Abstract
Background
Cell salvage has recently been recommended for obstetric use in cases with a high risk of massive hemorrhage during cesarean section (CS). However, limited data are available to support the use of one suction device to collect lost blood. This study aimed to investigate the volume of red blood cells (RBCs) salvaged and the components of amniotic fluid (AF) in blood salvaged by one suction device or two devices during CS in patients with placenta previa and/or accrete.
Methods
Thirty patients with placenta previa and/or accrete undergoing elective CS in the Women's Hospital of Zhejiang University School of Medicine were recruited for the present study from November 1, 2017 to December 1, 2018. The patients were randomly assigned to one of the two groups according to an Excel-generated random number sheet: Group 1 (n = 15), in which only one suction device was used to aspirate all blood and AF, and Group 2 (n = 15), in which a second suction device was mainly used to aspirate AF before the delivery of the placenta. Three samples of blood per patient (pre-wash, post-wash, and post-filtration) were collected to measure AF components. The salvaged RBC volumes were recorded. Continuous data of pre-wash, post-wash, and post-filtration samples were analyzed by using one-way analysis of variance with Tukey's test for multiple comparisons, or Kruskal-Wallis test with Dunn test for multiple comparisons. Comparisons of continuous data between Group 1 and Group 2 were conducted using Student's t test or Mann-Whitney U test.
Results
The salvaged RBC volume was significantly higher in Group 1 than that in Group 2 (401.6 ± 77.2 mL vs. 330.1 ± 53.3 mL, t = 4.175, P < 0.001). In both groups, squamous cells, lamellar bodies, and fat were significantly reduced by washing (all P<0.001) and squamous cells were further reduced by filtering (P < 0.001). Squamous cells were found in six post-filtration samples (three from each group). Lamellar bodies and fat were completely removed by filtering. Insulin-like growth factor binding protein 1, alpha-fetoprotein, albumin, lactate dehydrogenase, and potassium were significantly reduced post-wash (all P < 0.05), with no further significant reduction after filtration in either group (all P > 0.05). The mean percentage of fetal RBCs post-filtration was (1.8 ± 0.8)% with a range of 1.0% to 3.5% and (1.9 ± 0.9)% with a range of 0.7% to 4.0% in Groups 1 and 2, respectively, showing no significant difference between the two groups (U = 188.5, P = 0.651).
Conclusion
Cell salvage performed by one suction device could result in higher volume of salvaged RBCs and can be used safely for CS in patients with placenta previa and/or accrete when massive hemorrhage occurs.
Trial registration number
ChiCTR-INR-17012926, http://www.chictr.org.cn/ Chinese Clinical Trial Registry.
Keywords: Cell salvage, Blood transfusion, Placenta previa, Placenta accrete, Cesarean section
Introduction
Obstetric hemorrhage remains a leading cause of maternal death.[1,2] During the past two decades, intra-operative cell salvage (IOCS) has been routinely practiced in many types of surgical operations to reduce the need for allogeneic blood transfusion and to avoid its related risks.[3–5] However, the safety of IOCS in obstetrics has been questioned due to the perceived risk of contamination of the salvaged blood with amniotic fluid (AF) and the risk of maternal alloimmunization.[6–10] A number of studies to date have demonstrated that AF contaminants were almost completely removed by a washing process combined with a leucodepletion filter, and serious complications have not been reported.[10–17] The use of IOCS has been advocated for use in cesarean section (CS) where massive bleeding is expected, such as in the presence of abnormal placentation.[18–20]
It is standard practice to use two suction devices and to aspirate AF and blood before the delivery of the placenta.[6,10–14] In cases of placenta previa, cesarean section is sometimes conducted through a placental incision, and massive hemorrhage usually occurs before the delivery of the placenta. One suction device was previously shown to be safe for use in CS, as its use allowed AF contaminants, including squamous cells and alpha-fetoprotein (AFP), to be effectively removed.[13,21] However, data on whether IOCS utilizing one suction device can reduce blood waste and improve the collected red blood cell (RBC) volume during CS for placenta previa and/or accrete are still limited.
