Across 38 studies, interventions that changed people’s predictions about how a health choice or behavior would make them feel led to small, but consistent changes in behavioral outcomes
Keywords: Meta-analysis, Affective forecasting, Anticipated regret, Anticipated affect, Interventions
Abstract
Background
People often use affective forecasts, or predictions about how a decision will make them feel, to guide medical and health decision making. However, these forecasts are susceptible to biases and inaccuracies that can have consequential effects on decision making and health.
Purpose
A meta-analysis was performed to determine the effectiveness of intervening to address affective forecasting as a means of helping patients make better health-related choices.
Methods
We included between-subjects experimental and intervention studies that targeted variables related to affective forecasting (e.g., anticipated regret, anticipated affect) as a means of changing health behaviors or decisions. We determined the overall effect of these interventions on targeted affective constructs and behavioral outcomes, and whether conceptual and methodological factors moderated these effects.
Results
A total of 133 independent effect sizes were identified from 37 publications (N = 72,020). Overall, affective forecasting interventions changed anticipated regret, d = 0.24, 95% confidence interval (CI) (0.15, 0.32), p < .001, behavior, d = 0.29, 95% CI (0.13, 0.45), p < .001, and behavioral intentions, d = 0.19, 95% CI (0.11, 0.28), p < .001, all measured immediately postintervention. Interventions did not change anticipated positive and negative affect, and effects on intentions and regret did not extend to follow-up time points, ps > .05. Generally, effects were not moderated by conceptual model, intervention intensity, or behavioral context.
Conclusions
Affective forecasting interventions had a small consistent effect on behavioral outcomes regardless of intervention intensity and conceptual framework, suggesting such constructs are promising intervention targets across several health domains.
Introduction
When making decisions that are consequential for health, people often engage in affective forecasting, which is an attempt to predict and use information about how the decision will make them feel in the future. Patients often make medical screening and treatment decisions based on their predictions about how the decision will affect their future happiness and well-being, or how much they will regret their choice (1–3). Both risky and protective health behaviors, including exercise (4–6), weight-loss (7), smoking (8), condom use (9), alcohol use (10, 11), and others (12, 13) are likewise influenced by how people predict these behaviors and their consequences will make them feel. Decisions are often made to avoid feeling regret and other negative emotions, and promote enjoyment, happiness, well-being, and other positive emotions (12, 14).
Within the broad field of affective forecasting, several related constructs have been delineated and operationalized. Perhaps the greatest amount of work has examined anticipated regret, or one’s expectations that choosing one option over another will evoke aversive regret-based feelings and cognitions in the future (15, 16). Recent meta-analyses and systematic reviews suggest anticipated regret predicts engagement in health behaviors (12, 17, 18) beyond what is predicted by attitudes, social norms, self-efficacy, and related constructs (19).
Studies have also demonstrated that people’s predictions about the positive and negative emotions a behavior or decision will evoke, known as anticipated affect, are unique predictors of several health behaviors and decisions (e.g., 6, 9, 12, 20, 21, 22). The future-oriented focus of anticipated affect is a key feature that distinguishes it from other affective influences on behavior, including affective attitudes (i.e., affectively based evaluations of a behavior), and the affective states one is experiencing at the time of the decision (20). For example, a woman considering whether to have a mammogram to screen for breast cancer may have affective attitudes about mammograms (e.g., mammograms are scary). She may also feel worried or fearful that the procedure will be painful or detect cancer as she considers whether to have a mammogram. These affective attitudes and current affective states differ from her anticipated affect, or predictions about how she will feel if she decides to get screened. She may anticipate she will feel regret or guilt if she does not get screened, or that she will feel relieved and happy if she is screened and cancer-free. As another example of the distinction between these constructs, interventions that target current affect, such as fear appeals, aim to arouse fear about a decision’s negative consequences at the time of the decision (23, 24), whereas an intervention that targets anticipated affect, such as regret, aims to activate or increase how much regret one thinks will be evoked in the future as a consequence of having made an unhealthy choice (18). All these affective constructs (affective attitudes, current affect, and anticipated affect) influence behavior, but only anticipated affect falls within the purview of affective forecasting and is included in the current meta-analysis.
Although affective forecasts are often used to guide medically and health-relevant decision making (3, 14, 25), decades of research suggest people are often inaccurate in their affective predictions, which can have consequential results (e.g., 2, 4, 14, 22, 26, 27). For instance, patients with advanced illness are often asked to make decisions in advance about their preferences for aggressive or life-sustaining treatments at end-of-life. Because it is difficult to predict how one will feel in such extreme circumstances, forecasting errors abound, resulting in decisions, and end-of-life experiences that are misaligned with patients’ established plans (26, 28, 29).
Affective forecasting errors result from several biases. People generally overestimate the duration, intensity, and overall influence of their (usually negative) emotional reactions to events or decisions, a phenomenon known as impact bias (14, 30). People also engage in focalism, or a tendency to focus disproportionately on expected losses rather than on factors that will stay the same or improve. They also underestimate how quickly their own coping resources and adaptability will promote a return to baseline happiness, a bias known as immune neglect (31, 32). For instance, research shows that carriers for heritable diseases accurately predict a spike in negative affect after receiving genetic test results, but return to baseline happiness faster than predicted (1). Other factors that contribute to forecasting errors include a disproportionate focus on the differences between options rather than the similarities; inaccurate beliefs about the nature of the future event or behavior; poor memory of similar events in the past; and an inability to conceptualize or accurately predict how one will feel in a future emotional state that is not currently being experienced (i.e., the hot–cold empathy gap) (14, 33, 34–38).
Given the importance of affective forecasting in health decision making, researchers have called for greater efforts to address these biases as a means of helping patients make more informed medical choices (26), and improving health-related lifestyle behaviors (18). For many health behaviors, there is evidence of a predictable direction of the biases in affective forecasts. For instance, people generally anticipate exercise will make them feel worse than it actually does (39), and that unprotected sex will make them feel better than it actually does (40). When anticipated affect about a target health behavior tends to be biased in a predictable direction, interventions may aim to correct these biases by making the anticipated affect about a protective behavior more positive (e.g.,41), or the anticipated affect about a risky behavior more negative (e.g., 10). For instance, anticipated fear and disgust are widespread barriers to being screened for colorectal cancer with a colonoscopy. Reducing these negative anticipated emotions can make forecasts more in line with experienced emotions and increase screening rates (42).
Some experiments have successfully changed behavior or intentions simply by asking participants about their anticipated affect, usually centering on anticipated regret (18). For instance, across several studies, asking respondents one to three items about how much they would regret an unhealthy choice increased engagement in the healthier behavior alternative (43–53). These questionnaires may exert their effects by activating or increasing the salience of existing anticipated regret, increasing the level of anticipated regret, and/or strengthening the association between behavioral intentions and behavior (52, 54). Such interventions are particularly appealing because they require a relatively simple, low-touch, and noninvasive approach to changing behavior in real-world settings (e.g., 18).
Studies that have examined individual differences in affective forecasting suggest better emotional intelligence is associated with more accurate forecasting (26, 33, 34, 55). To the extent emotional intelligence is amenable to change through emotion education interventions (e.g., 56, 57), it suggests an additional mechanism through which affective forecasting can be improved. That is, emotional intelligence interventions should be expected to influence affective forecasting in similar ways to interventions specifically designed to target affective forecasting or anticipated regret.
It should be noted, however, that these approaches do not guarantee an increase in the accuracy of forecasts. Interventions may increase the positivity or negativity of anticipated affect beyond the affect that is (or would be) subsequently experienced by individuals. For example, interventions designed to increase anticipated regret or guilt about having unprotected sex (e.g., 9) may increase anticipated regret beyond the amount of regret that one would actually feel. Because little work has examined forecasting accuracy in the health domain, and for most health behaviors, biases occur in predictable directions, this meta-analysis examined the effectiveness of changing forecasts in the intended direction, regardless of whether these changes improved the accuracy of forecasts.
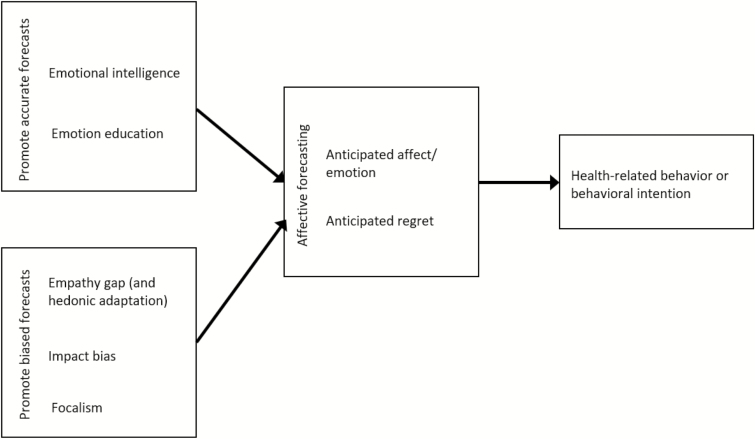
Despite evidence that affective forecasting constructs may be promising intervention targets, most public health and decision aid efforts have centered on changing other social-cognitive variables, such as attitudes, social norms, and self-efficacy, rather than affective forecasting. Moreover, several unique affective processes influence decision making (e.g., affective attitudes, anticipated affect, anticipated regret, current affect) and the distinctions between them can be inconsistent and blurred, in part because they are not regularly included in the Theory of Planned Behavior and other decision-making frameworks. Relatedly, there is diversity in the conceptual frameworks and constructs related to affective forecasting (e.g., anticipated regret, emotional intelligence/education, anticipated affect), and the consistency of intervention effects across these frameworks has not been examined. Thus, this meta-analysis sought to systematically examine the unique contributions of affective forecasting to health outcomes (see Fig. 1 for overview of included constructs).
Fig. 1.
Overview of constructs included in meta-analysis.
We examined extant intervention and experimental studies that have targeted variables related to affective forecasting as a means of changing health behaviors or decisions. Our two primary aims were to: (i) assess the strength of the evidence that affective forecasting variables can be experimentally changed or manipulated and (ii) quantify the extent to which affective forecasting interventions lead to subsequent changes in behavioral or decisional outcomes. We also sought to examine whether conceptual and methodological factors moderated the effects of affective forecasting interventions. Prior reviews have centered on anticipated regret, citing its uniqueness as a cognitive emotion, and suggesting effects may not generalize across other types of anticipated emotions (17, 18). Thus, we sought to assess the consistency of intervention effects across several conceptual frameworks, including, but not limited to, anticipated regret. Moreover, given the evidence of a mere measurement effect for anticipated regret (i.e., completing questionnaires about anticipated regret can change behavior), we also sought to assess whether intervention effects were consistent across interventions with varying intensity, and in different health domains. By establishing a quantitative summary of the existing experimental evidence surrounding affective forecasting, this meta-analysis can inform the development of future evidence-based decision-support and public health interventions (58).
