Abstract
Objectives
To identify the frequency with which antibiotics are prescribed in the absence of a documented indication in the ambulatory care setting, to quantify the potential effect on assessments of appropriateness of antibiotics, and to understand patient, provider, and visit level characteristics associated with antibiotic prescribing without a documented indication.
Design
Cross sectional study.
Setting
2015 National Ambulatory Medical Care Survey.
Participants
28 332 sample visits representing 990.9 million ambulatory care visits nationwide.
Main outcome measures
Overall antibiotic prescribing and whether each antibiotic prescription was accompanied by appropriate, inappropriate, or no documented indication as identified through ICD-9-CM (international classification of diseases, 9th revision, clinical modification) codes. Survey weighted multivariable logistic regression was used to evaluate potential risk factors for receipt of an antibiotic prescription without a documented indication.
Results
Antibiotics were prescribed during 13.2% (95% confidence interval 11.6% to 13.7%) of the estimated 990.8 million ambulatory care visits in 2015. According to the criteria, 57% (52% to 62%) of the 130.5 million prescriptions were for appropriate indications, 25% (21% to 29%) were inappropriate, and 18% (15% to 22%) had no documented indication. This corresponds to an estimated 24 million prescriptions without a documented indication. Being an adult male, spending more time with the provider, and seeing a non-primary care specialist were significantly positively associated with antibiotic prescribing without an indication. Sulfonamides and urinary anti-infective agents were the antibiotic classes most likely to be prescribed without documentation.
Conclusions
This nationally representative study of ambulatory visits identified a large number of prescriptions for antibiotics without a documented indication. Antibiotic prescribing in the absence of a documented indication may severely bias national estimates of appropriate antibiotic use in this setting. This study identified a wide range of factors associated with antibiotic prescribing without a documented indication, which may be useful in directing initiatives aimed at supporting better documentation.
Introduction
Inappropriate prescribing of antibiotics is a major public health problem, as it contributes to antibiotic resistance.1 2 In the US, medical providers often incorrectly prescribe antibiotics for acute viral respiratory infections, especially during peak influenza season.3 4 5 6 Antimicrobial therapy is extremely common in US ambulatory care settings,2 4 7 8 9 10 with an estimated 836 antibiotic prescriptions per 1000 people in 2016. Investigators have shown that more than 30% of antibiotic prescriptions in ambulatory care settings are inappropriate.11 12 13
Programs evaluating antibiotic use depend on the presence of a documented indication in patients’ medical records, as the frequency of inappropriate use is determined by these indications.14 However, this documentation is not universally required, and missing indication data may lead to underestimates of inappropriate antibiotic use.14 15 In turn, this hinders antibiotic stewardship and public health efforts, because the extent of the problem is neither measured accurately nor understood completely.
Our objective was to identify the frequency with which antibiotics are prescribed in the absence of a documented indication by using a nationally representative sample of ambulatory clinic encounters to estimate the degree to which previous estimates of appropriate prescribing may have been biased. We also sought to understand the patient, provider, and visit level characteristics associated with antibiotic prescribing without a documented indication.
Methods
Data sources
The National Ambulatory Medical Care Survey (NAMCS) is an annual national survey conducted by the National Center for Health Statistics. It uses a probabilistic sampling framework to obtain a representative sample of office based US physicians.16 Physicians complete an automated survey describing a sample of patients’ visits during a specified reporting period. NAMCS staff abstract additional information from electronic medical records. NAMCS provides more than 1000 variables related to various aspects of a medical visit, including patients’ demographic information, information on the provider, diagnosis and procedure codes, and drug administration.16 We analyzed the 28 332 visits (representing 990.8 million visits across the US) to office based healthcare providers that were sampled in 2015. Complete survey methods and descriptive statistics can be found in the 2015 NAMCS documentation file.16
Inclusion criteria
We included patients with a least one antibiotic prescription in our analyses. NAMCS uses the Cerner Multum Lexicon Plus database to convert information on drugs prescribed to therapeutic drug classes and includes up to 30 drug names for a single office visit.16 17 We determined that an antibiotic was prescribed during an in-person office visit if any of the Multum Level 2 category identifiers for antibacterial agents were present.