The aim of this study was to compare IOCS utilizing one suction device to that utilizing two suction devices during CS for placenta previa and/or accrete and to determine whether one suction device could safely improve post-wash RBC volume without increasing the risk of AF embolization and alloimmunization. We measured AF components and RBC volume following the use of one and two suction devices.
Methods
Ethical approval
This study was approved by the Ethical Committee of the Women's Hospital of Zhejiang University School of Medicine (No. 20150105) and registered at ChineseClinicalTrials.gov (No. ChiCTR-INR-17012926). Written informed consent was obtained from all the patients.
Study population
The current study was performed in the Women's Hospital, Zhejiang University School of Medicine, from November 1, 2017 to December 1, 2018. The sample size was determined based on the results of our preliminary study, which showed salvaged RBC volumes to be 380 ± 30 mL in the one suction device group and 320 ± 40 mL in the two suction device group. Calculated with independent samples t tests using PASS® (version 11.0.7 Windows, NCSS, LLC., Kaysville, UT, USA), a sample size of 24 in total (12 patients per group) would have 90% power to detect a difference between the two groups with a significance level of 0.05. We decided to enroll a total of 30 patients (15 patients per group) in the present study to allow for possible dropout. Therefore, a total of 30 patients with an American Society of Anesthesiologists physical status 2 who had placenta previa and/or accrete at 35 to 38 weeks of gestation and selected to undergo CS were enrolled in this study. Patients with infection, fever, diabetes or gestational diabetes, severe pre-eclampsia, significant coexisting maternal diseases such as cardiac disease or coagulopathy and those who refused to receive cell salvaged blood were excluded.
Study design and IOCS procedure
Before the commencement of the study, 30 randomization codes were computer generated by a random number generator in Excel. The code for each patient was placed into a consecutively numbered envelope by a research nurse who did not participate in the study. An anesthesiologist opened the envelope before the surgery and assigned the patient to one of two groups: Group 1 (n = 15), using only one suction device to aspirate all blood and AF or Group 2 (n = 15), which employed a second suction device to aspirate as much blood and AF as possible before the delivery of the placenta.
A common iliac artery or internal iliac artery balloon was implanted before the patient arrived in the operating room. After arrival in the operating room, a 16-gauge peripheral venous cannula, a double lumen internal jugular vein cannula, and a 20-gauge radial artery cannula were inserted. Electrocardiography, pulse oximetry, and invasive blood pressure were monitored for all patients. All patients received a spinal anesthetic using 3 mL of 0.5% hyperbaric ropivacaine.
Using an aspiration unit (Cooker, Queensland, Australia), lost blood was suctioned into a cell salvage reservoir. Suction pressure was set at 100 to 150 mmHg. Aspirated blood was mixed with heparin (30,000 IU per liter of saline).
The collected blood was processed when the anesthetist or the surgeon estimated the blood loss to be more than 500 mL and sufficient blood had been collected in the reservoir. Using the quality wash program, the collected blood was washed by a Continuous Autotransfusion System (Fresenius Kabi AG, Bad Homburg, Germany). The washed blood was then run through a leucocyte depletion filter (LeukoGuard RS, Pall Biomedical Products Co., East Hills, NY, USA) under gravity.
A sample of the blood from the cell salvage reservoir (pre-wash sample), washed blood pack (post-wash sample), and filtered blood from the reinfusion pack (post-filtration sample) was taken for testing.
Blood sample assay
The following assays were made for each blood sample (pre-wash, post-wash, and post-filtration):
-
(1)
According to one previous study,[12] 5 mL of blood was added to CytoLyt solution (Cytyc Corporation, West Sussex, UK) to assess squamous cells. After centrifugation at 1200 × g for 5 min, the supernatant was discarded. The cell bullet was then resuspended in PreservCyt (Cytyc Corporation) and processed on a ThinPrep 2000 Processor (Cytyc Corporation). One alcohol-fixed slide per sample was generated. The slides were stained by using the Papanicolaou technique. A pathologist blinded to the sample counted the squamous cells under light microscopy. Counts were performed when squamous cells were present, with ten consecutive high-magnification fields counted. Counts were repeated three times and then averaged.