Methods
We followed PRISMA consensus guidelines for conducting and reporting meta-analyses of studies that evaluate health-related interventions (59). Guidelines were adapted occasionally to accommodate experimental psychological research. The full study protocol was specified in advance and registered with PROSPERO, an international prospective register of systematic reviews with health-related outcomes (Registration # 42015027754).
Search Strategy
Published and in-press manuscripts, dissertations, and unpublished data were identified through: (a) searches of electronic databases (PsycINFO and PubMed); (b) email requests to members of relevant professional organizations using listservs; (c) searching reference lists of qualifying studies; and (d) emails to authors who have published in the field.
Studies met three primary inclusion criteria. First, the intervention had to engage or target an affective forecasting construct, such as anticipated regret or other anticipated emotions. Studies did not qualify if they included an affective forecasting measure as a dependent variable, but the intervention was conceptually unrelated to forecasting. For instance, interventions based on the theory of planned behavior (60), implementation intentions (61), or didactic knowledge provision (62) did not qualify if there was no conceptual discussion of how these interventions were intended to influence affective constructs. On the other hand, narrative interventions designed to change feelings about the behavioral outcome did qualify (e.g., 42), as did studies that included anticipated emotions as a component of a broader conceptual framework (e.g., 43, 63). Second, the study needed to employ a between-subjects experimental design; within-subjects designs (e.g., 64, 65) were excluded because they are not statistically comparable and cannot be meta-analyzed together with between-subjects studies. Lastly, studies needed to include a physical-health-related outcome variable. Studies that addressed mental illness, bullying, health-care workers’ job performance, or somatic symptoms were excluded because these domains were deemed qualitatively different in terms of the mechanisms of action and the traditional interventions that target them.
We used the following set of search terms to identify studies that met these criteria: [emotional intelligence; emotional education; affective forecast_; empathy gap; hedonic adaptation; anticipated emotion_; anticipat_ affect; impact bias; affective misforecast_; anticipated regret] AND [intervention_; induc_; manipulat_; experiment_; trial] AND [health_; medic_; patient preference_]. The first two sets of criteria needed to appear in the article title or abstract, whereas no restriction was placed on location of the third set of criteria. No language or date restrictions were specified, but all articles identified by the search were published in English. Searches were performed on the PsycINFO and PubMed databases in December 2015. The same search was performed again in December 2016 to detect recent publications not obtained in the original search. PubMed search results are available here: http://www.ncbi.nlm.nih.gov/sites/myncbi/1JkwpAIhd5_kD/collections/48877969/public/.
The original search of PsycINFO provided a total of 315 citations; PubMed provided 214 citations. After adjusting for 110 duplicates, 419 citations remained. Titles and abstracts were reviewed to determine whether they met the key inclusion criteria. The majority of excluded studies failed to meet the between-subjects experimental design criterion (e.g., they were observational studies, within-subjects designs, or review papers). Among studies with qualifying designs, 74 did not target an affective forecasting construct and/or did not have a health-related outcome.
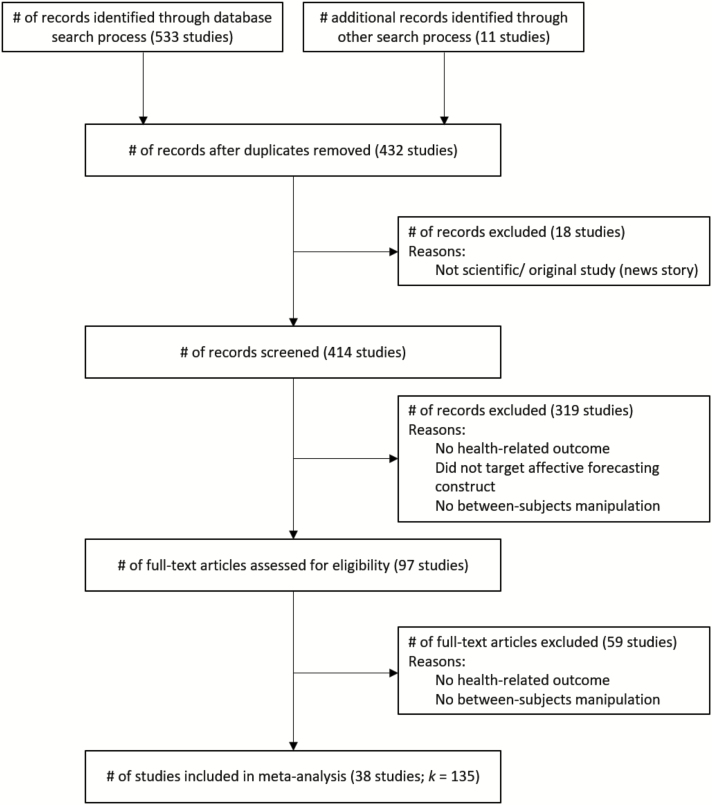
When the search was performed again in December 2016, two newly published studies were identified (53, 66). Eleven additional studies, including two unpublished, were identified through interpersonal communication via professional society listservs (Society for Personality and Social Psychology, Society for Judgement and Decision Making, Social Personality and Health Network, Society of Experimental Social Psychology, and Social and Affective Neuroscience Society), and direct emails with five top investigators in this field. Authors of published manuscripts and dissertations were contacted by email when studies did not include sufficient statistical information to calculate effect sizes; two authors could not be reached for the necessary statistical information (67, 68). This resulted in a final sample size of 38 studies for which 135 independent effect sizes could be extracted. Fig. 2 contains the PRISMA diagram of the manuscript search, retrieval, and coding process (59).
Fig. 2.
PRISMA diagram of study selection process.
Coding and Reliability
Method of data extraction
A coding form was developed and pilot tested on 10 randomly selected studies. No changes were made to it after pilot testing. The coding form can be obtained from the corresponding author. All articles were coded by two independent coders (EME and PS) and codes were compared to determine reliability (percent agreement = 90.29, κs > 0.33; mean κ = 0.62; median κ = 0.63). Consensus was reached with a third independent reviewer (RAF) when there was disagreement.
Coded variables
We coded the following publication statistics: (i) year of publication; (ii) publication status (dissertation, unpublished data, published); and (iii) country where study was conducted. The study population was also coded for age and gender. Because early pilot testing revealed that race/ethnicity and education were reported too inconsistently to be reliably coded, these variables were omitted from the final coding form.
Coded study characteristics were: (i) conceptual framework (based on affective forecasting, anticipated regret, anticipated affect, other phenomena); (ii) research setting (Internet, laboratory, clinic/medical); (iii) health context (cancer screening, blood/organ donation, drug and alcohol use, lifestyle behavior (e.g., exercise), medical decisions (e.g., vaccination); (iv) type of manipulation and control conditions (narrative, questionnaire, imagination, emotion education; “treatment as usual”); (v) experimenter and participant blinding (yes or no); and (vi) length of follow-up, if applicable.
Study Outcomes and Effect Sizes
Principle outcome measures were behavioral intentions and behavior. Secondary outcomes included anticipated regret about the consequences of not engaging in the target behavior, and negative and positive affect about engaging in the target behavior. For each of these outcomes, effect sizes (Cohen’s d) were calculated as the mean differences between the experimental and comparison condition divided by the pooled standard deviation (SD). If means and SDs were not available, t-tests or p-values from F-tests or regressions were used to calculate d (69, 70). To correct for sample size bias, effect sizes were weighted by the inverse of the variance of d (71).
For each effect size, a positive value indicates the experimental group had greater intentions or engagement in the target health behavior (e.g., exercise, condom use, blood donation), greater anticipated regret about not engaging in the target behavior, and higher levels of negative and positive affect about the behavior than the control group. This approach was taken because only two studies involved a decision for which the researchers did not aim to shift forecasts, decisions, and/or behavior in a specific direction a priori (72, 73). We included one of these studies in our analyses (two comparisons) because it examined interest in direct-to-consumer genetic testing and the default behavior would be to not get tested (73). Thus, we coded getting tested as the target behavior. The other study examined a decision between two breast cancer treatment options, and there was no default or objectively superior choice (72). Thus, there was no way to assign a directionality to this decision (i.e., no default choice or choice that would evoke greater health benefits), and therefore no way to assign directionality to its effect size. Because it was the only study to examine this type of decision, we could not statistically integrate it, and therefore, excluded it from our analyses. We revisit this decision and the broader challenge of these situations of clinical equipoise in the Discussion section.
Some studies included more than one conceptually relevant (i.e., targeted affective forecasting) experimental condition; in these cases, effect sizes were calculated by comparing each experimental condition to the control condition. To prevent interdependence of effect sizes, when the same control condition sample was used for multiple comparisons, we adjusted the sample size by dividing by the number of comparisons that used the control condition. Some studies did not explicitly articulate which condition served as the control. In these cases, the condition that most closely resembled usual treatment was used as the control condition. In sum, 133 independent effect sizes across studies, time point (immediately postintervention vs. extended), and outcome measures were extracted and included in analyses.
Analysis Strategy
All analyses were performed using Comprehensive Meta-analysis (74). We first quantified and examined homogeneity (i.e., similarity) of effect sizes across comparisons using the Q statistic, I2, and Τ2. Effects were not expected to be uniform, and indeed, heterogeneity in effect sizes was detected; therefore, all analyses used random-effects procedures.
We calculated separate main effects of the experimental inductions on the primary (behavior and behavioral intentions) and secondary outcomes (anticipated regret, positive, and negative affect about the target behavior) of interest at both immediately postintervention and extended follow-up time points. For all included studies, anticipated regret was only assessed and reported about not engaging in the target behavior (i.e., inaction regret, such as “If I did not use a condom, I would regret it.”).
