Abstract
Background:
Insomnia and depression are highly prevalent perinatal complications. Ruminating on stress is etiologically implicated in both disorders, and ruminating while trying to fall asleep has been linked to insomnia and depression during pregnancy. Incompatible with rumination is everyday mindfulness, i.e., living with intentional and nonjudgmental awareness of internal and external experiences in the present moment. Responding to stress mindfully may protect against stress-related perinatal complications such as insomnia and depression. The present study described the association between everyday mindfulness and nocturnal rumination, and examined whether these trait characteristics were independently related to perinatal insomnia and depression.
Methods:
Cross-sectional and secondary analysis of existing data from 65 pregnant women recruited from a multisite hospital in Metro Detroit, MI, USA. Subjects completed online surveys including the Insomnia Severity Index, Edinburgh Postnatal Depression Scale, Presleep Arousal Scale, and the revised Cognitive and Affective Mindfulness Scale.
Results:
Over half (53.8%) of women screened positive for clinical insomnia and 12.3% screened positive for major depression. Women high in mindfulness, relative to those low in mindfulness, reported less nocturnal rumination (Cohen’s d=1.16), insomnia symptoms (Cohen’s d=1.24), and depressive symptoms (Cohen’s d=1.35). Multivariate linear regression revealed that both mindfulness (β=−.24, p=.03) and rumination (β=.38, p<.01) were independently associated with insomnia. Similarly, a multivariate model showed that mindfulness (β=−.41, p<.001) and rumination (β=.35, p<.01) were independently associated with depression.
Conclusions:
Ruminating in bed at night is strongly associated with insomnia and depression during pregnancy, whereas mindfulness may potentially protect against these stress-related perinatal complications.
Keywords: Sleep, Prenatal, Perinatal, Cognitive arousal, Stress, Emotion regulation
Introduction
Although most women view pregnancy and motherhood positively, the perinatal period is a highly stressful period.1 Thus, it is unsurprising that prevalence rates of stress-related conditions are high during this time. Over half of pregnant women have significant insomnia symptoms and 15–20% have depressed mood.2–4 These sleep and mood symptoms are highly comorbid with 25% of pregnant women with insomnia also endorsing major depression (vs. 4% of pregnant good sleepers).3 Rumination (repetitive negative thinking) is an automatic and maladaptive emotion regulation strategy for coping with stress, which is etiologically implicated in insomnia and depression in the general adult population.5–7 Indeed, prospective data suggest that ruminative coping links insomnia to depression.5,8 Recent evidence has extended this research by linking rumination to insomnia and depression in perinatal women.3,9 While emphasis on rumination identifies etiological processes in perinatal insomnia and depression, potential protective factors have been overlooked.
One factor incompatible with rumination is mindfulness.10 Mindfulness involves intentional and nonjudgmental awareness of internal and external experiences in the present moment, self-compassion, and nonattachment to outcomes.6,11,12 By comparison, rumination is unmoored and corrosive wandering of the mind on past wrongs and/or future concerns, which often involves attachment to outcomes (e.g., ruminating on how things “should be”).5,6,11 Perinatal women endorse significant concerns about pregnancy, childbirth, and fetal/infant health, thus providing ample negative cognitive content for rumination.13 Responding to these perinatal concerns mindfully may lessen negative emotionality and allostatic overload associated with ruminative thoughts by disengaging from the process of rumination and/or by shifting metacognitions.10–12 In other words, mindfully responding to stress allows individuals to recognize and evaluate negative thoughts and feelings with compassionate awareness, which can prevent a downward spiral of toxic rumination into depression or insomnia.11,12 Notably, the “core skill” of mindfulness-based cognitive therapy involves patients learning the ability “to recognize and disengage from mind states characterized by self-perpetuating patterns of ruminative, negative thought” to prevent stress-related disease development.10
However, the extant literature on mindfulness and rumination in the perinatal period is limited in key ways. Although rumination after childbirth and in relation to parenting has received considerable attention,14–16 we know little about ruminative thinking during pregnancy. Emerging evidence suggests that pregnant women harbor many pregnancy- and child-related concerns and may overuse this maladaptive coping strategy. Understandably, pregnant women express high levels of concern about their pregnancy, childbirth, and motherhood.13 Women preoccupied by these thoughts have higher rates of mental illness than those less inclined to dwell on these concerns. Importantly, rumination appears elevated in pregnancy, which is associated with poor sleep and mental health,3,9 and prospective data show that pregnant women who ruminate on stress are at elevated risk for prenatal depression.17
Comparatively, even less is known about everyday mindfulness during pregnancy. Rather, mindfulness-focused studies in perinatal populations have typically focused on mindfulness-based interventions on maternal health outcomes. These studies offer promising results that suggest cultivating mindfulness through meditation improves mood and reduces stress and ruminative thought processes in pregnant women.18–23 Notably, much of the work on the relationship between mindfulness and ruminative thinking during pregnancy has centered on mindfulness-based interventions on worry,18 rather than focus on everyday mindfulness in relation to other forms of rumination. Evaluating the association of mindfulness with other forms of rumination (e.g., nocturnal, angry, depressive) may yield important clinical implications for serious perinatal complications such as insomnia and depression. Along these lines, although rumination has been hypothesized to underlie the transition from perinatal insomnia to depression,3 evidence for how this process occurs remains limited. Are mindfulness and rumination two different sides of the same coin in regard to their associations with perinatal insomnia and depression? Or are they related constructs with independent contributions to these perinatal complications?
