Abstract
Introduction:
Virtual reality (VR) is an emerging tool for anxiety and fear reduction in pediatric patients. VR use is facilitated by Certified Child Life Specialists (CCLS) at pediatric hospitals. The primary aim of this study was to retrospectively review the safety of VR by analyzing adverse events after the utilization of VR under CCLS supervision. Secondary objectives were to characterize the efficacy of VR in enhancing patient cooperation, describe the integration of VR into Child Life services, and identify interventions that accompanied VR.
Methods:
The Stanford Chariot Program developed VR applications, customized VR interfaces, and patient head straps, and distributed these to CCLS. Chart review analyzed VR utilization through CCLS patient notes. Inclusion criteria were all patients ages 6 to 18-years-old who received a Child Life intervention.
Results:
From June 2017 to July 2018, 31 CCLS saw 8,098 patients, 3,696 of which met age criteria with pre- and post-intervention cooperation data. Two hundred thirteen patients received VR with an accompanying intervention, while 34 patients received only VR. Adverse events were rare, and included increased anxiety (3.8%, n=8), dizziness (0.5%, n=1), and nausea (0.5%, n=1). Patients were more likely to be cooperative after receiving VR (99.5%, n=212) compared to pre-intervention (96.7%, n=206, p=0.041). VR use was most common in the perioperative setting (60%, n=128), followed by outpatient clinics (15%, n=32).
Conclusion:
VR is safe in pediatric patients with appropriate hardware, software, and patient selection. Side effects were rare and self-limited. VR appears to be associated with improvements in cooperation.
INTRODUCTION
Pediatric patients commonly report feeling afraid or anxious when interacting with medical professionals in healthcare environments.1,2 Common behavioral demonstrations of pediatric anxiety include withdrawal, aggression, and lack of cooperation.3 This distress can delay medical treatment and reduce patient satisfaction.4
Nonpharmacological interventions for reducing childhood anxiety include use of distraction, an inviting environment, child and parental preparation, and positive staff interactions.5–7 Certified Child Life Specialists (CCLS), who have master’s degrees focused on coping strategies for pediatric patients and promotion of optimal patient experiences, often lead these interventional services for pediatric hospitals.8 Although CCLS utilize multiple traditional coping strategies such as therapeutic play, preparation for procedures, and education, novel techniques play an important role in anxiolysis.8
Virtual reality (VR) is an emerging tool for anxiety reduction. VR effectively attenuates pain perception and distress during hospitalizations.9–13 Given the reduction in the cost of portable VR units, VR has expanded to a variety of hospital care areas.10,14–16 Reportedly, CCLS play an integral role in the utilization of VR headsets throughout the hospital.17–19 Although full hospital integration is rare, CCLS have successfully launched VR in perioperative units, heart centers, phlebotomy labs, acute care centers, and emergency departments.17–19
Studies have generally reported few or no side effects associated with VR for pediatric patients.11,13,19–22 Adverse events, although rare and short-lived, may include motion sickness, nausea, or dizziness. The risk of collision also exists for specific cases of VR use. Additionally, pediatric patients may be less able to verbalize VR-associated discomfort, and young children may require contextualization after interacting with a virtual world.23 As VR becomes more widely used in pediatric hospitals, often through Child Life services, it is critical to understand its safety and efficacy profile in this setting.
The primary aim of this retrospective review was to evaluate the safety of VR in a pediatric hospital by characterizing adverse events after VR. Secondary objectives of the study were to analyze VR efficacy in enhancing patient cooperation, describe the integration of VR into Child Life services throughout a pediatric hospital, and identify the frequency with which CCLS paired other interventions with VR.
METHODS
Context
This review was conducted at a freestanding, 365-bed academic, quaternary care children’s hospital in Northern California. The population included medical and surgical patients seen by 31 CCLS. Eligible patients were located in 3 acute care floor units, a pediatric intensive care unit, a cardiovascular intensive care unit, a perioperative department with 16 anesthetizing locations, and 5 ambulatory clinics.
