Abstract
Background
Mind-body approaches, particularly yoga, are used by cancer survivors to cope with treatment-related symptoms. Consistency of yoga-related effects on treatment-related symptoms are not known. This meta-analysis was designed to examine effects of yoga on pre- to postintervention improvements in fatigue among cancer patients.
Methods
PubMed and PsycINFO were searched for peer-reviewed articles of yoga randomized controlled trials including cancer survivors and reporting at least one fatigue measure. Twenty-nine studies met inclusion criteria (n = 1828 patients). Effect sizes (Hedge’s g) were calculated for fatigue, depression, and quality of life. Patient-related and intervention-related characteristics were tested as moderators of outcomes. All statistical tests were two-sided.
Results
Yoga practice was associated with a small, statistically significant decrease in fatigue (g = 0.45, P = .013). Yoga type was a statistically significant moderator of this relationship (P = .02). Yoga was associated with a moderate decrease in depression (g = 0.72, P = .007) but was not associated with statistically significant changes in quality of life (P = .48). Session length was a statistically significant moderator of the relationship between yoga and depression (P = .004). Neither timing of treatment (during treatment vs posttreatment) nor clinical characteristics were statistically significant moderators of the effects of yoga on outcomes. The effect of yoga on fatigue and depression was larger when the comparator was a “waitlist” or “usual care” than when the control group was another active treatment (P = .036).
Conclusions
Results suggest yoga may be beneficial as a component of treatment for both fatigue and depression in cancer survivors.
An estimated 1 735 350 new cases of cancer were diagnosed in the United States in 2018, and the population of long-term cancer survivors continues to increase (1). Approximately 15.5 million people in the United States in the year 2016 were classified as cancer survivors (2), defined by the National Cancer Institute as “one who remains alive and continues to function during and after overcoming a serious hardship or life-threatening disease. In cancer, a person is considered to be a survivor from the time of diagnosis until the end of life” (1). This is approximately 5% of the American population; the number of cancer survivors is expected to increase to 26.1 million by the year 2040 (2). As the prevalence of cancer survivors continues to increase and their survival time lengthens, clinicians and researchers have recognized the importance of addressing the side effects of treatment burden to improve quality of life.
The experience of a cancer diagnosis and its resulting treatments are associated with a wide range of physical and psychosocial changes such as fatigue, functional limitations, pain, cognitive changes, and psychological problems (3). Cancer-related fatigue (CRF) is a perceived state of reduction in mental and physical performance that is one of the most commonly reported symptoms accompanying cancer diagnosis and treatment (4–6). Approximately 40% of patients with malignant disease experience CRF at the time of diagnosis, and up to 90% of patients undergoing radiation or chemotherapy treatment experience CRF (5). For one-third of cancer survivors, fatigue persists after the conclusion of treatment for years (7); in breast cancer survivors, 34% report fatigue 5–10 years after treatment completion (8).
Many factors are thought to contribute to the development of CRF, including the direct effects of the disease, subsequent effects of cancer treatment, psychosocial factors, and comorbid physical symptoms (9). Psychosocial factors are strongly associated with CRF, particularly depressive symptoms (10), which may increase the risk for treatment-associated CRF, although the relationship between depression and CRF is more likely to be bi-directional (8). Recent evidence also suggests a relationship between inflammation and CRF, particularly long-term changes in the levels of circulating markers of proinflammatory cytokine activity (11). CRF is associated with elevated serum levels of proinflammatory cytokines that may persist up to 5 years after diagnosis. Increased CRF has also been associated with lower quality of life in several domains as well as increases in comorbid physical symptoms, such as sleep disturbance and pain (4).
In recent years, mind-body interventions are increasingly used by cancer survivors to aid in coping with these treatment-related symptoms, with yoga used most frequently (12). Originating in ancient Indian philosophy based in mindfulness and spiritual practice, yoga in Western society is most often practiced by performing physical exercises (asana), breathing exercises (pranayama), and meditation (dhyana) (13). Yoga is increasingly recommended as a holistic wellness approach in Western society (14). The National Center for Complementary and Integrative Health reports that current recommendations include yoga to treat specific medical conditions, such as cancer, and to maintain health and well-being (15). A range of yoga-based interventions for cancer survivors has been designed to reduce symptoms that are related to cancer or its treatment and impair quality of life, particularly fatigue. Different types of yoga have different modalities and foci, and require different levels of physical exertion.
Although, in general, studies show support for the effects of yoga-based interventions in reducing fatigue (16,17), some do not show a statistically significant benefit over treatment as usual (18). In addition, primary studies alone do not allow for analysis of the efficacy of specific components of the intervention design, such as length of the intervention, type of yoga practiced, and timing of the intervention regarding treatment. It may be that yoga-based interventions are effective in treating fatigue overall but that an intervention that is too long or begun too close to primary treatment may place additional burden on cancer survivors, negatively affecting treatment-related symptoms. A more comprehensive analysis of both intervention and clinical characteristics across cancer types can inform further development of yoga-based interventions in cancer populations.
Previous systematic reviews and meta-analyses have addressed the efficacy of yoga interventions primarily among Caucasian female breast cancer patients (19–22), who face a much better prognosis than patients with many other cancer types (23). Due to systematic variation across cancer types in recurrence, mortality rates, and treatment burden (24), uncertainty exists regarding the efficacy of yoga interventions in cancer types with higher rates of recurrence and mortality, such as ovarian or lung cancer. To our knowledge, only one other published meta-analysis has included nonbreast cancer survivors in their study search criteria (25). Although methodologically rigorous, that meta-analysis included 10 studies, with only four reporting fatigue outcomes. The current review comprehensively examines the evidence of yoga interventions associated with changes in fatigue, depressive symptoms, and quality of life across cancer types and explores specific patient and intervention characteristics that may be potential moderators of intervention effects. The current meta-analysis was intended to further build on the findings of prior systematic reviews by examining intervention-related and patient-related characteristics that may moderate the consistency of yoga-related effects. We conducted a comprehensive meta-analysis of randomized controlled trials examining the effects of yoga-based interventions on fatigue, depression, and quality of life across cancer populations. The specific aims were to 1) review the evidence of yoga interventions in treating fatigue, depressive symptoms, and poor quality of life in cancer survivors; 2) examine the efficacy of interventions for improving patient-reported outcomes, including fatigue, depression, and quality of life; and 3) identify components of efficacious interventions.
Methods
Inclusion/Exclusion Criteria
This study followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for systematic reviews. We included all randomized controlled trials of yoga-based interventions that examined effects on fatigue in adult patients diagnosed with any type of cancer in the current systematic review and meta-analysis. To capture the full range of cancer survivorship, the broadest definition of cancer survivor was deployed, allowing inclusion of individuals diagnosed with cancer of any stage and at any time in the treatment trajectory.
