluated multiple times over the next 210 min; children with peak results of <10 ng/ml were confirmed to have a growth hormone deficiency. Hypothyroidism was diagnosed based on a thyroid profile; the combination of a thyroid-stimulating hormone (TSH) value at or beyond 5 mU/L along with a free T4 value <12 pmol/l was diagnostic of hypothyroidism. Children were also diagnosed with hypertension if either systolic or diastolic blood pressure measurements exceeded the 95th percentile for age and gender on multiple occasions.
OSA was confirmed through polysomnography, otherwise known as a sleep study, in children who reported one or more of the following symptoms: excessive daytime sleepiness, bedwetting, snoring, and heavy breathing. A polysomnography is a study in which brain wave activity, breathing patterns, oxygen levels, heart rate, and muscle activity are monitored during sleep. Similarly, children were also confirmed to suffer from gastroesophageal reflux disease (GERD) using a 24-h pH monitor if they were found to have one or more of the following symptoms: irritability during meals, refusal to eat, frequent coughing or belching, and chest pain.
Statistical analysis
Data were entered, coded, cleaned, and analyzed using the Statistical Package for the Social Sciences (IBM, Armonk, NY, USA), version 22. The analysis was done by assessing the significance of various risk factors and sequelae in their contribution to pediatric obesity by one-way ANOVA for nominal variables of more than two categories and independent-samples t-test for the nominal variables with two categories.
RESULTS
The sample size included 151 participants achieving a near approximate gender distribution with 53% of the sample being of the female gender and the remaining 47% of the male gender. An unhealthy diet and a sedentary lifestyle were among the most prevalent risk factors at relative percentages of 71.5% and 69% of the total sample size. Harmful dietary habits such as skipping meals and emotional eating were identified in 63% and 27.4% of all children, respectively, and were proven to significantly affect the mean BMI at P = 0.019 and 0.009, respectively. Children who followed a healthier diet were found to have significantly lower BMI means, P = 0.007, whereas those who indulged in frequent (>1/week) consumption of fast foods had a significantly higher BMI mean, P = 0.037. In addition, 76.8% of all children were identified to have engaged in sedentary activities for prolonged durations, such as watching television beyond 3 h each day. Pathological causes of obesity were also identified in the sample with varying percentages; Vitamin D deficiency in 63% of the children, hypothyroidism in 23%, growth hormone deficiency in 15%, syndromic causes in 8%, Cushing’s disease in 1%, and 7.3% of the children were on glucocorticoid treatment. In terms of consequences associated with obesity, psychosocial disturbance was found at a prevalence of 35.3% of all children, of which 23.3% manifested in the form of aggression, whereas 12% were in the form of social withdrawal. Medically, gastroesophageal reflux was diagnosed in 22% of all children, OSA in 14.6%, precocious puberty in 10.6%, hypertension in 6.6%, insulin-independent diabetes mellitus in 3.3%, and nonalcoholic fatty liver disease (NAFLD) in 2%. OSA was found to be significantly associated with increases in mean BMI at P = 0.05, 0.001, and 0.0001, respectively.
DISCUSSION
The concept of obesity stems from an excess in weight gain as a result of an imbalance between energy intake and expenditure. While, roughly, this is mainly modulated through diet and level of activity, individual predisposition to obesity can vary according to metabolism. This might be explained pathologically by a genetic element, a hormonal discrepancy, or by a physiological disparity in basal metabolic rate.
Lifestyle influence
Dietary factors have been studied extensively in their contribution to obesity across all age groups. Junk food and fast foods are high in caloric content despite being low in nutritional benefit, and self-indulgence in their consumption will yield a corresponding outcome of an obese and malnutritioned individual.[6] In addition, it has been observed that the predisposition to obesity is further extended by dietary behavior, as individuals who skipped meals and consumed more frequent snacks were at a higher risk of being overweight/obese.[7,8] This is supported by our results where 71.5% of the sample had been following an unhealthy diet that is low in vegetables and fruits and high in fats. A higher snack frequency of more than twice per day was observed in 33% of the sample, of which 72.2% preferred unhealthy crisps, sweets, and carbonated beverages. A total of 63% were skipping meals, and a significant relationship with increases in BMI mean was proven in those who often skip meals by P = 0.019. An additional harmful dietary habit that was found to be significantly associated with a higher BMI mean is emotional eating (excessive consumption of food in response to stressful periods such as anxiety and depression.), proven by P = 0.009.