Classification of antibiotic prescribing indications
To identify indications for antibiotic prescribing, we evaluated encounter diagnosis codes for bacterial infections or other conditions for which antibiotics are frequently prescribed. NAMCS reports up to five ICD-9-CM (international classification of diseases, 9th revision, clinical modification) codes. On the basis of the complete list of ICD-9-CM codes available for each visit in which an antibiotic prescription was reported, we considered the indication to be “appropriate” if any bacterial infection or other condition for which antibiotics are always or sometimes indicated was documented, “inappropriate” if only a condition for which antibiotics are not indicated but are commonly prescribed (for example, upper respiratory tract infection) was documented, or “no documented indication” if neither of the preceding categories was applicable. We adapted these classifications from the three diagnosis tiers previously reported by Fleming-Dutra et al (see appendix).11 Our list was similar to those generated by other research groups examining inappropriate prescribing behaviors.12 18
Definitions of other variables
We evaluated several potentially important risk factors for prescription of antibiotics without a documented indication, including patient, provider, and visit level characteristics. We categorized age as under 18, 18 to 64, and 65 years and older. We categorized provider specialty as primary care (general/family medicine, pediatrics, and internal medicine), specialty care in which antibiotics are commonly prescribed (gynecology, urology, dermatology, and otolaryngology), and all other specialties.14 We also assessed seasonal variation (winter, spring, summer, and fall). We identified the presence of chronic disease through the NAMCS survey item “Total number of chronic diseases” (0-12) and then dichotomized the variable (0 v ≥1 chronic conditions).
Statistical analysis
All analyses accounted for the complex survey design by using variables provided by NAMCS. We calculated patient, provider, and visit level characteristics as weighted percentages and 95% confidence intervals stratified by whether antibiotics were prescribed with an appropriate, inappropriate, or missing indication.16 We used Rao-Scott χ2 tests to test for heterogeneity. Although our main interest was records that lacked a documented indication, we presented results for prescriptions that were written with an inappropriate indication for comparison.
We built a multivariable survey weighted logistic regression model to identify risk factors associated with antibiotic prescriptions with no documented indication. Variables with a P value of less than 0.15 in bivariable analyses were assessed for inclusion in the multivariable model, as was an interaction term for age and sex based on our previous findings.19 We did backward selection and retained variables that significantly (P<0.05) contributed to the model, along with age, sex, geographic region, and pre-surgery visit status, which we chose a priori as potential confounders. We generated stratum specific odds ratios and corresponding 95% confidence intervals by using the significant interaction term from the final model. We used SAS 9.4 for analyses and generated figures with R.
Patient and public involvement
This research was completed without patient involvement. Patients were not invited to comment on the study design and were not consulted to interpret the results. Patients were not invited to contribute to the reporting of our findings.
Results
Study population
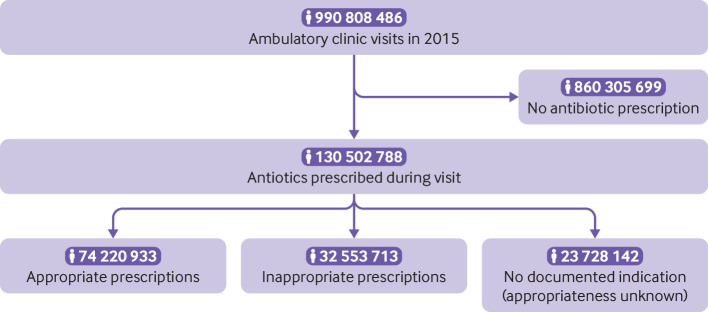
An estimated 990.8 million ambulatory care visits to office based healthcare providers took place in 2015, as reported by NAMCS (fig 1). Of those visits, approximately 130 million (13.2%, 95% confidence interval 11.6% to 13.7%) involved receipt of an antibiotic prescription and were included in our study. An average of 2.6 diagnosis codes were documented per visit (median=2), and 17% (14% to 20%) of visits had the maximum number of diagnosis codes (five codes) available in the dataset.
Fig 1.
Derivation of analytic sample: weighted counts from 2015 National Ambulatory Medical Care Survey
Prescribing without documented indication
Among included visits (130.5 million estimated), we deemed 57% (52% to 62%) of indications for antibiotic prescription to be appropriate according to our criteria and 25% (21% to 29%) to be inappropriate; 18% (15% to 22%) lacked either an appropriate or an inappropriate documented indication (fig 1). This corresponds to an estimated 23.7 million antibiotic prescriptions without a documented indication in 2015. The most common diagnoses reported among the no indication group were unspecified essential hypertension (401.9: 11%, 7% to 16%), diabetes mellitus without mention of complication (250.00; 8%, 4% to 13%), and other specified aftercare (V58.89; 7%, 1% to 14%). No other codes were present in more than 5% of “no indication” visits. We observed no clear difference in prescribing without an indication across seasons (P=0.58; fig 2).
Fig 2.