To qualify, interventions had to include either group-based or home-based yoga as the core component of the intervention. Studies were excluded for the following reasons: (1) not a published, peer-reviewed article, (2) not written in English, (3) data unavailable to compute standardized effect sizes, (4) no fatigue outcomes reported, (5) data already present in another included study, (6) no comparison group included (defined as no control group within the same population), (7) participants not limited to solely cancer survivors, (8) study quality score (as described below) less than 5.
Information Sources and Search Strategy
We searched two databases, PubMed and PsycInfo, from their inception until October 2018 without language restrictions for combinations of search terms related to yoga, cancer, and the relevant cancer survivorship outcomes (ie, fatigue). Citations from recent meta-analyses and systematic reviews were also reviewed.
Data Abstraction
All abstracts and articles identified during the literature search were coded independently by two different raters (J.S.A. and G.M.). Duplicate citations were first removed. Citations and abstracts were then screened by the authors for fulfillment of eligibility criteria. Any study that did not meet one or more criteria was excluded and assigned a reason for exclusion. The remaining full-text articles were then reviewed to assess eligibility. Standardized data entry spreadsheets were developed by the first author for coding both study-level and effect size data. The additional rater was trained by the first author through coding an initial sample of studies (n = 5), which was then compared for reliability. Inter-rater reliabilities were in the strong range (K = 0.84) (26). When sufficient data for computing standardized effect sizes were unavailable, study authors were contacted via email for additional data.
The following data were extracted: 1) bibliographic information (ie, author, year of publication, journal type); 2) study information (ie, primary and secondary outcomes, type of control group, follow-up timepoint(s), retention); 3) intervention information (ie, yoga type, duration and dose of intervention, setting and format of delivery); 4) participant characteristics (ie, age, sex, race, cancer type and stage, current treatment); 5) outcomes (ie, outcome measures used, hypothesized and observed findings); and 6) data required for effect size calculations.
Study Quality and Bias
A study quality score (0–10) was developed based on the Consolidated Standards of Reporting Trials statement for randomized controlled trials (27,28). One point was awarded for each criterion, including: 1) full description of randomization and concealment process; 2) baseline demographic and clinical characteristics reported separately for each study group; 3) acceptable participant attrition rate (≤20% for ≤6 months postbaseline; ≤30% for >6 months postbaseline); 4) assessor blinding; 5) defined and prespecified primary and secondary outcomes identified and measured with validated measures; 6) intention-to-treat analyses and appropriate approach to missing data; 7) potential confounders, including baseline levels of fatigue accounted for in analyses; 8) power calculation reported and trial adequately powered for the primary outcome; 9) use of validated behavioral measurements tools; and 10) summary results presented with between-group difference and precision estimates.
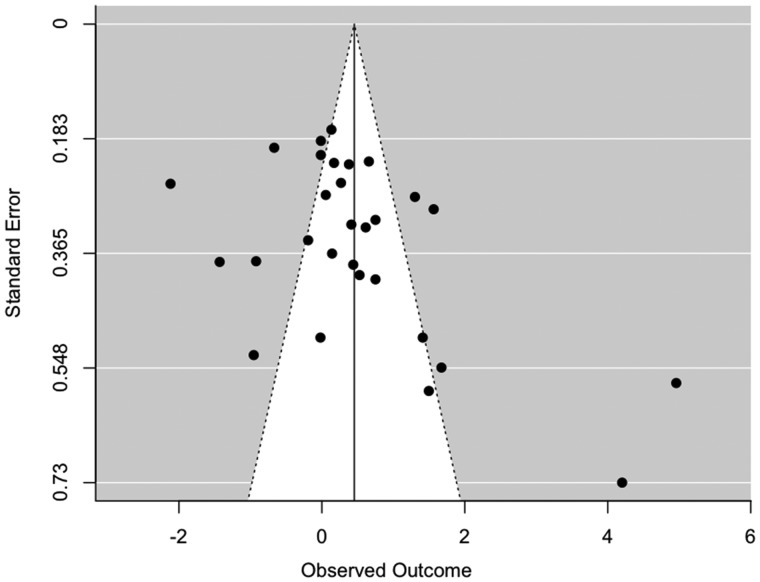
We also assessed publication bias by visually inspecting funnel plots for asymmetry within the model of interest then reestimating models using trim-and-fill methods accounting for asymmetric distribution of studies around an omnibus effect (29).
Statistical Analysis
Changes from preintervention assessment to postintervention assessment were obtained directly from the reported study results or calculated by determining the difference between the reported means before and after the intervention (using the first follow-up time-point after the end of the intervention). Study outcomes were analyzed using standardized mean differences (Hedges’ g) between outcomes for cancer patients receiving a yoga intervention (“yoga practice”) compared with cancer patients who did not, because this method helps reduce positive bias in small samples (30). A positive standardized mean difference indicates positive effects of the yoga intervention in reducing fatigue or depression when compared with the control group. For the purposes of our analyses, all effect sizes for studies where lower scores represent lower fatigue or depression were multiplied by −1 to reverse-code fatigue and depression scores and ensure a similarly coded metric across all included studies. For one study where the SDs were not available, a Cohen’s d was calculated using the t value of the difference between groups in fatigue (31) and then converted to a Hedges’ g using the J conversion value (30).
Analyses were conducted using the R statistical software (version 3.5.0) and the ‘metafor’ package (version 2.0–0) (29). The 95% confidence intervals are reported. Random effects models were used, assuming statistical heterogeneity between studies. Heterogeneity was explored by Cochrane’s Q test and I2, which may be interpreted as the proportion of the total between-study variation observed that is attributable to extant differences between studies rather than sampling error. A mixed-effects model was used to assess relevant moderators, including frequency of intervention, length of yoga session, and length of overall intervention. Studies without clear defining characteristics for a moderator (eg, studies that did not specify whether mindfulness was an intervention component) were excluded from that moderation analysis. In addition to the assessments of model heterogeneity described above, the R2 index is reported to describe the heterogeneity accounted for by each moderator. A P value of less than .05 was considered statistically significant and all tests were two-sided.