The current study examined the association between mindfulness and rumination and their associations with insomnia and depression in mid-to-late pregnancy. We specifically examined everyday mindfulness (proclivity to be present-focused, self-compassionate, and accepting) and nocturnal rumination (rumination that occurs at night while trying to fall asleep). Everyday mindfulness is negatively associated with rumination,24 and nocturnal rumination has been posited to link insomnia to depression during pregnancy.3 Thus, we hypothesized that mindfulness and nocturnal rumination would be strongly and inversely related to one another. Further, we hypothesized that both constructs would be independently associated with insomnia and depression, in opposite directions.
Participants and Methods
Participants and procedures
All procedures were approved by the institutional review board. This study was a secondary analysis of existing data. Data analyzed in this report were collected in the screening phase of a study to determine eligibility for a prospective investigation, which included naturalistic observation and treatment components. Pregnant patients in a 6-hospital health system in Metro Detroit were invited to participate in a study on sleep. We recruited women nearing/entering the third trimester as sleep disturbances are greatest in late pregnancy.25 A total of 267 women completed online screening surveys from home. We collected mindfulness data from 65 women, as this measure was added late into collection, thus we focus on this subsample.
Measures
Cognitive and Affective Mindfulness Scale e Revised (CAMS-R)24 measured everyday mindfulness (attention, awareness, present-focus, acceptance/nonjudgment). An example item from the CAMS-R is “I am able to focus on the present moment.” We analyzed the modified 10-item version (henceforth, CAMS-RM), which omits items redundant with worry and rumination. Scores range from 10 to 40 with higher scores indicating greater mindfulness. In the absence of empirically established cutoff criteria for the CAMS-RM to detect cases of high or low everyday mindfulness, we operationalized subjects who scored >28 (median of this sample) as high on mindfulness, whereas those who scored ≤28 were considered low in mindfulness. Internal consistency was high in the present study (Cronbach’s α=.87).
Presleep Arousal Scale e Cognitive factor (PSAS-C)26 measured nocturnal rumination. An example item from the PSAS-C is “review or ponder events of the day.” Scores range from 8 to 40 with higher scores indicating greater rumination. Puzino et al. showed that PSAS-C scores > 19 were predictive of clinically significant insomnia symptoms, sleep onset insomnia, and clinically significant anxiety.27 We adopted this cutoff to categorize our participants into high and low ruminators. Internal consistency was high in the present study (Cronbach’s α=.89).
Insomnia Severity Index (ISI) measured global insomnia.28 Scores range from 0 to 28 with higher scores indicating greater severity. ISI scores ≥ 10 indicate clinical insomnia. Because our previous work shows that difficulty falling asleep is closely tied to rumination and depression,3,29 we specifically assessed for sleep onset insomnia symptoms via the Pittsburgh Sleep Quality Index (PSQI).30 Based on responses to PSQI item 5a, sleep onset insomnia was operationalized as an inability to fall asleep within 30 mins ≥3 nights/week over the past month (binary variable). Internal consistency was high in the present study (Cronbach’s α=.90).
Edinburgh Postnatal Depression Scale (EPDS) measured depression.31 Scores range from 0 to 30 with higher scores indicating greater severity. EPDS scores ≥ 13 suggest major depression.32 Internal consistency was high in the present study (Cronbach’s α=.86).
Sociodemographics were assessed via online survey. Poverty was operationalized as annual household income <$20,000, which is consistent with the poverty line of $21,330 for a household of 3 per the US Department of Health and Human Services 2019 Poverty Guidelines. Body Mass Index (BMI) and Medicaid coverage were recorded from electronic medical records.
Analyses
Analyses were conducted in SPSS 25 (IBM Corporation, Armonk NY, USA) for Windows. After reporting sample characteristics, we used independent samples t-tests to compare high vs. low mindfulness and high vs. low nocturnal rumination on insomnia and depression. We then conducted two multivariate linear regression models to characterize specificity of associations between mindfulness and rumination with insomnia and depression while controlling for poverty in predicting insomnia and for poverty and Medicaid coverage in predicting depression as identified in a previous report.3 In addition, we controlled for depression status when predicting insomnia symptoms and controlled for insomnia status and sleep onset insomnia symptoms when predicting depression to establish whether any associations of mindfulness and nocturnal rumination with insomnia/depression are independent of comorbid symptoms.
Results
Sample characteristics and sociodemographics
Sample characteristics are reported in Table 1. The average age for women was 30.38±4.96 years and all were in the second or third trimester. Comparisons of primiparous (n=24) and multiparous women (n=41) revealed no differences in mindfulness (t[63]=−.21, p=.84), nocturnal rumination t[63]=.59, p=.56), insomnia (t[63]=1.39, p=.17), or depression (t[63]=.68, p=.50). An estimated 12.3% of the sample was in poverty and 24.6% had Medicaid insurance coverage. Most women identified as either non-Hispanic white or non-Hispanic black, whereas other racial categories each represented <5% of the sample. Only one participant reported a diagnosis of insomnia (1.54%) and five participants reported a diagnosis of obstructive sleep apnea (7.69%). Regarding medication use, three participants reported taking selective serotonin reuptake inhibitors (4.62%), whereas 11 reported using sleep aids (over-the-counter or prescription) over the past month (16.92%).
Table 1.