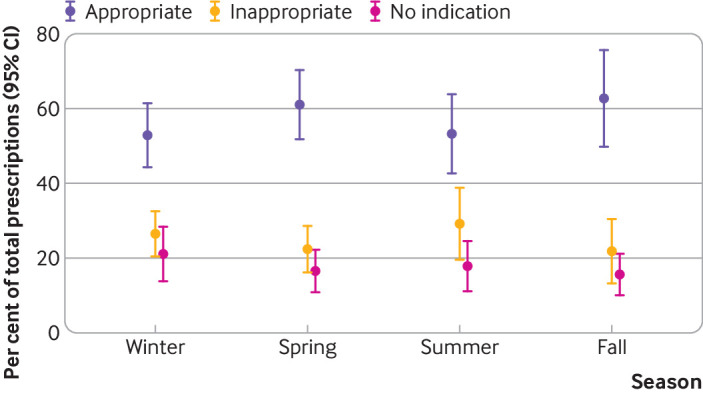
Seasonal trends for appropriateness of antibiotic prescribing. Rao-Scott χ2 test for differences in prescribing without indication, P=0.58. 37% of annual antibiotic prescriptions were in winter, 21% in spring, 18% in summer, and 24% in fall
Patients’ characteristics
Patients who received antibiotics were more likely to be male (61%) and non-Hispanic white (58%), compared with those who did not. The median age was 47 years. In bivariable comparisons, several patient level characteristics were significantly associated with receipt of an antibiotic prescription without an indication (table 1). Twenty per cent of adults aged 18-64 and 22% of those aged 65 years and older received antibiotics without a documented indication, compared with 8% of patients under 18 years (table 1). Chronic conditions were also associated with more prescribing without an indication (22% for patients with a chronic condition versus 14% for those without). Patients with Medicare or Medicaid insurance seemed to have a higher proportion of prescriptions without an indication (21% on Medicare/Medicaid versus 16% for those with private insurance), but differences were not statistically significant in bivariable analysis. We observed no apparent differences by race/ethnicity.
Table 1.
Bivariable comparisons of patient, provider, and visit characteristics by indication type. Values are percentages (95% CI) unless stated otherwise
| Characteristics | Overall | Indication type | P value* | ||
|---|---|---|---|---|---|
| Appropriate | Inappropriate | No indication | |||
| Overall proportion | - | 57 (52 to 62) | 25 (21 to 29) | 18 (15 to 22) | - |
| Patients | |||||
| Sex: | 0.54 | ||||
| Male | 61 (56 to 66) | 54 (48 to 60) | 29 (24 to 34) | 17 (12 to 22) | |
| Female | 39 (34 to 44) | 59 (52 to 65) | 23 (18 to 27) | 19 (15 to 23) | |
| Age, years: | <0.001 | ||||
| <18 | 21 (16 to 27) | 78 (72 to 84) | 13 (7 to 19) | 8 (5 to 11) | |
| 18-64 | 56 (50 to 63) | 56 (48 to 63) | 24 (19 to 29) | 20 (15 to 25) | |
| ≥65 | 22 (19 to 26) | 40 (32 to 47) | 38 (31 to 45) | 22 (16 to 28) | |
| Race/ethnicity: | 0.35 | ||||
| Non-Hispanic white | 58 (51 to 66) | 56 (51 to 62) | 25 (21 to 29) | 18 (14 to 23) | |
| Non-Hispanic black | 15 (11 to 18) | 50 (41 to 59) | 26 (18 to 33) | 24 (17 to 31) | |
| Hispanic | 19 (14 to 24) | 59 (50 to 68) | 27 (18 to 36) | 14 (8 to 19) | |
| Other non-Hispanic | 8 (2 to 14) | 67 (40 to 93) | 17 (2 to 33) | 16 (2 to 31) | |
| Payment type: | 0.26 | ||||
| Private insurance | 49 (43 to 54) | 62 (56 to 68) | 22 (18 to 27) | 16 (12 to 20) | |
| Medicare/Medicaid | 39 (34 to 45) | 48 (43 to 54) | 30 (26 to 35) | 21 (17 to 26) | |
| Self pay | 5 (1 to 8) | 74 (49 to 99) | 15 (0 to 30) | 11 (0 to 24) | |
| Other/missing | 7 (1 to 14) | 60 (41 to 78) | 20 (10 to 30) | 20 (10 to 31) | |
| Chronic disease: | 0.005 | ||||
| Yes | 56 (50 to 62) | 50 (43 to 56) | 29 (24 to 34) | 22 (17 to 27) | |
| No | 44 (38 to 50) | 66 (61 to 71) | 20 (16 to 24) | 14 (10 to 17) | |