Results
Study Selection
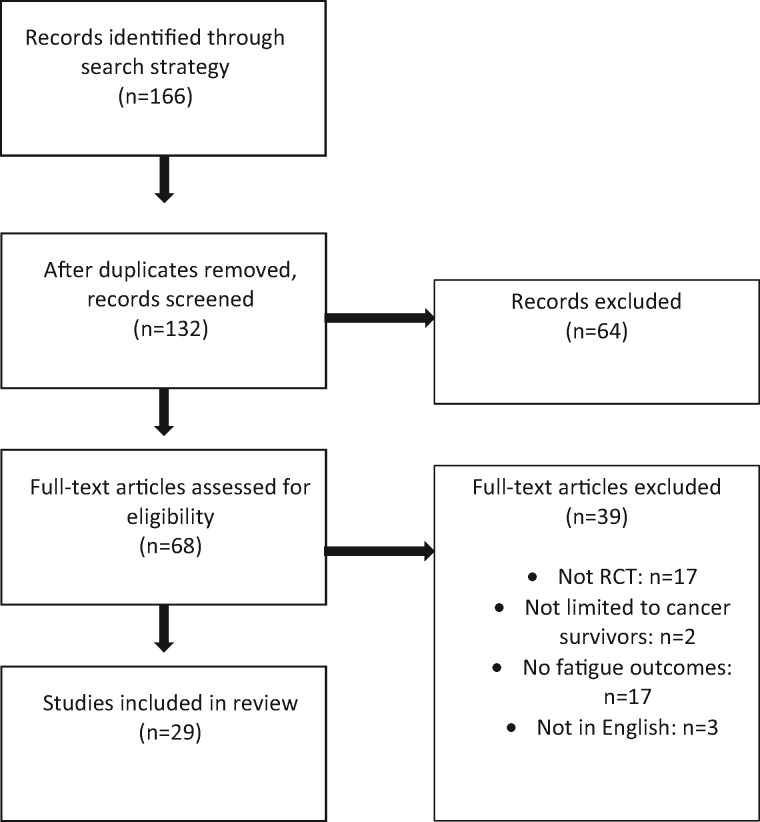
A total 156 citations were retrieved. After application of exclusion criteria, 29 studies met the inclusion criteria involving a total of 1828 participants (see Figure 1 for PRISMA flow diagram). Included studies were published between 2007 and 2018.
Figure 1.
PRISMA flow diagram of reviewed articles. RCT = randomized controlled trial.
Study and Participant Characteristics
The average age of participants was 55 years and 57% had some postsecondary education. Female breast cancer survivors accounted for 72% of the sample. The largest number of trials (17) was conducted in the United States (59%). Seven studies were conducted in Asia, four in Europe, and one in Australia. The largest proportion of studies used a waitlist comparison condition (41%). The average follow-up time posttreatment was 2.3 months (SD = 0.98, range = 1.5–6 months).
The median sample size was 62 randomly assigned participants per study (range = 15–200). A total 48% of studies included patients currently in primary cancer treatment. Twenty-four studies targeted only breast cancer survivors, two colorectal cancer, and one prostate cancer. The remaining two studies included multiple cancer types. All studies conducted in the United States reported race or ethnicity demographics, and the majority of the participants in these trials were made up of predominately Caucasian participants. However, two studies specifically targeted minority women (18,32). Six studies targeted early-stage cancer survivors, one late-stage cancer survivors, and the remaining 22 studies did not place restrictions on cancer stage at diagnosis. Overall, the majority of participants in these trials were middle-aged, Caucasian, identified as female, and were diagnosed with breast cancer. Twenty-one of the included studies have not been previously included in any published systematic review, with five of these newly included studies published within the last 2 years.
The average duration of the intervention was 2.3 months (SD = 0.95, range = 1–6 months). The average length of each yoga session was 77 minutes (SD = 24, range = 15–120 minutes), and the average number of sessions was 19.8 (SD = 20.2, range = 6–120). The intervention with the fewest sessions was a pranayama intervention consisting of four breathing techniques taught in six weekly classes. Eight studies identified as randomized controlled pilot or feasibility studies. Twelve studies used a waitlist control group, seven studies used a “treatment as usual” or standard care group, and 10 studies used an “active” control (supportive counseling, stretching, or exercise course). Seventeen studies incorporated mindfulness-based theory into the intervention material. A summary of the participant and intervention characteristics of each trial is provided in Table 1.
Table 1.
Summary of yoga trial study and participant characteristics*
| First author | Participants | Intervention | Design and outcomes |
|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
QoL = quality of life.
Synthesis of Results
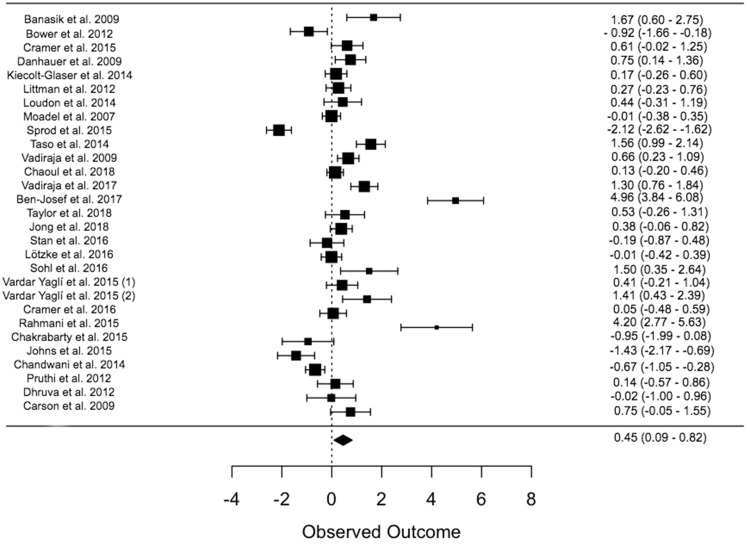
The outcome measures and calculated effect sizes with 95% confidence intervals for each study are listed in Table 2. Yoga practice was associated with a small but statistically significant decrease in fatigue from preintervention to the first follow-up when compared with a control group (n = 29, g = 0.45, 95% confidence interval [CI] = 0.09 to 0.82, P = .013; Figure 2). When active control groups (ie, exercise, stretching) were separated from waitlist control groups and usual care, control group type was a statistically significant moderator of both fatigue and depression outcomes, with yoga interventions performing better in both areas when compared with waitlist control and usual care but not when compared with active control (n = 29, Q[4] = 7.14, P = .0363). Statistically significant heterogeneity was present in this model (I2 = 90.87%, Q[28] = 306.71, P ≤ .0001), indicating a significant amount of between-studies variability in study outcomes. This heterogeneity suggests that our random-effects model is appropriate and that moderator analyses may help clarify generalizability of results.
Table 2.