Intervention
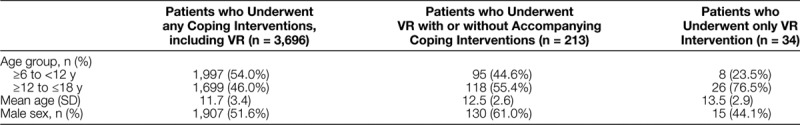
We conducted a retrospective cohort review of patients who received services from the hospital’s CCLS from June 7, 2017, to July 25, 2018. Inclusion criteria were all patients ages 6–18 years old who received a Child Life intervention. Patients were excluded from analysis if preintervention or postintervention cooperation data was missing (Table 1). Patient information was obtained through a customized report created from the electronic medical record (EMR). The IRB granted a waiver of approval for this study. This study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for case-control studies.24
Table 1.
Patient Characteristics
The integration of VR into the hospital was a collaboration between the Stanford Chariot Program and the Child Life and Creative Arts Department. The Chariot Program is funded through philanthropic donations and is composed of a multidisciplinary group of pediatric anesthesiologists, pediatric pain physicians, and research scientists. The Chariot Program utilized a 3-step approach to develop the hospital’s VR program: (1) software development; (2) hardware modification; and (3) integration into clinical care. Although there exists VR content that is commercially available for purchase, the Chariot Program developed and customized several VR applications specifically for pediatric patients. Developed content was nonviolent, was intuitive for the user to learn, had limited startup menus to ensure rapid access and immediate gameplay, utilized third-person rather than the first-person perspective, kept the head mostly or entirely still, and had no fail-states (eg, the user’s character cannot die or become incapacitated in any way). In some circumstances, the content was complementary to patient care; for example, content that kept the head still and paired the headset with a handheld controller could be used for ENT endoscopy, whereas gameplay designed to keep the extremities still and instead use slight head movement could be used for intravenous access or orthopedic procedures. We organized this VR content on a customized VR interface, also produced by Chariot, which curates a content library while also prohibiting typical cellular phone features such as access to the internet (this is simply a safety measure to ensure children cannot access anything besides what is intended by providers). Samsung (Seoul, South Korea) GearVR headsets fitted with Samsung S8+ cellular phones were used to display the VR interface and applications. Customized head straps were designed with 3D-printed attachments and commercially available ratchets to ensure infection control compliance and fit to pediatric head circumferences.
The integration of the VR units into a new care area was a multistep process. First, in collaboration with CCLS, a needs analysis determined the specific population of interest, such as anxiolysis before phlebotomy, wound care, and minor procedures. The physician Chariot Program Manager trained CCLS with an emphasis on sanitization procedures and a process for securing the device while not in use. Locked cabinets were used to store the devices in areas convenient for the users. Within these locked cabinets, we used a Samsung Wireless Charging station to charge the devices. CCLS were additionally trained by the physician Chariot Program Manager to assess potential adverse events during VR interventions. Patients were evaluated by trained CCLS, who made individualized treatment plans based on a repository of tools available to them. Potential VR patient candidates were 6 years or older without a history of seizure or motion sickness. After screening patients, CCLS introduced VR as a possible coping mechanism and, with patient agreement, proceeded to utilize it. A variety of active and passive applications were offered, and the patient had the option to choose their own experience. The individualized interventions were not controlled, as this was a retrospective review.
Measures
The Chariot Program and CCLS collaborated with the hospital information services (IS) department to develop customized child life intervention notes in the EMR. The integration of VR was measured through a retrospective analysis of CCLS documentation. The child life intervention notes included the questions “Was the child cooperative preintervention?” and “Was the child cooperative postintervention?” which CCLS answered by selecting “yes” or “no.” We defined cooperation as the patient not withdrawing from the medical intervention at hand and allowing the care team to proceed with the intervention. CCLS also documented which coping interventions the patient underwent, including family presence, comfort positioning, diaphragmatic breathing, environmental adaptions, imagery, pharmacologic assistance, tablet, bedside entertainment theater,25 VR, augmented reality, interactive video game, and/or movie. Age, gender, adverse events, patient location, and interventions accompanying VR were also measured through a chart review of the CCLS intervention note. Adverse events were reported in the EMR if observed by CCLS or stated by the patient. Although there was no standardized questioning of adverse events, as that was outside the scope of this retrospective review, CCLS were thoroughly trained to ascertain and report the presence of adverse events adequately.