We then used meta-regression techniques to examine whether study characteristics moderated the magnitude of the effect sizes of each outcome variable. The publication and population characteristics tested were: publication year; country (US, UK, other); sample gender (percent female); and mean age of the sample. We tested quality components of the study design, including: whether randomization methods were adequate and described, and whether participants and experimenters were blinded. Intervention characteristics tested were: conceptual framework (affective forecasting, anticipated regret, anticipated affect, emotion education); health context (cancer screening, blood/organ donation, lifestyle behavior, other); length of follow-up (in hours); setting (Internet, clinic, other); intervention type (questionnaire, narrative, imagination activity); and control type (no content/ treatment as usual).
We tested the effect of each of these variables on behavior, behavioral intentions, and anticipated regret at the immediate and extended time points separately. For positive and negative affect, due to small sample sizes and the fact that most studies had either an immediate or extended follow-up but not both, both time points were included in the same model. For studies that included both an immediate and extended outcome, the effect sizes were averaged in analyses rather than counted separately to avoid interdependence. Sensitivity analyses revealed no differences in effects when time points were examined separately.
Results
Overview of Included Studies
Study characteristics
Included studies are denoted with an asterisk in the reference section. Studies were published between 1996 and 2016 and were conducted in the United States (k = 15), United Kingdom (k= 13), or elsewhere (Canada, Australia, Greece, Netherlands, New Zealand; k = 10). Most studies were published in peer-reviewed journals (k = 32), and the rest were dissertations (k = 4) or unpublished (k = 2). Twelve studies (31.6%) were conducted online; nine (23.7%) were conducted in a laboratory or clinic; and 17 (44.7%) were conducted elsewhere, most often by postal mail.
Approximately half of the studies (k = 17) involved lifestyle behaviors, such as condom use (k = 5) and exercise (k = 6). Nineteen involved medical decision making, such as cancer screening (k = 6), blood or organ donation (k = 7), or vaccination (k = 2). Two studies involved other contexts (see Table 1).
Table 1.
Behavioral, conceptual, and population characteristics of studies included in meta-analysis
| % female | Sample size | Conceptual framework(s) | Target behavior | Intervention type | Affect change or saliencea | ||
|---|---|---|---|---|---|---|---|
| (43) | Abraham & Sheeran, 2003 | . | 229 | TPB plus anticipated regret | Exercise | 1-item anticipated regret questionnaire | salience |
| (44) | Abraham & Sheeran, 2004 | 50 | 70 | TPB plus anticipated regret | Exercise | 1-item anticipated regret questionnaire | salience |
| (122) | Abraham, et al., 2004 | . | 4,064 | TPB plus anticipated regret | Unsafe sex | School-based sex education program | change |
| (123) | Angott, et al., 2013 | 60.5 | 223 | Anticipated affect; immune neglect | Ostomy | Video about life with ostomy pouch | change |
| (124) | Barkoukis, et al., 2015 | 25 | 60 | TPB plus anticipated regret | Athlete doping | Self-affirmation intervention | change |
| (125) | Brown, et al., 2011 | 51.04 | 480 | Emotional intelligence; anticipated regret | Unsafe sex | School-based sex education program | change |
| (126) | Bui, 2009 | . | 338 | Anticipated affect; regret regulation | Eating behavior | Questionnaire about future feelings | salience |
| (66) | Chambers, et al., 2016 | 100 | 856 | TPB plus anticipated regret | Breast cancer screening | 2-item anticipated regret questionnaire | salience |
| (127) | Clowes & Masser, 2012 | 56.6 | 76 | Anticipated affect; TPB | Blood donation | Mimicked real blood donation environment | salience |
| (51) | Cox, et al., 2014 | 100 | 320 | Anticipated regret | HPV vaccination | 2-item anticipated regret questionnaire | salience |
| (128) | Dillard & Wertheimer, 2016 | 64.7 | 17 | Affective forecasting; impact bias | Colorectal cancer screening | Adaptation recall exercise | salience |
| (42) | Dillard, et al., 2010 | 53 | 1,533 | Affective forecasting | Colorectal cancer screening | Educational message plus a forecasting-based narrative | change |
| (56) | Ferrer, et al., 2011 | 52 | 132 | Emotional intelligence; anticipated affect | Unsafe sex | School-based sex education program | change |
| (129) | Ferrer, et al., 2012 | 67 | 61 | Anticipated and anticipatory affect | Colorectal cancer screening | Message aimed at increasing anticipated emotions | change |
| (130) | Fisher, et al., 2012 | 61.1 | 208 | Anticipated regret; Protection Motivation Theory | Genetic testing | Biased information about whole genome sequencing | change |
| (131) | France, et al., 2013 | 62 | 673 | Anticipated regret; coping | Blood donation | Video about donor concerns and coping strategies | change |
| (45) | Godin, et al., 2014 | 50 | 2,000 | TPB plus anticipated regret | Blood donation | 3-item anticipated regret questionnaire | salience |
| (46) | Godin, et al., 2010 | 53 | 4,391 | TPB plus anticipated regret | Blood donation | 3-item anticipated regret questionnaire | salience |
| (39) | Helfer, et al., 2014 | 63.57 | 140 | Anticipated affect | Exercise | Questionnaire about future feelings | salience |
| (67) | Leaf, 2008 | 66 | 150 | Anticipated affect | Sun protection | Questionnaire about future feelings | salience |
| (132) | Martinez, 2014 | 100 | 245 | Anticipated regret | Folic acid consumption | Anticipated regret message about folic acid consumption | salience |
| (133) | Moser, 2011 | 100 | 352 | Anticipated affect | Sun protection | Images depicting photoaging and skin cancer (to evoke anticipated fear and disgust) | change |
| (134) | Muller, et al., 2014 | 80 | 176 | Anticipated affect; coping | Prenatal screening | Video message about prenatal testing | change |
| (10) | Murgraff, et al., 1999 | 60.6 | 99 | Anticipated affect | Alcohol consumption | Questionnaire about future feelings | salience |
| (47) | O’Carroll, et al., 2015 | 51 | 38,938 | TPB plus anticipated regret | Colorectal cancer screening | 2-item anticipated regret questionnaire | salience |
| (48) | O’Carroll, et al., 2011 | 63.29 | 286 | TPB plus anticipated regret | Colorectal cancer screening | 2-item anticipated regret questionnaire | salience |
| (49) | O’Carroll, et al., 2011 | 50.8 | 193 | TPB plus anticipated regret | Organ donation | 2-item anticipated regret questionnaire | salience |
| (53) | O’Carroll, et al., 2016 | 56.65 | 9,139 | TPB plus anticipated regret | Organ donation | 2-item anticipated regret questionnaire | salience |
| (135) | Ogden, et al., 2009 | 65.2 | 418 | Anticipated regret | Medical choices | Vignettes with anticipated regret about a medical choice | salience |
| (136) | O’Hara, 2011 | 60.7 | 117 | Anticipated affect; Prototype Willingness model | Alcohol consumption; flu vaccinations | Questionnaire about future feelings | salience |
| (57) | Peter & Brinberg, 2012 | 35.71 | 28 | Emotional intelligence; anticipated affect | Eating behavior | Emotional intelligence curriculum | change |
| (137) | Reid, et al., 2013 | 58.72 | 109 | Emotional intelligence; anticipated affect | Eating behavior | Emotional intelligence curriculum targeting anticipated emotions | change |
| (9) | Richard, et al., 1996 | 69.94 | 343 | Anticipated affect | Unsafe sex | Questionnaire about future feelings | salience |
| (4) | Ruby, et al., 2011 | 78 | 207 | Anticipated affect; forecasting myopia | Exercise | Questionnaire about future feelings | salience |
| (50) | Sandberg & Conner, 2009 | 100 | 4,277 | TPB plus anticipated regret | Cervical cancer screening | 2-item anticipated regret questionnaire | salience |
| (52) | Sandberg & Conner, 2011 | 61.98 | 576 | TPB plus anticipated regret | Exercise | 3-item anticipated regret questionnaire | salience |
| (138) | Smerecnik & Ruiter, 2010 | 65 | 60 | Anticipated regret; perceived threat and coping | Unsafe sex | Threat and coping messages about HIV prevention | change |
| (73) | Sweeny & Legg, 2011 | 80 | 61 | Anticipated regret | Genetic testing | Messages with positive, negative, or both forms of genetic testing information | change |
TPB Theory of planned behavior.
aAffect change or salience reflects an intervention’s effort to either increase the salience of existing anticipated affect at time of decision (e.g., anticipated regret questionnaires), or change anticipated affect in terms of valence or intensity (e.g., through narratives).
Sample and comparison characteristics
The average sample size per comparison was N = 1,412 (range: 17–38,938); the median sample size was N = 132. There were 72,020 total individual participants across all studies. Mean age across comparisons was 29.25 years (SD = 6.05 years) and samples were 64.5% female. The proportion of independent effect sizes across each outcome were as follows: behavioral intentions (36.8%), behavior (17.9%), anticipated regret (21.4%), negative affect about the target behavior (10.3%), and positive affect about the target behavior (6.8%). Approximately one-quarter (22.2%) of outcomes were assessed at a follow-up time point averaging 4 months after the experimental manipulation (range: 7 days to 15 months). The remaining outcomes were assessed immediately following the intervention or manipulation.
Analyses of Homogeneity
The effect sizes for the affective forecasting interventions were heterogeneous for all immediately assessed outcomes except anticipated regret, Q (20) = 9.85, p = .956, Τ2 < .001, I2 < 0.001 (see Table 2). For the extended time points, effects were more homogenous for behavioral intentions, Q (5) = 2.861, p = .581, Τ2 < .001, I2 < 0.001, and anticipated regret, Q (7) = 3.074, p = .800, Τ2 < .001, I2 < 0.001. Effects on behavioral outcomes at extended time points were heterogeneous, Q (10) = 35.769, p < .001, Τ2 = .064, I2 = 74.838. Given this heterogeneity in effects and in accordance with our analysis plan, we examined several sample and study characteristics that may have moderated the interventions’ effects.
Table 2.