A summary of the outcomes and effect sizes for yoga intervention trials*
| Study (year) | Follow-up, mo | Fatigue | QoL | Depression |
|---|---|---|---|---|
| Banasik et al. (2009) (16) | 2 | FACT-B Fatigue | FACT-B QoL | — |
| 1.67 (0.60 to 2.75) | 5.59 (4.66 to 6.52) | |||
| Ben-Josef et al. (2017) (33) | 2 | BFI | — | — |
| 4.96 (3.84 to 6.08) | ||||
| Bower et al. (2012) (34) | 3 | FSI | — | BDI-II |
| −0.92 (−1.66 to −0.18) | 0.73 (0.00 to 1.46) | |||
| Carson et al. (2009) (35) | 2 | Daily fatigue diary | — | Daily mood diary |
| 0.75 (−0.05 to 1.55) | 0.35 (−0.22 to 0.92) | |||
| Chakrabarty et al. (2015) (36) | 1.5 | CFS-F | — | — |
| 4.20 (2.77 to 5.63) | ||||
| Chandwani et al. (2014) (37) | 1.5 | BFI | SF-36 | CES-D |
| −0.67 (−1.05 to −0.28) | −17.18 (−17.70 to −16.67) | 3.45 (2.85 to 4.04) | ||
| Chaoul et al. (2018) (38) | 1 | BFI | — | — |
| 0.13 (0.07 to 1.46) | ||||
| Cramer et al. (2015) (39) | 3 | FACIT-F | FACT-B QoL | HADS-D |
| 0.61 (−0.20 to 0.46) | 5.85 (5.21 to 6.48) | 0.37 (−0.26 to 0.99) | ||
| Cramer et al. (2016) (40) | 2.5 | FACIT-F | FACT-C QoL | HADS-D |
| 0.68 (0.25 to 1.12) | 0.74 (0.20 to 1.28) | 0.39 (−0.15 to 0.93) | ||
| Danhauer et al. (2009) (41) | 2.5 | FACT-B | FACT-B | CES-D |
| 0.75 (0.14 to 1.36) | 7.71 (7.10 to 8.32) | 0.73 (0.12 to 1.34) | ||
| Dhruva et al. (2012) (42) | 1.5 | PFS | SF-12 | HADS-D |
| 0.02 (−1.00 to 0.96) | 0.43 (−0.56 to1.42) | −0.01 (−0.99 to 0.97) | ||
| Johns et al. (2015) (43) | 1.75 | FSI | — | PSQ-8 |
| −0.95 (−1.99 to 0.08) | −1.30 (−1.82 to −0.79) | |||
| Jong et al. (2018) (44) | 3 | MFI | — | HADS-D |
| 0.38 (−0.06 to 0.82) | 0.65 (0.21 to 1.10) | |||
| Kiecolt-Glaser et al. (2014) (17) | 3 | MFSI-SF | — | CES-D |
| 0.17 (−0.26 to 0.60) | 0.11 (−0.16 to 0.39) | |||
| Littman et al. (2012) (45) | 6 | FACIT-F | FACT-G QoL | — |
| −0.27 (−0.23 to 0.76) | 4.18 (3.68 to 4.68) | |||
| Lötzke et al. (2016) (46) | 3 | CFS-D | EORTC GHS | — |
| −0.01 (−0.42 to 0.39) | −0.33 (=0.74 to 0.07) | |||
| Loudon et al. (2014) (47) | 2 | 10 CM VAS | LYMQOL | — |
| 0.44 (−0.31 to 1.19) | 2.99 (2.25 to 3.73) | |||
| Moadel et al. (2007) (18) | 3 | FACIT-F | FACT-G QoL | — |
| −0.01 (−0.38 to0.35) | −0.41 (−0.77 to −0.04) | |||
| Pruthis et al. (2012) (48) | 3 | BFI | FACT-G | POMS-Dep |
| 0.14 (−0.57 to 0.86) | 1.07 (0.35 to 1.79) | 0.00 (−0.71 to 0.71) | ||
| Rahmani et al. (2015) (49) | 2 | EORTC C30 | EORTC GHS | — |
| 0.05 (−0.48 to 0.59) | 7.87 (6.97 to 8.78) | |||
| Sohl et al. (2016) (50) | 2 | FACT-C | FACT-C QoL | — |
| 1.50 (0.35 to 2.64) | 4.38 (3.26 to 5.50) | |||
| Sprod et al. (2015) (51) | 1 | MFSI-SF | — | — |
| −2.12 (−2.62 to−1.62) | ||||
| Stan et al. (2016) (52) | 3 | MFSI-SF | FACT-B QoL | — |
| −0.19 (−0.87 to 0.48) | −1.62 (−2.29 to −0.95) | |||
| Taso et al. (2014) (53) | 2 | BFI (Taiwanese) | — | — |
| 1.56 (0.99 to2.14) | ||||
| Taylor et al. (2018) (32) | 2 | BFI | — | CES-D |
| 0.53 (−0.26 to 1.31) | 0.81 (0.00 to 1.61) | |||
| Vadiraja et al. (2009) (54) | 1.5 | FSI | — | — |
| 0.66 (0.23 to 1.09) | ||||
| Vadiraja et al. (2017) (55) | 3 | FSI | — | — |
| 1.30 (0.76 to 1.84) | ||||
| Vardar-Yagli et al. (2015) (56)(1) | 1.5 | EORTC C30 | EORTC GHS | — |
| 0.41 (−0.21 to 1.04) | 4.05 (3.43 to 4.67) | |||
| Vardar-Yagli et al. (2015) (57) | 2 | 10 CM VAS | NOTTINGHAM | BDI |
| 1.41 (0.43 to 2.39) | −5.66 (−6.57 to −4.75) | 1.05 (0.12 to 1.99) |
BDI = Beck Depression Inventory; BFI = Brief Fatigue Inventory; CES-D = Center for Epidemiologic Studies Depression Scale; CFS = Chalder Fatigue Scale; CM VAS= centimeter Visual Analogue Scale; EORTC = European Organisation for Research and Treatment of Cancer; FACIT-F = Functional Assessment of Chronic Illness Therapy-Fatigue Scale; FACT-B = Functional Assessment of Cancer Therapy-Breast Cancer; FSI = Fatigue Symptom Inventory; GHS = Global Health Score; HADS-D = Hospital Anxiety and Depression Scale-Depression Subscale; LYMQOL = Lymphoedema Quality of Life Scale; MFSI = Multidimensional Fatigue Symptom Inventory; PFS = Piper Fatigue Scale; POMS-Dep = Profile of Mood States-Depression Subscale; PSQ-8 = Personal Health Questionnaire Depression Scale; QoL = quality of life; SF = Short Form Health Survey.
Figure 2.
Forest plot for fatigue effect sizes. RE = Random Effects.
Yoga type (coded physical poses vs nonphysical poses) was a statistically significant moderator of the relationship between yoga practice and fatigue; nonphysical yoga types, such as pranayama interventions, were still effective but less effective than physical yoga types (n = 29, Q[1] = 11.66, P = .022, I2 = 94.41%). Neither timing of treatment (during vs posttreatment) nor patient clinical characteristics were found to be statistically significant moderators of the effects of yoga practice on outcomes (n = 29, cancer type: P = .27, I2 = 99.79%; cancer stage dichotomized as late vs early: P = .78, I2 = 99.99%), although it is important to note that this may be due to a lack of power to detect moderation.