-
(2)
Two milliliters of blood was injected into a sample tube containing ethylene diamine tetraacetic acid (EDTA) and placed in an envelope to avoid light degradation of the lamellar bodies. Lamellar body count was performed using a platelet channel on the Sysmex XE-2100 hematological analyzer (Sysmex, Kobe, Japan).
-
(3)
Five milliliters of blood was taken to measure fat. After centrifuging the blood at 1200 × g for 5 min, the supernatant was taken to count the number of fat particles. Each slide was examined for the presence of fat under light microscopy by a pathologist who did not know the origin of the sample. Counts were performed when fat particles were present. Fat particles from ten consecutive high-magnification fields were counted; the counts were repeated three times and then averaged.
-
(4)
Five milliliters of blood was transferred to endotoxin-free heparin tubes to measure the concentration of insulin-like growth factor binding protein 1 (IGFBP1). The blood was centrifuged at 1500 × g for 10 min at room temperature, and the supernatant was stored at −70°C until analysis. The serum concentrations of IGFBP1 were measured using enzyme-linked immunosorbent assay kit (Abnova, Taipei, Taiwan, China).
-
(5)
Two milliliters of blood was transferred to endotoxin-free heparin tubes to measure the concentration of AFP. Blood was centrifuged at 1500 × g for 10 min at room temperature, and the supernatant was stored at −70°C until analysis. The serum concentrations of AFP were measured using automatic electrochemiluminescence immunoassay analyzer Roche E170 (Roche, Mannheim, Germany).
-
(6)
Five milliliters of blood was transferred to endotoxin-free heparin tubes to measure the concentrations of albumin, lactate dehydrogenase (LDH), and potassium by using an automatic biochemical analyzer AU680 (Beckman Coulter lnc, Tokyo, Japan).
-
(7)
Five milliliters of blood was injected into a sample tube containing EDTA for quantitative fetal hemoglobin by using the Kleihauer-Betke test with a HemoCue® Plasma/Low Hb System (HemoCue Ltd, Derbyshire, UK).
Statistical analysis
Statistical analysis was performed with the SPSS 17.0 software package (SPSS Inc., Chicago, IL, USA). The Kolmogorov-Smirnov test was used to evaluate normality of distribution for continuous data. The data with normal distribution were presented as mean ± standard deviation and those with abnormal distribution were shown as median (Q1, Q3). For comparisons of continuous data between the pre-wash, post-wash, and post-filtration samples, those with a normal distribution were analyzed by using one-way analysis of variance followed by Tukey's test, and those with a non-normal distribution were analyzed by using the Kruskal-Wallis test followed by Dunn test. For comparisons of continuous data between Group 1 and 2, Student's t test and Mann-Whitney U test were used as appropriate. A P < 0.05 was considered statistically significant.
Results
Patient characteristics
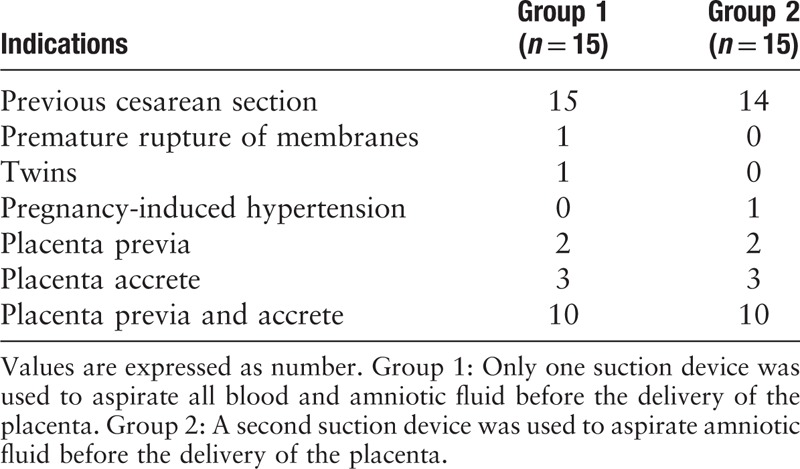
Thirty patients were enrolled in this study. In Group 1, the mean age of the patients was 34.3 ± 3.5 years, and the mean weight was 74.1 ± 4.1 kg. The mean age in Group 2 was 34.5 ± 3.8 years, and the mean weight was 73.9 ± 3.9 kg. The mean maternal hemoglobin level was 116.5 ± 12.0 g/L in Group 1 and 113.8 ± 13.2 g/L in Group 2. The indications for CS in the two groups are shown in Table 1.