Measures of heterogeneity in effects across comparisons
| Outcome | K | Q | p (Q) | I 2 | Τ 2 |
|---|---|---|---|---|---|
| Time 1 | |||||
| Behavior | 18 | 247.53 | <.001 | 93.13 | .096 |
| Behavioral intentions | 42 | 135.99 | <.001 | 69.85 | .037 |
| Anticipated regret | 20 | 8.67 | .979 | 0.000 | .000 |
| Negative affect about target behavior | 12 | 25.61 | .007 | 57.04 | .036 |
| Positive affect about target behavior | 8 | 75.54 | <.001 | 90.73 | .471 |
| Time 2 | |||||
| Behavior | 10 | 35.77 | <.001 | 74.84 | .064 |
| Behavioral intentions | 5 | 2.86 | .581 | 0.000 | .000 |
| Anticipated regret | 7 | 3.07 | .800 | 0.000 | .000 |
Q and p (Q) test whether the heterogeneity between studies is significant, which would suggest they do not share a common effect size (a nonsignificant p value may reflect a lack of statistical power). I2 a proportion that represents the ratio of true heterogeneity to total variance across the effect size estimates; Τ2 is a test of homogeneity between studies that removes the dependence on the number of studies and is in the same metric as the effect size (similar to a standard deviation).
Main Effects
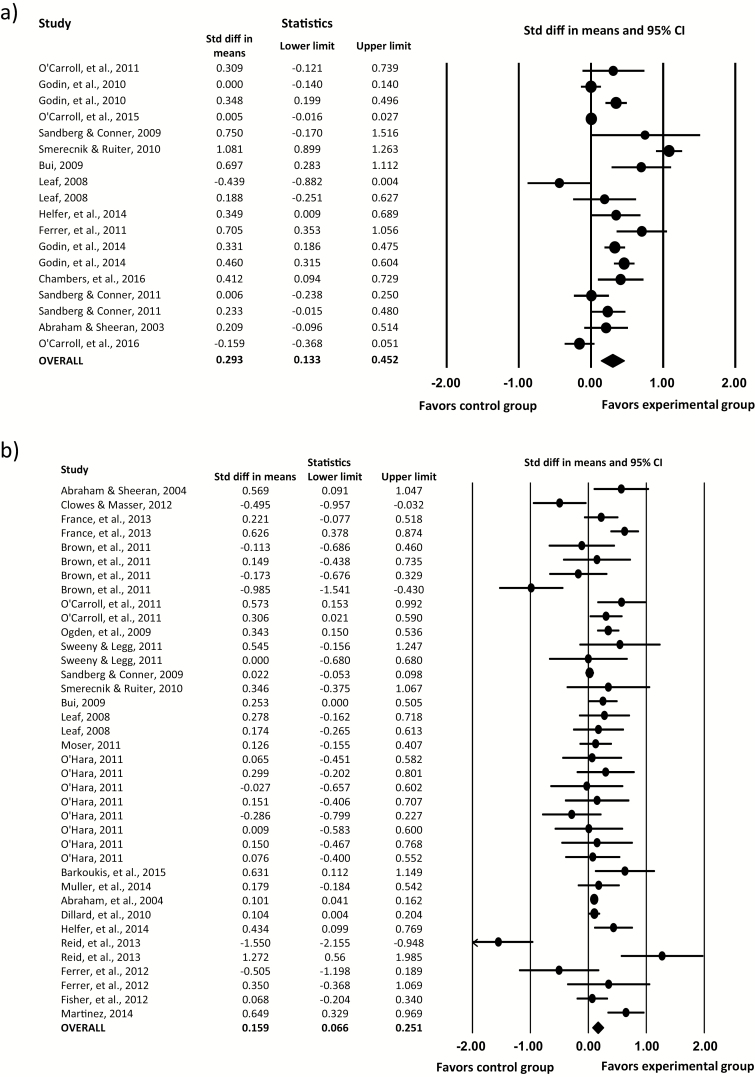
The overall effect sizes for the affective forecasting interventions on each outcome variable are reported in Table 3. The overall effects on both behavior and behavioral intentions immediately postintervention were significant: behavior: d = 0.29, 95% confidence interval (CI) (0.13, 0.45), p < .001; behavioral intentions: d = 0.19, 95% CI (0.11, 0.28), p < .001 (see forest plots in Fig. 3). The effect on anticipated regret was also significant, d = 0.24, 95% CI (0.15, 0.32), p < .001, but the effects on positive and negative affect about the health behavior were not, ps > .05. These represent small effect sizes in accordance with Cohen’s (1988) interpretation (75).
Table 3.
Effects of interventions on key outcomes of interest (from random-effects models)
| Outcome | k | d | 95% CI | P |
|---|---|---|---|---|
| Time 1 | ||||
| Behavior | 18 | 0.293 | 0.13, 0.45 | <.001 |
| Behavioral intentions | 42 | 0.178 | 0.091, 0.264 | <.001 |
| Anticipated regret | 20 | 0.235 | 0.150, 0.321 | <.001 |
| Negative affect about target behavior | 12 | 0.036 | −0.114, 0.187 | .639 |
| Positive affect about target behavior | 8 | 0.28 | −0.238, 0.790 | .292 |
| Time 2 | ||||
| Behavior | 10 | 0.323 | 0.114, 0.533 | .002 |
| Behavioral intentions | 5 | −0.319 | −0.538, −0.101 | .004 |
| Anticipated regret | 7 | −0.098 | −0.302, 0.106 | .348 |
CI confidence interval; k number of comparisons; d overall effect of intervention on dependent variable.
Fig. 3.
Forest plots illustrating intervention effects on (a) behavior and (b) behavioral intentions at immediate follow-up. CI confidence interval.
At extended or follow-up time points, effects were more mixed. There was a significant small effect of interventions on behavior in the intended direction, d = 0.19, 95% CI (0.11, 0.28), p < .001. The magnitude of this effect did not differ across time points based on meta-regression results, suggesting a consistent effect of interventions on behavior, b = −.034, p = .82, 95% CI (−0.32, 0.26). However, the effect on behavioral intentions and anticipated regret were different between immediate and extended time points, intentions: b = −.52, p < .001, 95% CI (−0.81, −0.23); anticipated regret: b = −.33, p = .003, 95% CI (−0.55, −0.11). The effect on intentions at extended time points (based on five observations across two studies) was significant in the reverse direction, d = −0.32, 95% CI (−0.54, −0.10), p = .004, suggesting a rebound effect. The effect on anticipated regret at extended time points was nonsignificant, d = −0.098, 95% CI (−0.30, 0.11), p = .35.
Moderator Analyses
Moderator analyses were conducted to examine causes for the observed heterogeneity in effect sizes across studies. A series of univariate meta-regressions tested whether study and population characteristics moderated effect sizes for each outcome variable. A summary of these results is reported in Table 4.
Table 4.
Study characteristics as predictors (moderators) of intervention effects
| Behavioral intentions | Behavior | Anticipated regret | Anticipated negative affect | Anticipated positive affect | ||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | |||
| % Female gender | −.0019 | .0002 | .0086* | .0009 | −.0005 | .0019 | 0.0029 | −0.0132 |
| Age | .0002 | .1317 | .0001 | −.0006 | −.0043 | .0063 | 0.0077 | −0.0013 |
| Internet-based | .1084 | — | −.144 | — | .0892 | — | −0.0204 | — |
| Conceptual framework | ||||||||
| Anticipated regret | .0339 | — | −.3199 | −.0118 | — | .2311 | 0.6210* | −0.5294 |
| Anticipated affect/emotion | −.0399 | — | .0307 | −.130 | −.0278 | — | −0.558*** | 0.5152 |
| Emotion education | .277 | — | .4635 | .348 | .0842 | — | 0.0591 | — |
| Behavioral context | ||||||||
| Health behaviors (e.g., exercise) | −.0989 | — | −.1764 | −.1866 | −.1347 | .2311 | 0.2862 | 0.0936 |
| Cancer screening | −.127 | — | .242 | −.0255 | −.2019 | .2311 | — | −0.0936 |
| Blood/organ donation | .0458 | — | −.0945 | — | .0842 | — | −0.1464 | — |
| Intervention | ||||||||
| Questionnaire as intervention | −.0905 | −.3149 | −.0908 | .0833 | .0586 | −.299 | −0.1319 | 0.468 |
| “No content” control | −.0881 | — | .0953 | .1952 | −.2019 | .2311 | −0.2967 | 0.2802 |
| Length of follow-up (# hours) | n/a | −.009 | n/a | .000 | n/a | .000 | n/a | n/a |
Beta coefficients from univariate meta-regression models. Anticipated negative and positive affect are in relation to the targeted health behavior. “No content” controls refer to control groups for which there was no or minimal contact. Questionnaire as intervention studies were comprised entirely of anticipated regret items.
*p < .05; ***p < .001.
Across these univariate analyses, sample gender and conceptual framework were the only variables that moderated effect sizes (see Table 4). Greater proportion of female participants was associated with greater intervention effects on behavior at Time 1, b = .0086, 95% CI (0.0001, 0.017), p = .049. Intervention effects on anticipated negative affect associated with engaging in a target behavior were also weaker for interventions with an anticipated regret conceptual framework, b = .62, 95% CI (0.068, 1.17), p = .028, and stronger for interventions with an anticipated affect framework, b = −.56, 95% CI (−0.84, −0.28), p < .001.
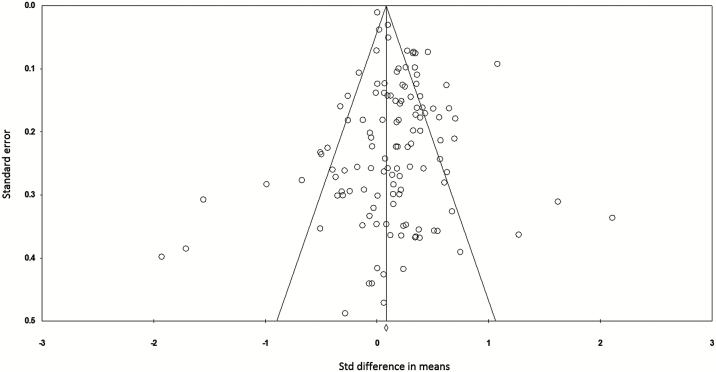
Publication Bias
We examined evidence for publication bias among the full sample of studies by calculating Rosenthal’s fail-safe N (76). The fail-safe N was 3,784, suggesting that even if many additional studies with null results were included, the overall effect size would remain significant. Given the limitations of the fail-safe N for estimating bias (77), we also generated a funnel plot of the standard error by the standard mean difference (see Fig. 4). The distribution is largely symmetrical, suggesting little publication bias. However, Egger’s regression suggests asymmetry and potential bias in results, intercept = 0.99, p < .001, 95% CI (0.44, 1.52). This asymmetry could be due to several sources of bias in addition to publication bias, including methodological variability and heterogeneity in effects, especially in the smaller studies (78). Trim-and-fill calculations (79) suggest that removing the 29 effect sizes contributing to the asymmetry does not render the effect size nonsignificant, d = 0.30, 95% CI (0.24, 0.36).