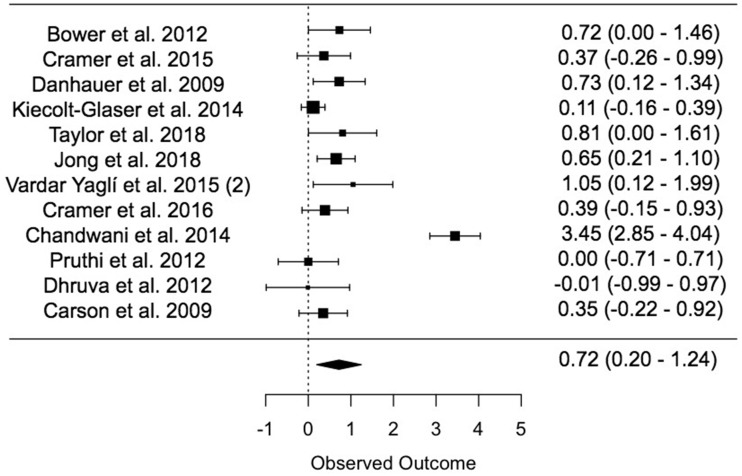
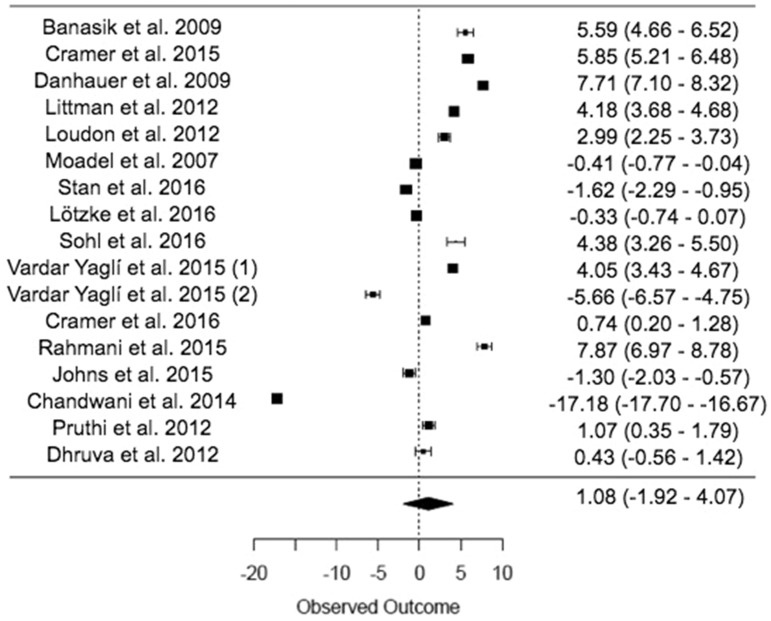
Yoga practice was associated with a moderate decrease in depression (n = 12, g = 0.72, 95% CI = 0.20 to 1.24, P = .007, I2 = 89.82%; Figure 3) but was not associated with statistically significant changes in quality of life (n = 17, P = .48, I2 = 99.75%; Figure 4). Statistically significant heterogeneity was present in both models (depression: Q[11] = 108.09; quality of life: Q[16] = 6361.84, both P < .0001). Session length was a statistically significant moderator of the relationship between yoga practice and depression with longer sessions associated with stronger effects (n = 12, Q[10] = 4.5182, P = .033, I2 = 84.08%).
Figure 3.
Forest plot for depression effect sizes. RE = Random Effects.
Figure 4.
Forest plot for quality of life effect sizes. RE = Random Effects.
Risk of Bias Across Studies
Asymmetric funnel plots suggested evidence for publication bias for several analyses, including examination of the primary outcome of fatigue (Figure 5). Asymmetry of findings revealed a lack of published studies with smaller sample sizes and negative or nonsignificant findings. In addition, asymmetric funnel plots suggested the presence of outlier effect sizes, particularly for fatigue. Trim-and-fill analyses resulted in modified effect size estimates (Table 3). However, notably, the statistical significance of all estimates remained unchanged. The direction of the quality-of-life analyses changed but remained nonsignificant, suggesting a large amount of variability present in published studies that may be largely influenced by outlier effect sizes.
Figure 5.
Publication bias funnel plot for fatigue outcomes.
Table 3.
Comparison of primary effect sizes with trim and fill analyses
| Variable | Primary effect size | Trim and fill effect size |
|---|---|---|
| Fatigue | g = 0.45; I2 = 90.87%, P = .013 | g = 0.43, I2 = 90.82%, P = .02 |
| Depression | g = 0.72; I2 = 89.92%, P = .007 | g = 1.071, I2 = 93.29%, P < .001 |
| QoL | g = 1.07, I2 = 99.75%, P = .48 | g = −1.5671, I2 = 99.77%, P = .27 |
g = Hedges' g effect size measure; I2 = percentage of variation across studies that is due to heterogeneity rather than chance; QoL = quality of life;
In addition, an examination of studies using intent-to-treat analyses was conducted as a more conservative estimate of yoga’s effects on fatigue, depression, and quality of life. Notably, although reduced, both the direction and statistical significance of estimated effect sizes for fatigue (n = 15, g = 0.24, 95% CI = 0.03 to 0.37, P = .044) and depression (n = 9, g = 0.39, 95% CI = 0.17 to 0.62, P = .0006) did not change when only studies using an intent-to-treat approach were included (n = 15). Yoga practice was not associated with a statistically significant effect on increasing quality of life. (n = 11, g= 2.46, 95% CI = −0.06 to 4.93, P = .055).
Clinical significance as estimated by pretreatment and posttreatment means in the yoga practice group showed that a clinical level of depression (identified as a score ≥16 on the CES-D measure) pretreatment (mean = 16.74) was reduced to a nonclinical level at posttreatment (mean = 9.55). Changes in fatigue scores on multiple scales (BFI, FACIT, FSI), while statistically significant, were not clinically significant as defined by an average change greater than three points from pre- to posttreatment.
Discussion
The purpose of this review was to examine effects of yoga randomized controlled trials on fatigue, depression, and quality of life in cancer survivors. Yoga-based interventions were shown to be generally effective when compared with waitlist, standard care, and active comparison conditions in the treatment of fatigue and depressive symptoms in cancer survivors. These effects were generally robust when publication bias and study quality were taken into account.