| Providers | |||||
| Geographic region: | 0.92 | ||||
| West | 21 (15 to 27) | 63 (49 to 77) | 18 (11 to 26) | 19 (11 to 26) | |
| Midwest | 17 (13 to 22) | 56 (47 to 65) | 22 (17 to 26) | 17 (13 to 20) | |
| North east | 24 (17 to 31) | 48 (41 to 56) | 34 (27 to 42) | 17 (11 to 23) | |
| South | 38 (30 to 47) | 59 (51 to 68) | 22 (17 to 26) | 19 (12 to 26) | |
| Specialty category: | <0.001 | ||||
| Primary care | 60 (52 to 68) | 69 (64 to 75) | 18 (14 to 23) | 12 (9 to 16) | |
| Common antibiotic. prescribers† | 14 (10 to 18) | 43 (38 to 49) | 32 (28 to 36) | 24 (18 to 31) | |
| All other specialties | 25 (19 to 32) | 35 (18 to 52) | 36 (24 to 48) | 29 (18 to 39) | |
| Ownership type: | 0.092 | ||||
| Physician or physician group | 77 (69 to 84) | 54 (48 to 61) | 27 (22 to 31) | 19 (15 to 24) | |
| Medical/academic center | 7 (3 to 11) | 62 (46 to 77) | 18 (7 to 28) | 21 (13 to 28) | |
| Insurance company/HMO/other | 16 (10 to 23) | 67 (59 to 75) | 21 (12 to 30) | 12 (7 to 17) | |
| Visits | |||||
| Primary care physician: | 0.004 | ||||
| Yes | 52 (44 to 59) | 70 (64 to 76) | 17 (13 to 20) | 14 (10 to 17) | |
| No | 47 (39 to 54) | 42 (34 to 51) | 34 (28 to 41) | 23 (17 to 29) | |
| Median time with provider, min: | 0.023 | ||||
| <17 | 48 (42 to 54) | 65 (59 to 72) | 20 (16 to 24) | 15 (11 to 19) | |
| ≥17 | 52 (46 to 58) | 49 (43 to 55) | 30 (24 to 35) | 21 (17 to 26) | |
| Culture taken: | <0.001 | ||||
| Yes | 11 (6 to 16) | 71 (60 to 82) | 24 (12 to 37) | 5 (1 to 9) | |
| No | 89 (84 to 94) | 55 (49 to 61) | 25 (21 to 29) | 20 (16 to 24) | |
| Antibiotic class: | <0.001 | ||||
| Cephalosporins | 12 (9 to 14) | 64 (53 to 75) | 16 (10 to 23) | 20 (12 to 27) | |
| Macrolides | 18 (12 to 23) | 67 (57 to 78) | 19 (11 to 26) | 14 (7 to 21) | |
| Miscellaneous | 9 (7 to 11) | 44 (35 to 54) | 32 (22 to 43) | 23 (16 to 31) | |
| Penicillins | 23 (19 to 26) | 72 (64 to 79) | 18 (12 to 23) | 11 (7 to 15) | |
| Quinolones | 20 (16 to 24) | 42 (32 to 52) | 38 (29 to 47) | 20 (13 to 28) | |
| Sulfonamides | 2 (0 to 3) | 32 (3 to 61) | 16 (1 to 31) | 52 (17 to 87) | |
| Tetracyclines | 7 (6 to 9) | 51 (41 to 62) | 30 (21 to 39) | 18 (10 to 26) | |
| Urinary anti-infectives | 4 (2 to 6) | 33 (21 to 45) | 33 (18 to 48) | 34 (21 to 47) | |
| Other‡ | 5 (4 to 8) | 55 (44 to 67) | 25 (15 to 34) | 20 (9 to 31) | |
| Main reason for visit: | <0.001 | ||||
| New problem | 54 (49 to 59) | 71 (65 to 77) | 20 (16 to 24) | 9 (12 to 27) | |
| Chronic problem, routine | 19 (15 to 22) | 45 (33 to 57) | 29 (21 to 37) | 26 (16 to 36) | |
| Chronic problem, flare-up | 7 (4 to 10) | 50 (35 to 65) | 32 (23 to 42) | 18 (7 to 29) | |
| Pre-surgery | 2 (1 to 3) | 3 (0 to 5) | 68 (53 to 84) | 29 (14 to 44) | |
| Post-surgery | 8 (4 to 12) | 43 (30 to 56) | 37 (23 to 50) | 21 (9 to 32) | |
| Preventive care | 10 (7 to 12) | 31 (19 to 43) | 21 (13 to 29) | 49 (37 to 60) | |
HMO=health maintenance organization.
Rao-Scott χ2 P value for any (appropriate or inappropriate) versus no indication.