Fig. 4.
Funnel plot of standard error by standardized difference in means using full sample to assess publication bias.
Discussion
Across included studies, affective forecasting interventions increased engagement in the target health behavior both immediately after the intervention, as well as at subsequent assessments. Effects on immediately assessed behavior were stronger for samples that included a greater proportion of females. This finding suggests females’ behavior may be more amenable to change, and/or existing interventions may be designed in ways that make them particularly effective for females (e.g., by targeting decision-making inputs that resonate more for females, or using behavior change techniques that are more effective for females). Interventions also had their intended effects on behavioral intentions immediately after the intervention. However, a rebound effect on intentions was observed at follow-up time points. This finding may suggest any immediately activated changes in decisional predictors or behavior may have adverse effects longer term. For example, a sexual health intervention may increase participants’ experience with condoms immediately following the intervention, and with this experience, positive beliefs about condoms may erode (80). However, given the small number of observations that informed this finding (originating from only two studies), these results should be interpreted with caution. More work is needed to reliably determine long-term effects of forecasting interventions on behavioral intentions.
The included interventions also increased feelings of anticipated regret about failure to engage in the target behavior, but only when it was assessed immediately after the intervention; interventions had no effect on anticipated regret at subsequent time points. This was the case regardless of the intensity of the intervention, suggesting that even low-touch interventions (e.g., questionnaires) produce short-term increases in anticipated regret, but these effects are not durable over time. These findings may reflect evidence that affective experiences are generally more variable and fluctuating than other social-cognitive constructs, such as knowledge or risk perceptions (81). Thus, levels of anticipated regret may return to baseline more quickly, particularly if the interventions increased anticipated regret beyond naturally experienced levels. However, even temporary elevations in anticipated regret may nonetheless facilitate sustained behavior change even after the emotional experience has ceased (82).
Intervention effects on anticipated positive and negative emotions were not significant, suggesting health interventions designed to make people anticipate more positive or negative reactions to engaging in a health behavior are not effective in facilitating those reactions (although they may still be effective in changing behavior through different decisional mechanisms). Prospective and cross-sectional studies suggest anticipated emotions about behavior engagement or behavior consequences are unique predictors of several health behaviors and decisions (e.g., (6, 9, 12, 20, 21, 22)). Moreover, several prominent theories highlight affect and emotion as crucial for accurate and efficient information processing (83), perception and judgment (84–86), and risk-related decision making (87, 88). Empirical work suggests people develop emotional associations with health behaviors even prior to engaging in them (e.g., 80), and that these affective associations are a proximal determinant of behavior (89–92), often outweighing the effects of cognitive constructs (93–96). Thus, more work is needed to identify effective methods of intervening on anticipated emotions in health domains, and for testing the behavioral, contextual, or population characteristics for which these interventions are effective. For instance, there are age differences in affective forecasting errors, with older individuals displaying fewer errors, that may influence the effectiveness of related interventions (97).
Although there was statistical heterogeneity in effect sizes across studies, a series of meta-regressions suggest aspects of study quality, the conceptual framework, behavioral context, and intensity of the intervention generally did not explain these differences. The conceptual framework was only consequential for anticipated negative affect about the target behavior, for which “anticipated affect” interventions produced larger declines than “anticipated regret” interventions. Although this effect should be interpreted with caution given the other nonsignificant effects of conceptual framework, it does suggest that an intervention’s effects may depend on the framework informing it. Anticipated affect and anticipated regret are not interchangeable frameworks in terms of their effects on the corresponding affective outcomes. This finding is consistent with prior work showing anticipated regret is different from other anticipated negative emotions, perhaps because of its more cognitively based or decision-specific nature (98–100). Thus, these findings make sense, in that an intervention designed to influence anticipated regret about not engaging in a target behavior should not necessarily be expected to reduce negative affect about engaging in that behavior.
This meta-analysis included a broad range of conceptual frameworks, intervention methodology, and behavioral contexts, and there may be complex and interrelated nuances between these constructs that could not be statistically discerned with our meta-regressions and coded variables. On the other hand, the consistency of intervention effects on behavior, intentions, and anticipated regret across these different factors suggests affective forecasting is a robust decision-making predictor and may be a viable intervention target across a broad scope of contexts and approaches.
The results of this meta-analysis and nature of the included studies suggest the full potential of affective forecasting interventions is yet to be realized within the health context. Both low-touch interventions in which participants simply answered survey items, as well as more intensive emotion education interventions, produced significant effects on behavioral outcomes. Interventions were also consistent across behavioral domains that included both lifestyle behaviors (e.g., exercise, sun protection, safe sex), as well as medical decision making (e.g., vaccination, colonoscopy screening). These findings suggest interventions could be tailored to meet context-specific constraints and needs.
Moreover, the included studies represented only a fraction of the possible approaches to improve the accuracy of affective forecasting. No studies used approaches such as cognitive behavioral therapy to target coping abilities and emotion regulation or management, and few used emotion education or other techniques to improve emotional intelligence. However, research suggests individual differences in these factors are associated with affective forecasting abilities (101) and intervening on these individual differences has been recommended in several domains (26, 102, 103). A small body of experimental work suggests this may be an effective means of producing the desired changes in affective forecasting (104, 105), anticipated, and anticipatory emotion (e.g., 106). Thus, future intervention work ought to explore the potential of these approaches in health contexts. For instance, asking patients what helped them overcome difficult times in the past may help reduce the immune neglect that often follows an illness diagnosis (107). Improving their emotion regulation skills may likewise enable them to understand and cope more effectively with negative emotions, thereby improving the accuracy of their affective forecasts as well (34).
Although the results of this meta-analysis lend broad support for targeting variables related to affective forecasting as a means of targeting health behaviors, several questions remain for future work. First, our sample size was not large enough to reliably examine the mechanisms underlying the interventions’ effects on behavioral outcomes. For instance, anticipated regret may act as a mediator between the intervention and behavioral outcomes, or it may act as a moderator, strengthening the association between intentions and behavior (108). Future work ought to examine these more sophisticated pathways, given that the small sample size and lack of baseline data prohibited testing them in the current study.
Prior work suggests individuals can anticipate regret about both acting and not acting (inaction regret; also see (109, 110) for related differences between commission and omission biases). Regret over action is often, but not always, hypothesized to have more powerful effects on behavior (17, 99, 110–112). Although researchers have emphasized the need to examine both, only one study in the current meta-analysis assessed anticipated regret about performing the target behavior (i.e. action regret), but the results of these analyses were not reported (50). Thus, future work should separately examine both types of anticipated regret to determine whether the current results generalize across both action and inaction anticipated regret.
Although this meta-analysis provides preliminary support for the potential of affective forecasting as a health intervention target, several conceptual and empirical questions remain for future work. Scientifically rigorous research necessitates a level of artificial control and assessment of these affective factors as more discrete and unidimensional than they are in the real world, where potentially mixed or ambivalent forecasts about the health behavior and many other aspects of individuals’ lives are weighed together to inform decisions. For instance, individuals’ forecasts surrounding condom use may include anticipated feelings of romantic closeness, sexual pleasure, worry over their partner losing trust in them, and fear of pregnancy or disease. Moreover, both anticipated emotions and the decisions they inform may be interpersonal, evolving, or iterative in nature, rather than representing a single discrete moment. Thus, interventions and the research informing them will be most effective when they target anticipated feelings, values, and preferences in a way that reflects the complexities of affective forecasting in the real world.
With one exception, the studies included in this meta-analysis intervened to increase engagement in or positive affect about a target behavior, such as condom use or exercise, for which there is general agreement on the behavioral choice that produces better health outcomes. A dearth of work has examined whether affective forecasting can be intervened upon to improve decision making and health outcomes in instances of clinical equipoise where several treatment options are available and none is objectively or universally superior (for an exception, see (72)). For example, there is no consensus regarding the optimal management of localized low-risk prostate cancer, and patients are encouraged to weigh the risks and benefits of active surveillance and more invasive therapies in light of their personal values and goals (113). In these and other cases of clinical equipoise, accurate affective forecasting may help patients choose the most suitable treatment or feel more confident in their decision, but predictions about how colostomy bags (114), kidney transplants (115), and other treatments will affect quality of life are often biased (26, 35, 36, 116). Intervening to reduce bias in patients’ affective forecasts may facilitate decision making by helping patients make choices based on a broader scope of factors (i.e., with less focalism) or feel more satisfied and confident in their decision (72). An insufficient number of these studies has been conducted to integrate them meta-analytically, and much more work is needed to examine affective forecasting in the clinical equipoise context.
There may also be some health contexts for which affective forecasting is particularly challenging. For instance, patients’ forecasts about their end-of-life care preferences tend to fluctuate with emotional state (117), and change drastically (often without conscious awareness (118)) as their health deteriorates and distress intensifies (28, 116, 118, 119). Perhaps because these forecasts are prone to inaccuracy, patients often prefer their end-of-life care be guided by current preferences instead (119). Cancer screening presents another area where accurate forecasting may be particularly challenging. The proportion of individuals who experience direct benefit from screening (i.e., people for whom screening detects treatable cancer) is relatively low, uncertainty about one’s perceived risk is common, and cancer prevention recommendations are often perceived as ambiguous, all of which may motivate avoidance (120). These perceptions may hinder the formation and use of accurate affective forecasts about the consequences of one’s screening decision. Greater research is needed to elucidate whether more accurate forecasts can improve decision making in the contexts of clinical equipoise, end-of-life care, and cancer screening, and if so, the most ethical approach to increasing the accuracy of such forecasts.
Relatedly, changing affective forecasts to increase engagement in health behaviors does not directly indicate that these forecasts increased in accuracy. Indeed, it seems likely that the anticipated regret interventions included in this meta-analysis may have increased the magnitude or salience of regret in the decision-making process beyond what one would experience without intervention. For protective (e.g., exercising) and risk behaviors (e.g., smoking) for which an objectively better outcome is well-established, augmenting positive and negative anticipated affect may be a reasonable and ethically justifiable approach regardless of whether these efforts increase accuracy. There may even be instances when inaccurate positive forecasts are beneficial (121). However, forecast accuracy becomes a particularly important consideration in situations of clinical equipoise (58, 103). Affective forecasting interventions in these contexts would require a longitudinal evaluation and more individualized approach than those used in the current set of studies.