Patients were analyzed in 3 groups. The first group included patients who received any coping intervention, even those without VR. The second group included patients who underwent a VR coping intervention, with or without an accompanying intervention. Patients in the third group underwent a VR coping intervention only and did not experience any accompanying intervention. All groups were guided by CCLS.
Analysis
All summary statistics and calculations were performed using R Statistical Computing Software, Version 3.0 (https://www.R-project.org/). We sought to characterize the changes in cooperation with induction preintervention and postintervention. The primary hypothesis was that postintervention cooperation rates would be significantly higher than preintervention cooperation rates. Furthermore, we conducted 2 subgroup analyses to determine whether postintervention cooperation rates were increased in both younger and older children, and children of both sexes. We hypothesized that postintervention cooperation rates would be higher than preintervention cooperation rates irrespective of age and sex. Because we conducted 2 subgroup analyses (with 2 hypotheses each), as well as 1 primary analysis (comparing preintervention and postintervention cooperation rates overall), P values were the Bonferroni corrected for the 5 hypotheses. The P values for changes in cooperation were calculated using McNemar’s test, given the binary and repeated nature of the outcome (cooperation with induction). A corrected P value of <0.05 was used as the threshold for significance.
As an exploratory analysis, we also examined preintervention and postintervention cooperation rates in patients for whom intervention included VR. Again, McNemar’s test was used to calculate the P value comparing preintervention and postintervention cooperation. As this was an exploratory analysis, we did not correct for multiple hypothesis testing because the present study was designed to retrospectively examine the usage of clinical interventions (including VR) at a single institution. Therefore, it was underpowered to quantify the efficacy of VR within the subset of patients who received that form of intervention.
RESULTS
From June 2017 to July 2018, CCLS saw 8,098 patients and documented preintervention and postintervention cooperation data on 5,241 patients, 3,696 of which met age criteria (Fig. 1). Patients receiving any intervention were 51.6% male (n = 1,907) and 54.0% younger (age 6–12 years old, n = 1,997), with a mean age of 11.7 years (Table 1). Patients receiving a VR intervention with or without accompanying intervention were 61.0% male (130 out of 213), ranging from 6 to 18 years old, with a mean age of 12.5 years (Table 1). Of these patients, 55.4% were between 12 and 18 years old (n = 118 out of 213). Patients who received VR alone were 44.1% male (15 out of 35), ranged from 7 to 18 years old, with a mean age of 13.5 years. Of these, the majority were in the 12- to 18-year-old age group (76.5%, age 12–18 years old) (Table 1).
Fig. 1.
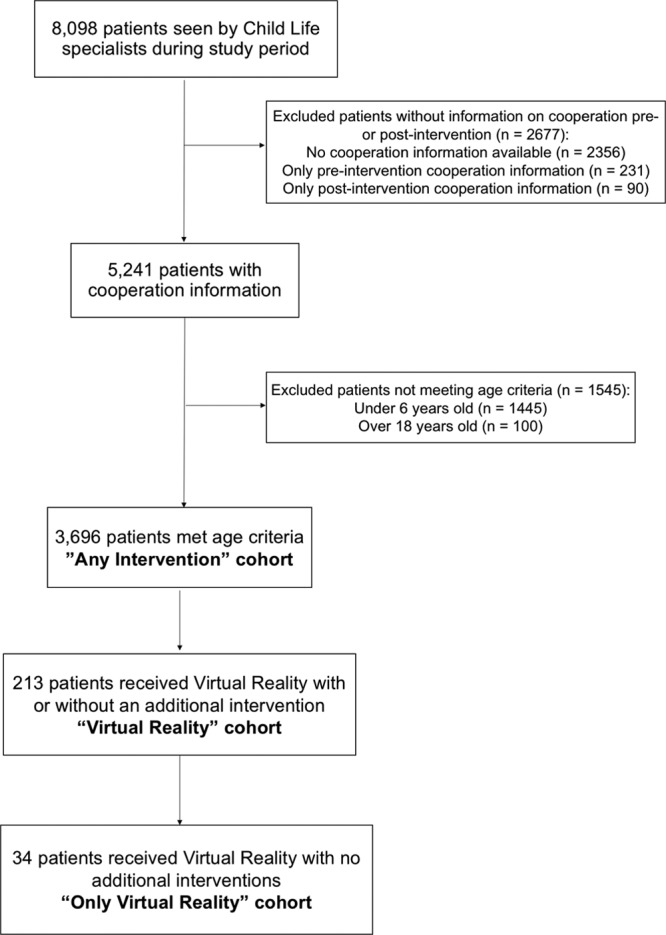
Flow diagram of patients included in this analysis.
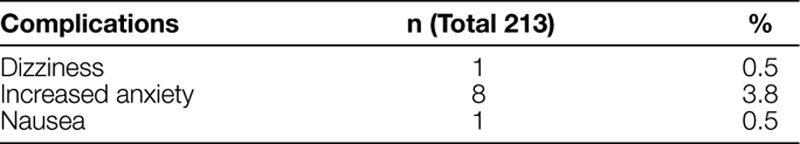
VR Safety
There were few adverse events when using VR (Table 2). The most common complication was increased anxiety (3.8%, n = 8), followed by dizziness (0.5%, n = 1) and nausea (0.5%, n = 1).
Table 2.
Adverse Events Reported in Pediatric Patients Undergoing VR Coping Intervention
Intervention and VR Effectiveness
Patients were more likely to be cooperative after receiving any coping intervention (97.9%, n = 3619, 95% confidence interval [CI] 97.4%–98.3%) than compared to preintervention (96.4%, n = 3,564, 95% CI 95.8%–97.0%, P < 0.001) (Tables 3–5). The significant increase in the proportion of cooperative patients was seen in younger age groups (preintervention: 94.8%, n = 1,894, 95% CI 93.8%%–95.7%; postintervention: 97.1%, n = 1,939, 95% CI 96.2%–97.7%, P < 0.001), but not in older age groups (preintervention: 98.2%, n = 1,670, 95% CI 97.6%–98.8%; postintervention: 98.9%, n = 1,680, 95% CI 98.3%–99.3%, corrected P = 0.221). When divided by sex, both males (preintervention: 96.1%, n = 1,832, 95% CI 95.1%–96.9%; postintervention: 98.0%, n = 1,868, 95% CI 97.2%–98.5%, corrected P < 0.001) and females (preintervention: 96.8%, n = 1,732, 95% CI 95.8%–97.5%; postintervention: 97.9%, n = 1,751, 95% CI of 97.1%–98.4%, corrected P = 0.043) were significantly more likely to cooperate with induction after receiving some form of intervention.
Table 3.
Patient Cooperation: Cooperation with Any Intervention
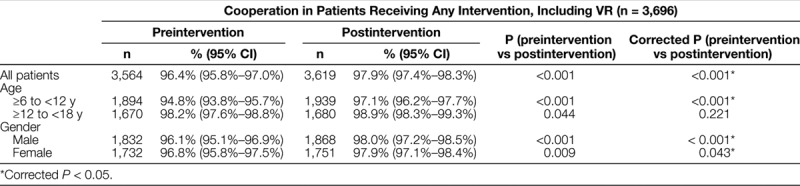
Table 5.
Patient Cooperation: Cooperation in Patients Receiving VR Only in the Absence of Other Interventions*
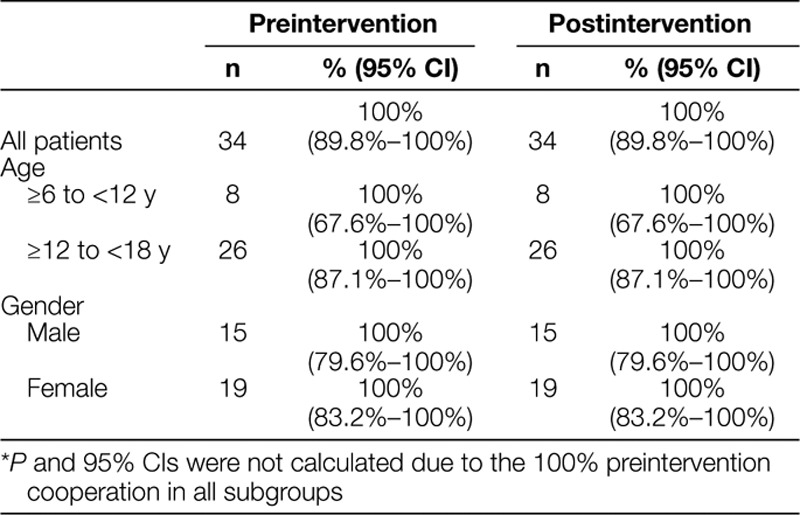
Table 4.
Patient Cooperation: Cooperation in Patients Receiving VR Intervention
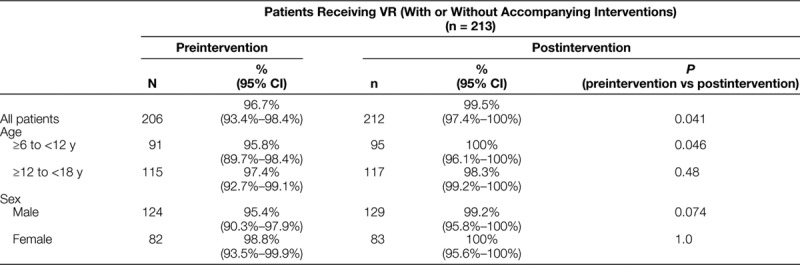
In the exploratory VR analysis, patients were more likely to be cooperative after receiving a VR coping intervention (with or without accompanying interventions) (99.5%, n = 212, 95% CI 97.4%–100%) compared to preintervention (96.7%, n = 206, 95% CI 93.4%–98.4%, P = 0.041). This increase in cooperativity was observed in younger patients (preintervention: 95.8%, n = 91, 95% CI 89.7%–98.4%; postintervention: 100%, n = 95, 95% CI 96.1%–100%, P = 0.046), but not in older patients (preintervention: 97.4%, n = 115, 95% CI 92.7%–99.1%; postintervention: 98.3%, n = 117, 95% CI 99.2%–100%, P = 0.48). There was no significant difference between pre-VR intervention and post-VR intervention cooperation in either males or females.
All patients who received VR only were cooperative both preintervention and postintervention (100%, n = 34).
Integration of VR into Child Life Services
VR was integrated throughout the pediatric hospital (Fig. 2). From June 2017 to July 2018, 213 patients received VR with an accompanying intervention, and 34 patients received VR alone (Table 1). The highest proportion of VR use was in the perioperative setting (60%, n = 128), followed by outpatient clinics (15%, n = 32), which included pediatric otolaryngology, orthopedics, general surgery, allergy and immunology, and gastroenterology (Fig. 2). The remaining locations included acute care (9%, n = 19), short stay (8%, n = 16), intensive care (7%, n = 16), and radiology (1%, n = 2) (Fig. 2).
Fig. 2.
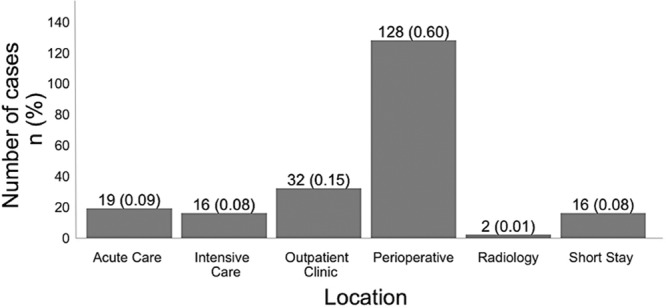
Location of VR utilization.
Accompanying Coping Interventions
VR was utilized alone and with other accompanying interventions (Fig. 3). Most common accompanying interventions included diaphragmatic breathing (n = 93), family presence (n = 85), pharmacological assistance (n = 80), environmental adaptations (n = 64), and video games (n = 53).
Fig. 3.
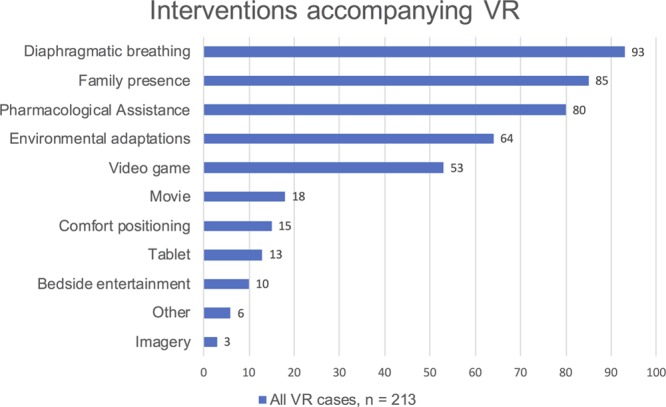
Interventions accompanying VR.
DISCUSSION
This retrospective study describes the safety and effectiveness of VR headsets as accompanying tools for CCLS in a pediatric hospital. VR was deployed by the Chariot Program and CCLS in multiple settings, including perioperative, outpatient, acute care, short stay, intensive care, and radiology. Partnership with CCLS enabled the adoption of VR across numerous care settings throughout the hospital as a tool for the reduction of pediatric anxiety. Partnering with hospital IS enabled further integration of CCLS through a specialized EMR note, which allowed for tracking of coping interventions and patient cooperativity. Finally, the Chariot Program served as the champion through VR software development, hardware modification, and integration into clinical care. The Chariot Program developed several VR applications that were explicitly customized for pediatric patients.
This study adds to the growing evidence that VR can be safely used in children in a healthcare setting.11,13,19–22,25,26 Side effects were infrequent, with the most common being an increase in anxiety, which has not been previously reported. Nausea and dizziness were far less common than anticipated, likely secondary to enhanced content and careful patient selection. The use of VR is not intended for all patients and was only charted in about 5% of patients seen by CCLS. Such patient selection is critical: though VR is generally safe, a patient’s age and history of motion sickness or seizure disorders should be considered before VR utilization. VR hardware and software should also be customized to the patient’s age, size, and clinical presentation.
Adverse events were very rare in this study, whereas typical VR gameplay systems have a high risk of motion sickness in adults.27 Although this study is not designed to identify the differences, the low risk of adverse events we observe likely stems from the highly curated VR content that we specifically designed for pediatric healthcare use. For example, all the VR experiences maintain a third-person rather than the first-person point of view, because the first-person point of view is more likely to contribute to motion sickness.28 The content additionally limits the head range of motion, especially flexion and extension of the neck, to reduce vestibular motion. Patients are also typically not moving around during VR use. They are interacting with a carefully designed VR world that helps to prevent the motion sickness that may be more common during the use of commercial VR systems.
General clinical intervention (of any type) was associated with increased cooperation overall in both male and female participants. Although younger patients were significantly more cooperative with induction following the intervention, the same differences were not seen in older patients (between 12 and 18 years old). This observation may be attributable to the high baseline rates of preintervention cooperation (98.2%) within this patient population.
In this exploratory analysis, the use of VR appears to be associated with improvements in cooperation, although the study was not powered to detect the significance of this association. The CCLS rarely used VR as a standalone intervention. Instead, it was usually complemented by other interventions, including diaphragmatic breathing, family presence, pharmacological assistance, environmental adaptations, and video games. When VR was used alone, VR was provided to patients who were cooperative before the CCLS encounter. VR often requires a cooperative patient who is willing to wear a headset and suspend belief to partake in a VR environment. Although it appears that younger patients (age 6 to 12 years old) were more likely to benefit from VR, this analysis was exploratory and not powered to detect subgroups that may respond more or less robustly to VR. Although the increases in cooperation may seem like small absolute differences, an improvement, however, small, in cooperation is not what would be anticipated. Generally speaking, when facing imminent medical interventions, most pediatric patients become less cooperative and may withdraw from the intervention. Maintenance or improvement of patient cooperation is clinically significant, in our opinion.
Limitations of this study included its lack of control group, as is common in retrospective reviews. Another limitation of retrospective reviews regarding the effectiveness of an intervention is that a before-and-after design time series is susceptible to the Hawthorne effect. Although time-series event data were out of the scope of this study, future studies should collect data over time to understand variation in data over time, including common versus special cause variation. The patient cooperativity scale was subjectively rated by CCLS. There also is the possibility of selection bias, because CCLS did not randomize patients to interventions but instead applied evaluation criteria, judgment, and expertise in selecting the appropriate intervention for each patient.
Given that this is a retrospective study, we have no reason to suspect that CCLS skewed the results since the CCLS was unaware of the forthcoming study during data collection. Additionally, as this is a large study relying on point-of-care providers, it would be extremely challenging to integrate into the EMR validated outcome measures of cooperativity. Our approach of using surrogates, such as self-reported measures in large numbers, is not ideal but provides initial evidence with a large sample size that can be corroborated by smaller studies using validated outcome measures. Because CCLS reported adverse events without a standardized set of questions asked of patients, there may have been adverse events not observed by CCLS or verbalized by patients. Some patients were excluded from the analysis because they lacked complete data. Our findings examining the efficacy of VR interventions are exploratory, and the present study was not powered to compare the effectiveness of VR to existing interventions. As VR appears to be a safe intervention, future studies should quantify the efficacy of VR compared to other existing interventions and aim to uncover specific subpopulations for which VR is most effective. Finally, we were unable to capture patients who used VR outside of CCLS due to the lack of an electronic charting entry field for other healthcare providers who use VR at our institution, including physicians, nurses, volunteers, or rehabilitation services.
CONCLUSIONS
Although the use of VR in pediatric patients is becoming increasingly common, it has been limited by the paucity of studies performed in young patients and lack of adequate infection control-compliant hardware and healthcare-ready software for small children. This preliminary review suggests that VR is safe in pediatric patients given appropriate hardware and software and careful patient selection under the guidance of trained CCLS. Side effects were rare and self-limited. VR is associated with improvements in cooperation, although the study was not powered to compare the efficacy of VR to existing interventions. This study demonstrates the feasibility of widescale VR implementation with data tracking through the medical record by CCLS. It describes the integration of VR into Child Life services throughout a pediatric hospital and identifies the interventions that accompanied VR.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
ACKNOWLEDGMENTS
We would like to acknowledge the Stanford Chariot Program at Lucile Packard Children’s Hospital Stanford for providing the software and hardware used in this study. The Chariot Program provides software and hardware for free to clinicians around the world.
Footnotes
Published online April 10, 2020
To cite: Caruso TJ, O’Connell C, Qian JJ, Kung T, Wang E, Kinnebrew S, Pearson M, Kist M, Menendez M, Rodriguez ST. Retrospective Review of the Safety and Efficacy of Virtual Reality in a Pediatric Hospital. Pediatr Qual Saf 2020;2:e293.
REFERENCES
- 1.Brewer S, Gleditsch SL, Syblik D, et al. Pediatric anxiety: child life intervention in day surgery. J Pediatr Nurs. 2006; 21:13–22 [DOI] [PubMed] [Google Scholar]
- 2.Lerwick JL. Psychosocial implications of pediatric surgical hospitalization. Semin Pediatr Surg. 2013; 22:129–133 [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez CM, Clough V, Gowda AS, et al. Multimethod assessment of children’s distress during noninvasive outpatient medical procedures: child and parent attitudes and factors. J Pediatr Psychol.. 2012; 37:557–566 [DOI] [PubMed] [Google Scholar]
- 4.Chon T, Ma A, Mun-Price C. Perioperative fasting and the patient experience. Cureus. 2017; 9:e1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rice G, Ingram J, Mizan J. Enhancing a primary care environment: a case study of effects on patients and staff in a single general practice. Br J Gen Pract. 2008; 58:465–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perry JN, Hooper VD, Masiongale J. Reduction of preoperative anxiety in pediatric surgery patients using age-appropriate teaching interventions. J Perianesth Nurs. 2012; 27:69–81 [DOI] [PubMed] [Google Scholar]
- 7.Hoekstra S, Margolis L. The importance of the nursing role in parental vaccine decision making. Clin Pediatr (Phila). 2016; 55:401–403 [DOI] [PubMed] [Google Scholar]
- 8. Committee on Hospital Care and Child Life Council. Child life services. Pediatrics. 2014; 133:e1471–1478 [DOI] [PubMed] [Google Scholar]
- 9.Furman E, Jasinevicius TR, Bissada NF, et al. Virtual reality distraction for pain control during periodontal scaling and root planing procedures. J Am Dent Assoc. 2009; 140:1508–1516 [DOI] [PubMed] [Google Scholar]
- 10.Li A, Montaño Z, Chen VJ, et al. Virtual reality and pain management: current trends and future directions. Pain Manag. 2011; 1:147–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gold JI, Kim SH, Kant AJ, et al. Effectiveness of virtual reality for pediatric pain distraction during i.v. placement. Cyberpsychol Behav. 2006; 9:207–212 [DOI] [PubMed] [Google Scholar]
- 12.Schneider SM, Kisby CK, Flint EP. Effect of virtual reality on time perception in patients receiving chemotherapy. Support Care Cancer. 2011; 19:555–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clin J Pain. 2009; 25:815–826 [DOI] [PubMed] [Google Scholar]
- 14.Rizzo AA, Difede J, Rothbaum BO, et al. VR PTSD exposure therapy results with active duty OIF/OEF combatants. Stud Health Technol Inform. 2009; 142:277–282 [PubMed] [Google Scholar]
- 15.Gorini A, Pallavicini F, Algeri D, et al. Virtual reality in the treatment of generalized anxiety disorders. Stud Health Technol Inform. 2010; 154:39–43 [PubMed] [Google Scholar]
- 16.Rothbaum BO, Hodges L, Kooper R. Virtual reality exposure therapy. J Psychother Pract Res. 1997; 6:219–226 [PMC free article] [PubMed] [Google Scholar]
- 17.Yuan JC, Rodriguez S, Caruso TJ, et al. Provider-controlled virtual reality experience may adjust for cognitive load during vascular access in pediatric patients. Can J Anaesth. 2017; 64:1275–1276 [DOI] [PubMed] [Google Scholar]
- 18.Chad R, Emaan S, Jillian O. Effect of virtual reality headset for pediatric fear and pain distraction during immunization. Pain Manag. 2018; 8:175–179 [DOI] [PubMed] [Google Scholar]
- 19.Gold JI, Mahrer NE. Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J Pediatr Psychol. 2018; 43:266–275 [DOI] [PubMed] [Google Scholar]
- 20.Ravi DK, Kumar N, Singhi P. Effectiveness of virtual reality rehabilitation for children and adolescents with cerebral palsy: an updated evidence-based systematic review. Physiotherapy. 2017; 103:245–258 [DOI] [PubMed] [Google Scholar]
- 21.Tashjian VC, Mosadeghi S, Howard AR, et al. Virtual reality for management of pain in hospitalized patients: results of a controlled trial. JMIR Ment Health. 2017; 4:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Faber AW, Patterson DR, Bremer M. Repeated use of immersive virtual reality therapy to control pain during wound dressing changes in pediatric and adult burn patients. J Burn Care Res. 2013; 34:563–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Won A, Bailey J, Bailenson J, et al. Immersive virtual reality for pediatric pain. Children. 2017; 4:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.von Elm E, Altman DG, Egger M, et al. ; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008; 61:344–349 [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez S, Caruso T, Tsui B. Bedside entertainment and relaxation theater: size and novelty does matter when using video distraction for perioperative pediatric anxiety. Paediatr Anaesth. 2017; 27:668–669 [DOI] [PubMed] [Google Scholar]
- 26.Arane K, Behboudi A, Goldman RD. Virtual reality for pain and anxiety management in children. Can Fam Physician. 2017; 63:932–934 [PMC free article] [PubMed] [Google Scholar]
- 27.Akiduki H, Nishiike S, Watanabe H, et al. Visual-vestibular conflict induced by virtual reality in humans. Neurosci Lett. 2003; 340:197–200 [DOI] [PubMed] [Google Scholar]
- 28.Nishiike S, Okazaki S, Watanabe H, et al. The effect of visual-vestibulosomatosensory conflict induced by virtual reality on postural stability in humans. J Med Invest. 2013; 60:236–239 [DOI] [PubMed] [Google Scholar]