Includes gynecologists, dermatologists, urologists, and otolaryngologists.
Includes carbapenems, leprostatics, aminoglycosides, lincomycin derivatives, glycylcyclines, and glycopeptide antibiotics.
Providers’ characteristics
In bivariable analysis (table 1), primary care providers had a significantly lower percentage of antibiotic prescriptions without a documented indication (12%), compared with other specialists who commonly prescribe antibiotics (24%), as well as those in all other specialties (29%). We observed no difference between solo and group practitioners (data not shown), but differences existed according to practice ownership. Insurance company or health maintenance organization (HMO) affiliated offices had a lower proportion (12%) of prescriptions without an indication than did offices owned by a physician or group of physicians (19%) or academic health centers (21%) (table 1).
Characteristics of visits
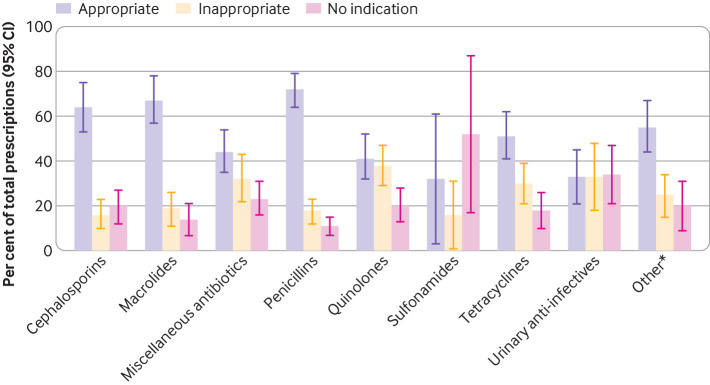
In bivariable analyses (table 1), prescribing without a documented indication was significantly less frequent when a patient received the prescription from his or her designated primary care physician (14%) compared with another provider (23%). Patients who spent less time with a physician were less likely to receive an antibiotic without indication (15% for those with shorter visits versus 21% with longer visits). When a microbiology culture (blood, urine, throat, or other) was collected during a visit, 5% of prescriptions lacked an indication compared with 20% in the absence of a culture. No clear difference in indications by antibiotic class was apparent (table 1 and fig 3). Among all prescriptions without a documented indication, 22% were for quinolones, 14% for macrolides, 13% for penicillins, and 13% for cephalosporins. No clear differences in prevalence of indication by day of the week were apparent (data not shown).
Fig 3.
Appropriateness of prescribing by class of antibiotic. *Includes carbapenems, leprostatics, aminoglycosides, lincomycin derivatives, glycylcyclines, and glycopeptide antibiotics
Multivariable modeling
Table 2 shows the results of our multivariable logistic regression analysis. We identified a significant interaction between age group and sex. Adult men (18 years and older) were more likely to receive an antibiotic prescription without a documented indication than were male patients under 18 years (adjusted odds ratio 2.3, 95% confidence interval 1.0 to 5.3); however, these age groups did not differ significantly for female patients. Specialties that frequently prescribe antibiotics and all other specialties were twice as likely to prescribe antibiotics without an indication than were primary care physicians. Longer visits were associated with an almost twofold increase in the odds of prescribing without a documented indication compared with shorter visits. For visits with a blood, urine, or throat culture, clinicians were much less likely to prescribe without an indication compared with visits at which no culture was taken (adjusted odds ratio 0.2, 0.1 to 0.4). Sulfonamides and urinary anti-invectives were more likely to be prescribed without an indication than were penicillins, which had the highest prevalence of antibiotics with a documented indication.
Table 2.
Adjusted odds ratios for association between significant independent predictors and antibiotic prescription without documented indication
| Predictors | Adjusted odds ratio* (95% CI) |
|---|---|
| Age and sex: | |
| Males: ≥18 v <18 | 2.3 (1.02 to 5.3) |
| Females: ≥18 v <18 | 1.1 (0.6 to 2.2) |
| Chronic disease | 1.4 (0.95 to 2.2) |
| Specialty: | |
| Primary care | Reference |
| All other specialties | 2.1 (1.2 to 3.7) |
| Common prescribers† | 1.9 (1.1 to 3.3) |
| Longer visit: ≥17 min v <17 min | 1.6 (1.1 to 2.5) |
| Culture taken | 0.2 (0.1 to 0.4) |
| Antibiotic class: | |
| Penicillins | Reference |
| Cephalosporins | 1.6 (0.96 to 2.7) |
| Macrolides | 0.9 (0.4 to 2.1) |
| Miscellaneous | 1.6 (0.8 to 3.2) |
| Other‡ | 1.3 (0.7 to 2.5) |
| Quinolones | 1.5 (0.8 to 2.7) |
| Sulfonamides | 4.9 (1.5 to 15.7) |
| Tetracyclines | 1.3 (0.6 to 2.7) |
| Urinary anti-infectives | 3.1 (1.3 to 7.6) |
Adjusted for age, sex, geographic region, and pre-surgery visit.