Some limitations should be considered when interpreting the current findings. Although we aimed to be inclusive with respect to conceptual frameworks and intervention modalities, atheoretical work and interventions in applied settings may have targeted forecasting constructs without referring to them as such. Although our efforts to reach out to scientists via professional society listservs and email may have attenuated this concern to an extent, it remains a limitation of this and most meta-analyses. Also, despite our relatively broad inclusion criteria, the sample size for some outcomes remained small, particularly for studies that assessed extended time points. This may have compromised our power to detect whether intervention characteristics, conceptual framework, study quality, or population characteristics influenced the effectiveness of the interventions. Thus, some of the null findings from the meta-regression analyses should be interpreted with caution. Relatedly, although the broad inclusion criteria increased the sample size and allowed us to test the consistency of effects across conceptual frameworks, it may have also diluted the observed effects by introducing greater variability across studies. Of particular importance, future work should separately examine intervention effects across different types of anticipated regret; use more precise measures of anticipated affect; include conditions of clinical equipoise; and test whether more complex mediational or moderation pathways can elucidate the mechanisms underlying the interventions’ effects on behavioral outcomes. Lastly, the samples were somewhat skewed toward younger, healthier, and Western culture populations, which may limit the generalizability of the findings.
In conclusion, our findings suggest interventions targeting affective forecasting variables had a small, but significant effect on their target health behavior outcomes. These effects remained consistent across conceptual models and intervention intensity, suggesting affective forecasting constructs hold promise as intervention targets across a variety of health domains, populations, and intervention modalities. Despite this evidence of their potential, it remains unclear how best to target anticipated positive and negative affect, and how to address the accuracy of forecasts specifically. As future research addresses these unanswered questions, the potential of affective forecasting interventions, particularly in conditions of clinical equipoise, may be fully realized.
Compliance With Ethical Standards
COI and Ethical Adherence: The research reported was conducted in accordance with the ethical guidelines of the American Psychological Association, has not been published previously, and is not currently under review at any other journal. There are no conflicts of interest to report. All authors have reviewed approved the manuscript. No author has any COI’s to disclose.
Note: An asterisk (*) denotes studies that were included in the analytic sample for the meta-analysis.
References
- 1. Peters SA, Laham SM, Pachter N, Winship IM. The future in clinical genetics: affective forecasting biases in patient and clinician decision making. Clin Genet. 2014;85(4):312–317. [DOI] [PubMed] [Google Scholar]
- 2. Rhodes R, Strain JJ. Affective forecasting and its implications for medical ethics. Camb Q Healthc Ethics. 2008;17(1):54–65. [DOI] [PubMed] [Google Scholar]
- 3. Ferrer RA, Taber JM, Klein WM, Harris PR, Lewis KL, Biesecker LG. The role of current affect, anticipated affect and spontaneous self-affirmation in decisions to receive self-threatening genetic risk information. Cogn Emot. 2015;29(8):1456–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *4. Ruby MB, Dunn EW, Perrino A, Gillis R, Viel S. The invisible benefits of exercise. Health Psychol. 2011;30(1):67–74. [DOI] [PubMed] [Google Scholar]
- 5. Williams DM. Exercise, affect, and adherence: an integrated model and a case for self-paced exercise. J Sport Exerc Psychol. 2008;30(5):471–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dunton GF, Vaughan E. Anticipated affective consequences of physical activity adoption and maintenance. Health Psychol. 2008;27(6):703–710. [DOI] [PubMed] [Google Scholar]
- 7. Nelissen RM, de Vet E, Zeelenberg M. Anticipated emotions and effort allocation in weight goal striving. Br J Health Psychol. 2011;16(Pt 1):201–212. [DOI] [PubMed] [Google Scholar]
- 8. Janssen E, Waters EA, van Osch L, Lechner L, de Vries H. The importance of affectively-laden beliefs about health risks: the case of tobacco use and sun protection. J Behav Med. 2014;37(1):11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *9. Richard R, Van Der Pligt J, De Vries N. Anticipated regret and time perspective: changing sexual risk-taking behavior. J Behav Decis Mak. 1996;9(3):185–199. [Google Scholar]
- *10. Murgraff V, McDermott MR, White D, Phillips K. Regret is what you get: the effects of manipulating anticipated affect and time perspective on risky single-occasion drinking. Alcohol Alcohol. 1999;34(4):590–600. [DOI] [PubMed] [Google Scholar]
- 11. Cooke R, Sniehotta F, Schüz B. Predicting binge-drinking behaviour using an extended TPB: examining the impact of anticipated regret and descriptive norms. Alcohol Alcohol. 2007;42(2):84–91. [DOI] [PubMed] [Google Scholar]
- 12. Conner M, McEachan R, Taylor N, O’Hara J, Lawton R. Role of affective attitudes and anticipated affective reactions in predicting health behaviors. Health Psychol. 2015;34(6):642–652. [DOI] [PubMed] [Google Scholar]
- 13. Norris E, Myers L. Determinants of personal protective equipment (PPE) use in UK motorcyclists: exploratory research applying an extended theory of planned behaviour. Accid Anal Prev. 2013;60:219–230. [DOI] [PubMed] [Google Scholar]
- 14. Wilson TD, Gilbert DT. Affective forecasting. Adv Exp Soc Psychol. 2003;35:345–411. [Google Scholar]
- 15. Bell DE. Regret in decision making under uncertainty. Oper Res. 1982;30(5):961–981. [Google Scholar]
- 16. Loomes G, Sugden R. Regret theory: an alternative theory of rational choice under uncertainty. Econ J. 1982;92(368):805–824. [Google Scholar]
- 17. Brewer NT, DeFrank JT, Gilkey MB. Anticipated regret and health behavior: A meta-analysis. Health Psychol. 2016;35(11):1264–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Koch EJ. How does anticipated regret influence health and safety decisions? A literature review. Basic Appl Soc Psych. 2014;36(5):397–412. [Google Scholar]
- 19. Sandberg T, Conner M. Anticipated regret as an additional predictor in the theory of planned behaviour: a meta-analysis. Br J Soc Psychol. 2008;47(Pt 4):589–606. [DOI] [PubMed] [Google Scholar]
- 20. Loewenstein GF, Lerner JS. The role of affect in decision making. In: Davidson RJ, Scherer KR, Goldsmith HH, eds. Handbook of affective sciences: Series in affective science. New York, NY: Oxford University Press; 2003:619–642. [Google Scholar]
- 21. Conner M, Godin G, Sheeran P, Germain M. Some feelings are more important: cognitive attitudes, affective attitudes, anticipated affect, and blood donation. Health Psychol. 2013;32(3):264–272. [DOI] [PubMed] [Google Scholar]
- 22. Loewenstein GF, Schkade D. Wouldn’t It be nice? Predicting future feelings. In: Kahneman D, Diener E, Schwarz N, eds. Well-being: The foundations of hedonic psychology. New York, NY: Russell Sage Foundation Press; 1999:85–103. [Google Scholar]
- 23. Ruiter RAC, Abraham C, Kok G. Scary warnings and rational precautions: a review of the psychology of fear appeals. Psychol Health. 2001;16:613–630. [Google Scholar]
- 24. Rogers RW. Cognitive and physiological processes in fear appeals and attitude change: a revised theory of protection motivation. In: Cacioppo JT, Petty R, eds. Social Psychophysiology: A Sourcebook. New York, NY: Guilford Press; 1983:153–177. [Google Scholar]
- 25. Krawczyk A, Knäuper B, Gilca V et al. Parents’ decision-making about the human papillomavirus vaccine for their daughters: I. Quantitative results. Hum Vaccin Immunother. 2015;11(2):322–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Halpern J, Arnold RM. Affective forecasting: an unrecognized challenge in making serious health decisions. J Gen Intern Med. 2008;23(10):1708–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hoerger M, Quirk SW, Lucas RE, Carr TH. Immune neglect in affective forecasting. J Res Pers. 2009;43:91–94. [Google Scholar]
- 28. Winter L, Moss MS, Hoffman C. Affective forecasting and advance care planning: anticipating quality of life in future health statuses. J Health Psychol. 2009;14(3):447–456. [DOI] [PubMed] [Google Scholar]
- 29. Padgett LS, Ferrer RA. Palliative care in cancer: enhancing our view with the science of emotion and decision making. J Palliat Med. 2015;18(6):479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wilson TD, Gilbert DT. Affective forecasting: knowing what to want. Curr Dir Psychol Sci. 2005;14(3):131–134. [Google Scholar]
- 31. Hoerger M. Coping strategies and immune neglect in affective forecasting: direct evidence and key moderators. Judgm Decis Mak. 2012;7(1):86–96. [PMC free article] [PubMed] [Google Scholar]
- 32. Dunn DS, Uswatte G, Elliott TR. Happiness, resilience, and positive growth following physical disability: issues for understanding, research, and therapeutic intervention. In: Shane JL, Snyder CR, eds. Oxford handbook of positive psychology. New York, NY: Oxford University Press; 2009:651–664. [Google Scholar]
- 33. Dunn EW, Wilson TD, Gilbert DT. Location, location, location: the misprediction of satisfaction in housing lotteries. Pers Soc Psychol Bull. 2003;29(11):1421–1432. [DOI] [PubMed] [Google Scholar]
- 34. Dunn EW, Brackett MA, Ashton-James C, Schneiderman E, Salovey P. On emotionally intelligent time travel: individual differences in affective forecasting ability. Pers Soc Psychol Bull. 2007;33(1):85–93. [DOI] [PubMed] [Google Scholar]