These results appear to roughly match the weighted mean effects in prior meta-analyses of the impact of yoga practice on depression in breast cancer survivors (20) and in heterogeneous cancer groups (25). The results of this review are in contrast to the findings of Lin et al. (2011), the most recent systematic review of yoga interventions in a heterogeneous group of cancer survivors; their findings suggest no statistically significant difference between yoga practice and comparison groups in the treatment of CRF. However, this may be due to the restricted number of studies measuring CRF included in their sample (N = 4).
Notably, depressive symptoms accounted for a large portion of the heterogeneity in the fatigue model (R2 = 36.32%). This is likely due to a persistent cluster of cancer-related symptoms that many patients continue to experience posttreatment, including both fatigue and mood disturbances as well as sleep problems and cognitive impairment (58). A multifactorial model is likely to explain the shared variance between posttreatment symptoms, including potential underlying factors such as increased systemic inflammation, DNA damage, and disruption to endocrine and circadian rhythms (59–61). In the context of yoga interventions, our results suggest that yoga practice acts in parallel on both depressive symptoms and fatigue, with shared variance between the two posttreatment symptoms contributing to difficulties in further exploring mechanisms underlying yoga’s efficacy. Although a few studies have explored associations between yoga practice and inflammation (17,62) or yoga practice and cortisol dysregulation (16) in the context of cancer, at present there are not enough studies to systematically analyze these effects. Future studies should include biological variables that may allow for systematic exploration of potential underlying factors (ie, inflammatory cytokines such as interleukin-6, salivary cortisol, blood sampling for single-cell gel electrophoresis, or detailed sleep sampling such as an actigraphy watch).
Our secondary aim was to assess specific patient and intervention characteristics that may be potential moderators of intervention effects. Our moderation results suggest specific components of interventions that are likely related to larger decreases in fatigue and depressive symptoms. Yoga type was associated with differences in fatigue reductions; while nonphysical yoga practices such as pranayama (breathing techniques) were effective in reducing fatigue, other more physical yoga types were associated with larger reductions in fatigue. Due to large heterogeneity between yoga postures and foci during practice between yoga types as well as a lack of published study protocol for many studies included in this meta-analysis, it is difficult to assess other common components of yoga types associated with increased effectiveness. Notably, inclusion of mindfulness was not associated with any significant change in effect size estimates for fatigue or depressive symptoms, suggesting that mindfulness may not be the sole effective component of yoga interventions. The length of the yoga session was associated with differences in the reduction of depressive symptoms, with longer sessions associated with greater reductions in depressive symptoms. It is notable that yoga was significantly more effective compared with “passive” control groups (ie, usual care and waitlist control) but equivalent to “active” control groups (ie, exercise and stretching). This may indicate a broader mechanism at work that is not limited to yoga alone, such as the overall benefits of physical activity in potentially reducing inflammation (63) or the possibility that yoga acts as a component of the larger mechanism of behavioral activation, where patients improve by increasing pleasant activities and positive interactions with their environment (64,65).
This review has several limitations. At the conceptual level, this review is limited in scope because fatigue, quality of life, and depression were the only outcomes included. Although sleep problems and cognitive impairment may also be affected by yoga practice due to their presence in the posttreatment symptom cluster affecting many cancer patients, these three outcomes were selected because they were the most likely to be reported in the available literature and across the widest variety of cancer populations. Although there are too few studies at present to conduct a meta-analysis, findings from a recent study do suggest that yoga practice is associated with both decreases in sleep disruption and improvements in memory in cancer patients (66).
In addition, construct validity is an important limitation to our findings due to the overlapping variance between fatigue and depressive symptoms as a result of those outcomes being part of a larger, overlapping cluster of posttreatment symptoms. Fatigue (ie, loss of energy) is often one potential diagnostic criterion for major depressive disorder, and all results should be interpreted with this limitation in mind. The search strategy included only articles published in English in peer-reviewed journals. It is likely that there are other studies published in other languages or not published due to null findings that may have contributed to knowledge of yoga interventions in cancer survivors. Additionally, asymmetry of findings revealed a lack of published studies with smaller sample sizes and negative or nonsignificant findings. This is particularly concerning considering the large number of pilot trials in this area of research and is strong evidence of publication bias. Asymmetric funnel plots suggested the presence of outlier effect sizes, particularly for fatigue. These large, positive effect sizes from studies with smaller sample sizes and greater standard error may be disproportionately influencing conclusions about the overall effects of yoga, and these conclusions should be made with caution. Efforts were made to obtain publications related to the studies included in this analysis, such as published study protocols and secondary analyses such as longitudinal follow-ups. However, most studies did not have additional resources available. It is important for future research in this area to incorporate both specific and standardized reporting methods that describe specific intervention components, particularly specific components of yoga poses. Additionally, despite efforts to include other cancer types, many available studies included primarily female breast cancer survivors from higher socioeconomic backgrounds; it is important for future research to be inclusive of the wide variety of cancer diagnoses and individuals present in the overall population of cancer survivors. Finally, the median sample size of these studies is small (N = 62), suggesting the need for larger randomized controlled trials in this area of research, particularly trials that include long-term follow-up to assess potential sustained effects of yoga interventions in this population.
Despite the limitations of this review, it is evident that yoga interventions demonstrate promise for effectively reducing fatigue and depressive symptoms in cancer patients. Although the current findings demonstrate the efficacy of yoga interventions in randomized controlled trials, these interventions have not yet been implemented into standard survivorship care. Future research should focus on both methods of promoting reductions in CRF and depressive symptoms and methods of making these interventions sustainable. Many of the interventions described in this review are not typically covered or reimbursed by health insurance. Dissemination of mind-body interventions with a focus on developing multidisciplinary teams within oncology as well as utilizing community resources are important next steps for this research.
In conclusion, our meta-analysis of published, randomized controlled trials showed that yoga interventions improved CRF and symptoms of depression in cancer survivors. Our moderation results suggest specific components of interventions that are related to larger decreases in these areas; specific yoga types are associated with greater decreases in CRF, and longer session length is associated with greater decreases in depressive symptoms. Given the large amount of variability both seen across these studies and present in the growing population of cancer survivors, much work is still needed to better understand what aspects of these interventions are most effective across different cancer diagnoses as well as what mechanisms may underlie similar reductions across symptoms in the same symptom cluster.
Funding
This work was supported by the National Institutes of Health (R01CA193249 and T32GM108540 to SKL).
Notes
Affiliations of authors: Department of Psychological & Brain Sciences (JSA and SKL), Gynecologic Oncology, Obstetrics & Gynecology (SKL), Holden Comprehensive Cancer Center (SKL), and Department of Urology (SKL), University of Iowa, Iowa City, IA.
The funder had no role in the design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
The authors declare no potential conflicts of interest.