Table 1.
Indications for cesarean section in patients undergoing intra-operative cell salvage with one and two suction devices (N = 30).
Blood volume collected and salvaged RBC volume
The total collected blood volume was 1765.6 ± 347.2 mL in Group 1 and 1123.3 ± 185.9 mL in Group 2 (t = 8.933, P < 0.001). The salvaged RBC volume was 401.6 ± 77.2 and 330.1 ± 53.3 mL in Group 1 and Group 2, respectively (t = 4.175, P < 0.001).
AF components and fetal RBC contamination
AF contamination for both groups is shown in Table 2. Fetal squamous cells were detected in all pre-wash, post-wash, and post-filtration samples, with a significant reduction at post-wash (both P < 0.001) and further statistical reduction in post-filtration (both P < 0.001). At post-filtration, squamous cells were found in three samples in each group with no significant difference between the two groups (P > 0.05). Both lamellar bodies and fat were significantly reduced after wash (both P < 0.001) and with no further statistical reduction after filter (both P > 0.05). No lamellar bodies and fat were detected in all post-filtration samples in both groups. IGFBP1, an important marker of AF, was also evaluated. The post-wash levels were significantly reduced (both P < 0.001) with no further statistical reduction seen post-filtration (both P > 0.05). No significant difference in IGFBP1 at post-filtration was found between the two groups (t = 0.606, P = 0.547). Similarly, the AFP, albumin, LDH, and potassium levels were significantly reduced post-wash (all P < 0.01), with no further statistical reduction observed in the post-filtration samples in either group (all P > 0.05). There was no significant difference in the AFP (t = 0.795, P = 0.430), albumin (t = 1.387, P = 0.171), LDH (t = 0.614, P = 0.542), and potassium (t = 0.557, P = 0.580) levels at post-filtration between the two groups.
Table 2.
Comparison of the AF components in the blood salvaged with one and two suction devices during cesarean section in patients with placenta previa and/or accrete.
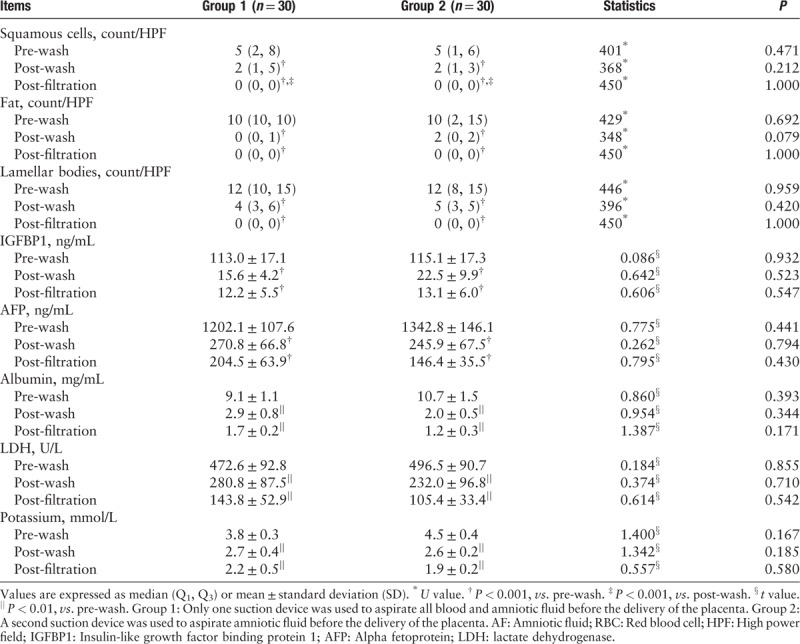
Fetal RBCs were present in all post-filtration samples. The mean percentage of fetal RBCs post-filtration was (1.8 ± 0.8) % with a range of 1.0% to 3.5% in Group 1 and (1.9 ± 0.9) % with a range of 0.7% to 4.0% in Group 2. There was no statistically significant difference between the two groups (U = 188.5, P = 0.651).