- 35. Loewenstein G. Hot-cold empathy gaps and medical decision making. Health Psychol. 2005;24(4S):S49–S56. [DOI] [PubMed] [Google Scholar]
- 36. Loewenstein G. Projection bias in medical decision making. Med Decis Making. 2005;25(1):96–105. [DOI] [PubMed] [Google Scholar]
- 37. Wilson TD, Meyers J, Gilbert DT. Lessons from the past: do people learn from experience that emotional reactions are short-lived?Pers Soc Psychol Bull. 2001;27(12):1648–1661. [Google Scholar]
- 38. McConnell AR, Dunn EW, Austin SN, Rawn CD. Blind spots in the search for happiness: implicit attitudes and nonverbal leakage predict affective forecasting errors. J Exp Soc Psychol. 2011;47(3):628–634. [Google Scholar]
- 39. Helfer SG, Elhai JD, Geers AL. Affect and exercise: positive affective expectations can increase post-exercise mood and exercise intentions. Ann Behav Med. 2015;49(2):269–279. [DOI] [PubMed] [Google Scholar]
- 40. Calabrese SK, Reisen CA, Zea MC, Poppen PJ, Bianchi FT. The pleasure principle: the effect of perceived pleasure loss associated with condoms on unprotected anal intercourse among immigrant Latino men who have sex with men. AIDS Patient Care STDS. 2012;26(7):430–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. LaBrie J, Earleywine M, Schiffman J, Pedersen E, Marriot C. Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. J Sex Res. 2005;42(3):259–266. [DOI] [PubMed] [Google Scholar]
- *42. Dillard AJ, Fagerlin A, Dal Cin S, Zikmund-Fisher BJ, Ubel PA. Narratives that address affective forecasting errors reduce perceived barriers to colorectal cancer screening. Soc Sci Med. 2010;71(1):45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *43. Abraham C, Sheeran P. Acting on intentions: the role of anticipated regret. Br J Soc Psychol. 2003;42(Pt 4):495–511. [DOI] [PubMed] [Google Scholar]
- *44. Abraham C, Sheeran P. Deciding to exercise: the role of anticipated regret. Br J Health Psychol. 2004;9(Pt 2):269–278. [DOI] [PubMed] [Google Scholar]
- *45. Godin G, Germain M, Conner M, Delage G, Sheeran P. Promoting the return of lapsed blood donors: a seven-arm randomized controlled trial of the question-behavior effect. Health Psychol. 2014;33(7):646–655. [DOI] [PubMed] [Google Scholar]
- *46. Godin G, Sheeran P, Conner M et al. Which survey questions change behavior? Randomized controlled trial of mere measurement interventions. Health Psychol. 2010;29(6):636–644. [DOI] [PubMed] [Google Scholar]
- *47. O’Carroll RE, Chambers JA, Brownlee L, Libby G, Steele RJ. Anticipated regret to increase uptake of colorectal cancer screening (ARTICS): a randomised controlled trial. Soc Sci Med. 2015;142:118–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *48. O’Carroll RE, Dryden J, Hamilton-Barclay T, Ferguson E. Anticipated regret and organ donor registration–a pilot study. Health Psychol. 2011;30(5):661–664. [DOI] [PubMed] [Google Scholar]
- *49. O’Carroll RE, Foster C, McGeechan G, Sandford K, Ferguson E. The “ick” factor, anticipated regret, and willingness to become an organ donor. Health Psychol. 2011;30(2):236–245. [DOI] [PubMed] [Google Scholar]
- *50. Sandberg T, Conner M. A mere measurement effect for anticipated regret: impacts on cervical screening attendance. Br J Soc Psychol. 2009;48(Pt 2):221–236. [DOI] [PubMed] [Google Scholar]
- *51. Cox D, Sturm L, Cox AD. Effectiveness of asking anticipated regret in increasing HPV vaccination intention in mothers. Health Psychol. 2014;33(9):1074–1083. [DOI] [PubMed] [Google Scholar]
- *52. Sandberg T, Conner M. Using self-generated validity to promote exercise behaviour. Br J Soc Psychol. 2011;50(4):769–783. [DOI] [PubMed] [Google Scholar]
- *53. O’Carroll RE, Shepherd L, Hayes PC, Ferguson E. Anticipated regret and organ donor registration: a randomized controlled trial. Health Psychol. 2016;35(11):1169–1177. [DOI] [PubMed] [Google Scholar]
- 54. Sprott DE, Spangenberg ER, Block LG et al. The question–behavior effect: What we know and where we go from here. Soc Influ. 2006;1(2):128–137. [Google Scholar]
- 55. Hoerger M, Chapman BP, Epstein RM, Duberstein PR. Emotional intelligence: a theoretical framework for individual differences in affective forecasting. Emotion. 2012;12(4):716–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *56. Ferrer RA, Fisher JD, Buck R, Amico KR. Pilot test of an emotional education intervention component for sexual risk reduction. Health Psychol. 2011;30(5):656–660. [DOI] [PubMed] [Google Scholar]
- *57. Peter PC, Brinberg D. Learning emotional intelligence: an exploratory study in the domain of health. J Appl Soc Psychol. 2012;42(6):1394–1414. [Google Scholar]
- 58. Elwyn G, Stiel M, Durand MA, Boivin J. The design of patient decision support interventions: addressing the theory-practice gap. J Eval Clin Pract. 2011;17(4):565–574. [DOI] [PubMed] [Google Scholar]
- 59. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Caron F, Godin G, Otis J, Lambert LD. Evaluation of a theoretically based AIDS/STD peer education program on postponing sexual intercourse and on condom use among adolescents attending high school. Health Educ Res. 2004;19(2):185–197. [DOI] [PubMed] [Google Scholar]
- 61. Kellar I, Abraham C. Randomized controlled trial of a brief research-based intervention promoting fruit and vegetable consumption. Br J Health Psychol. 2005;10(Pt 4):543–558. [DOI] [PubMed] [Google Scholar]
- 62. Hersch J, Barratt A, Jansen J et al. Use of a decision aid including information on overdetection to support informed choice about breast cancer screening: a randomised controlled trial. Lancet. 2015;385(9978):1642–1652. [DOI] [PubMed] [Google Scholar]
- *63. Fisher A, Bonner C, Biankin AV, Juraskova I. Factors influencing intention to undergo whole genome screening in future healthcare: a single-blind parallel-group randomised trial. Prev Med. 2012;55(5):514–520. [DOI] [PubMed] [Google Scholar]
- 64. Cameron LD, Sherman KA, Marteau TM, Brown PM. Impact of genetic risk information and type of disease on perceived risk, anticipated affect, and expected consequences of genetic tests. Health Psychol. 2009;28(3):307–316. [DOI] [PubMed] [Google Scholar]
- 65. Volandes AE, Lehmann LS, Cook EF, Shaykevich S, Abbo ED, Gillick MR. Using video images of dementia in advance care planning. Arch Intern Med. 2007;167(8):828–833. [DOI] [PubMed] [Google Scholar]
- *66. Chambers JA, Gracie K, Millar R et al. A pilot randomized controlled trial of telephone intervention to increase Breast Cancer Screening uptake in socially deprived areas in Scotland (TELBRECS). J Med Screen. 2016;23(3):141–149. [DOI] [PubMed] [Google Scholar]
- *67. Leaf SL. Do the Right Thing: Anticipated Affect as a Guide to Behavioral Choice [dissertation]. Salt Lake City, UT: University of Utah; 2009 [Google Scholar]
- 68. Shaffer VA, Focella ES, Scherer LD, Zikmund-Fisher BJ. Debiasing affective forecasting errors with targeted, but not representative, experience narratives. Patient Educ Couns. 2016;99(10):1611–1619. [DOI] [PubMed] [Google Scholar]
- 69. Johnson BT, Eagly AH. Quantitative synthesis of social psychological research. In: Reis HT, Judd CM, eds. Handbook of Research Methods in Social and Personality Psychology. New York, NY: Cambridge University Press; 2000:496–528. [Google Scholar]
- 70. Lipsey MW, Wilson DB.. Practical Meta-Analysis. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- 71. Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Behav Stat. 1981;6(2):107–128. [Google Scholar]
- 72. Shaffer VA, Hulsey L, Zikmund-Fisher BJ. The effects of process-focused versus experience-focused narratives in a breast cancer treatment decision task. Patient Educ Couns. 2013;93(2):255–264. [DOI] [PubMed] [Google Scholar]
- *73. Sweeny K, Legg AM. Predictors of interest in direct-to-consumer genetic testing. Psychol Health. 2011;26(10):1259–1272. Availiable at http://www.meta-analysis.com/index.php [DOI] [PubMed] [Google Scholar]
- 74. Biostat. Comprehensive Meta-analysis. 2014. [Google Scholar]
- 75. Cohen J. The effect size index: d. In: Cohen J, ed. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York, NY: Routledge; 1988:284–288. [Google Scholar]
- 76. Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull. 1979;86(3):638–641. [Google Scholar]
- 77. Orwin RG. A fail-safe N for effect size in meta-analysis. J Educ Behav Stat. 1983;8(2):157–159. [Google Scholar]
- 78. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. [DOI] [PubMed] [Google Scholar]
- 80. Romer D, Stanton BF. Feelings about risk and the epidemic diffusion of adolescent sexual behavior. Prev Sci. 2003;4(1):39–53. [DOI] [PubMed] [Google Scholar]
- 81. Houben M, Van Den Noortgate W, Kuppens P. The relation between short-term emotion dynamics and psychological well-being: a meta-analysis. Psychol Bull. 2015;141(4):901–930. [DOI] [PubMed] [Google Scholar]
- 82. Andrade EB, Ariely D. The enduring impact of transient emotions on decision making. Organ Behav Hum Decis Process. 2009;109(1):1–8. [Google Scholar]
- 83. Schwarz N, Clore GL. Feelings and phenomenal experiences. In: Kruglanski A, Higgins T, eds. Social Psychology: Handbook of Basic Principles. 2nd ed. New York, NY: Guilford Press; 1996:385–400. [Google Scholar]
- 84. Zajonc RB. Feeling and thinking: Preferences need no inferences. Am Psychol. 1980;35(2):151–175. [Google Scholar]
- 85. Damasio AR, Everitt BJ, Bishop D. The somatic marker hypothesis and the possible functions of the prefrontal cortex [and discussion]. Philos Trans R Soc Lond. B. 1996;351(1346):1413–1420. [DOI] [PubMed] [Google Scholar]
- 86. Peters E, Lipkus I, Diefenbach MA. The functions of affect in health communications and in the construction of health preferences. J Commun. 2006;56(S1):S140–S162. [Google Scholar]
- 87. Loewenstein GF, Weber EU, Hsee CK, Welch N. Risk as feelings. Psychol Bull. 2001;127(2):267–286. [DOI] [PubMed] [Google Scholar]
- 88. Slovic P, Peters E, Finucane ML, Macgregor DG. Affect, risk, and decision making. Health Psychol. 2005; 24(4S):S35–S40. [DOI] [PubMed] [Google Scholar]
- 89. Ellis EM, Homish GG, Parks KA, Collins RL, Kiviniemi MT. Increasing condom use by changing people’s feelings about them: an experimental study. Health Psychol. 2015;34(9):941–950. [DOI] [PubMed] [Google Scholar]
- 90. Walsh EM, Kiviniemi MT. Changing how I feel about the food: experimentally manipulated affective associations with fruits change fruit choice behaviors. J Behav Med. 2014;37(2):322–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kiviniemi MT, Duangdao KM. Affective associations mediate the influence of cost-benefit beliefs on fruit and vegetable consumption. Appetite. 2009;52(3):771–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Kiviniemi MT, Voss-Humke AM, Seifert AL. How do I feel about the behavior? The interplay of affective associations with behaviors and cognitive beliefs as influences on physical activity behavior. Health Psychol. 2007;26(2):152–158. [DOI] [PubMed] [Google Scholar]
- 93. Lawton R, Conner M, McEachan R. Desire or reason: predicting health behaviors from affective and cognitive attitudes. Health Psychol. 2009;28(1):56–65. [DOI] [PubMed] [Google Scholar]
- 94. Lawton R, Conner M, Parker D. Beyond cognition: predicting health risk behaviors from instrumental and affective beliefs. Health Psychol. 2007;26(3):259–267. [DOI] [PubMed] [Google Scholar]
- 95. Keer M, van den Putte B, Neijens P. The interplay between affect and theory of planned behavior variables. Am J Health Behav. 2012;36(1):107–115. [DOI] [PubMed] [Google Scholar]
- 96. Keer M, van den Putte B, Neijens P. The role of affect and cognition in health decision making. Br J Soc Psychol. 2010;49(Pt 1):143–153. [DOI] [PubMed] [Google Scholar]
- 97. Nielsen L, Knutson B, Carstensen LL. Affect dynamics, affective forecasting, and aging. Emotion. 2008;8(3):318–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Zeelenberg M, Nelissen RM, Breugelmans SM, Pieters R. On emotion specificity in decision making: why feeling is for doing. Judgm Decis Mak. 2008;3(1):18–27. [Google Scholar]
- 99. Zeelenberg M, Pieters R. A theory of regret regulation 1.0. J Consum Psychol. 2007;17(1):3–18. [Google Scholar]
- 100. Saffrey C, Summerville A, Roese NJ. Praise for regret: people value regret above other negative emotions. Motiv Emot. 2008;32(1):46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Hoerger M, Quirk SW. Affective forecasting and the Big Five. Pers Individ Dif. 2010;49(8):972–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Brenner CJ, Ben-Zeev D. Affective forecasting in schizophrenia: comparing predictions to real-time Ecological Momentary Assessment (EMA) ratings. Psychiatr Rehabil J. 2014;37(4):316–320. [DOI] [PubMed] [Google Scholar]
- 103. Elwyn G, Kreuwel I, Durand MA et al. How to develop web-based decision support interventions for patients: a process map. Patient Educ Couns. 2011;82(2):260–265. [DOI] [PubMed] [Google Scholar]
- 104. Hoerger M, Quirk SW, Lucas RE, Carr TH. Cognitive determinants of affective forecasting errors. Judgm Decis Mak. 2010;5(5):365–373. [PMC free article] [PubMed] [Google Scholar]
- 105. Quoidbach J, Wood AM, Hansenne M. Back to the future: The effect of daily practice of mental time travel into the future on happiness and anxiety. J Posit Psychol. 2009;4(5):349–355. [Google Scholar]
- 106. Van Boven L, Loewenstein G, Welch E, Dunning D. The illusion of courage in self-predictions: mispredicting one’s own behavior in embarrassing situations. J Behav Decis Mak. 2012;25(9):1–12. [Google Scholar]
- 107. Block SD. Psychological issues in end-of-life care. J Palliat Med. 2006;9(3):751–772. [DOI] [PubMed] [Google Scholar]
- 108. Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: a meta-analysis. Psychol Bull. 1999;125(1):90–132. [DOI] [PubMed] [Google Scholar]
- 109. Baron J, Ritov I. Reference points and omission bias. Organ Behav Hum Decis Process. 1994;59(3):475–498. [DOI] [PubMed] [Google Scholar]
- 110. Ritov I, Baron J. Outcome knowledge, regret, and omission bias. Organ Behav Hum Decis Process. 1995;64(2):119–127. [DOI] [PubMed] [Google Scholar]
- 111. Anderson CJ. The psychology of doing nothing: forms of decision avoidance result from reason and emotion. Psychol Bull. 2003;129(1):139–167. [DOI] [PubMed] [Google Scholar]
- 112. Knobe J. Intentional action and side effects in ordinary language. Analysis. 2003;63(279):190–194. [Google Scholar]
- 113. Parker C, Gillessen S, Heidenreich A, Horwich A; ESMO Guidelines Committee Cancer of the prostate: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26 (suppl. 5):v69–v77. [DOI] [PubMed] [Google Scholar]
- 114. Ubel PA, Loewenstein G, Schwarz N, Smith D. Misimagining the unimaginable: the disability paradox and health care decision making. Health Psychol. 2005;24(4S):S57–S62. [DOI] [PubMed] [Google Scholar]
- 115. Smith D, Loewenstein G, Jepson C, Jankovich A, Feldman H, Ubel P. Mispredicting and misremembering: patients with renal failure overestimate improvements in quality of life after a kidney transplant. Health Psychol. 2008;27(5):653–658. [DOI] [PubMed] [Google Scholar]
- 116. Halpern SD. Shaping end-of-life care: behavioral economics and advance directives. Semin Respir Crit Care Med. 2012;33(4):393–400. [DOI] [PubMed] [Google Scholar]
- 117. Chochinov HM, Tataryn D, Clinch JJ, Dudgeon D. Will to live in the terminally ill. Lancet. 1999;354(9181):816–819. [DOI] [PubMed] [Google Scholar]
- 118. Gready RM, Ditto PH, Danks JH, Coppola KM, Lockhart LK, Smucker WD. Actual and perceived stability of preferences for life-sustaining treatment. J Clin Ethics. 2000;11(4):334–346. [PubMed] [Google Scholar]
- 119. Ditto PH, Hawkins NA, Pizarro DA. Imagining the End of Life: on the psychology of advance medical decision making. Motiv Emot. 2005;29(4):475–496. [Google Scholar]
- 120. Han PK, Moser RP, Klein WM. Perceived ambiguity about cancer prevention recommendations: associations with cancer-related perceptions and behaviours in a US population survey. Health Expect. 2007;10(4):321–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Marroquín B, Nolen-Hoeksema S, Miranda R. Escaping the future: Affective forecasting in escapist fantasy and attempted suicide. J Soc Clin Psychol. 2013;32(4):446–463. [Google Scholar]
- *122. Abraham C, Henderson M, Der G. Cognitive impact of a research-based school sex education programme. Psychol Health. 2004;19:689–703. [Google Scholar]
- *123. Angott AM, Comerford DA, Ubel PA. Imagining life with an ostomy: does a video intervention improve quality-of-life predictions for a medical condition that may elicit disgust?Patient Educ Couns. 2013;91(1):113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *124. Barkoukis V, Lazuras L, Harris PR. The effects of self-affirmation manipulation on decision making about doping use in elite athletes. Psychol Sport Exerc. 2015;16:175–181. [Google Scholar]
- *125. Brown KE, Hurst KM, Arden MA. Improving adolescent contraceptive use: evaluation of a theory-driven classroom-based intervention. Psychol Health Med. 2011;16(2):141–155. [DOI] [PubMed] [Google Scholar]
- *126. Bui M. Consumer Regret Regulation: Examining the Effects of Anticipated Regret on Health-Related Decisions [dissertation]. New Orleans, LA: Loyola University; 2009. [Google Scholar]
- *127. Clowes R, Masser BM. Right here, right now: the impact of the blood donation context on anxiety, attitudes, subjective norms, self-efficacy, and intention to donate blood. Transfusion. 2012;52(7):1560–1565. [DOI] [PubMed] [Google Scholar]
- *128. Dillard AJ, Wertheimer M.. Emotion Adaptation Recall Reduces Expectations of Pain for Colon Cancer Screening. 2016, unpublished data. [Google Scholar]
- *129. Ferrer RA, Klein WM, Zajac LE, Land SR, Ling BS. An affective booster moderates the effect of gain- and loss-framed messages on behavioral intentions for colorectal cancer screening. J Behav Med. 2012;35(4):452–461. [DOI] [PubMed] [Google Scholar]
- *130. Fisher A, Bonner C, Biankin AV, Juraskova I. Factors influencing intention to undergo whole genome screening in future healthcare: a single-blind parallel-group randomised trial. Prev Med. 2012;55(5):514–520. [DOI] [PubMed] [Google Scholar]
- *131. France CR, France JL, Kowalsky JM et al. A Web-based approach to blood donor preparation. Transfusion. 2013;53(2):328–336. [DOI] [PubMed] [Google Scholar]
- *132. Martinez LS. Explaining the effects of anticipated regret messages on young women’s intention to consume folic acid: a moderated-mediation model. J Health Commun. 2014;19(1):115–132. [DOI] [PubMed] [Google Scholar]
- *133. Moser SE. Development and Evaluation of an Intervention to Increase Sun Protection in Young Women [dissertation]. Tempe, AZ: Arizona State University; 2012. [Google Scholar]
- *134. Muller C, Cameron LD. Trait anxiety, information modality, and responses to communications about prenatal genetic testing. J Behav Med. 2014;37(5):988–999. [DOI] [PubMed] [Google Scholar]
- *135. Ogden J, Daniells E, Barnett J. When is choice a good thing? An experimental study of the impact of choice on patient outcomes. Psychol Health Med. 2009;14(1):3s4–47. [DOI] [PubMed] [Google Scholar]
- *136. O’Hara RE. Anticipated Emotion in Health Decision Making: An Extension of the Prototype-Willingness Model [dissertation]. Hanover, NH: Dartmouth College; 2012. [Google Scholar]
- *137. Reid M, Ryda C, Jessop D.. The Impact of Attention Spreading and Self-Affirmation Interventions on Myopic Forecasting in Exercising. 2013, unpublished data. [Google Scholar]
- *138. Smerecnik CM, Ruiter RA. Fear appeals in HIV prevention: the role of anticipated regret. Psychol Health Med. 2010;15(5):550–559. [DOI] [PubMed] [Google Scholar]