The global pandemic of severe acute respiratory coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), continues to spread around the world, having infected more than 1·8 million people and causing over 100 000 deaths as of April 13, 2020. High-quality evidence showing the effectiveness of treatments for COVID-19 is scarce, but over 400 studies are now registered in ClinicalTrails.gov testing a range of therapies, including immunosuppressants and the anti-malarial drugs chloroquine and hydroxychloroquine. One therapy being tested is convalescent plasma, a type of passive antibody therapy, in which blood plasma is isolated from people who have recovered from the disease of interest and is administered to those with the disease to suppress viraemia and improve clinical symptoms.
By the 1930s, serum therapy was widely used to treat a range of infectious diseases, such as scarlet fever and pneumococcal pneumonia; however, its use had declined by the middle of the 20th century as a result of the development of antimicrobials. The interest in passive antibody therapy has been renewed periodically, especially when new epidemics or pandemics emerge, including previous coronavirus outbreaks—SARS in 2002–04 and Middle East respiratory syndrome in 2012. Promise was shown for SARS, with a 2004 study done in Hong Kong showing earlier discharge from hospital and lower mortality in patients given convalescent plasma earlier than those who were given it later. For other infectious diseases, positive results led the WHO to publish guidance on the use of the treatment for Ebola virus disease, and treatment benefits have been shown in terms of lower morality in patients with pandemic 2009 influenza A H1N1 virus infection. However, definitive clinical evidence showing the efficacy of convalescent plasma is scarce.
Initial findings for convalescent plasma therapy for the treatment of COVID-19 are encouraging but have so far only come from two small studies done in China; a case series of five patients with critical COVID-19 receiving mechanical ventilation, and a pilot study done in ten patients with severe COVID-19. In both studies, convalescent plasma therapy was shown to be safe and clinical outcomes improved, including fever, Sequential Organ Failure Assessment score, and respiratory symptoms, in some cases within 1–3 days of treatment. The US Food and Drug Administration (FDA) has approved the use of convalescent plasma under compassionate use rules, but randomised controlled trials are now needed to provide clinical evidence. Three trials initiated by the US National COVID-19 Convalescent Plasma Project are currently being evaluated by the FDA to test the activity and safety of convalescent plasma in three groups of patients: people who have been exposed to the virus and are at high risk of developing severe COVID-19 (NCT04323800); hospitalised patients with acute respiratory symptoms (NCT04325672); and patients with severe COVID-19 who are mechanically ventilated. Other trials are also planned or underway in China, Colombia, Iran, Mexico, and the Netherlands.
The success of convalescent plasma therapy hinges on the donation of plasma by people who have recovered from COVID-19 and have high concentrations of anti-SARS-CoV-2 antibodies, and on the safe preparation of serum to eliminate potential risk factors, such as the transmission of viruses via transfusion. Many donors are needed, as the plasma from one donor can only be used to treat a few patients. In the USA, the Red Cross—in collaboration with the FDA—has published a call for donors, and each country will need to do similar if this therapy is to be used to treat the most severely ill patients. An additional use for anti-SARS-CoV-2 antibodies isolated from plasma is the development of a concentrated therapy known as hyperimmune globulin, in which the antibodies from many donors are pooled. Such hyperimmune therapies could offer a more consistent and predictable therapeutic option, with companies such as Takeda and CSL Behring planning to test these therapies in clinical trials.
The current pandemic provides the greatest opportunity yet to develop convalescent plasma therapy into a viable treatment option for COVID-19 while a vaccine is developed. The global reach of this pandemic, and the desperate need for effective treatments for patients with severe and critical COVID-19, is driving both basic and clinical research at an unprecedented rate. Time will tell if convalescent plasma can improve outcomes for patients in a meaningful way, the need for high-quality research in this arena is vital.
For podcasts discussing the COVID-19 pandemic, including the use of convalescent plasma, see thelancet.com/the-lancet-voice
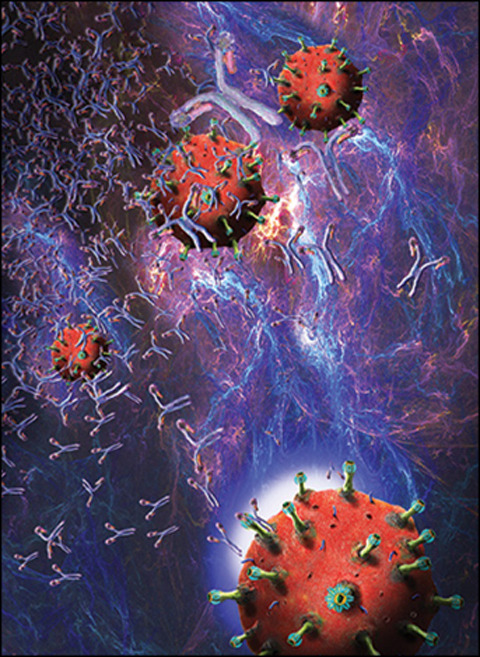
© 2020 Keith Chambers/Science Photo Library