Reinfusion of salvaged RBC and adverse events
Nineteen patients received autologous blood (ten in Group 1 and nine in Group 2) finally. No adverse events were observed in these patients.
Discussion
This study demonstrated that AF contaminants, including squamous cells, lamellar bodies, fat, IGFBP1, AFP, albumin, LDH, and potassium, could be effectively reduced by using either one or two suction devices in combination with a leucodepletion filter. Fetal RBCs were found in all post-filtration salvaged blood. Importantly, the salvaged RBC volume was significantly enhanced when using one suction device.
A previous study by Sullivan et al[13] showed that, compared to the use of two suction devices, one suction device was associated with higher volumes of blood collection and RBC reinfusion. Although these differences were not significant in that study, a larger sample could potentially result in statistical significance. When massive bleeding occurs before the delivery of the placenta, such as in cases with abnormal placentation, one suction device may be used to reduce blood waste.
In an earlier study,[10] fetal squamous cells were present in the majority of post-filtration samples. However, Waters et al[12] showed that an advanced leucodepletion filter effectively reduces fetal squamous cell contamination. Sullivan et al[13] also found that fetal squamous cells were present in only two of 34 samples post-filtration. Our study found that squamous cells were markedly reduced post-filtration and present in only six of 30 samples post-filtration, confirming the results of previous research.[12,13,15]
Our study showed that fetal squamous cells were present in post-filtration samples when either one or two suction devices were used. However, Sullivan et al[13] found that fetal squamous cells were only found in post-filtration samples when one suction device was used. The reason for this difference is unknown but may be due to variations in different types of cell salvage machines and leucodepletion filters used in the previous and present studies. The contamination with fetal squamous cells may show no clinical significance.[13] This lack of significance is observed because fetal squamous cells can be present in maternal circulation at the time of placental separation in both normal delivery and CS.[12,22,23] In addition, AF embolism is no longer thought to be a result of the embolization of squamous cells but, rather, an anaphylactoid reaction triggered by an unidentified fetal antigen.[7,24]
Consistent with published data,[12] lamellar bodies, which serve as a marker of AF, were significantly reduced post-wash when two suction devices were used and were completely removed by filtering. However, no previous study has investigated the effectiveness of eliminating lamellar bodies by using one suction device. Our results found that lamellar bodies were also markedly reduced post-wash when one suction device was used, and they were completely removed by filtering.
Since reinfusion of fat particles may cause fat embolism, the elimination of fat during cell salvage is an important aspect of guaranteeing the safety of autologous blood.[25–28] It has been reported that fat can be removed by using a continuous cell salvage device.[28–30] The present study is the first to find that fat can be completely removed during CS by using either one or two suction devices.
Consistent with previous studies,[12,13,15,16] levels of AFP, albumin, LDH, and potassium were significantly reduced post-wash. This study was the first to examine the level of IGFBP1, which is an important AF marker,[31] and found that IGFBP1 levels were significantly reduced post-wash when using either one or two suction devices.
As expected, RBCs were found in all post-filtration salvaged blood, a finding that is consistent with previous studies.[10,12,13,15,16,21] Fetal RBC contamination may be clinically significant when there are RBC antigen incompatibilities between the mother and fetus.[13,21] Rhesus factor antigen incompatibilities can be prevented by routine Anti-D immune globulin treatment throughout pregnancy.[13,21] Other antibodies, such as anti-K, anti-c, anti-Fy (a), and anti-Jk (a), which can lead to RBC antigen incompatibilities, may cause fetal hyperbilirubinemia and anemia in future pregnancies.[13,21,32] However, fetal RBCs routinely enter maternal circulation during pregnancy and during vaginal delivery.[12,21] In addition, a sensitizing event or allogeneic blood transfusion during pregnancy may also result in maternal alloimmunization.[13] Recently, Ralph et al[21] reported that only anti-S antibodies had been detected at follow-up in one of 48 patients who received cell salvage reinfusion during CS. The clinical significance of anti-S antibodies is unknown, and that study was unable to determine whether the anti-S antibodies were formed as a result of the autologous blood reinfusion. To date, the clinical significance of fetal RBC contamination is uncertain, and follow-up with studies possessing larger sample sizes is required to evaluate the risk of maternal alloimmunization.
In this study, nineteen patients received autologous blood that had been collected by either one or two suction devices. Consistent with previous studies, no significant changes in blood pressure, heart rate, or other clinical complications were observed during autologous blood reinfusion.[13,16,21] Several studies have reported that hypotension could be induced by rapid reinfusion of autologous blood following the use of a leucodepletion filter.[33–35] The difference between our study and the above mentioned studies could be due to rapid volume resuscitation and slower reinfusion of autologous blood through a leucodepletion filter.
This present study contributes additional evidence for the efficacy of eliminating AF contaminants by using one suction device, which showed similar results to those obtained by using two suction devices. There was little to no possibility of AF contamination of the reinfused blood when a leucodepletion filter was used. Fetal RBCs were present in the reinfused blood, and further research is required to clarify the risk of maternal alloimmunization. One suction device may be used to reduce blood waste in cases with abnormal placentation when massive bleeding occurs before the delivery of the placenta.
In conclusion, performing cell salvage with one suction device rather than two such devices could result in higher volumes of salvaged RBCs and can be safely used when massive hemorrhage occurs during CS in patients with placenta previa and/or accrete.
Acknowledgements
The authors thank all the staff from the operation room (Women's Hospital, School of Medicine, Zhejiang University, Hangzhou, China) for their help with this study.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 81471126 and No. 81870868).
Conflicts of interest
None.
Footnotes
How to cite this article: Chen H, Tan H, Luo PX, Shen YF, Lyu CC, Qian XW, Chen XZ. Comparison of cell salvage with one and two suction devices during cesarean section in patients with placenta previa and/or accrete: a randomized controlled trial. Chin Med J 2020;133:638–643. doi: 10.1097/CM9.0000000000000699
References
- 1.Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet 2006; 367:1066–1074. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 2.Liston W. Haemorrhage. In: Lewis G, ed. The confidential enquiry into maternal, child health (CEMACH). Saving mothers’ lives: reviewing maternal deaths to make motherhood safer—2003-2005. The seventh report on confidential enquiries into maternal deaths in the United Kingdom. London: CEMACH; 2007:80. [Google Scholar]
- 3.Horstmann WG, Ettema HB, Verheyen CC. Dutch orthopedic blood management surveys 2002 and 2007: an increasing use of blood-saving measures. Arch Orthop Trauma Surg 2010; 130:55–59. doi: 10.1007/s00402-009-0910-0. [DOI] [PubMed] [Google Scholar]
- 4.Geoghegan J, Daniels JP, Moore PA, Thompson PJ, Khan KS, Gülmezoglu AM. Cell salvage at caesarean section: the need for an evidence-based approach. BJOG 2009; 116:743–747. doi: 10.1111/j.1471-0528.2009.02129.x. [DOI] [PubMed] [Google Scholar]
- 5.Weiskopf RB. Erythrocyte salvage during cesarean section. Anesthesiology 2000; 92:1519–1522. doi: 10.1097/00000542-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Allam J, Cox M, Yentis SM. Cell salvage in obstetrics. Int J Obstet Anesth 2008; 17:37–45. doi: 10.1016/j.ijoa.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Goucher H, Wong CA, Patel SK, Toledo P. Cell salvage in obstetrics. Anesth Analg 2015; 121:465–468. doi: 10.1213/ANE.0000000000000786. [DOI] [PubMed] [Google Scholar]
- 8.Neb H, Zacharowski K, Meybohm P. Strategies to reduce blood product utilization in obstetric practice. Curr Opin Anesthesiol 2017; 30:294–299. doi: 10.1097/ACO.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 9.Dhariwal SK, Khan KS, Allard S, Wilson M, Moore P. SALVO study group. Does current evidence support the use of intraoperative cell salvage in reducing the need for blood transfusion in caesarean section? Curr Opin Obstet Gynecol 2014; 26:425–430. doi: 10.1097/GCO.0000000000000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Catling SJ, Williams S, Fielding A. Cell salvage in obstetrics: an evaluation of the ability of cell salvage combined with leucocyte depletion filtration to remove amniotic fluid from operative blood loss at caesarean section. Int J Obstet Anesth 1999; 8:79–84. doi: 10.1016/s0959-289x(99)80002-8. [DOI] [PubMed] [Google Scholar]
- 11.Bernstein HH, Rosenblatt MA, Gettes M, Lockwood C. The ability of the haemonetics 4 cell saver system to remove tissue factor from blood contaminated with amniotic fluid. Anesth Analg 1997; 85:831–833. doi: 10.1097/00000539-199710000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Waters JH, Biscotti C, Potter PS, Phillipson E. Amniotic fluid removal during cell salvage in the cesarean section patient. Anesthesiology 2000; 92:1531–1536. doi: 10.1097/00000542-200006000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan I, Faulds J, Ralph C. Contamination of salvaged maternal blood by amniotic fluid and fetal red cells during elective caesarean section. Br J Anaesth 2008; 101:225–229. doi: 10.1093/bja/aen135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rainaldi MP, Tazzari PL, Scagliarini G, Borghi B, Conte R. Blood salvage during caesarean section. Br J Anaesth 1998; 80:195–198. doi: 10.1093/bja/80.2.195. [DOI] [PubMed] [Google Scholar]
- 15.Teare KM, Sullivan IJ, Ralph CJ. Is cell salvaged vaginal blood loss suitable for re-infusion? Int J Obstet Anesth 2015; 24:103–110. doi: 10.1016/j.ijoa.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Elagamy A, Abdelaziz A, Ellaithy M. The use of cell salvage in women undergoing cesarean hysterectomy for abnormal placentation. Int J Obstet Anesth 2013; 22:289–293. doi: 10.1016/j.ijoa.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 17.McDonnell NJ, Kennedy D, Long LJ, Gallagher-Swann MC, Paech MJ. The development and implementation of an obstetric cell salvage service. Anaesth Intensive Care 2010; 38:492–499. doi: 10.1177/0310057X1003800313. [DOI] [PubMed] [Google Scholar]
- 18.Committee on Obstetric Practice. ACOG committee opinion. Placenta accreta. Number 266, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet 2002; 77:77–78. doi: 10.1016/s0020-7292(02)80003-0. [DOI] [PubMed] [Google Scholar]
- 19.American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Practice guidelines for obstetric anesthesia: an updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Anesthesiology 2007; 106:843–863. doi: 10.1097/01.anes.0000264744.63275.10. [DOI] [PubMed] [Google Scholar]
- 20.Liumbruno GM, Liumbruno C, Rafanelli D. Intraoperative cell salvage in obstetrics: is it a real therapeutic option? Transfusion 2011; 51:2244–2256. doi: 10.1111/j.1537-2995.2011.03116.x. [DOI] [PubMed] [Google Scholar]
- 21.Ralph CJ, Sullivan I, Faulds J. Intraoperative cell salvaged blood as part of a blood conservation strategy in Caesarean section: is fetal red cell contamination important? Br J Anaesth 2011; 107:404–408. doi: 10.1093/bja/aer168. [DOI] [PubMed] [Google Scholar]
- 22.Lee W, Ginsburg KA, Cotton DB, Kaufman RH. Squamous and trophoblastic cells in the maternal pulmonary circulation identified by invasive hemodynamic monitoring during the peripartum period. Am J Obstet Gynecol 1986; 155:999–1001. doi: 10.1016/0002-9378(86)90334-0. [DOI] [PubMed] [Google Scholar]
- 23.Waters JH, Tuohy MJ, Hobson DF, Procop G. Bacterial reduction by cell salvage washing and leukocyte depletion filtration. Anesthesiology 2003; 99:652–655. doi: 10.1097/00000542-200309000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Clark SL. Amniotic fluid embolism. Clin Obstet Gynecol 2010; 53:322–328. doi: 10.1097/GRF.0b013e3181e0ead2. [DOI] [PubMed] [Google Scholar]
- 25.Eyjolfsson A, Plaza I, Brondén B, Johnsson P, Dencker M, Bjursten H. Cardiorespiratory effects of venous lipid micro embolization in an experimental model of mediastinal shed blood reinfusion. J Cardiothorac Surg 2009; 4:48.doi: 10.1186/1749-8090-4-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown WR, Moody DM, Challa VR. Cerebral fat embolism from cardiopulmonary bypass. J Neuropathol Exp Neurol 1999; 58:109–119. doi: 10.1097/00005072-199902000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Seyfried TF, Gruber M, Breu A, Aumeier C, Zech N, Hansen E. Fat removal during cell salvage: an optimized program for a discontinuous autotransfusion device. Transfusion 2016; 56:153–159. doi: 10.1111/trf.13286. [DOI] [PubMed] [Google Scholar]
- 28.Seyfried TF, Haas L, Gruber M, Breu A, Loibl M, Hansen E. Fat removal during cell salvage: a comparison of four different cell salvage devices. Transfusion 2015; 55:1637–1643. doi: 10.1111/trf.13035. [DOI] [PubMed] [Google Scholar]
- 29.Booke M, Fobker M, Fingerhut D, Storm M, Mortlemans Y, Van Aken H. Fat elimination during intraoperative autotransfusion: an in vitro investigation. Anesth Analg 1997; 85:959–962. doi: 10.1097/00000539-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Booke M, Van Aken H, Storm M, Fritzsche F, Wirtz S, Hinder F. Fat elimination from autologous blood. Anesth Analg 2001; 92:341–343. doi: 10.1097/00000539-200102000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Ruanphoo P, Phupong V. Evaluation of the performance of the insulin-like growth factor-binding protein-1/alpha-fetoprotein test in diagnosing ruptured fetal membranes in pregnant women. J Perinatol 2015; 35:558–560. doi: 10.1038/jp.2015.6. [DOI] [PubMed] [Google Scholar]
- 32.Roberts I. Prenatal and childhood transfusions. In: Murphy MF, Pamphilon DH, eds. Practical Transfusion Medicine. 2nd ed. Oxford: Blackwell Publishing Ltd; 2005:97–118. [Google Scholar]
- 33.Cyr M, Eastlund T, Blais C, Jr, Rouleau JL, Adam A. Bradykinin metabolism and hypotensive transfusion reactions. Transfusion 2001; 41:136–150. doi: 10.1046/j.1537-2995.2001.41010136.x. [DOI] [PubMed] [Google Scholar]
- 34.Domen RE, Hoeltge GA. Allergic transfusion reactions: an evaluation of 273 consecutive reactions. Arch Pathol Lab Med 2003; 127:316–320. doi: 10.1043/0003-9985(2003)127<0316:ATR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 35.Li MH, Yan LN, Wang SR. Autologous transfusion with modified total hepatic vascular exclusion for extracapsular resection of giant hepatic cavernous hemangioma. Hepatobiliary Pancreat Dis Int 2007; 6:43–48. [PubMed] [Google Scholar]