References
- 1. Siegel RL, Miller KD, Jemal A.. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7. [DOI] [PubMed] [Google Scholar]
- 2. Bluethmann SM, Mariotto AB, Rowland JH.. Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25(7):1029–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hewitt M, Rowland JH, Yancik R.. Cancer survivors in the United States: age, health, and disability. J Gerontol Ser A Biol Sci Med Sci. 2003;58(1):M82–M91. [DOI] [PubMed] [Google Scholar]
- 4. Byar KL, Berger AM, Bakken SL, Cetak MA.. Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life. Oncol Nurs Forum. 2006;33(1):E18–E26. [DOI] [PubMed] [Google Scholar]
- 5. Hoffman AJ, Given BA, von Eye A, Gift AG, Given CW.. Relationships among pain, fatigue, insomnia, and gender in persons with lung cancer. Oncol Nurs Forum. 2007;34(4):785–792. [DOI] [PubMed] [Google Scholar]
- 6. Servaes P, Verhagen C, Bleijenberg G.. Fatigue in cancer patients during and after treatment: prevalence, correlates and interventions. Eur J Cancer. 2002;38(1):27–43. [DOI] [PubMed] [Google Scholar]
- 7. Schwartz AL. Daily fatigue patterns and effect of exercise in women with breast cancer. Cancer Pract. 2000;8(1):16. [DOI] [PubMed] [Google Scholar]
- 8. Bower JE, Ganz PA, Desmond KA, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106(4):751. [DOI] [PubMed] [Google Scholar]
- 9. Wagner LI, Cella D.. Fatigue and cancer: causes, prevalence and treatment approaches. Br J Cancer. 2004;91(5):822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jacobsen PB, Weitzner MA.. Evaluating the relationship of fatigue to depression and anxiety in cancer patients. In: Portenoy RK, Bruera E, eds. Issues in Palliative Care Research; Oxford, United Kingdom: Oxford University Press; 2011. [Google Scholar]
- 11. Collado-Hidalgo A, Bower JE, Ganz PA, Cole SW, Irwin MR.. Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin Cancer Res. 2006;12(9):2759–2766. [DOI] [PubMed] [Google Scholar]
- 12. Fouladbakhsh JM, Stommel M.. Gender, symptom experience, and use of complementary and alternative medicine practices among cancer survivors in the U.S. cancer population. Oncol Nurs Forum. 2010;37(1):E7–E15. [DOI] [PubMed] [Google Scholar]
- 13. Feuerstein G. The Yoga Tradition: Its History, Literature, Philosophy and Practice Chino Valley, AZ: Hohm Press; 2013.
- 14. Jeter PE, Slutsky J, Singh N, Khalsa S.. Yoga as a therapeutic intervention: a bibliometric analysis of published research studies from 1967 to 2013. J Altern Complement Med. 2015;21(10):586–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Birdee GS, Legedza AT, Saper RB, Bertisch SM, Eisenberg DM, Phillips RS.. Characteristics of yoga users: results of a national survey. J Gen Intern Med. 2008;23(10):1653–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Banasik J, Williams H, Haberman M, Blank SE, Bendel R.. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23(3):135–142. [DOI] [PubMed] [Google Scholar]
- 17. Kiecolt-Glaser JK, Bennett JM, Andridge R, et al. Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2014;32(10):1040–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moadel AB, Shah C, Wylie-Rosett J, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: effects on quality of life. J Clin Oncol. 2007;25(28):4387–4395. [DOI] [PubMed] [Google Scholar]
- 19. Buffart LM, van Uffelen JGZ, Riphagen II, et al. Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 2012;12(1):559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cramer H, Lange S, Klose P, Paul A, Dobos G.. Yoga for breast cancer patients and survivors: a systematic review and meta-analysis. BMC Cancer. 2012;12(1):412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harder H, Parlour L, Jenkins V.. Randomised controlled trials of yoga interventions for women with breast cancer: a systematic literature review. Support Care Cancer. 2012;20(12):3055–3064. [DOI] [PubMed] [Google Scholar]
- 22. Sadja J, Mills PJ.. Effects of yoga interventions on fatigue in cancer patients and survivors: a systematic review of randomized controlled trials. Explore (NY). 2013;9(4):232–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Quaresma M, Coleman MP, Rachet B.. 40-year trends in an index of survival for all cancers combined and survival adjusted for age and sex for each cancer in England and Wales, 1971-2011: a population-based study. Lancet. 2015;385(9974):1206–1218. [DOI] [PubMed] [Google Scholar]
- 24. Society AC. Cancer Facts and Figures Atlanta, GA: American Cancer Society; 2018.
- 25. Lin K-Y, Hu Y-T, Chang K-J, Lin H-F, Tsauo J-Y.. Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. Evid Based Complement Alternat Med. 2011;2011:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22(3):276. [PMC free article] [PubMed] [Google Scholar]
- 27. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement (Chinese edition). J Chinese Integr Med. 2009;7(9):889–896. [PMC free article] [PubMed] [Google Scholar]
- 28. Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials (Chinese version). J Chinese Integr Med. 2010;8(7):604–612. [DOI] [PubMed] [Google Scholar]
- 29. Viechtbauer W. Conducting meta-analyses in R with the metafor Package. J Stat Softw. 2010;36(3):1–48. [Google Scholar]
- 30. Hedges LV, Olkin I.. Statistical Methodology in Meta-Analysis Princeton, NJ: Educational Testing Service; 1985.
- 31. Rosnow RL, Rosenthal R. Assessing the effect size of outcome research. In: Nezu AM, Nezu CM, eds. Evidence-Based Outcome Research: A Practical Guide to Conducting randomized Control Trials Psychosocial Interventions Oxford, United Kingdom: Oxford University Press; 2008.