Includes specialists in gynecology, urology, dermatology, and otolaryngology.
Includes carbapenems, leprostatics, aminoglycosides, lincomycin derivatives, glycylcyclines, and glycopeptide antibiotics.
Discussion
We observed that approximately 24 million US ambulatory care visits with antibiotic prescriptions lacked a documented indication in 2015. Taken with the 32 million prescriptions that we identified as inappropriate, as many as 43% of prescriptions in our dataset were potentially inappropriate. Without evidence of an indication, the appropriateness of these prescriptions cannot be ascertained. Potentially compounding the high rates of inappropriate antibiotic prescribing, the magnitude of antibiotic prescriptions without a documented indication poses a barrier to antimicrobial stewardship and public health efforts intended to evaluate and improve antibiotic prescribing in ambulatory care settings. Several studies have estimated the prevalence of antibiotic prescribing,7 11 20 21 or examined inappropriate prescribing for upper respiratory tract infections,3 4 5 8 but these estimates have typically relied on documented diagnosis codes to classify the appropriateness of antibiotic prescribing. The primary objective of this study was to highlight the potential degree of misclassification that may occur due to under-coding. Unnecessary antibiotic prescriptions represent an important target for antimicrobial stewardship efforts in ambulatory care settings. Our work complements previous work in this area by assessing the potential effect that prescribing without a documented indication may have on the estimated burden of unnecessary antibiotic use.
Our study is among the first to examine factors associated with antibiotic prescriptions with a lack of documented indication. We identified both patient and provider level characteristics associated with a greater likelihood of antibiotic prescribing without documentation of an indication. Adult male patients were significantly more likely than younger male patients to receive an antibiotic prescription without documentation of the indication in their medical record. Visits with specialty care providers who frequently prescribe antibiotics were also significantly less likely to provide a coded indication than were primary care providers. Sulfonamides and urinary anti-infectives had a higher proportion of missing indications than did penicillins. Among recipients of urinary anti-infectives, 9% had ICD-9-CM codes indicating non-specific urinary symptoms (for example, dysuria, urinary frequency, incontinence, urgency) that could potentially indicate urinary tract infection but were not considered a possible indication in our analysis. Although this provides some insight into the possible indication for these antibiotics, it represents only 0.6% of the total prescribing without a documented indication.
By identifying factors associated with prescribing without a documented indication, we can better inform antimicrobial stewardship and public health interventions. For example, Meeker et al found that requiring primary care clinicians to enter free text justifications when ordering antibiotics lowered rates of inappropriate prescribing.22 23 Similar strategies may benefit ambulatory specialty care clinics. Our findings suggest that improving coding practices in non-primary care practice settings could facilitate accurate assessments of the appropriateness of antibiotic prescribing.
Limitations of study
Because our study used nationally representative survey data, our results are highly generalizable to the US population. However, several limitations should be noted. Only the first five ICD-9-CM codes documented in the health record were included in the survey data. Thus, we were not able to ascertain whether indications would have been present if additional codes were available or documented in providers’ notes. In the event that all 17% of visits with no indication with the maximum number of ICD-9-CM codes reported were misclassified (that is, an indication would have been identified if additional codes were reported), 15% (95% confidence interval 12% to 18%) of visits associated with an antibiotic prescription would still lack a documented indication. In other words, at best, only an additional 3% of prescriptions could be evaluated for appropriateness if more than five diagnosis codes were available. We were also unable to identify prescriptions for anticipated future use, such as for travel. Finally, to be included in the NAMCS dataset, the patient must have made an in-person visit to an ambulatory care facility, and we were unable to assess the appropriateness of any prescriptions provided as part of virtual or telephone encounters. Retail health clinics have also emerged as a major source of antibiotic prescribing, especially for acute respiratory illness.24 The increasing trend of antibiotic prescribing via telemedicine and the prevalence of non-prescription antibiotic use are additional areas to examine for inappropriate use of antibiotics.25 26
An additional limitation involves the cross sectional study design, which prevented the use of the patient’s history of the present illness in exploring possible indications. We found that 60% of antibiotic prescriptions without documentation were documented as continuing (versus new) compared with 24% of appropriate prescriptions. Among those with all five codes and no documented indication, half of the major reasons for the visit were chronic problems (31% for routine and 21% for flare-up). Although the indication for the prescribed antibiotic might have been documented during a previous visit, the lack of documentation at the time of prescribing poses a challenge to ongoing efforts to evaluate appropriateness. These results point to a recurring theme whereby prescription of an antibiotic may be warranted but, owing to the lack of documented indication, we cannot be certain.