Sociodemographics, insomnia symptoms, and psychological characteristics (n=65)
| M±SD | n, % | ||
|---|---|---|---|
| Age | 30.38±4.96 | Multiparous (n, %) | 41/65; 63.1% |
| Gestational week | 27.55±1.15 | ||
| BMI, before pregnancy | 28.25±8.48 | BMI ≥35 before pregnancy | 11/62; 17.7% |
| BMI, at assessment | 30.88±7.73 | BMI ≥35 at assessment | 14/63; 22.2% |
| ISI (M±SD) | 10.86±6.26 | ISI ≥ 10 | 35/65; 53.8% |
| Mean sleep latency | 30.08±26.55 mins | Sleep Onset Insomnia | 19/65; 29.2% |
| EPDS (M±SD) | 6.57±4.63 | EPDS ≥ 13 | 12.3% |
| CAMS-R(M±SD) | 35.08±6.29 | ||
| Race | |||
| White | 43/64; 67.2% | ||
| Black | 13/64; 20.3% | ||
| Middle Eastern or Arab | 3/64; 4.7% | ||
| Hispanic or Latinx | 2/3.1; 3.7% | ||
| Mixed | 3/64; 4.7% | ||
| Relationship Status | |||
| Single | 3/65; 4.6% | ||
| In relationship, unmarried | 9/65; 13.8% | ||
| Married | 52/65; 80.0% | ||
| Separated or divorced | 1/65; 1.5% |
Note: BMI = body mass index (kg/m2), derived from electronic medical records; Poverty = <$20,000 in annual household income; ISI = insomnia severity index; EPDS = Edinburgh postnatal depression scale; Suicidality assessed by EPDS item #10; CAMS-R = cognitive and affective mindfulness scale, revised (12 items); CAMS-RM = cognitive and affective mindfulness scale, revised and modified (10 items); PSAS-C = presleep arousal scale, cognitive factor.
Mindfulness, nocturnal rumination, insomnia, and depression in pregnancy
See Table 1 for descriptives for insomnia, depression, nocturnal rumination, and mindfulness measures. Over half of the sample endorsed clinical insomnia (53.8%) and 29.2% reported sleep onset insomnia symptoms. Regarding depression, 12.3% screened positive for major depression. Important to emphasize here is that all depressed participants screened positive for clinical insomnia. Another way of looking at it, 22.9% of insomnia participants screened positive for major depression (n=8/35), whereas no good sleepers were depressed (n=0/30).
Next, we explored zero-order correlations among everyday mindfulness, nocturnal rumination, insomnia symptoms, and depressive symptoms (Table 2), which revealed strong bivariate associations among predictors and outcomes. For descriptive purposes regarding group differences, we compared women high vs. low in mindfulness on nocturnal rumination, insomnia, and depression (Figure 1). Highly mindful women, relative to those low in mindfulness, reported significantly lower levels of nocturnal rumination (M±SD: 15.31±5.67 vs. 22.33±6.42, t[63]=−4.67, p<.001, Cohen’s d=1.16), insomnia symptoms (7.50±4.47 vs. 14.12±6.07, t[63]−4.99, p=<.001, Cohen’s d=1.24), and depressive symptoms (3.94±3.30 vs. 9.12±4.31, t[63]=−5.43, p<.001, Cohen’s d=1.35). All effect sizes were large.
Table 2.
Zero-order correlations among everyday mindfulness, nocturnal rumination, insomnia, and depression
Note: CAMS-RM = cognitive and affective mindfulness scale, revised and modified (10 items); PSAS-C = presleep arousal scale, cognitive factor; ISI = insomnia severity index; EPDS = Edinburgh postnatal depression scale;
p<.01;
p<.001.
Figure 1.
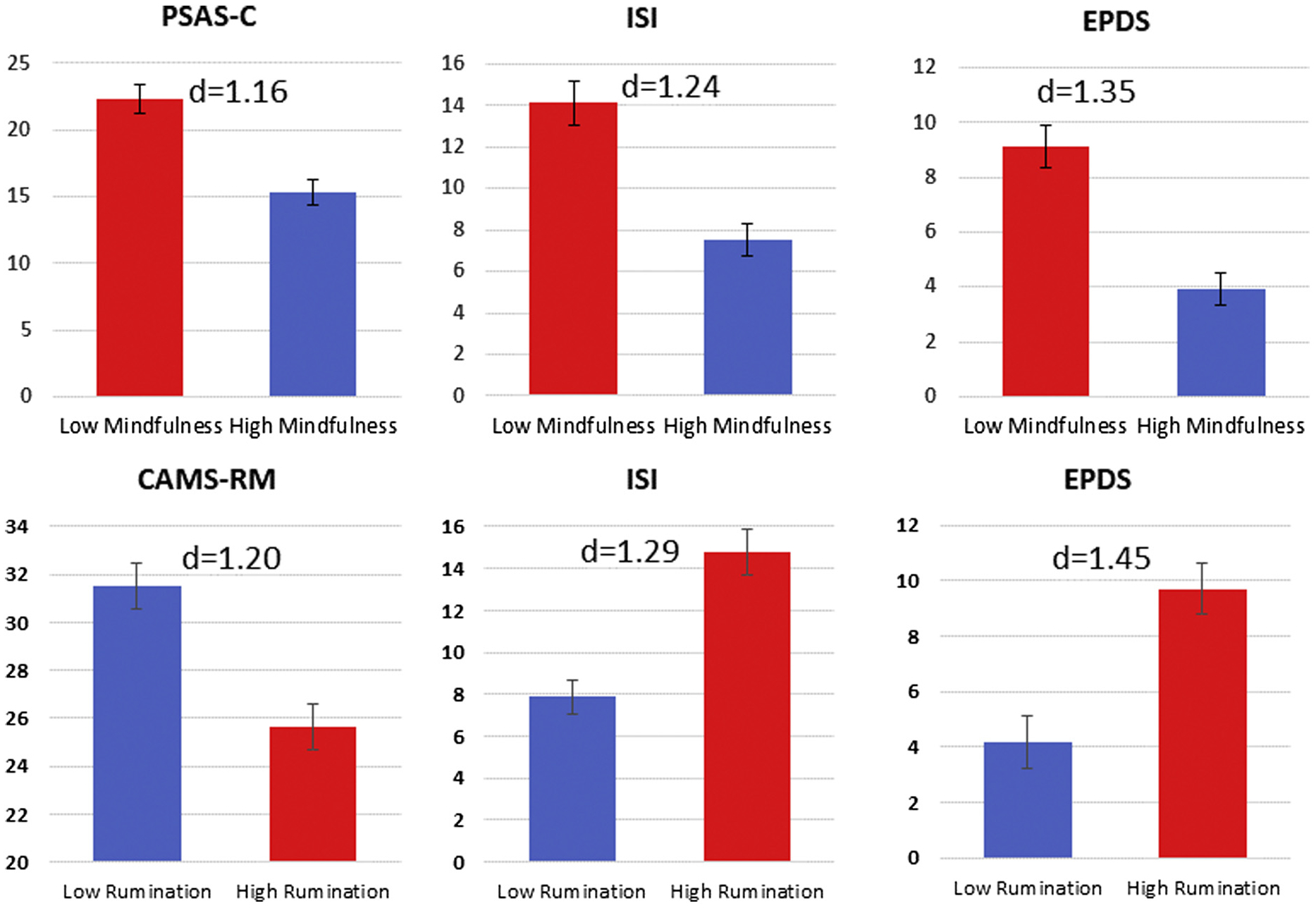