- 32. Taylor TR, Barrow J, Makambi K, et al. A restorative yoga intervention for African-American breast cancer survivors: a pilot study. J Racial Ethn Heal Disparities. 2018;5(1):62–72. [DOI] [PubMed] [Google Scholar]
- 33. Ben-Josef AM, Chen J, Wileyto P, et al. Effect of Eischens yoga during radiation therapy on prostate cancer patient symptoms and quality of life: a randomized phase II trial. Int J Radiat Oncol Biol Phys. 2017;98(5):1036–1044. [DOI] [PubMed] [Google Scholar]
- 34. Bower JE, Garet D, Sternlieb B, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer. 2012;118(15):3766–3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Carson JW, Carson KM, Porter LS, Keefe FJ, Seewaldt VL.. Yoga of Awareness program for menopausal symptoms in breast cancer survivors: results from a randomized trial. Support Care Cancer. 2009;17(10):1301–1309. [DOI] [PubMed] [Google Scholar]
- 36. Chakrabarty J, Vidyasagar M, Fernandes D, Joisa G, Varghese P, Mayya S.. Effectiveness of pranayama on cancer-related fatigue in breast cancer patients undergoing radiation therapy: a randomized controlled trial. Int J Yoga. 2015;8(1):47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chandwani KD, Perkins G, Nagendra HR, et al. Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy. J Clin Oncol. 2014;32(10):1058–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chaoul A, Milbury K, Spelman A, et al. Randomized trial of Tibetan yoga in patients with breast cancer undergoing chemotherapy. Cancer. 2018;124(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cramer H, Rabsilber S, Lauche R, Kümmel S, Dobos G.. Yoga and meditation for menopausal symptoms in breast cancer survivors-a randomized controlled trial. Cancer. 2015;121(13):2175–2184. [DOI] [PubMed] [Google Scholar]
- 40. Cramer H, Pokhrel B, Fester C, et al. A randomized controlled bicenter trial of yoga for patients with colorectal cancer. Psychooncology. 2016;25(4):412–420. [DOI] [PubMed] [Google Scholar]
- 41. Danhauer SC, Mihalko SL, Russell GB, et al. Restorative yoga for women with breast cancer: findings from a randomized pilot study. Psychooncology. 2009;18(4):360–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Dhruva A, Abrams D, Hecht FM, et al. Yoga breathing for cancer chemotherapy–associated symptoms and quality of life: results of a pilot randomized controlled trial. J Altern Complement Med. 2012;18(5):473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Johns SA, Brown LF, Beck-Coon K, Monahan PO, Tong Y, Kroenke K.. Randomized controlled pilot study of mindfulness-based stress reduction for persistently fatigued cancer survivors. Psychooncology. 2015;24(8):885–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jong MC, Boers I, Schouten van der Velden AP, et al. A randomized study of yoga for fatigue and quality of life in women with breast cancer undergoing (neo) adjuvant chemotherapy. J Altern Complement Med. 2018;24(9-10):942–953. [DOI] [PubMed] [Google Scholar]
- 45. Littman AJ, Bertram LC, Ceballos R, et al. Randomized controlled pilot trial of yoga in overweight and obese breast cancer survivors: effects on quality of life and anthropometric measures. Support Care Cancer. 2012;20(2):267–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lötzke D, Wiedemann F, Rodrigues Recchia D, et al. Iyengar-yoga compared to exercise as a therapeutic intervention during (neo)adjuvant therapy in women with stage I-III breast cancer: health-related quality of life, mindfulness, spirituality, life satisfaction, and cancer-related fatigue. Evidence-Based Complement Altern Med. 2016;2016:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Loudon A, Barnett T, Piller N, Immink MA, Williams AD.. Yoga management of breast cancer-related lymphoedema: a randomised controlled pilot-trial. BMC Complement Altern Med. 2014;14(1):214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pruthi S, Stan DL, Jenkins SM, et al. A randomized controlled pilot study assessing feasibility and impact of yoga practice on quality of life, mood, and perceived stress in women with newly diagnosed breast cancer. Glob Adv Heal Med. 2012;1(5):30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rahmani S, Talepasand S.. The effect of group mindfulness-based stress reduction program and conscious yoga on the fatigue severity and global and specific life quality in women with breast cancer. Med J Islam Repub Iran. 2015;29:175. [PMC free article] [PubMed] [Google Scholar]
- 50. Sohl SJ, Danhauer SC, Birdee GS, et al. A brief yoga intervention implemented during chemotherapy: a randomized controlled pilot study. Complement Ther Med. 2016;25:139–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sprod LK, Fernandez ID, Janelsins MC, et al. Effects of yoga on cancer-related fatigue and global side-effect burden in older cancer survivors. J Geriatr Oncol. 2015;6(1):8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Stan DL, Croghan KA, Croghan IT, et al. Randomized pilot trial of yoga versus strengthening exercises in breast cancer survivors with cancer-related fatigue. Support Care Cancer. 2016;24(9):4005. [DOI] [PubMed] [Google Scholar]
- 53. Taso C-J, Lin H-S, Lin W-L, Chen S-M, Huang W-T, Chen S-W.. The effect of yoga exercise on improving depression, anxiety, and fatigue in women with breast cancer: a randomized controlled trial. J Nurs Res. 2014;22(3):155–164. [DOI] [PubMed] [Google Scholar]
- 54. Vadiraja SH, Rao MR, Nagendra RH, et al. Effects of yoga on symptom management in breast cancer patients: a randomized controlled trial. Int J Yoga. 2009;2(2):73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Vadiraja HS, Rao RM, Nagarathna R, et al. Effects of yoga in managing fatigue in breast cancer patients: a randomized controlled trial. Indian J Palliat Care. 2017:23(3):247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yaʇli VN, Çener G, Arikan H, et al. Do yoga and aerobic exercise training have impact on functional capacity, fatigue, peripheral muscle strength, and quality of life in breast cancer survivors? Integr Cancer Ther. 2015:14(2):125–132. [DOI] [PubMed] [Google Scholar]
- 57. Yagli NV, Ulger O.. The effects of yoga on the quality of life and depression in elderly breast cancer patients. Complement Ther Clin Pract. 2015;21(1):7–10. [DOI] [PubMed] [Google Scholar]
- 58. Bower JE. Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol. 2008;26(5):768–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rich TA. Symptom clusters in cancer patients and their relation to EGFR ligand modulation of the circadian axis. J Support Oncol. 2007;5(4):167–174. [PubMed] [Google Scholar]
- 60. Habbal OA, Al-Jabri AA.. Circadian rhythm and the immune response: a review. Int Rev Immunol. 2009;1–2:93–108. [DOI] [PubMed] [Google Scholar]
- 61. Cermakian N, Lange T, Golombek D, et al. Crosstalk between the circadian clock circuitry and the immune system. Chronobiol Int. 2013;30(7):870–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bower JE, Greendale G, Crosswell AD, et al. Yoga reduces inflammatory signaling in fatigued breast cancer survivors: a randomized controlled trial. Psychoneuroendocrinology. 2014;43:20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ford ES. Does exercise reduce inflammation? Physical activity and C-reactive protein among U.S. adults. Epidemiology. 2002;13(5):561. [DOI] [PubMed] [Google Scholar]
- 64. Cuijpers P, van Straten A, Warmerdam L.. Behavioral activation treatments of depression: a meta-analysis. Clin Psychol Rev. 2007;27(3):318–326. [DOI] [PubMed] [Google Scholar]
- 65. Dimidjian S, Hollon SD, Dobson KS, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74(4):658–670. [DOI] [PubMed] [Google Scholar]
- 66. Janelsins MC, Peppone LJ, Heckler CE, et al. YOCAS©® yoga reduces self-reported memory difficulty in cancer survivors in a nationwide randomized clinical trial: investigating relationships between memory and sleep. Integr Cancer Ther. 2016;15(3):263–271. [DOI] [PMC free article] [PubMed] [Google Scholar]