Conclusions and public health implications
We identified a large number of ambulatory visits in which antibiotics were prescribed without a documented indication in this nationally representative survey. Antibiotic prescribing in the absence of a documented indication may severely bias national estimates of appropriate antibiotic use in this setting and misinform antimicrobial stewardship efforts. Our study identified several independent risk factors for antibiotic prescribing without a documented indication; these may be useful in directing initiatives aimed at improving documentation. With 60% of antibiotic expenditure and up to 90% of antibiotic use originating in ambulatory care settings,27 28 29 30 more focus is needed to support well informed stewardship efforts beyond the hospital.
What is already known on this topic
Previous studies have identified a high degree of unnecessary antibiotic prescribing in the ambulatory care setting as an important target for antibiotic stewardship
Studies examining the appropriateness of antibiotic prescribing rely on documentation of the indication for the antibiotic
Few studies to date have examined the proportion of antibiotic prescriptions that lack a documented indication
What this study adds
Of 130.5 million antibiotic prescriptions estimated by a nationally representative survey for 2015, 18% (approximately 24 million) lacked a documented indication
Being an adult male, having at least one chronic disease, spending more time with a provider, and seeing a non-primary care specialist were positively associated with prescribing without indication
Receipt of a prescription for sulfonamide or a urinary anti-infective was also associated with absence of a documented infection
Web extra.
Extra material supplied by authors
Appendix
Contributors: MJR and JCM designed the study. GBT and MRE assisted with data preparation and analysis. MJR analyzed and interpreted the data. JCM supervised the study. GBT and DTB provided clinical expertise. MJR drafted the manuscript. MJR, GBT, DTB, MRE, and JCM critically revised the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. MJR is the guarantor.
Funding: This was an unfunded project.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; JCM has received grants from Merck, Agency for Health Care Research and Quality (AHRQ), and Centers for Disease Control and Prevention (CDC) outside the submitted work; MRE has received grants from the AHRQ, CDC, Society for Infectious Diseases Pharmacists, and Oregon State University outside the submitted work; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Owing to the use of publicly available data, no institutional review board approval was necessary.
Data sharing: The data used in this study are publicly available from the US National Center for Health Statistics
Transparency: The lead author (the manuscript’s guarantor) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1. Schmidt ML, Spencer MD, Davidson LE. Patient, Provider, and Practice Characteristics Associated with Inappropriate Antimicrobial Prescribing in Ambulatory Practices. Infect Control Hosp Epidemiol 2018;39:307-15. 10.1017/ice.2017.263 [DOI] [PubMed] [Google Scholar]
- 2. Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991-1999. Ann Intern Med 2003;138:525-33. 10.7326/0003-4819-138-7-200304010-00008 [DOI] [PubMed] [Google Scholar]
- 3. Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA 1997;278:901-4. 10.1001/jama.1997.03550110039033 [DOI] [PubMed] [Google Scholar]
- 4. Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis 2001;33:757-62. 10.1086/322627 [DOI] [PubMed] [Google Scholar]
- 5. Havers FP, Hicks LA, Chung JR, et al. Outpatient Antibiotic Prescribing for Acute Respiratory Infections During Influenza Seasons. JAMA Netw Open 2018;1:e180243. 10.1001/jamanetworkopen.2018.0243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Suda KJ, Hicks LA, Roberts RM, Hunkler RJ, Taylor TH. Trends and seasonal variation in outpatient antibiotic prescription rates in the United States, 2006 to 2010. Antimicrob Agents Chemother 2014;58:2763-6. 10.1128/AAC.02239-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007-09. J Antimicrob Chemother 2014;69:234-40. 10.1093/jac/dkt301 [DOI] [PubMed] [Google Scholar]
- 8. Cantrell R, Young AF, Martin BC. Antibiotic prescribing in ambulatory care settings for adults with colds, upper respiratory tract infections, and bronchitis. Clin Ther 2002;24:170-82. 10.1016/S0149-2918(02)85013-5 [DOI] [PubMed] [Google Scholar]
- 9. Palms DL, Hicks LA, Bartoces M, et al. Comparison of antibiotic prescribing in retail clinics, urgent care centers, emergency departments, and traditional ambulatory care settings in the United States. JAMA Intern Med 2018;178:1267-9. 10.1001/jamainternmed.2018.1632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis 2015;60:1308-16. 10.1093/cid/civ076 [DOI] [PubMed] [Google Scholar]
- 11. Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA 2016;315:1864-73. 10.1001/jama.2016.4151 [DOI] [PubMed] [Google Scholar]
- 12. Chua K-P, Fischer MA, Linder JA. Appropriateness of outpatient antibiotic prescribing among privately insured US patients: ICD-10-CM based cross sectional study. BMJ 2019;364:k5092. 10.1136/bmj.k5092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dobson EL, Klepser ME, Pogue JM, et al. SIDP Community Pharmacy Antimicrobial Stewardship Task Force Outpatient antibiotic stewardship: Interventions and opportunities. J Am Pharm Assoc (2003) 2017;57:464-73. 10.1016/j.japh.2017.03.014 [DOI] [PubMed] [Google Scholar]
- 14. Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core elements of outpatient antibiotic stewardship. MMWR Recomm Rep 2016;65:1-12. 10.15585/mmwr.rr6506a1 [DOI] [PubMed] [Google Scholar]
- 15. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 2016;62:e51-77. 10.1093/cid/ciw118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. NAMCS micro-data file documentation: summary of changes for 2015. 2015. https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm.