In our sample, 76.8% were found to be spending more than 3 h each day watching television. A sedentary lifestyle has long been recognized to have a negative impact on weight; one study showed that the prevalence of obesity increased by 2% with each hour spent watching television per day (18 in 5). This is corroborated by another study that uncovered an inversely proportional relationship between the duration spent in physical activity and the time spent engaging in sedentary habits, such as watching television and playing video games.[9] Similarly, 68.9% of our sample led a sedentary lifestyle [Figure 1]. To elaborate, 34.4% of the children in our study were reported to rarely ever engage in physical activity prompting cardiovascular effort, and another 34.5% reported an occasional, between 1 and 2 times/week, engagement in such exercises. Therefore, lifestyle factors such as diet and level of activity are strongly believed to significantly impact the prevalence of obesity in children [Figure 2].
Figure 1.
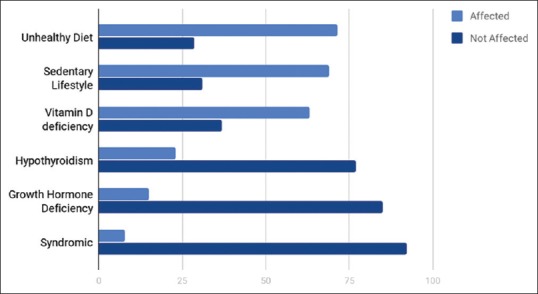
Percentage of causative factors among obese children
Figure 2.
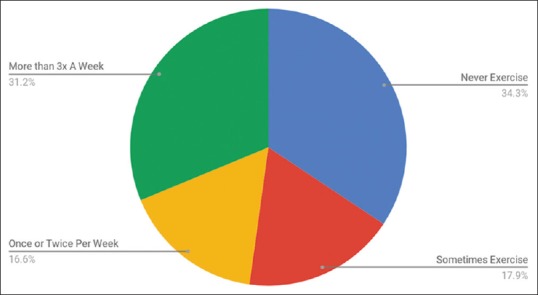
Rate of physical activity among obese children
Endocrinopathy
The mechanism by which hypothyroidism relates to obesity is still controversial; some studies claim that elevations in TSH are an adaptive response in an attempt to prevent further weight gain by increasing the metabolic rate. Some argue that it is a biological indicator of resistance and thereby may play a role in lipid and glucose metabolism, whereas others reinforce that most of the weight gain seen in hypothyroidism is in actuality a result of salt and water retention and is, therefore, not related to fat content.[2] Regardless, hypothyroidism was found to be a prevalent morbidity among obese children in our study, constituting a total of 23% of our sample. In addition, 15% of the total sample size were also diagnosed with growth hormone deficiency. Growth hormone induces lipolysis and promotes preferential oxidation of lipids and protein synthesis, and therefore, the relationship between its deficiency and the development of obesity is clearly understood. Although <1% of our sample suffered from Cushing syndrome, up to 7.3% were found to be taking glucocorticoids. Glucocorticoids raise the fatty acid content in circulation through hydrolysis of circulating triglycerides, increasing their availability for ectopic fat deposition on liver, muscle, and central adipocytes. They also promote preadipocyte conversion to mature adipocytes, causing hyperplasia of the adipose tissue, and express an acute antilipolytic effect on the mature adipocytes.
Vitamin D deficiency
It is postulated that activated Vitamin D (1,25-dihydroxycholecalciferol) may play a role in the mobilization of free fatty acids from adipose tissue as well as in the metabolism of adipocytes. However, the exact mechanism by which this occurs remains unclear.[10] A study in the United States demonstrated that an increase in BMI was associated with lower levels of Vitamin D.[11] This is similar to the findings of our study, in which 63% of our total sample were diagnosed with Vitamin D deficiency.
Precocious puberty
Adipose tissue is not only a depot to store excess energy in the form of fat but also an endocrine organ that secretes bioactive peptides known as adipokines which play an important role in the regulation of the reproductive axis. Adipose tissue reserves can influence the timing of the onset of puberty and the ability to maintain reproductive function. This explains why overweight and obese girls are shown to develop breasts about a year earlier than their normal-weight equivalents.[12] A study carried by the University of Bologna, Italy, showed a higher prevalence of 17% in precocious puberty within a population that was highly prevalent (74%) in overweight/ obesity when compared to the control group, of which only 1.9% expressed precocious puberty. In addition, isolated signs of accelerated pubertal development such as thelarche, pubic hair, and advanced bone age were present at a prevalence of 41%.[13] In this study, precocious puberty was found at a prevalence of 10.6% of all overweight/obese children.
Syndromic disorders
Syndromes are almost always considered in cases of childhood obesity, especially when morbid and resistant to diet and exercise. Obesity is a component of several syndromic disorders, some of which are Prader–Willi and Bardet–Biedl, both presenting with other congenital manifestations alongside obesity. The prevalence of syndromic disorders as a cause for obesity in this study was up to 8%, of which the most common was trisomy 21, found at a prevalence of 2.6% in our sample of overweight/obese children. Weight gain in this particular group is mostly attributed to the implications of this syndrome on a child’s capacity to carry out a normal lifestyle. Physical characteristics such as short stature and hypotonicity and health concerns such as congenital cardiac pathology all limit a child’s ability to live with an activity level similar to his or her peers.[14]
Medical consequences
One study outlined an 8.5-fold increase in clinically recognizable hypertension in adolescents who suffered from obesity in comparison to lean adolescents.[15] This is in keeping with our findings, as we present a significant direct relationship between an increase in the BMI mean and the development of hypertension (P = 0.001). Another cardiovascular risk factor found in association with obesity is insulin-independent diabetes mellitus, which has become increasingly observed in children, and was found at a prevalence of 3.3% in our study. OSA is characterized by a prolonged obstruction of the upper airway during sleep-disturbing sleeping patterns and may manifest with increased daytime sleepiness, hypertension, and neurobehavioral disturbances.[16] In addition, insufficient sleep may, in turn, lead to weight gain as proposed by one study, where it elaborated the association with pathologically elevated levels of ghrelin and decreased levels of leptin augmenting the appetite.[17] OSA was found to be among 14.6% of the population, with a significant relationship to obesity at P = 0.0001.
Another similar relationship was found between obesity and prevalence of GERD at P = 0.05, where it was prevalent by 22%. A fatty infiltration of the liver in the absence of alcohol intake constitutes NAFLD, which has become the most common cause of cirrhosis in children of the United States in parallel to the increase in frequency of obesity.[2] Thankfully, it was among the lowest prevalence in our study at 2% [Figure 3].
Figure 3.
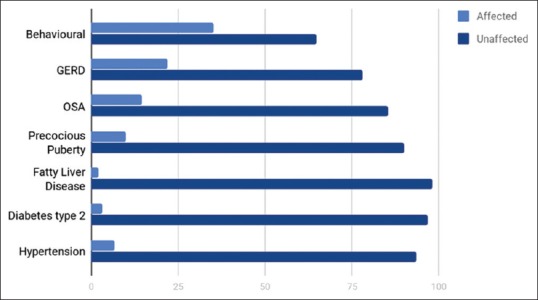
Percentage of each complication among obese children
Psychosocial impact
A review that was conducted to investigate the relationship between psychiatric health and obesity concluded that overweight/obese children are more likely to suffer from depression, anxiety, low self-esteem, social withdrawal, and behavioral abnormalities when compared to their healthy-weight peers.[18] This is strengthened by our findings of social withdrawal in 12% of the sample and another 23.3% exhibiting aggressive behavior.
CONCLUSION
Environmental factors were found to be the most predominant and most significant cause. The majority of children were found to be leading a sedentary lifestyle, following an unhealthy diet that is low in nutritional value yet high in caloric content, as well as exhibit harmful dietary habits such skipping meals and emotional eating, which were found as significant contributors to the development of obesity. The most prevalent consequence overall was psychosocial and behavioral abnormalities, and among medical complications, gastroesophageal reflux and OSA were the most common. However, precocious puberty, type 2 diabetes, and hypertension were also found in obese children at a considerable rate.
Recommendation
Efforts should be directed at preventing childhood obesity by targeting modifiable causative factors such as physical activity and dietary habits in addition to optimizing nonmodifiable factors such as endocrinopathies. This can be done by raising community health awareness of the serious complications resulting from childhood obesity.
Study limitations
The study included a small number of participants, only 151 children, and therefore, cannot be used to generalize conclusions but can be taken into consideration when reviewing multiple studies from different geographical areas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Al Dhaifallah A, Mwanri L, Aljoudi A. Childhood obesity in Saudi Arabia: Opportunities and challenges. [Last accessed on 2019 Nov 13];Saudi J Obest. 2015 13:1–7. Available from: http://www.saudijobesity.com . [Google Scholar]
- 2.Koyuncuoǧlu Güngör N. Overweight and obesity in children and adolescents. J Clin Res Pediatr Endocrinol. 2014;6:129–43. doi: 10.4274/jcrpe.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Hazzaa HM. Prevalence and trends in obesity among school boys in central Saudi Arabia between 1988 and 2005. Saudi Med J. 2007;28:1569–74. [PubMed] [Google Scholar]
- 4.Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: Causes and consequences. J Family Med Prim Care. 2015;4:187–92. doi: 10.4103/2249-4863.154628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics. About Childhood Obesity. [Last accessed on 2019 Nov 13]. Available from: http://www.aap.org/obesity/abouthtml .
- 6.Ebbeling CB, Sinclair KB, Pereira MA, Garcia-Lago E, Feldman HA, Ludwig DS, et al. Compensation for energy intake from fast food among overweight and lean adolescents. JAMA. 2004;291:2828–33. doi: 10.1001/jama.291.23.2828. [DOI] [PubMed] [Google Scholar]
- 7.Watanabe Y, Saito I, Henmi I, Yoshimura K, Maruyama K, Yamauchi K, et al. Skipping breakfast is correlated with obesity. J Rural Med. 2014;9:51–8. doi: 10.2185/jrm.2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murakami K, Livingstone MB. Eating frequency is positively associated with overweight and central obesity in US Adults. J Nutr. 2015;145:2715–24. doi: 10.3945/jn.115.219808. [DOI] [PubMed] [Google Scholar]
- 9.Story M, Neumark-Sztainer D, French S. Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc. 2002;102:S40–51. doi: 10.1016/s0002-8223(02)90421-9. [DOI] [PubMed] [Google Scholar]
- 10.A plasma protein which increases with Vitamin K deficiency. Nutr Rev. 1972;30:211–3. doi: 10.1111/j.1753-4887.1972.tb04046.x. [DOI] [PubMed] [Google Scholar]
- 11.Kotecha S. Management issues in CLD of prematurity. Arch Dis Child Fetal Neonatal Ed. 2002;87:F2. doi: 10.1136/fn.87.1.F2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sam AH, Dhillo WS. Endocrine links between fat and reproduction. Obstet Gynecol. 2010;12:231–6. [Google Scholar]
- 13.Poli F, Pizza F, Mignot E, Ferri R, Pagotto U, Taheri S, et al. High prevalence of precocious puberty and obesity in childhood narcolepsy with cataplexy. Sleep. 2013;36:175–81. doi: 10.5665/sleep.2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dettlaff-Weglikowska, Urszula Evamarie Hey-Hawkins and Hans Georg von Schnering Einfluß des Kations auf die Struktur des [Si(O2C6H4)2F]⊖-Anions: Struktur von [K(18-Krone-6)][Si(O2C6H4)2F] / The Influence of the Cation on the Structure of the Anion [Si(O2C6H4)2F]⊖: The Structure of [K(18-Krone-6)][Si(O2C6H4)2F]” Zeitschrift für Naturforschung B. 2014;46:609–14. doi:101515/znb-1991-0508. [Google Scholar]
- 15.Kaplowitz P. Delayed puberty in obese boys: Comparison with constitutional delayed puberty and response to testosterone therapy. J Pediatr. 1998;133:745–9. doi: 10.1016/s0022-3476(98)70144-1. [DOI] [PubMed] [Google Scholar]
- 16.Section on Pediatric Pulmonology, Subcommittee on Obstructive Sleep Apnea Syndrome. American Academy of Pediatrics. Clinical practice guideline: Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;109:704–12. doi: 10.1542/peds.109.4.704. [DOI] [PubMed] [Google Scholar]
- 17.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rankin J, Matthews L, Cobley S, Han A, Sanders R, Wiltshire HD, et al. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc Health Med Ther. 2016;7:125–46. doi: 10.2147/AHMT.S101631. [DOI] [PMC free article] [PubMed] [Google Scholar]