Group differences in symptoms of insomnia and depression based on mindfulness and nocturnal rumination (means, standard errors, and Cohen’s d effect sizes). Note. PSAS-C = presleep arousal scale, cognitive factor; High rumination = PSAS-C > 19; Low rumination = PSAS-C ≤ 19; ISI = insomnia severity index; EPDS = Edinburgh postnatal depression scale; CAMS-RM = cognitive and affective mindfulness scale, revised and modified (10-item version); High mindfulness = CAMS-RM > 28; Low mindfulness ≤ 28. d = Cohen’s d effect size.
Comparisons of high vs. low ruminators also revealed large group differences (Figure 1). Specifically, high ruminators, relative to low ruminators, reported lower mindfulness levels (25.61±4.38 vs. 31.51±5.41, t[63]=−4.72, p<.001, Cohen’s d=1.20) as well as greater insomnia symptoms (14.79±5.71 vs. 7.89±4.93, t[63]=5.22, p<.001, Cohen’s d=1.29) and depressive symptoms (9.71±4.26 vs. 4.19±3.31, t[63]=5.89, p<.001, Cohen’s d=1.45).
Specificity of associations for mindfulness and rumination with insomnia and depression
We then examined whether mindfulness and nocturnal rumination were independently related to insomnia and depression while controlling for potential confounders. First, we regressed insomnia symptoms on mindfulness and rumination while controlling for poverty and depression status (Table 3). Our model accounted for 56% of the variance in insomnia symptoms. Mindfulness (β=−.24, p=.03) and nocturnal rumination (β .38, p<.01) were each independently associated with insomnia in the expected directions. In addition, a positive depression status corresponded to scoring 5.39 points higher on our insomnia symptoms measure (p<.01) relative to nonde-pressed women.
Table 3.
Multivariate linear regression models predicting insomnia and depressive symptoms as predicted by mindfulness, nocturnal rumination, and relevant sociodemographic factors
| Outcome | Predictors | b | β | p |
|---|---|---|---|---|
| ISI | – | |||
| F=21.35, p<.001 | Poverty | 2.75 | .15 | .09 |
| Adjusted R2=.56 | CAMS-RM | −.26 | −.24 | .03 |
| PSAS-C | .34 | .38 | <.01 | |
| EPDS ≥ 13 | 5.39 | .29 | <.01 | |
| EPDS | ||||
| F=14.92, p<.001 | Poverty | 2.12 | .15 | .13 |
| Adjusted R2=.57 | Medicaid | −1.76 | −.17 | .13 |
| CAMS-RM | −.33 | −.41 | <.001 | |
| PSAS-C | .23 | .35 | <.01 | |
| ISI ≥ 10 | −.71 | −.15 | .18 | |
| SOI | 3.42 | .34 | <.01 |
Note: ISI = insomnia severity index; ISI ≥ 10 indicates positive insomnia status; Poverty = <$20,000 in annual household income CAMS-R = cognitive and affective mindfulness scale – revised, 10-item version; PSAS, Cognitive = presleep arousal scale, cognitive factor; EPDS = Edinburgh postnatal depression scale; EPDS ≥ 13 indicates positive major depression status; SOI = sleep onset insomnia symptoms, i.e., inability to fall asleep within 30 minutes at least 3 nights per week over the past month.
Finally, we regressed depressive symptoms on nocturnal rumination and mindfulness while controlling for poverty, Medicaid coverage, insomnia status, and sleep onset insomnia (Table 3). The model accounted for 57% of the variance in depression. Similar to our previous model, mindfulness (β=−.41, p<.001) and nocturnal rumination (β=.35, p<.01) were independently associated with depression in the expected directions. Notably, pregnant women with sleep onset insomnia scored 3.42 points higher on our depressive symptoms measure (p<.01) compared with those without sleep onset insomnia symptoms.
Discussion
In a sample of 65 women in mid-to-late pregnancy, mindfulness and nocturnal rumination shared a strong inverse relationship such that women low in mindfulness ruminated substantially more at night while trying to fall asleep compared with highly mindful women. This is consistent with previous reports of negative associations between mindfulness and other forms of cognitive-emotional arousal.18,24 Importantly, pregnant women (irrespective of insomnia or depression symptoms) reported especially high levels of nocturnal rumination on par with levels reported by clinical populations with insomnia, depression, and other rumination-laden conditions.33–36 To the contrary, everyday mindfulness levels reported by pregnant women were consistent with levels reported by the broader US adult population.24 Despite the close connection between rumination and everyday mindfulness, it is possible that rumination as a maladaptive stress-coping strategy increases during pregnancy, whereas one’s otherwise mindful approach to daily life (or lack thereof) remains relatively unchanged during pregnancy.
Everyday mindfulness, nocturnal rumination, insomnia, and depression in pregnancy
Rates of clinically significant insomnia and depression in our study were consistent with other studies of pregnant women, which are higher than rates found in the broader US adult population.37,38 Importantly, everyday mindfulness and nocturnal rumination were independently associated with insomnia and depression in our sample. Specifically, highly ruminative pregnant women reported greater insomnia and depressive symptoms, even when controlling for sociodemographic factors and other symptoms. These findings support previous reports on perinatal rumination and worry, insomnia, and depression.3,9 Nearly half of the sample was identified as having clinically significant presleep cognitive arousal based on empirically derived cutoffs linked to clinical morbidities.27 These data suggest that nocturnal rumination is a widespread maladaptive coping strategy in mid-to-late pregnancy, which may contribute to the high rates of insomnia and depression during this period.
By comparison, highly mindful pregnant women reported more normal sleep and mood than women low in mindfulness. Importantly, these positive health associations were independent of rumination in our study. Previous studies have shown that cultivating mindfulness reduces ruminative thought processes6,35 and that reducing rumination through formal mindfulness practice mediates the alleviation of depressive symptoms.39 These data suggest that living mindfully may improve health and wellbeing partly through the decreased automaticity of ruminating on stressors. But our cross-sectional data indicate that mindfulness also shares independent—and potentially protective—associations with stress-related conditions such as insomnia and depression. Prospective research is needed to determine whether mindfulness practice promotes good sleep and a healthy mind during pregnancy and postpartum via two nonexclusive pathways: (1) directly, through living in the moment with unconditional self-acceptance and compassion, and (2) indirectly, by offering a more adaptive approach to coping with stress than reliance on ruminative thinking. Given the high rates of stress and rumination during pregnancy,1,3 cultivating mindfulness during the perinatal period has potential to prevent or alleviate harmful perinatal complications.
Can cultivating mindfulness reduce health consequences associated with perinatal stress?
Pregnancy is a stressful life event, which can be complicated by issues relating to medical appointments and testing, fetal health concerns, fear of childbirth, pregnancy complications, and myriad other factors.1,13,40 Maternal psychological stress has been linked to not only pregnancy complications but also to unfavorable fetal and child development.40,41 Notably, however, the manner in which individuals respond to stress largely mediates the effects of the exposure on health outcomes.7,42 In the general adult population, a burgeoning literature of prospective and experimental research shows that ruminating in response to stress is a key behavior that increases mood and sleep pathology.7,29,43–46 However, growing evidence suggests similar patterns in perinatal women and mothers of young children such that maternal rumination is associated with mental illness in both mother and child,14,17,47 poor mother-fetal attachment, and mother-child bonding,14,16,48,49 and impaired problem-solving and parental responsiveness.14,15
Evidence from our study shows that rumination and mindfulness are inversely related to one another and that they have independent associations with insomnia and depression, thereby reflecting a complex interplay between pregnancy-related sleep, mood, and stress-response. Mindfulness intervention trials show that clinical applications of meditation and mindfulness-based stress reduction (MBSR) strategies decrease ruminative and perseverative thinking.6,50,51 Results from the present study, along with the success of these previous trials, suggest that the corrosive effects of maternal stress and rumination on sleep and mental health could potentially be alleviated by mindfulness-based stress-coping strategies. In the opposite direction, however, it is possible that a mindful approach to living can be derailed by excessive rumination; especially in this population as rumination levels appear high in mid-to-late pregnancy. Rumination is a common automatic response to stress exposure, but if a metacognitive shift is engaged allowing for intentional awareness on these negative thoughts and feelings with compassion and nonjudgment, then negative emotionality and allostatic overload can be minimized.
Ong et al. have augmented cognitive-behavioral therapy for insomnia (CBTI)—gold standard and recommended first-line treatment for insomnia disorder52—with MBSR-based strategies to enhance both rumination and sleep outcomes in people with insomnia.35,50,53,54 Although standard CBTI has minimal effects on ruminative thinking,55 mindfulness-augmented CBTI and mindfulness-based therapy for insomnia (altered CBTI+MBSR-based strategies, see Ong, 2017 for details54) substantially decreases sleep and nocturnal rumination as measured by the PSAS-C (reduction of 4.6 points).35 In a follow-up randomized controlled trial (RCT) of two mindfulness interventions (MBTI vs. MBSR vs. control), presleep arousal was reduced and stayed improved over long-term follow-up.50 A benefit of MBTI over MBSR, however, was that long-term sleep outcomes were superior in the MBTI condition. Similar findings have been replicated in a more recent RCT.53 These data suggest that augmenting cognitive and behavioral interventions for insomnia with formal mindfulness practice successfully reduces key symptoms that are undertreated by standard CBTI.
Given the high levels of rumination and depression in pregnant women with insomnia, mindfulness interventions have immense potential for improving maternal health. Important to emphasize is that over half of the women in our study had clinical insomnia, and nearly a quarter of these insomniacs screened positive for major depression (whereas no good sleepers were depressed). These data, combined with the extant literature, highlight the importance of good sleep in pregnancy for mental health. Despite this, only one RCT using CBTI has been published on prenatal insomnia, which shows that CBTI significantly improves sleep during pregnancy and has modest therapeutic benefit for depressive symptoms.56 Important to emphasize here is that no over-the-counter or prescription sleep aids are approved for safe use in pregnant women, thereby leaving this highly afflicted population with few treatment options. As pregnant women report high levels of both insomnia and rumination, incorporating mindfulness interventions with insomnia treatment has potential to enhance outcomes. Research is needed to evaluate whether mindfulness-based interventions can successfully treat (or even prevent) these highly prevalent and serious perinatal complications by increasing mindful strategies for coping with stress and reducing rumination in expecting and new mothers.
Limitations
Our study findings should be interpreted in the context of methodological limitations. Namely, this study was cross-sectional. Thus, directionality cannot be established, but rather only considered within the context of the extant literature. Along these lines, women in our sample comprised a limited range in gestational age. Owing to the cross-sectional design and limited range in gestational age, we were unable to examine whether symptoms and associations among symptoms change throughout pregnancy. Future studies should examine the extent to which mindful living, ruminative thinking, and symptoms of insomnia and depression change across the perinatal periods and how associations among these factors evolve over time. Additionally, the study sample was relatively small. Although effect sizes were large and thus we did not likely suffer from limited statistical power, these results may not represent symptom levels or associations in a larger more representative pregnant population.
Another limitation regards the self-report nature of sleep. While patient impressions of sleep are critical and best represent the clinical experience of insomnia, self-reported sleep parameters can be inconsistent with objective data via polysomnography and wearable technology. Prospective research characterizing possible changes in mindfulness and rumination across pregnancy and the first postpartum year is needed to better understand both protective and etiological factors in the development of insomnia and depression. Assessing sleep with both objective and self-report measures will offer a more comprehensive picture of how sleep quality changes across the perinatal period and relates to changes in stress and mood.
Conclusions
Ruminating at night is a common behavior among pregnant women, especially for those with elevated insomnia and depressive symptoms. Importantly, highly ruminative pregnant women approach everyday life and stress less mindfully than those with low rumination. Navigating the perinatal period and everyday living with intentional awareness, self-compassion, and nonjudgment is associated with better mood and sleep in this period. Research is needed to characterize the prospective associations among mindfulness, rumination, insomnia, and depression across pregnancy and after childbirth. Importantly, these factors may not only affect maternal health but likely also affect children and family relationships. Better understanding how these constructs evolve and interact during these periods may inform the timing of treatment and identify therapeutic targets to improve maternal and child health and relationship quality. Evidence-based mindfulness interventions have rapidly emerged for insomnia54,57 and depression,10,58 and recent findings show promise for these approaches to improve stress regulation and mood in perinatal women.18 Additional controlled trials are needed to determine whether cultivating mindfulness in the perinatal period can reduce rumination to prevent perinatal insomnia and depression or to improve outcomes over available interventions.
Financial support:
This study was funded by the American Academy of Sleep Medicine (198-FP-18; PI: Kalmbach). Dr. Cheng’s effort was funded by the National Heart, Lung, & Blood Institute (K23 HL13866, PI: Cheng).
Disclosure statement: Dr. Kalmbach has received research support from Merck & Co. Dr. Roth. has received research support from Aventis, Cephalon, Glaxo Smith Kline, Neurocrine, Pfizer, Sanofi, Schering-Plough, Sepracor, Somaxon, Syrex, Takeda, TransOral, Wyeth and Xenoport and has acted as a consultant for Abbott, Acadia, Acoglix, Actelion, Alchemers, Alza, Ancil, Arena, Astra Zeneca, Aventis, AVER, BMS, BTG, Cephalon, Cypress, Dove, Elan, Eli Lilly, Evotec, Forest, Glaxo Smith Kline, Hypnion, Impax, Intec, Intra-Cellular, Jazz, Johnson & Johnson, King, Lundbeck, McNeil, Medici Nova, Merck & Co., Neurim, Neurocrine, Neurogen, Novartis, Orexo, Organon, Prestwick, Procter-Gamble, Pfizer, Purdue, Resteva, Roche, Sanofi, Schering-Plough, Sepracor, Servier, Shire, Somaxon, Syrex, Takeda, TransOral, Vanda, Vivometrics, Wyeth, Yamanuchi, and Xenoport. Dr. Cheng has received research support from Harmony Biosciences. Dr. Drake has received research support from Merck & Co., Eisai Co., Aladdin Dreamer, Jazz, Actelion, and Teva; and has served on speakers bureau for Merck & Co. No other financial or non-financial interests exist. The other authors declare that they have no conflict of interest.
Footnotes
ClinicalTrials.gov Identifier: NCT03596879
References
- 1.Geller PA. Pregnancy as a stressful life event. CNS Spectr. 2004;9(3):188–197. [DOI] [PubMed] [Google Scholar]
- 2.Dørheim SK, Bjorvatn Br, Eberhard-Gran M. Insomnia and depressive symptoms in late pregnancy: a population-based study. Behav Sleep Med. 2012;10(3): 152–166. [DOI] [PubMed] [Google Scholar]
- 3.Kalmbach DA, Cheng P, Ong JC, et al. Depression and suicidal ideation in pregnancy: Exploring relationships with insomnia, short sleep, and nocturnal rumination. Sleep Med. 2019;65:62–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christian LM, Carroll JE, Porter K, Hall MH. Sleep quality across pregnancy and post-partum: effects of parity and race. Sleep Health. 2019;5(4):327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pillai V, Drake CL. Sleep and repetitive thought: the role of rumination and worry in sleep disturbance In: Babson KA, Feldner MT, eds. Sleep and affect. London: Elsevier; 2015:201–225. [Google Scholar]
- 6.Deyo M, Wilson KA, Ong J, Koopman C. Mindfulness and rumination: does mindfulness training lead to reductions in the ruminative thinking associated with depression? EXPLORE. 2009;5(5):265–271. [DOI] [PubMed] [Google Scholar]
- 7.Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. 2008;3(5):400–424. [DOI] [PubMed] [Google Scholar]
- 8.Batterham PJ, Glozier N, Christensen H. Sleep disturbance, personality and the onset of depression and anxiety: prospective cohort study. Aust N Z J Psychiatr. 2012;46(11):1089–1098. [DOI] [PubMed] [Google Scholar]
- 9.Swanson LM, Pickett SM, Flynn H, Armitage R. Relationships among depression, anxiety, and insomnia symptoms in perinatal women seeking mental health treatment. J Women’s Health. 2011;20(4):553–558. [DOI] [PubMed] [Google Scholar]
- 10.Segal ZV, Williams M, Teasdale J. Mindfulness-based cognitive therapy for depression. 2nd ed. New York: Guilford Publications; 2018. [Google Scholar]
- 11.Ong JC, Ulmer CS, Manber R. Improving sleep with mindfulness and acceptance: a metacognitive model of insomnia. Behav Res Ther. 2012;50(11):651–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. 2nd ed. New York: Bantam Books; 2013. [Google Scholar]
- 13.Martini J, Asselmann E, Einsle F, Strehle J, Wittchen H-U. A prospective-longitudinal study on the association of anxiety disorders prior to pregnancy and pregnancy-and child-related fears. J Anxiety Disord. 2016;40:58–66. [DOI] [PubMed] [Google Scholar]
- 14.DeJong H, Fox E, Stein A. Rumination and postnatal depression: A systematic review and a cognitive model. Behav Res Ther. 2016;82:38–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Mahen HA, Boyd A, Gashe C. Rumination decreases parental problem-solving effectiveness in dysphoric postnatal mothers. J Behav Ther Exp Psychiatry. 2015;47:18–24. [DOI] [PubMed] [Google Scholar]
- 16.Tester-Jones M, Karl A, Watkins E, O’Mahen H. Rumination in dysphoric mothers negatively affects mother–infant interactions. J Child Psychol Psychiatry. 2017;58(1):38–45. [DOI] [PubMed] [Google Scholar]
- 17.O’Mahen HA, Flynn HA, Nolen-Hoeksema S. Rumination and interpersonal functioning in perinatal depression. J Soc Clin Psychol. 2010;29(6):646–667. [Google Scholar]
- 18.Dhillon A, Sparkes E, Duarte RV. Mindfulness-based interventions during pregnancy: a systematic review and meta-analysis. Mindfulness. 2017;8(6): 1421–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Wom Ment Health. 2008;11(1):67–74. [DOI] [PubMed] [Google Scholar]
- 20.Dunn C, Hanieh E, Roberts R, Powrie R. Mindful pregnancy and childbirth: effects of a mindfulness-based intervention on women’s psychological distress and well-being in the perinatal period. Arch Wom Ment Health. 2012;15(2):139–143. [DOI] [PubMed] [Google Scholar]
- 21.Guardino CM, Dunkel Schetter C, Bower JE, Lu MC, Smalley SL. Randomised controlled pilot trial of mindfulness training for stress reduction during pregnancy. Psychology & health. 2014;29(3):334–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goodman JH, Guarino A, Chenausky K, et al. CALM Pregnancy: results of a pilot study of mindfulness-based cognitive therapy for perinatal anxiety. Arch Wom Ment Health. 2014;17(5):373–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Felder JN, Laraia B, Coleman-Phox K, et al. Poor sleep quality, psychological distress, and the buffering effect of mindfulness training during pregnancy. Behav Sleep Med. 2018;16(6):611–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feldman G, Hayes A, Kumar S, Greeson J, Larenceau J-P. Mindfulness and emotion regulation: The development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). J Psychopathol Behav Assess. 2007;29(3):177. [Google Scholar]
- 25.Mindell JA, Jacobson BJ. Sleep disturbances during pregnancy. J Obstet Gynecol Neonatal Nurs. 2000;29(6):590–597. [DOI] [PubMed] [Google Scholar]
- 26.Nicassio PM, Mendlowitz DR, Fussell JJ, Petras L. The phenomenology of the pre-sleep state: the development of the pre-sleep arousal scale. Behav Res Ther. 1985;23(3):263–271. [DOI] [PubMed] [Google Scholar]
- 27.Puzino K, Frye SS, Vgontzas AN, Fernandez-Mendoza J. Am I (hyper) aroused or anxious? Clinical significance of pre-sleep somatic arousal in young adults. J Sleep Res. 2019:e12829. [DOI] [PubMed] [Google Scholar]
- 28.Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psycho-metric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kalmbach DA, Pillai V, Drake CL. Nocturnal insomnia symptoms and stress-induced cognitive intrusions in risk for depression: A 2-year prospective study. PLoS One. 2018;13(2):e0192088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 31.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6): 782–786. [DOI] [PubMed] [Google Scholar]
- 32.Matthey S, Henshaw C, Elliott S, Barnett B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale–implications for clinical and research practice. Arch Wom Ment Health. 2006;9(6):309–315. [DOI] [PubMed] [Google Scholar]
- 33.Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. 2003;65(2):259–267. [DOI] [PubMed] [Google Scholar]
- 34.Smith MS, Smith MT, Perlis ML, Giles DE, Carmody TP. Sleep quality and presleep arousal in chronic pain. J Behav Med. 2000;23(1):1–13. [DOI] [PubMed] [Google Scholar]
- 35.Ong JC, Shapiro SL, Manber R. Combining mindfulness meditation with cognitive-behavior therapy for insomnia: a treatment-development study. Behav Ther. 2008;39(2):171–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatr Hum Dev. 2010;41(2):156–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mindell JA, Cook RA, Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. 2015;16(4):483–488. [DOI] [PubMed] [Google Scholar]
- 38.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol. 2004;103(4): 698–709. [DOI] [PubMed] [Google Scholar]
- 39.Hawley LL, Schwartz D, Bieling PJ, et al. Mindfulness practice, rumination and clinical outcome in mindfulness-based treatment. Cogn Ther Res. 2014;38(1):1–9. [Google Scholar]
- 40.Woods SM, Melville JL, Guo Y, Fan M-Y, Gavin A. Psychosocial stress during pregnancy. Am J Obstet Gynecol. 2010;202(1):61 e1–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mulder EJH, Robles de Medina PG, Huizink AC, Van den Bergh BRH, Buitelaar JK, Visser GHA. Prenatal maternal stress: effects on pregnancy and the (unborn) child. Early Hum Dev. 2002;70(1–2):3–14. [DOI] [PubMed] [Google Scholar]
- 42.Pillai V, Roth T, Mullins HM, Drake CL. Moderators and mediators of the relationship between stress and insomnia: stressor chronicity, cognitive intrusion, and coping. Sleep. 2014;37(7):1199–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kalmbach DA, Pillai V, Ciesla JA. The correspondence of changes in depressive rumination and worry to weekly variations in affective symptoms: A test of the tripartite model of anxiety and depression in women. Aust J Psychol. 2016;68(1): 52–60. [Google Scholar]
- 44.Zoccola PM, Dickerson SS, Lam S. Rumination predicts longer sleep onset latency after an acute psychosocial stressor. Psychosom Med. 2009;71(7):771–775. [DOI] [PubMed] [Google Scholar]
- 45.Singareddy R, Vgontzas AN, Fernandez-Mendoza J, et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med. 2012;13(4):346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pillai V, Steenburg LA, Ciesla JA, Roth T, Drake CL. A seven day actigraphy-based study of rumination and sleep disturbance among young adults with depressive symptoms. J Psychosom Res. 2014;77(1):70–75. [DOI] [PubMed] [Google Scholar]
- 47.Gatét MA, Watkins ER, Simmons JG, et al. Maternal parenting behaviors and adolescent depression: The mediating role of rumination. J Clin Child Adolesc Psychol. 2013;42(3):348–357. [DOI] [PubMed] [Google Scholar]
- 48.Müller D, Tiesmann T, Havemann B, Michalak J, Seehagen S. Ruminative thinking as a predictor of perceived postpartum mother–infant bonding. Cogn Ther Res. 2013;37(1):89–96. [Google Scholar]
- 49.Schmidt D, Seehagen S, Vocks S, Schneider S, Tiesmann T. Predictive importance of antenatal depressive rumination and worrying for maternal–Foetal attachment and maternal well-being. Cogn Ther Res. 2016;40(4):565–576. [Google Scholar]
- 50.Ong JC, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt JK. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37(9): 1553–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12. [DOI] [PubMed] [Google Scholar]
- 52.Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2): 125–133. [DOI] [PubMed] [Google Scholar]
- 53.Ong JC, Xia Y, Smith-Mason CE, Manber R. A randomized controlled trial of mindfulness meditation for chronic insomnia: Effects on daytime symptoms and cognitive-emotional arousal. Mindfulness. 2018;9(6):1702–1712. [Google Scholar]
- 54.Ong JC. Mindfulness-based therapy for insomnia. Washington DC: American Psychological Association; 2017. [Google Scholar]
- 55.Kalmbach DA, Cheng P, Arnedt JT, et al. Treating Insomnia Improves Depression, Maladaptive Thinking, and Hyperarousal in Postmenopausal Women: Comparing Cognitive-Behavioral Therapy for Insomnia (CBTI), Sleep Restriction Therapy, and Sleep Hygiene Education. Sleep Med. 2019;55:124–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Manber R, Bei B, Simpson N, et al. Cognitive Behavioral Therapy for Prenatal Insomnia: A Randomized Controlled Trial. Obstet Gynecol. 2019;133(5):911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Orzech CP, Moorcroft WH. Mindfulness for Insomnia: A Four-Week Guided Program to Relax Your Body, Calm Your Mind, and Get the Sleep You Need. Oakland, CA: New Harbinger Publications; 2019. [Google Scholar]
- 58.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010;78(2):169. [DOI] [PMC free article] [PubMed] [Google Scholar]