- 17.Cerner Corporation. Multum Lexicon Plus. 2016. https://www.cerner.com/solutions/drug-database.
- 18. Ray MJ, Trick WE, Lin MY. Assessing the Ability of Hospital Diagnosis Codes to Detect Inpatient Exposure to Antibacterial Agents. Infect Control Hosp Epidemiol 2018;39:377-82. 10.1017/ice.2018.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGregor JC, Elman ME, Bearden DT. Antibiotic Prescribing in Ambulatory Setting without a Documented Indication. IDWeek 2012; San Diego, CA. [Google Scholar]
- 20. Magill SS, Edwards JR, Beldavs ZG, et al. Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team Prevalence of antimicrobial use in US acute care hospitals, May-September 2011. JAMA 2014;312:1438-46. 10.1001/jama.2014.12923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA. Estimating National Trends in Inpatient Antibiotic Use Among US Hospitals From 2006 to 2012. JAMA Intern Med 2016;176:1639-48. 10.1001/jamainternmed.2016.5651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA 2016;315:562-70. 10.1001/jama.2016.0275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Linder JA, Meeker D, Fox CR, et al. Effects of behavioral interventions on inappropriate antibiotic prescribing in primary care 12 months after stopping interventions. JAMA 2017;318:1391-2. 10.1001/jama.2017.11152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fleming-Dutra KE, King LM, Boghani S, et al. 969. Antibiotic Prescribing in a Large Retail Health Clinic Chain: Opportunities for Stewardship. Open Forum Infect Dis 2019;6(Suppl 2):S32-3 10.1093/ofid/ofz359.071. [DOI] [Google Scholar]
- 25. Martinez KA, Rood M, Jhangiani N, Boissy A, Rothberg MB. Antibiotic Prescribing for Respiratory Tract Infections and Encounter Length: An Observational Study of Telemedicine. Ann Intern Med 2019;170:275-7. 10.7326/M18-2042 [DOI] [PubMed] [Google Scholar]
- 26. Grigoryan L, Germanos G, Zoorob R, et al. Use of Antibiotics Without a Prescription in the U.S. Population: A Scoping Review. Ann Intern Med 2019;171:257-63. 10.7326/M19-0505 [DOI] [PubMed] [Google Scholar]
- 27. Suda KJ, Hicks LA, Roberts RM, Hunkler RJ, Danziger LH. A national evaluation of antibiotic expenditures by healthcare setting in the United States, 2009. J Antimicrob Chemother 2013;68:715-8. 10.1093/jac/dks445 [DOI] [PubMed] [Google Scholar]
- 28. Hawker JI, Smith S, Smith GE, et al. Trends in antibiotic prescribing in primary care for clinical syndromes subject to national recommendations to reduce antibiotic resistance, UK 1995-2011: analysis of a large database of primary care consultations. J Antimicrob Chemother 2014;69:3423-30. 10.1093/jac/dku291 [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Outpatient antibiotic prescriptions—United States, 2014. 2017. https://www.cdc.gov/antibiotic-use/community/programs-measurement/state-local-activities/outpatient-antibiotic-prescriptions-US-2014.html.
- 30. Duffy E, Ritchie S, Metcalfe S, Van Bakel B, Thomas MG. Antibacterials dispensed in the community comprise 85%-95% of total human antibacterial consumption. J Clin Pharm Ther 2018;43:59-64. 10.1111/jcpt.12610 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix