Structured Abstract
Objectives:
To examine differences in family environment and associations between family environment and key speech, language, and cognitive outcomes in samples of children with normal hearing and deaf and hard-of-hearing (DHH) children who use hearing aids and cochlear implants.
Design:
Thirty families of children with normal hearing (n = 10), hearing aids (n = 10), or cochlear implants (n = 10) completed questionnaires evaluating executive function, social skills, and problem behaviors. Children’s language and receptive vocabulary were evaluated using standardized measures in the children’s homes. In addition, families were administered a standardized in-home questionnaire and observational assessment regarding the home environment.
Results:
Family environment overall was similar across hearing level and sensory aid, although some differences were found on parental responsivity and physical environment. The level of supportiveness and enrichment within family relationships accounted for much of the relations between family environment and the psychosocial and neurocognitive development of DHH children. In contrast, the availability of objects and experiences to stimulate learning in the home was related to the development of spoken language.
Conclusions:
Whereas broad characteristics of the family environments of DHH children may not differ from those of hearing children, variability in family functioning is related to DHH children’s at-risk speech, language, and cognitive outcomes. Results support the importance of further research to clarify and explain these relations, which might suggest novel methods and targets of family-based interventions to improve developmental outcomes.
Keywords: Family environment, cochlear implant, hearing aid, language, executive function
Short Summary
Family environment and at-risk developmental outcomes were examined in children with normal hearing, hearing aids, and cochlear implants. Family environment overall was similar across groups, although differences were found on parental responsivity and physical environment. The supportiveness and enrichment of family relationships accounted for most of the relations observed between family environment and the social-behavioral and neurocognitive development of deaf and hard-of-hearing children. In contrast, the availability of objects and experiences to stimulate learning in the home were related to the development of spoken language. Results suggest novel targets for future interventions at the level of the family environment.
Introduction
Permanent childhood hearing loss presents challenges for both the family and child. For this reason, hearing-related challenges pose risks for child outcomes in various domains, including spoken language (Geers & Brenner 2003; Holt & Svirsky 2008; Niparko et al., 2010; Geers et al. 2011; Cruz et al. 2013), neurocognition (Surowiecki et al., 2002; Hauser et al. 2008; Pisoni et al. 2010; Kronenberger et al. 2013), and psychosocial development (Moeller, 2007; Freeman et al. 2017; Castellanos et al. 2018). Variability in how families adapt to these challenges is routinely observed with some families adapting well and others demonstrating greater difficulty. Explaining variability in family and child outcomes are important first steps in understanding family adaptation to hearing loss, in explaining the role of the family in child outcomes, and developing novel family-centered interventions that promote optimal outcomes. The purpose of the current investigation is two-fold: 1) to describe the effects of hearing loss on family environment; and 2) to investigate the associations between family environment and child-related outcome measures in children with hearing loss.
This work is framed within a Social-Behavioral Risk (S-B-R) Model of development of children with hearing loss that is rooted in Systems Theory (Kazak 1989; Kronenberger & Pisoni in press). A Systems approach recognizes that development does not occur within a vacuum; instead, it views human development as part of an open-loop system, which occurs within rings of environmental influence, the most proximal and potent of which is the family (Kazak 1992). The S-B-R Model is Transactional (Sameroff & Chandler 1975), in that it emphasizes that development occurs within a series of bidirectional interactions between people in the family. The S-B-R Model is also Ecological (Bronfenbrenner 1977), meaning that development also occurs within interactions between people and their environments (Kronenberger & Pisoni in press).
Childhood hearing loss poses cascading neurodevelopmental challenges for children that extend beyond audibility (Flexer 2011). Childhood hearing loss interferes with spoken language development, as well as any social, neurocognitive, and emotional process mediated by language, including social understanding and perspective-taking, which are core underlying skills for social learning (e.g., Peterson & Siegal, 1999; Nikolopoulos et al. 2004; Peterson, 2004; Desjardin & Eisenberg 2007; Pisoni et al. 2008, 2010; Barker et al. 2009; Niparko et al. 2010; Teagle & Eskridge 2010). Speech communication - the primary mechanism through which family environment affects developmental outcomes - is disrupted and reorganized in hearing families of children with hearing loss (over 96% of children with hearing loss have hearing parents in the United States [Mitchell & Karchmer 2004]). Therefore, family influences on developmental outcomes are expected to differ in the presence of childhood hearing loss relative to its absence. The S-B-R Model posits that children primarily learn language through proximal parent-child interactions and that childhood hearing loss increases risk for poor language, psychosocial, and neurocognitive outcomes by interfering with these typical language-learning mechanisms. Families, children, and the broader social-developmental environment respond to challenges associated with hearing loss with behaviors, resources, and interventions that offer the potential for resilience, compensation, and positive outcomes.
Family environment includes the “patterns of activities, roles, and interpersonal relations experienced by the developing child” (Bronfenbrenner 1977, p. 22), and may be viewed as the most proximal of the concentric rings of environmental systems influences on young children (Bronfenbrenner 1977; Belsky 1981; Cicchetti & Rizley 1981; Cicchetti & Lynch 1993). Family influences on outcomes ranging from language to psychosocial adjustment may be affected by hearing loss as well as by intervention efforts including sensory aids and speech-language therapies. Degree of hearing loss and thus, sensory aid status, not only limits the amount of auditory information that a listener has access to, but also impacts the social interactions a child experiences. For example, Moeller and Tomblin (2015) have suggested that childhood hearing loss changes communication dynamics between children and caregivers, in addition to reducing access to language. Because children’s social experiences differ with hearing status and sensory aid use based on access to language and communication, differences in family environments are expected among children with normal hearing, deaf children who use cochlear implants, and children with less severe degrees of hearing loss who use hearing aids.
Several family-related influences on outcomes in deaf and hard-of-hearing (DHH) children have been investigated in prior research: family communication modality (e.g., Kirk et al. 2002; Geers et al. 2003; Holt & Svirsky 2008; Geers et al. 2011), family support given to the child (e.g., Nikolopoulos et al. 2004; Edwards et al. 2009), the family’s role in therapy (Bertram & Päd 1995; Moeller 2000), the family’s size and socioeconomic status (SES), the primary caregiver’s highest education level (Geers et al., 2003, 2011; Holt & Svirsky, 2008), maternal attachment and sensitivity (e.g., Lederberg & Mobley 1990; Pratt 1991; Pressman et al. 1999), maternal involvement and self-efficacy (Desjardin 2005; Desjardin & Eisenberg 2007), and maternal linguistic input (e.g., Desjardin & Eisenberg 2007; Desjardin et al. 2008). Results of these studies suggest that children have better spoken language outcomes when they are reared in family environments in which communication partners emphasize oral language, have families that are highly involved in therapy, and have smaller families with higher incomes. However, the effect of material resources (i.e., higher incomes) on spoken language development can be mediated by other factors, such as maternal language input (Hoff 2003). Children’s spoken language development tends to be facilitated by mothers’ use of higher-level facilitative language techniques, such as recasting (a form of modelling in which the child’s utterance is rephrased by adding new or different grammar or semantic information by the mother). Furthermore, mothers’ beliefs about their ability to support their child’s language development are positively related to their own use of higher-level language techniques with their children (Desjardin & Eisenberg 2007). These studies demonstrate significant family influences on cognitive, language, and psychosocial outcomes of children with cochlear implants and hearing aids.
Although prior research has investigated specific family attributes (such as SES) or aspects of parent-child relationships (maternal language) on developmental outcomes in DHH children with cochlear implants and hearing aids, relatively little prior research has investigated broad systems components of the family environment, such as how the family organizes its daily schedule and priorities, and how the members in the family relate to one another. In one such study, Holt et al. (2012) examined the contribution of family environment to individual differences in language, receptive vocabulary and executive function in 45 children with cochlear implants using the Family Environment Scale [FES – 4th Edition (Moos & Moos 2009)], a psychometrically sound, questionnaire-based measure of family environment. The FES measures interpersonal relationships, goals, activities, interests, structure and organization in the family. Higher receptive vocabularies were found in children whose families reported lower levels of behavioral control in the home (defined as the degree to which families employ set rules and actions for running family life, emphasize those rules inflexibly, and use an obvious hierarchy of power). Families that placed a higher emphasis on achievement had children with fewer executive function and working memory problems. Finally, families that placed a higher emphasis on organization in the home (defined as the level of importance placed on transparent organization and structure in planning family events and duties; focus on planning, clear expectations and neatness) had children with fewer problems with inhibitory control.
In a follow-up, Holt et al. (2013) reported that in preschool-age DHH children, supportive families and families with low levels of conflict (defined as how much open disagreement and anger are expressed among family members) had children with fewer behavioral problems related to emotional control. Families of school-age DHH children reported higher levels of behavioral control than those of preschool-age DHH children. More organized families of school-age DHH children had children with larger receptive vocabularies, and families with higher levels of control had school-age DHH children with smaller receptive vocabularies, supporting and extending previous findings (Holt et al. 2012). Higher degrees of structure and organization within the family unit promoted better receptive vocabulary development, whereas attempts to maintain internal family functioning through unbalanced behavioral control and rigidly fixed rules among parents might, in fact, have the opposite effect on vocabulary development. Finally, for school-age children, families with low conflict and high cohesiveness (defined as the amount of support family members give each other) had children with fewer problems related to inhibitory control.
These earlier studies suggest that family environment characteristics are associated with neurocognitive and spoken language outcomes in deaf children with cochlear implants and that the influence of family environment varies across developmental stage. Importantly, specific subdomains of executive function that are at high risk for delayed or deficient development in children with hearing loss who use cochlear implants (Beer et al. 2011; Holt et al. 2013; Kronenberger et al. 2014a,b) – inhibition and working memory – were associated with specific aspects of family environment.
Findings from samples of DHH children with cochlear implants do not address an understudied population of children with hearing loss: children with mild-to-severe degrees of permanent hearing loss who use hearing aids (Donahue 2007). Consistent with earlier work showing that mothers of children with profound hearing loss tend to use a higher proportion of directive utterances (phrases that contain instructions or corrections) than mothers of children with typical hearing (e.g., Vaccari & Marschark 1997), caregivers of toddlers with mild-to-severe hearing loss who use hearing aids used a higher proportion of directive utterances than those of typically hearing toddlers (Ambrose et al. 2015). Use of directive utterances was associated with poorer language outcomes in children who used hearing aids. Language outcomes in children with hearing aids were related to qualitative aspects of caregiver speech such as directive speech, rather than the quantity of speech that caregivers used (Ambrose et al. 2015). However, as with CI research, studies of the association of family factors and developmental outcomes have focused almost exclusively on parent-child interactions and language outcomes. No systematic research has investigated broad characteristics of family environment and language or neurocognitive outcomes in families of children who use hearing aids.
Most studies of DHH children have investigated audiological (McCreery et al. 2015; Walker et al. 2015), spoken language (Geers & Brenner 2003; Holt & Svirsky 2008; Geers et al. 2011), and neurocognitive (Pisoni et al. 2010; Kronenberger et al. 2013; Kronenberger et al. 2014a,b) characteristics of children with hearing loss. Much less is known about the family environments of DHH children with cochlear implants and hearing aids. Furthermore, family influences on important core language, neurocognitive, and psychosocial outcomes have received much less attention than other factors (e.g., hearing history, early language development). Given the importance of understanding biopsychosocial influences on key developmental outcomes at multiple levels of development ranging from the biological (sensory and neurological components) to the social (family, school, and societal components), investigation of the family environments of DHH children with cochlear implants and hearing aids is a very significant and understudied topic. Identifying how family environment is related to developmental outcomes is important for future intervention research, because whereas hearing history is not malleable, family environments can be altered with family-oriented programs (Hill & Balk 1987; Mills & Hansen 1991; Bruce & Emshoff 1992). The current investigation expands upon our previous work by examining family environment, as well as the influences of family environment on a diverse set of developmental outcomes in DHH children with cochlear implants or hearing aids. The purpose of the current investigation was two-fold: 1) to compare environments of families of young children with hearing loss who use sensory aids (i.e., HAs and CIs) to typically developing children; and 2) to identify family factors that are associated with language, psychosocial and neurocognitive development in children with CIs or HAs.
Method
Participants
Thirty 5- to 8-year-old children and their primary caregivers participated in this investigation: 10 children with normal hearing (NH Control group), 10 children with mild through moderately-severe sensorineural hearing loss who used hearing aids (HA group), and 10 children with severe-to-profound sensorineural hearing loss who used cochlear implants (CI group). All of the primary caregivers included in this investigation were mothers, except for two fathers of normal-hearing children. Inclusion criteria were as follows:
All Participants
Age 5–8 years
Use of spoken English as primary language
Availability of the primary caregiver to participate in research
No diagnosis of severe intellectual or neurological disability
HA Group
Bilateral permanent (sensorineural) mild to severe hearing loss: better ear pure-tone average ranged from 33 to 69 dB HL (re: ANSI 2004)
Use of bilateral hearing aids
Identified with hearing loss and enrolled in early intervention by age 3 years, 6 months;
Enrolled in a rehabilitative program or living in a home environment that encourages the development and use of speech and spoken language skills
CI Group
Bilateral permanent (sensorineural) severe to profound hearing loss: better ear pure-tone average greater than 70 dB HL (re: ANSI 2004)
Identified with hearing loss and enrolled in early intervention by 3 years, 6 months
Cochlear implantation before age 3 years, 0 months
Use of a modern, multichannel CI system for 3 years or more
Enrolled in a rehabilitative program or living in a home environment that encourages the development and use of speech and spoken language skills
The HA and CI groups were recruited from a hospital database of DHH children with HAs and/or CIs. The NH Control group was recruited from a university research recruitment database. Table 1 displays a summary of the demographic characteristics of the children and their families. Participant groups were significantly different in chronological age, F (2, 29) = 3.392, p = .049, with the NH group averaging about 1 year older than the HA group (p = .040). In addition, hearing loss in the CI group was identified approximately 1 year earlier than in the HA group, t (18) = 2.480, p = .001, which is not uncommon given the more significant degree of loss that the children with cochlear implants experience. The following remaining demographic factors were not significantly different across the groups: mean annual income, F (2, 29) = 1.323, p = .283; primary caregiver education, F (2, 29) = 2.157, p = .135; family size, F (2, 29) = .025, p = .975 (all evaluated by one-way ANOVAs); gender, χ2 (2) = .268, p = .875, and marital status, χ2 (2) = 3.900, p = .142 (both evaluated with Pearson chi-square tests). Pearson chi-square tests for percentage of two-parent homes, communication mode, and whether children had additional disabilities could not be performed because of low number of participants combined with significantly unbalanced distributions. Across the groups, 70–100% of homes were headed by two parents.
Table 1.
Participant Demographics and Hearing History
| NH | HA | CI | |
|---|---|---|---|
| Mean (SD) age at test (yrs) | *7.16 (1.16) | *6.04 (1.04) | 6.47 (0.73) |
| Mean (SD) age at HL ID (mos) | -- | *18.8 (14.6) | *6.4 (6.4) |
| Mean (SD) age at CI/HA fitting (mos) | -- | a25.7 (16.6) | 22 (17.3) |
| Mean unaided better-earbPTA range (dB HL) | <25 | 33–70 | >70 |
| cMean annual income bracket | $65,000–79,999 | $35,000–49,999 | $50,000–49,999 |
| dMean primary caregiver education | 4.2 (.92) | 3.5 (1.27) | 3.1 (1.45) |
| Mean family size (number of members) | 4.1 | 4.2 | 4.3 |
| Oral communicators (%) | -- | 100% | 90% |
| Female (%) | 50% | 40% | 50% |
| Married parents (%) | 90% | 60% | 60% |
| Two-parent household (%) | 90% | 70% | 100% |
| Additional developmental disabilities (%) | 0% | 20% | 10% |
| Mean S&L intervention per weeke | -- | *2.75 | *7.45 |
| Receiving private S&L therapy (number) | -- | 0 | 6 |
Note. NH = normal hearing; HA = hearing aid; CI = cochlear implant; SD = standard deviation; yrs = years; mos = months; HL = hearing loss; ID = identification; mos = months; PTA = Pure-tone average re: ANSI (2004); S&L = speech and language
Based on data from 9 participants, because one parent could not recall age at first hearing aid fitting, nor were records available
at .5, 1, and 2 kHz
Primary caregivers reported their gross household income in the preceding year according to category bins ranging from “under $5500” to “over $95000.”
Primary caregiver education was scored by assigning integer values (1 through 7) to primary caregivers’ highest levels of formal education: 1 = some high school, 2 = high school diploma, 3 = some college, 4 = Associate degree, 5 = Bachelor’s degree, 6 = Master’s degree, 7 = Doctorate degree
Speech and language (S&L) intervention according to 15-min category bins ranging from 1 = “0–15 min/week” to 9 = “more than 120 minutes/week.” Amount was summed for intervention received in school and out of school in private therapy.
p ≤ .05
All but one child used oral communication; the one who used Total communication was in the CI group. Children with CIs received significantly more speech-language (S&L) therapy per week (approximately 1 hour, 45 minutes/week) than children with HAs (approximately 45 minutes/week), t (18) = −2.211, p = .040. Moreover, none of the HA users received S&L therapy outside of school/daycare from a private provider, whereas six of the children in the CI group did.
One child in the CI group with a diagnosis of ADHD was included in the study because executive function difficulties (which are frequently manifest behaviorally as symptoms of ADHD) are consistently observed in approximately 1/3 of children with CIs (e.g., Kronenberger et al. 2014a,b). As expected, this child had elevated scores on our executive function measure as well as average to low-average language and receptive vocabulary scores.
One child in the HA group had mild neurological differences including mild characteristics of Chiari malformation, decreased myelin, and hypoplasia of the corpus callosum, which were judged not to meet neurological severity exclusionary criteria. This child was retained in the analysis because he was mainstreamed and not receiving services beyond those directed towards his hearing loss. Moreover, this child’s scores on the language and executive function measures were at or above the HA group’s mean scores.
Materials
Family Environment Measures
Home Observation Measurement of the Environment (HOME).
The HOME (Caldwell & Bradley 2003) is a widely used measure of home environment that evaluates the quality and quantity of support and stimulation provided to the child at home. The instrument is administered through a semi-structured interview with a caregiver, as well as an observation of the home environment and interactions between the parent and the child in the home. Consistent with test age guidelines, the Early Childhood version was used with caregivers of the 5-year-old children (1 NH Control and 7 HA families), whereas the Middle Childhood version was used with caregivers of the 6- to 8-year-old children (9 NH Control families, 10 CI families, and 3 HA families). The Early Childhood HOME consists of 55 items arranged into eight different subscales: Learning Materials, Language Stimulation, Physical Environment, Parental Responsivity, Academic Stimulation, Modeling of Social Maturity, Variety in Experience, and Acceptance of Child. The Middle Childhood HOME contains 59 items arranged into eight subscales: Parental Responsivity, Encouraging Maturity, Emotional Climate, Learning Materials, Enrichment, Family Companionship, Family Integration, and. Three subscales – Physical Environment, Parental Responsivity, and Learning Materials – appear on both versions of the HOME, as does the ability to calculate a Total score that reflects how enriched the home environment is as a whole. There are a different number of items used to assess the subscales that overlap across the two versions: Physical Environment differs by one question (EC = 7 questions; MC = 8 questions), whereas both Parental Responsivity (EC = 7; MC = 10) and Learning Materials (EC = 11, MC = 8) differ by 3 questions each. The questions themselves overlap quite a bit on the Physical Environment subscale, with 6 being identical. For the Responsivity and Learning Materials subscales, the specific content of the question overlaps little across the two versions because the expectations of how families interact with children around these two constructs necessarily differ based on the developmental levels of the child. For example, the expression of parental responsivity changes with child development, as does the appropriateness of learning materials and activities. Thus, the two versions of this questionnaire ask questions that tap these underlying constructs using developmentally appropriate (and therefore different) content between the two versions of the assessment. It is important to note that across the two versions, both assess the same underlying construct within each subscale. In order to allow comparison across the two versions of the HOME, analyses in the current study used the percent of the Total HOME score and the percentage of the maximum raw score obtained on each of the three subscales that appear on both HOME versions (e.g., 100 × (raw score obtained by the participant)/(the total raw score possible), because the HOME does not have normative data.
Family Environment Scale (FES).
The FES (Moos & Moos 2009) is a 90-item self-report, true-false questionnaire that assesses three dimensions of family environment. (1) The Family Relationship Dimension is composed of three subscales: Cohesion, Expressiveness, and Conflict. (2) The Personal Growth Dimension consists of five subscales: Independence, Achievement Orientation, Intellectual-Cultural Orientation, Active-Recreational Orientation, and Moral-Religious Emphasis. (3) And the System Maintenance Dimension contains two subscales: Organization and Control. FES subscale raw scores are converted to T-scores (mean of 50 and standard deviation of 10 based on a large normative sample). The FES has been used with various clinical pediatric populations, including children with hearing loss (Holt et al. 2012) and children with behavioral, emotional, and developmental disabilities (Rousey 2002). In order to report results from a broad set of family environment characteristics, we used all 10 FES subscales in the current study.
Child Language Measures
Peabody Picture Vocabulary Test–4 (PPVT–4).
The PPVT-4 (Dunn & Dunn 2007) is a norm-referenced measure of single-word receptive vocabulary for individuals between 2.5 to 90 years of age. It has routinely been used with preschool and school-age children with hearing loss. PPVT-4 age-based normed standard score was used in the current study.
Clinical Evaluation of Language Fundamentals–4 (CELF–4).
The CELF-4 (Semel 2003) is a comprehensive global measure of language ability for children ages 5 to 18 years. The Core Language Score, a composite of subtests that evaluate multiple domains of language development, was used in the current study to assess general language ability. The Core Language Score is based on an age-based norm sample. Like the PPVT-4, the CELF-4 is routinely used with young children with hearing loss.
Child Executive Function Measures
Behavior Rating Inventory of Executive Function (BRIEF).
The BRIEF (Gioia et al. 2000) is an 86-item parent-report questionnaire that assesses everyday real-world executive function behaviors of children ages 5 to 18 years. The BRIEF measures eight core domains of executive functioning: Inhibit, Shift, Emotional Control, Initiate, Working Memory, Plan/Organize, Organization of Materials, and Monitor.
The Behavior Rating Inventory of Executive Function-Preschool version (BRIEF-P).
The BRIEF-P (Gioia et al. 2003) is similar to the BRIEF, but is designed for children aged 2;0 to 5;11 (year;month). Because some of the items on the BRIEF address executive function in a formal school setting, the BRIEF-P was used with parents of the 5-year-old children because many of these children had not yet started school. The BRIEF-P consists of 63 items that measure a subset of the domains of executive functioning used in the BRIEF, including Inhibit, Shift, Emotional Control, Working Memory, and Plan/Organize. Scores for the specific domains on both the BRIEF and the BRIEF-P are converted to T-scores using age- and gender-specific norms; T scores at or above 65 are considered to reflect clinically significant executive function problems and scores above 60 are elevated. Both the BRIEF and the BRIEF-P have been used in several clinical populations including children with ADHD, autism spectrum disorder, TBI, and cochlear implants (Gilotty et al. 2002; Mangeot et al. 2002; Jarratt et al. 2005; Pisoni et al. 2010; Beer et al. 2011; Holt et al. 2012, 2013). For the purpose of the analyses, two BRIEF subscales that have been shown in prior research to be related to hearing status were used: Working Memory and Inhibition (e.g., Beer et al. 2014; Hall et al. 2018).
Psychosocial Adjustment Measure
The Social Skills Improvement System (SSiS) Rating Scales.
The SSiS (Gresham & Elliott 2008) is a standardized 79-item questionnaire that evaluates social skills (e.g., cooperation, responsibility, self-control, empathy), problem behaviors (e.g., externalizing, bullying, hyperactivity/inattention, internalizing), and academic competence (reading, math, motivation to learn) in children between the ages of 3–18 years. Teacher, parent and child forms are available. Only the parent form was used in the current investigation. Furthermore, only the Social Skills and Problem Behavior composites and subscales were analyzed. The subskills that comprise Social Skills are: communication, cooperation, assertion, responsibility, empathy, engagement, and self-control. Those that comprise Problem Behaviors are: externalizing, bullying, hyperactivity/inattention, internalizing, and autism spectrum tendencies. Raw scores are converted to standard scores (mean = 100, SD = 15) based on normative data. Higher scores on the Social Skills Scale (and its subscales) indicate better social skills, whereas higher scores on the Problem Behavior Scale (and its subscales) indicate higher levels of problem behaviors.
Procedure
Parent questionnaires (FES, BRIEF/BRIEF-P, and SSiS) were mailed to families approximately 1 week before their scheduled home visit with instructions regarding how to complete the forms. Only one family did not have the questionnaires completed when the researchers arrived for the home visit. In this case, the researchers had the parent complete the forms during the home visit.
The remaining assessments (HOME, PPVT-4, and CELF-4) were administered by the researchers during a 1.5- to 2-hour visit in the family’s home. Two researchers visited each home together. While one researcher reviewed questionnaires and administered the HOME with the parent, the other researcher administered the PPVT-4 and CELF-4 to the child in a separate, quiet space. The parent and child also completed a videotaped parent-child play interaction, which was not used for the current set of analyses. After each assessment, the child received a small prize (a book, stickers, a pencil, etc.), and at the completion of the home visit the caregiver and the child each received payment for participation. The study was approved by the university IRB.
Statistical Analysis
In order to address the first research question comparing groups on family environment and other developmental outcomes, a one-way ANOVA was used to compare the three subsamples (NH, CI, and HA) on family measures (FES subscale T-scores; HOME Total; HOME Parental Responsivity, Learning Materials, and Physical Environment subscale scores), as well as outcome measures of language (PPVT-4 Standard Score, CELF-4 Core Language Score), executive functioning (BRIEF Working Memory and Inhibition T-scores), and psychosocial adjustment (SSiS Social Skills and Problem Behaviors Composite, and Subscale Standard Scores). Significant ANOVA results were followed up with t-tests comparing groups to better understand differences contributing to the significant ANOVA result. Planned analyses (independent samples t-tests) were also conducted comparing the NH group to the DHH group (combined HA and CI groups) on these measures.
The second goal of this study was to investigate the associations between family environment and a broad set of outcomes (spoken language, psychosocial, and neurocognitive) in DHH children. Associations between family factors and developmental outcomes in children with hearing loss were examined using Pearson correlations. A combined sample of all DHH participants (e.g., those with CIs or HAs) was used for these analyses, in order to increase statistical power.
In order to reduce risk for alpha error in evaluating statistical significance (using 2-tailed p < 0.05 as the criterion for significance), we either used a small number of measures/subscales for each construct, or we tested significance for a composite total score prior to evaluating results for subscales (with the exception of the FES, as noted below). Specifically, for the observational/interview measure of family environment, only the HOME Total score and three subscale scores from both HOME versions (Parental Responsivity, Learning Materials, and Physical Environment) were used. For language, only a single global norm-based score was used for each measure (PPVT-4 Standard Score and CELF Core Language Score). For psychosocial adjustment, the two SSiS composite scores (Social Skills and Problem Behaviors) were used as the primary measures, and results for SSiS subscales were considered to be statistically significant only if the composite score yielded a significant result; for example, correlations between SSiS subscales and family environment scores were reported and interpreted as statistically significant only if correlations between the SSiS composite and family environment score was statistically significant. Because the FES does not yield a composite score, we used all FES subscales in the statistical analysis, with the understanding that this is an exploratory analysis at a higher level of risk for alpha error.
Results
Language, Psychosocial, and Executive Function Outcomes by Sample
Table 2 displays descriptive statistics for language, psychosocial, and executive function outcomes, results of one-way ANOVAs comparing performance across the three participant groups for each outcome measure and results of independent samples t-tests on the NH vs. the DHH groups. As expected, language and receptive vocabulary differed across groups. The NH Control group had better language than both the HA (p = .003) and the CI groups (p < .001). Similarly, their receptive vocabulary was better than both the HA (p = .001) and CI groups (p < .001). Further, one-sample t-tests revealed that the CELF-4 and PPVT-4 scores for the NH group were significantly higher than the test norms, t (9) = 9.273, p < .001 and t (9) = 7.919, p < .001, respectively, with mean standard scores on both language tests that were more than 1 SD greater than the normative mean. Whereas the CELF-4 and PPVT-4 scores were not significantly different between the HA and CI groups (p = .165 and p .122, respectively), only the CI group’s scores fell significantly below the test norms (CELF-4, t (9) = 4.914, p =.001, and PPVT-4, t (9) = 5.366, p <.001).
Table 2.
Language, Psychosocial, and Executive Functioning Scores by Group
| Group Mean (SD) | NH vs. HA vs. CI ANOVA | NH vs. DHH t-test | ||||||
|---|---|---|---|---|---|---|---|---|
| Outcome Measure | NH | HA | CI | DHH (HA+CI) |
F | P | t | p |
| I. Language | ||||||||
| CELF-4 Core | 117.8*+ | 82.4* | 63.2+ | 72.8 | F (2, 29) = 16.759 | p < .0001 | t (28) = 5.159 | p < .0001 |
| Language Standard | (6.1) | (27.8) | (23.7) | (6.04) | ||||
| Score | ||||||||
| PPVT-4 Standard | 122.1*+ | 93.5* | 78.4+ | 86.0 | F (2, 29) = 19.977 | p < .0001 | t (28) = 5.593 | p < .0001 |
| Score | (8.8) | (22.4) | (12.7) | (19.3) | ||||
| II. Psychosocial | ||||||||
| SSiS Social Skills | 109.9 | 94.6 | 96.1 | 95.4 | F (2, 29) = 0.829 | p = .447 | t (28) = 1.258 | p = .209 |
| Standard Score | (9.6) | (10.2) | (18.5) | (14.6) | ||||
| SSiS Problem | ||||||||
| Behaviors Standard Score |
95.4 (10.0) |
108.3 (14.7) |
102.7 (11.8) |
105.5 (13.3) |
F (2, 29) = 2.755 | p = .081 | t (28) = 2.115 | p = .043 |
| III. Executive Functioning | ||||||||
| BRIEF/P T-Score | ||||||||
| Inhibition | 46.4 (6.9) | 55.9(11.7) | 59.0(15.1) | 57.5(13.2) | F (2, 29) = 3.143 | p = .059 | t (28) = 2.465 | p = .020 |
| Working Memory | 47.7(10.7) | 56.7(18.6) | 54.9 (8.9) | 55.8(14.3) | F (2, 29) =1.258 | p = .300 | t (28) =1.584 | p = .125 |
Note. CELF = Clinical Evaluation of Language Fundamentals; PPVT = Peabody Picture Vocabulary Test; SSiS = Social Skills Improvement System Rating Scales; BRIEF = Behavior Rating Inventory of Executive Function
t-test significant (p ≤ .05) between two identified groups
Social skills and problem behaviors were not significantly different across the three groups in the one-way ANOVA, (see Table 2). Similarly, the two executive function domains of inhibitory control and working memory were not significantly different across the groups in the one-way ANOVAs (see Table 2).
For planned analyses comparing the NH and DHH groups, the NH Control group had better language and better receptive vocabulary than the DHH group (see Table 2), as would be expected based on the results of the one-way ANOVA and planned follow-up t-tests. Expanding upon the one-way ANOVA results, planned analyses comparing the NH to the DHH groups revealed that combining the highly variable HA and CI groups into a single DHH group increased power: two domains – Problem Behaviors and Inhibitory Control (which were nearing significance in the one-way ANOVAs) – were significant in the planned Independent Samples t-tests (see Table 2). Parents of DHH children reported more problem behaviors and concerns related to inhibitory control in their children than parents of NH children. Social skills and working memory remained similar between the NH and DHH groups.
Group Differences in Family Environment
Results of ANOVAs comparing FES scores across the three samples (Table 3, Part I) indicated significant differences on only one subscale – Intellectual Cultural Orientation, F (2, 29) = 4.078, p = .028, with families of children with NH reporting higher levels of interest in political, intellectual and cultural activities than families of children with HAs (p = .037). For the planned comparison between the NH and DHH groups, the same single subscale - Intellectual Cultural Orientation - remained significant, t (28) = 2.854, p = .008, with families of NH children reporting higher levels than those of DHH children. Note that the mean T-score for the HA group was 50.5, which is near the normative mean of 50, whereas the NH Control group mean T-score was 60.5, which is 1 SD greater than the normative mean, suggesting that the NH Control group had parents that reported particularly high levels of interest in intellectual and cultural activities.
Table 3.
Family Environment Scores by Group
| Group Mean (SD) | NH vs. HA vs. CI ANOVA | NH vs. DHH t-test | ||||||
|---|---|---|---|---|---|---|---|---|
| Family | ||||||||
| Environment | ||||||||
| Measure | NH | HA | CI | DHH (HA+CI) |
F | P | t | P |
| I. FES | ||||||||
| Achievement Or’n | 47.1 (14.6) | 47.0 (8.0) | 48.8 (8.5) | 47.9 (8.1) | F (2, 29) = .088 | p = .916 | t (28) = −.194 | p = .847 |
| Active- | ||||||||
| Recreational Or’n | 57.4 (10.2) | 49.3 (12.6) | 53.1 (13.0) | 51.2 (12.6) | F (2, 29) = 1.141 | p = .335 | t (28) = 1.346 | p = .189 |
| Control | 56.0 (11.2) | 56.7 (6.7) | 51.0 (8.5) | 53.9 (8.0) | F (2, 29) =1.193 | p = .319 | t (28) = .606 | p = .549 |
| Cohesion | 61.1 (8.5) | 52.6 (13.7) | 60.6 (6.2) | 56.6 (11.2) | F (2, 29) = 2.275 | p = .122 | t (28) = 1.119 | p = .273 |
| Conflict | 49.1 (10.5) | 47.0 (10.6) | 43.2 (8.4) | 45.1 (9.5) | F (2, 29) = .915 | p = .413 | t (28) = 1.050 | p = .303 |
| Expressiveness | 58.9 (10.0) | 55.8 (13.4) | 56.6 (7.0) | 56.2 (11.2) | F (2, 29) = .236 | p = .791 | t (28) = .677 | p = .504 |
| Independence | 47.4 (10.0) | 51.4 (9.1) | 49.8 (14.2) | 50.6 (11.6) | F (2, 29) = .316 | p = .732 | t (28) = −.742 | p = .464 |
| Intellectual- | ||||||||
| Cultural Or’n | 60.5 (2.6)* | 50.5 (10.1)* | 52.3 (10.0) | 51.4 (9.8) | F (2, 29) = 4.078 | p = .028 | t (28) = 2.854 | p = .008 |
| Moral-Religious | ||||||||
| Emphasis | 58.4 (15.0) | 61.5 (7.6) | 55.5 (10.4) | 58.5 (9.4) | F (2, 29) = .693 | p = .509 | t (28) = −.022 | p = .982 |
| Organization | 54.5 (11.9) | 53.2 (9.4) | 57.2 (7.7) | 55.2 (8.6) | F (2, 29) = .431 | p = .654 | t (28) = −.184 | p = .855 |
| II. HOME | ||||||||
| Total (% of possible) | 83.0 (8.4) | 77.0 (18.0) | 79.5 (8.6) | 45.1 (8.0) | F (2, 29) = .575 | p = .569 | t (28) = .993 | p = .329 |
| Responsivity (% of possible) | 82.1 (10.2) | 63.9 (14.3) | 90.0 (8.2) | 76.9 (17.6) | F (2, 29) = 14.369 | p < .001 | t (28) = .864 | p = .395 |
| Learning Materials (% of possible) Physical | 73.9 (19.9) | 65.0 (24.7) | 61.3 (17.1) | 63.1 (20.8) | F (2, 29) = .969 | p = .392 | t (28) = 1.353 | p = .187 |
| Environment (% of possible) | 90.0 (12.9) | 79.5 (24.5) | 95.0 (8.7) | 87.2 (19.6) | F (2, 29) = 2.237 | p = .126 | t (28) = .403 | p = .690 |
Note. FES = Family Environment Scale, Or’n = Orientation, HOME = Home Observation Measurement of the Environment
bold (p ≤ .05)
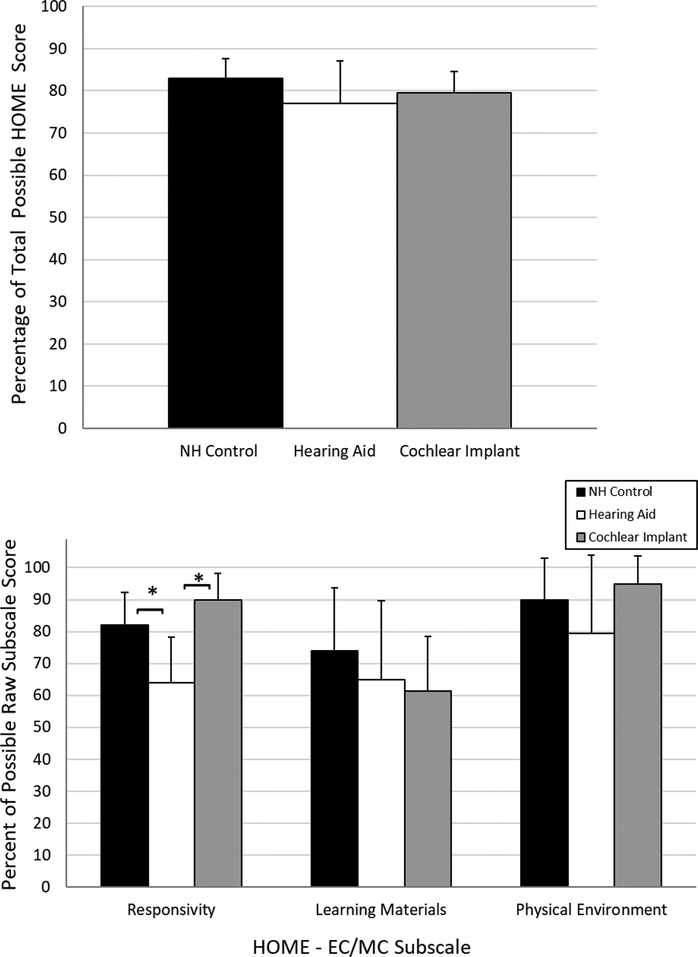
The top panel of Figure 1 displays the mean Total HOME scores (+1 SD) as a function of group. No significant differences in Total HOME scores were found across the participant groups, F (2, 29) = 0.575, p =.569. The bottom panel of Figure 1 displays the mean raw subscale scores obtained by each group on the HOME. Only one subscale revealed differences among the groups on any dimension of family environment: Parental Responsivity, F (2, 29) = 14.369, p < .001. Based on post-hoc comparisons with a conservative Bonferroni correction, the group differences in parental responsivity were due to the parents of the children with HAs being rated as less responsive to their children than the parents of children with CIs (p < .0001) and those with NH (p = .003). All of the planned analyses comparing the NH and DHH groups on the HOME (Total, Responsivity, Physical Environment, and Learning Materials) were not significant (two-tailed p-values all >.187). Results of the ANOVAs and t-tests for the HOME are displayed in Part II of Table 3.
Figure 1.
Mean Home Observation Measurement of the Environment (HOME) Total score (+1 SD) as a function of participant group (panel top panel). Mean percent of the possible raw scores (+1 SD) on the overlapping subscales of the HOME-Early Childhood (EC) and HOME-Middle Childhood (MC) as a function of participant group (bottom panel).
Associations between Family Environment and At-Risk Outcomes in DHH Children
Our second research aim concerned examining associations between family environment and developmental outcomes in DHH children. Therefore, the following analyses were completed on data from DHH children (n=20) and their families only.
Spoken Language Development
Families with more enriched home environments (Total HOME), including those that offered more toys and activities that promoted their child’s intellectual development (HOME – Learning Materials), and those that reported lower levels of open disagreement and anger among family members (FES – Conflict), had children with better spoken language and larger receptive vocabularies (see Table 4). Additionally, those families that were safer both inside and out (HOME – Physical Environment) had children with better receptive vocabularies and a trend for better spoken language (Table 4).
Table 4.
Associations between Family Environment and Language for Children with Hearing Loss
| CELF-4 Core Language | PPVT-4 | |
|---|---|---|
| I. FES | ||
| Achievement Or’n | r = .072, p = .764 | r = −.008, p = .974 |
| Active-Recreational Or’n | r = .224, p = .342 | r = .234, p = .321 |
| Cohesion | r = .266, p = .257 | r = .320, p = .170 |
| Conflict | r = −.478, p = .033* | r = −.633, p = .003** |
| Control | r = .265, p = .259 | r = .219, p = .354 |
| Expressiveness | r = .421, p = .065 | r = .412, p = .071 |
| Independence | r = −.302, p = .196 | r = −.025, p = .917 |
| Intellectual-Cultural Or’n | r = .190, p = .421 | r = .107, p = .654 |
| Moral-Religious Emphasis | r = .356, p = .124 | r = .269, p = .251 |
| Organization | r = −.067, p = .779 | r = −.012, p = .959 |
| II. HOME | ||
| HOME – Total (% of possible) | r = .593, p = .006** | r = .654, p = .002* |
| HOME – Responsivity (% of possible) | r = −.175, p = .460 | r = −.157, p = .508 |
| HOME – Learning Materials (% of possible) | r = .598, p = .005** | r = .642, p = .002** |
| HOME – Physical Environment (% of possible) | r = .440, p = .052 | r = .455, p = .044* |
Note. Values are Pearson correlations. CELF = Clinical Evaluation of Language Fundamentals; PPVT = Peabody Picture Vocabulary Test; FES = Family Environment Scale; HOME = Home Observation Measurement of the Environment.
p ≤ .05,
p ≤ .01
Psychosocial Development
Families that placed an emphasis on joint recreational activities (FES – Active-Recreational) had children with better overall social skills (SSiS – Social Skills; Table 5 displays correlations for SSiS composite scales only; subscale SSiS correlations are provided in the text), specifically in the areas of Cooperation (r = 0.515), Responsibility (r = 0.514), and Empathy (r = 0.477) (all p < 0.05). Families that supported each other in openly expressing feelings among family members (FES – Expressiveness) also had children with better overall social skills (SSiS – Social Skills), specifically in the subdomains of Cooperation (r = 0.551), Responsibility (r = 0.459), and Self-control (r = 0.460) (all p < 0.05).
Table 5.
Associations between Family Environment and Psychosocial Skills for Children with Hearing Loss
| SSiS - Social Skills | SSiS - Problem Behaviors | |
|---|---|---|
| I. FES | ||
| Achievement Or’n | r = .222, p = .346 | r = .107, p = .653 |
| Active-Recreational Or’n | r = .483, p = .031* | r = −.145, p = .542 |
| Cohesion | r = .251, p = .285 | r = −.547, p = .013* |
| Conflict | r = −.388, p = .091 | r = .272, p = .246 |
| Control | r = −.225, p = .339 | r = .121, p = .610 |
| Expressiveness | r = .503, p = .024* | r = −.330, p = .155 |
| Independence | r = .142, p = .551 | r = .052, p = .828 |
| Intellectual-Cultural Or’n | r = −.226, p = .338 | r = .332, p = .152 |
| Moral-Religious Emphasis | r = −.151, p = .525 | r = −.078, p = .743 |
| Organization | r = .177, p = .456 | r = −.072, p = .762 |
| II. HOME | ||
| HOME - Total (% of possible) | r = .328, p = .158 | r = −.480, p = .032* |
| HOME - Responsivity (% of possible) | r = .185, p = .434 | r = −.366, p = .112 |
| HOME - Learning Materials (% of possible) | r = .401, p = .080 | r = −.283, p = .227 |
| HOME - Physical Environment (% of possible) | r = .182, p = .442 | r = −.389, p = .090 |
Note. Values are Pearson correlations; SSiS = Social Skills Improvement System Rating Scales; FES = Family Environment Scale; Or’n = Orientation; HOME = Home Observation Measurement of the Environment.
p ≤ .05,
p ≤ .01
Parents who reported that family members provided higher levels of support to one another (FES – Cohesion) had children with fewer overall behavior problems (SSiS – Behavior Problems), particularly in the areas of Hyperactivity-Inattention (r = −0.488) and Autism Spectrum (r = −0.572) (all p < 0.05). More generally enriched home environments (Total HOME Score) correlated with fewer overall behavior problems in children (SSiS – Behavior Problems; Table 5), specifically in the areas of Externalizing (r = −0.488), Hyperactivity-Inattention (r = −0.533), and Autism spectrum (r = −0.603) (all p < 0.05).
Executive Function Development
As shown in Table 6, parents reported better working memory in their children who were from more enriched home environments (Total HOME Score), specifically homes that appeared safe inside and outside the home (HOME – Physical Environment), as well as in families that placed an emphasis on being engaged in recreational activities together (FES – Active-Recreational), provided higher levels of support to one another (FES – Cohesion), and supported each other in openly expressing their feelings among family members (FES – Expressiveness). In addition, parents reported better inhibitory control in their children in homes with higher levels of support for one another and who encouraged expressing feelings to each other.
Table 6.
Associations between Family Environment and Executive Function for Children with Hearing Loss.
| BRIEF/P-Inhibitory Control | BRIEF/P-Working Memory | |
|---|---|---|
| I. FES | ||
| Achievement Or’n | r = −.193, p = .415 | r = −.251, p = .286 |
| Active-Recreational | r = −.298, p = .202 | r = −.513, p = .021* |
| Cohesion | r = −.465, p = .039* | r = −.549, p = .012* |
| Conflict | r = .392, p = .088 | r = .284, p = .224 |
| Control | r = −.096, p = .686 | r = .227, p = .336 |
| Expressiveness | r = −.569, p = .009** | r = −.688, p = .001** |
| Independence | r = −.075, p = .754 | r = .073, p = .759 |
| Intellectual-Cultural Or’n | r = .272, p = .246 | r = .122, p = .607 |
| Moral-Religious Emphasis | r = −.177, p = .455 | r = −.063, p = .792 |
| Organization | r = −.291, p = .213 | r = −.180, p = .449 |
| II. HOME | ||
| HOME - Total (% of possible) | r = −.405, p = .076 | r = −.495, p = .027* |
| HOME – Responsivity (% of possible) | r = .058, p = .809 | r = −.267, p = .255 |
| HOME - Learning Materials (% of possible) | r = −.422, p = .064 | r = −.436, p = .055 |
| HOME - Physical Environment (% of possible) | r = −.282, p = .229 | r = −.521, p = .019* |
Note. Values are Pearson correlations; BRIEF = Behavior Rating Inventory of Executive Function; FES = Family Environment Scale; Or’n = Orientation; HOME = Home Observation Measurement of the Environment.
p ≤ .05,
p ≤ .01
Discussion
Child development occurs within social systems of bidirectional influence, the most potent and proximal of which is the family environment. Our S-B-R Model of development of children with hearing loss provides a conceptual framework for understanding and explaining family factors contributing to at-risk developmental outcomes in children with hearing loss. The current investigation was carried out to test two questions in this model, using small samples of NH and DHH children with either CIs or HAs: (1) Are specific dimensions of family environment different in DHH children using sensory aids, compared to NH children? (2) Is family environment associated with at-risk developmental outcomes in DHH children using sensory aids? To address these questions, we collected behavioral, observational, interview, and parental-report data from 5- to 8-year-old children and their primary caregivers in their homes.
Research Question 1: Are specific dimensions of family environment different in DHH children using sensory aids, compared to NH children?
With rare exceptions, the global characteristics of family environment assessed in this study did not differ between families of DHH and NH children. The only differences found between groups were for families of children with HAs to score lower than one or both of the other groups (families of NH children or families of children with CIs) on measures related to shared intellectual-cultural activities and parental responsivity.
Higher levels of intellectual-cultural activities and parental responsivity are characteristic of families with greater levels of stimulation that is organized, positive, and interactive. Intellectual-cultural activities create greater levels of verbal and nonverbal stimulation as well as positive family interactions around intellectual endeavors. Parental responsivity implies a positive emotional connection between the parent and child on which the parent appropriately acts on those emotions in synchrony with the child’s behaviors. Parents of younger children who score high on responsivity are observed doing a combination of verbally responding to their child’s questions, communicating with their child, praising their child, showing physical affection during the home visit, and reporting that they hold their children for at least 10–15 minutes per day. Parents of older children who score high on responsivity are observed doing a combination of verbally responding to their child’s questions and using full sentences with long words in conversation, showing positive emotional responses to their child and conveying positive feelings when speaking of their child, reporting that the child’s schedule is fairly predictable, and that they succumb to the child’s fears or rituals, encourage the child to read, and praise the child.
Results of some studies of maternal sensitivity, which is related to parental responsivity and environmental stimulation, have shown lower levels of sensitivity in mothers of DHH children relative to NH controls (e.g., Meadow-Orleans & Steinberg 1993). However, not all studies have concluded that maternal sensitivity is different between parents of children with hearing loss versus those with hearing (e.g., Lederberg & Mobley 1990). Maternal sensitivity affects children’s language development (Quittner et al. 2013), specifically through healthy attachment and affective-cognitive stimulation (Lederberg & Mobley 1990; Belsky & Fearon 2002; Friedman & Boyle 2008; Taylor et al. 2009). Moreover, maternal sensitivity has been positively linked to children’s inhibitory control (Kochanska et al. 2000; Eisenberg et al. 2005; Bernier et al. 2010).
It is notable that the mean family income of the HA group was the lowest of all the groups, and that families of children with HAs were more likely to have a single-parent home than the other two groups, although the samples did not significantly differ on family income. Because family income was not significantly different across the groups, we did not control for mean income in any of the analyses of family environment. In future work with larger sample sizes, this could be an area to investigate and/or control, as it could contribute to differences across groups. Thus, there are indications that the HA sample had more sociodemographic risk factors (e.g., lower socioeconomic status), which may have contributed to lower levels of shared intellectual activities and parental responsivity, although explaining differences between groups based on material resources alone can be erroneous (e.g., Hoff 2003). It is not clear whether the sociodemographic trends in family composition and SES resulted from a sampling effect of this particular study or reflected a broader epidemiological effect; studies with larger samples would be needed to answer this question. Nevertheless, in general, the family environments of the DHH and NH samples were much more similar than they were different, and no differences were found between the NH and CI samples on the family measures obtained in this study.
Another possible explanation for differences in intellectual stimulation and shared interactions between the HA and CI groups may be differences in the type and intensity of intervention received. Children with CIs received over twice the amount of minutes of speech-language therapy on average than children with HAs, which may have been more effective in teaching parents how to respond appropriately to their children with well-timed and warm interactions. Furthermore, no children with HAs received private intervention in addition to that received in school, whereas six of those with CIs did.
These results support and extend the findings of previous investigations that employed the FES to study families of DHH children (Holt et al. 2012, 2013). Families of children with cochlear implants differed from the test norms on some subscales, but on average scores were within one standard deviation of the mean. The current study employed hearing children as controls (which was not used in our previous investigations), rather than comparing the clinical groups to test norms, and found almost no differences in FES scores between NH and DHH children’s families. This study was the first time the HOME has been used to assess family environment in this clinical population.
In summary, characteristics of family environments overall were similar in the NH, CI, and HA samples. Differences in intellectual activities and parental responsivity (with the caveat that different versions the HOME were used across participants) found in the HA sample should be explored in future research.
Research Question 2: Is family environment associated with at-risk developmental outcomes in DHH children with sensory aids?
As expected, spoken language was significantly poorer in DHH children (both the CI group and the HA group) than in NH peers. Only when the HA and CI groups were combined was there enough power to observe the expected differences in inhibitory control and problem behaviors in DHH children relative to their NH peers, consistent with other literature in this area (Beer et al. 2011; Holt et al. 2013; Kronenberger et al. 2014a,b). However, social skills and working memory were not significantly different between the DHH and NH children, which diverges from the literature in this area, and is likely due to the wide variability in scores combined with the small participant numbers in the clinical groups. For example, differences in norm-based scores between the NH and DHH samples for nonsignificant comparisons of SSiS composites and BRIEF subscales (e.g., Social Skills and Working Memory scores) were in the 0.5 to 1.0 SD range – differences of a magnitude that are not trivial.
Family environment was significantly associated with language, psychosocial, and executive function outcomes of the children with hearing loss, with some trends emerging across family characteristics and outcomes. The dimensions of the home environment that were correlated with better receptive vocabulary and overall spoken language included a generally enriched home environment that includes the availability of learning materials that promoted intellectual development in the home, that is free of hazards and appears safe, has a bright interior that is visually interesting, clean and minimally cluttered, and maintains lower levels of conflict among family members. Families with high scores on the HOME – Learning Materials provide their child unlimited access to at least 10 age-appropriate books, a method for playing recorded music as well as a musical instrument, a space to study or read that is quiet (if the child is older) or toys and puzzles that teach concepts and encourage free expression (if the child is younger), and take a daily paper and subscribe to a magazine. These characteristics of the family environment provide activities that are likely to stimulate language and vocabulary (Bradley et al. 2001). Hence, these findings suggest that parents of DHH children that provide both objects and experiences that stimulate learning in the home can reduce the risk of poor spoken language outcomes in their child.
For psychosocial adjustment and executive functioning, family cohesion, expressiveness, shared recreational activities, and a generally enriched home environment were associated with better outcomes. Specifically, families who were more expressive and who shared more recreational activities had children with better social skills, while families that were more positive, supportive, and provided enriched experiences/environments had children with fewer problem behaviors. Children with better inhibitory control and working memory experience more positive, supportive, and expressive family interactions. Greater interactional and environmental enrichment in the family, including shared family recreational activities, was also related to better working memory in the child. Importantly, the three FES subscales that were positively associated with psychosocial adjustment and executive functioning (Active Recreational Orientation, Cohesion, and Expressiveness) all fall on a single empirically-defined factor representing a general family environment of supportiveness and stimulation. This factor has been associated with positive psychosocial outcomes in families with children who have chronic physical conditions (Kronenberger & Thompson 1990).
In summary, study results identified several characteristics of family environment that are related to important at-risk developmental outcomes in DHH children who use HAs and CIs. Whereas the overall quality of enrichment in the home environment was related to most outcome measures, specific dimensions of family functioning were related to psychosocial and executive function development and differed from those dimensions that related to language development. Supportiveness and enrichment in family relationships were associated with psychosocial and executive function development of DHH children, while availability of objects and experiences to stimulate learning in the home, a safe environment, and absence of family conflict related to spoken language development. These findings support our S-B-R Model and extend the explanation of diverse outcomes (language, psychosocial, and executive function) in DHH children by indicating family domains are related to outcomes. Furthermore, findings suggest novel, family-level targets for intervention to promote positive developmental outcomes in the DHH population. Family environments are malleable, as evidenced by improved support and functioning, and reduced conflict and control following family-oriented communication and education programs (Hill & Balk 1987; Mills & Hansen 1991; Bruce & Emshoff 1992), which raises a potential effective avenue for new intervention approaches for this clinical population.
Limitations of this work include the following: 1) Because this was a preliminary investigation, there was a limited number of participants within each group, and the NH and HA groups differed significantly in age. This limits the types and power of statistical analyses. 2) The characteristics of the family that were investigated were limited by the measures employed. Whereas we selected a set of measures that provided broad information about family environment and used several methods of assessment (questionnaire, interview, observation), other characteristics of family environment not studied here could also be influential in explaining developmental outcomes. Additionally, two developmentally appropriate versions of the HOME were used depending on the age of the child, limiting the comparisons that can be made across the various subdomains. However, the subdomains that are in common still assess the same underlying construct, and those were used in the current investigation. 3) The design of the study (multiple measures, multiple constructs, and comparison of three groups) resulted in multiple tests of statistical significance (although they were all planned and theoretically motivated), which raises the risk of alpha error in results. 4) Because of the correlational design of the study, analyses cannot confirm a causal direction. Future work with more participants should use statistical approaches that combine variables into single factors to reduce the number of tests, as well as investigate longitudinal effects to better understand the causative nature of relations in the S-B-R model. 5) Measures of outcome were focused on specific risk domains and used a subset of assessment methods (primarily questionnaires for psychosocial and neurocognitive outcomes), which should be expanded in future research to include additional behavioral performance measures.
Conclusions
Family environments of DHH children showed few differences from those of NH children, but supportive, interactive, enriched family environments were found to be related to better language, psychosocial, and executive function outcomes in the DHH sample. These results support the hypothesis that family factors are key contributors to variability in language, psychosocial, and executive function outcomes for DHH children, and point to the importance of further research of family factors in our S-B-R risk model to better understand these complicated relations. New, targeted family-based interventions may offer the promise of improved developmental outcomes in DHH children.
Acknowledgements
This work was supported by Indiana University’s Collaborative Research Grant (to Holt and Kronenberger) and the NIH-NIDCD R01014956 (to Holt and Pisoni) and T3200011 (to Pisoni). Portions of this work were presented at the American Auditory Society Meeting, Scottsdale, AZ (March, 2013) and the CI 2013 Symposium (October, 2013). Author contribution statement: RFH and WGK designed experiments, analyzed data and wrote the paper; JB and DBP designed experiments, provided interpretive analysis and critical revision; KL collected data, provided interpretive analysis, and critical revision; and LM collected data and provided critical revision.
References
- Ambrose SE, Walker EA, Unflat-Berry LM, et al. (2015). Quantity and quality of caregivers’ linguistic input to 18-month and 3-year-old children who are hard of hearing. Ear and Hearing, 36 (Suppl.), 48S–59S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American National Standards Institute (2004). Specification for audiometers (ANSI S3.6–2004). New York: Acoustical Society of America. [Google Scholar]
- Barker DH, Quittner AL, Fink NE, et al. (2009). Predicting behavior problems in deaf and hearing children: The influences of language, attention, and parent-child communication. Developmental psychopathology, 21, 373–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beer J, Kronenberger WG, Castellanos I, et al. (2014). Executive functioning skills in preschool-age children with cochlear implants. Journal of Speech, Language and Hearing Research, 57, 1521–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beer J, Kronenberger WG, & Pisoni DB (2011). Executive function in everyday life: Implications for young cochlear implant users. Cochlear Implants International, 12 (Suppl.), S89–S91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J (1981). Early human experience: A family perspective. Developmental Psychology, 17, 3–23. [Google Scholar]
- Belsky J, & Fearon RMP (2002). Infant–mother attachment security, contextual risk, and early development: A moderational analysis. Development and Psychopathology, 14, 293–310. 10.1017/S0954579402002067 [DOI] [PubMed] [Google Scholar]
- Bernier A, Carlson SM, & Whipple N (2010). From external regulation to self-regulation: Early parenting precursors of young children’s executive functioning. Child Development, 81, 326–339. [DOI] [PubMed] [Google Scholar]
- Bertram B, & Päd D (1995). Importance of auditory-verbal education and parents’ participation after cochlear implantation of very young children. Annals of Otology, Rhinology and Laryngology, 166 (Suppl.), 97–100. [PubMed] [Google Scholar]
- Bradley R, Corwyn RF, Burchinal M, et al. (2001). The home environments of children in the United States Part II: Relations with behavioral development through age thirteen. Child Development, 72, 1868–1886. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32, 513–531. [Google Scholar]
- Bruce C, & Emshoff J (1992). The SUPER II Program: An early intervention program. Journal of Community Psychology, OSAP Special Issue, 10–21. [Google Scholar]
- Caldwell BM, & Bradley RH (2003). Home Observation for Measurement of the Environment: Administration Manual. Tempe, AZ: Family & Human Dynamics Research Institute, Arizona State University. [Google Scholar]
- Castellanos I, Kronenberger WG, & Pisoni DB (2018). Psychosocial outcomes in long-term cochlear implant users. Ear and Hearing, 39, 527–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti DV & Lynch M (1993). Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children’s development. Psychiatry, 56, 96–118. [DOI] [PubMed] [Google Scholar]
- Cicchetti DV & Rizley R (1981). Developmental perspectives on the etiology, intergenerational transmission and sequelae of child maltreatment. New Directions for Child Development, 11, 31–56. [Google Scholar]
- Cruz I, Quittner AL, Marker C, et al. (2013). Identification of effective strategies to rpomote language in deaf children with cochlear implants. Child Development, 84, 543–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desjardin JL (2005). Maternal Perceptions of Self-Efficacy and Involvement in the Auditory Development of Young Children with Prelingual Deafness. Journal of Early Intervention, 27, 193–209. [Google Scholar]
- Desjardin JL, Ambrose SE, & Eisenberg LS (2008). Literacy skills in children with cochlear implants: The importance of early oral language and joint storybook reading. Journal of Deaf Studies and Deaf Education, 14, 22–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desjardin JL, & Eisenberg LS (2007). Maternal contributions: Supporting language development in young children with cochlear implants. Ear & Hearing, 28, 456–469. [DOI] [PubMed] [Google Scholar]
- Donahue A (2007). Guest editorial: Current state of knowledge - Outcomes research in children with mild to severe hearing loss. Ear and Hearing, 28, 713–714. [DOI] [PubMed] [Google Scholar]
- Dunn LM, & Dunn DM (2007). Peabody Picture Vocabulary Test, Fourth Edition Minneapolis, MN: Pearson. [Google Scholar]
- Edwards L, Thomas F, & Rajput K (2009). Use of revised children’s implant profile (GPSHChIP) in candidacy for paediatric cochlear implantation and in predicting outcome. International Journal of Audiology, 48, 554–560. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Zhou Q, Spinrad TL, et al. (2005). Relations among positive parenting, children’s effortful control, and externalizing problems: A three-wave longitudinal study. Child Development, 76, 1055–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flexer C (2011). Cochlear implants and neuroplasticity: Linking auditory exposure and practice. Cochlear Implants International, 12(Suppl.), S19–S21. [DOI] [PubMed] [Google Scholar]
- Freeman V, Pisoni DB, Kronenberer WG, et al. (2017). Speech intelligibility and psychosocial functioning in deaf children and teens with cochlear implants. Journal of Deaf Studies and Deaf Education, 22, 278–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SL, & Boyle DE (2008). Attachment in US children experiencing nonmaternal care in the early 1990s. Attachment and Human Development, 10, 225–261. 10.1080/14616730802113570 [DOI] [PubMed] [Google Scholar]
- Geers AE & Brenner C (2003). Background and educational characteristics of prelingually deaf children implanted by five years of age. Ear & Hearing, 24 (Suppl.), 2S–14S. [DOI] [PubMed] [Google Scholar]
- Geers A, Brenner C, & Davidson L (2003). Factors associated with development of speech perception skills in children implanted by age five. Ear and Hearing, 24 (Suppl.), 24S–35S. [DOI] [PubMed] [Google Scholar]
- Geers AE, Strube MJ, Tobey EA, et al. (2011). Epilogue: Factors Contributing to Long-Term Outcomes of Cochlear Implantation in Early Childhood. Ear and Hearing, 32 (Suppl.), 84S–92S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilotty L, Kenworthy L, Sirian L, et al. (2002). Adaptive skills and executive function in autism spectrum disorders. Child Neuropsychology, 8, 241–248. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Espy KA, & Isquith PK (2003). Behavior Rating Inventory of Executive Function - Preschool Version (BRIEF-P). Lutz, FL: Psychological Assessment Resources, Inc. [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, et al. (2000). Behavior Rating Inventory of Executive Function (BRIEF). Lutz, FL: Psychological Assessment Resources, Inc. [Google Scholar]
- Gresham FM, & Elliott SN (2008). Social Skills Improvement System Rating Scales. San Antonio, TX: Pearson. [Google Scholar]
- Hall ML, Eigsti I-M, Bortfeld H, et al. (2018). Executive function in deaf children: Auditory access and language access. Journal of Speech, Language, and Hearing Research, ePublish ahead of print. 10.1044/2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser PC, Lukomski J, & Hillman T. (2008). Development of deaf and hard-of-hearing students’ executive function In Marschark M & Hauser PC (Eds.), Deaf cognition: Foundations and outcomes (pp. 286–308). New York, NY: Oxford University Press. [Google Scholar]
- Hill D, & Balk D (1987). The effect of an education program for families of the chronically mentally ill on stress and anxiety. Psychosocial Rehabilitation Journal, 10, 25–40. [Google Scholar]
- Hoff E (2003). The specificity of environmental influence: Socioeconomic status affects early vocabulary development via maternal speech. Child Development, 74, 1368–1378. [DOI] [PubMed] [Google Scholar]
- Holt RF, Beer J, Kronenberger WG, et al. (2012). Contribution of family environment to pediatric cochlear implant users’ speech and language outcomes: Some preliminary findings. Journal of Speech, Language, and Hearing Research, 55, 848–864. doi: 10.1044/1092-4388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt RF, Beer J, Kronenberger WG, et al. (2013). Developmental effects of family environment on outcomes in pediatric cochlear implant recipients. Otology and Neurotology, 34, 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt RF, & Svirsky MA (2008). An exploratory look at pediatric cochlear implantation: Is earliest always best? Ear and Hearing, 29, 492–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarratt KP, Riccio CA, & Siekierski B (2005). Assessment of Attention Deficit Hyperactivity Disorder (ADHD) using the BASC and BRIEF. Applied Neuropsychology, 12, 83–93. [DOI] [PubMed] [Google Scholar]
- Kazak AE (1989). Families of chronically ill children: A systems and social ecological model of adaptation and challenge. Journal of Consulting and Clinical Psychology, 57, 25–30. [DOI] [PubMed] [Google Scholar]
- Kazak AE (1992). The Social Context of Coping with Childhood Chronic Illness: Family Systems and Social Support In Stress and coping in child health (La Greca AM, Siegel LJ, Wallander JL, & Walker CE, Eds.). New York, NY: The Guilford Press. [Google Scholar]
- Kirk KI, Miyamoto RT, Lento CL, et al. (2002). Effects of age at implantation in young children. Annals of Otology Rhinology and Laryngology, 189 (Suppl.), 69–73. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Murray KT, & Harlan ET (2000). Effortful control in early childhood: continuity and change, antecedents, and implications for social development. Developmental Psychology, 36, 220–232. 10.1037/0012-1649.36.2.220 [DOI] [PubMed] [Google Scholar]
- Kronenberger WG, Beer J, Catellanos I, et al. (2014a). Neurocognitive risk in children with cochlear implants. JAMA Otolaryngology - Head and Neck Surgery, 140, 608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronenberger WK, Colson BG, Henning SC, et al. (2014b). Executive functioning and speech-language skills following long-term use of cochlear implants. Journal of Deaf Studies and Deaf Education, 2014. 19: p. 456–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronenberger WG, & Pisoni DB (in press). Why are children with cochlear implants at risk for executive functioning delays: Language only or something more? In (Marschark M & Knoors H, Eds), Oxford Handbook of Deaf Studies in Learning and Cognition. [Google Scholar]
- Kronenberger WG, Pisoni DB, Henning SC, et al. (2013). Executive functioning skills in long-term users of cochlear implants: a case control study. Journal of Pediatric Psychology, 38, 902–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronenberger WG, & Thompson RJ Jr. (1990). Dimensions of family functioning with chronically ill children: A higher order factor analysis of the Family Environment Scale. Journal of Clinical Child Psychology, 19, 380–388. [Google Scholar]
- Lederberg AR, & Mobley CE (1990). The effect of hearing impairment on the quality of attachment and mother-toddler interaction. Child Development, 61, 1596–1604. [DOI] [PubMed] [Google Scholar]
- Mangeot S, Armstrong K, Colvin AN, et al. (2002). Long-term executive function deficits in children with traumatic brain injuries: Assessment using the Behavior Rating Inventory of Executive Function (BRIEF). Child Neuropsychology, 8, 271–284. [DOI] [PubMed] [Google Scholar]
- McCreery RW, Walker EA, Spratford M, et al. (2015). Longitudinal predictors of aided speech audibility in infants and children. Ear and Hearing, 36 (Suppl.), 24S–37S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliam R, & Scott S (2001). A support approach to early intervention: A three-part framework. Infants and Young Children, 13, 55–66. [Google Scholar]
- Meadow-Orlans KP, & Steinberg A (1993). Effects of infant hearing loss and maternal support on mother-infant interaction at 18 months. Journal of Applied Developmental Psychology, 14, 407–426. [Google Scholar]
- Mills PD, & Hansen JC (1991). Short-term group interventions for mentally ill young adults living in a community residence and their families. Hospital and Community Psychiatry, 42, 1144–1150. [DOI] [PubMed] [Google Scholar]
- Mitchell RM & Karchmer MA (2004). Chasing the mythical ten percent: Parental hearing status of deaf and hard of hearing students in the United States. Sign Language Studies, 4, 138–163. [Google Scholar]
- Moeller MP (2000). Early intervention and language development in children who are deaf and hard of hearing. Pediatrics, 106, 1–9. [DOI] [PubMed] [Google Scholar]
- Moeller MP (2007). Current state of knowledge: Psychosocial development in children with hearing impairment. Ear and Hearing, 28, 729–739. [DOI] [PubMed] [Google Scholar]
- Moeller MP, & Tomblin JB (2015). Introduction to the outcomes of children with hearing loss study. Ear and Hearing, 36 (Suppl.), 4S–13S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, & Moos BS (2009). Family Environment Scale manual (4th Ed.). Menlo Park: CA: Mind Garden, Inc. [Google Scholar]
- Nikolopoulos TP, Gibbin KP, & Dyar D (2004). Predicting speech perception outcomes following cochlear implantation using Nottingham Children’s Implant Profile (NChIP). International Journal of Pediatric Otorhinolaryngology, 68, 137–141. [DOI] [PubMed] [Google Scholar]
- Niparko JK, Tobey EA, Thal DJ, et al. (2010). Spoken language development in children following cochlear implantation. JAMA, 303, 1498–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C (2004). Theory-of-mind development in oral deaf children with cochlear implants or conventional hearing aids. Journal of Child Psychology and Psychiatry, 45, 1096–1106. [DOI] [PubMed] [Google Scholar]
- Peterson C & Siegal M (1999). Representing inner worlds: Theory of mind in autistic, deaf, and normal hearing children. Psychological Science, 10, 126–129. [Google Scholar]
- Pisoni DB, Conway CM, Kronenberger W, et al. (2010). Executive function and cognitive control in deaf children with cochlear implants In M. S. Marschark PE(Ed.), Oxford Handbook of Deaf Studies, Language, and Education (pp. 439–457). New York: Oxford University Press. [Google Scholar]
- Pisoni DB, Conway CM, Kronenberger WG, et al. (2008). Efficacy and effectiveness of cochlear implants in deaf children In Marschark M & Hauser PC (Eds.), Perspectives on deafness. Deaf cognition: Foundations and outcomes (pp. 52–101). New York, NY, US: Oxford University Press. [Google Scholar]
- Pratt S (1991). Nonverbal play interaction between hearing mothers and young deaf children. Ear & Hearing, 12, 328–336. [DOI] [PubMed] [Google Scholar]
- Pressman L, Pipp-Siegel S, Yoshinaga-Itano C, et al. (1999). Maternal sensitivity predicts language gain in preschool children who are deaf and hard of hearing. Journal of Deaf Studies, 2, 27–36. [DOI] [PubMed] [Google Scholar]
- Quittner AL, Cruz I, Barker DH, et al. (2013). Effects of maternal sensitivity and cognitive and linguistic stimulation on cochlear implant users’ language development over four years. Journal of Pediatrics, 162, 343–348. doi: 10.1016/j.jpeds.2012.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rousey AM, Wild M, & Blacher J (2002). Stability of measures of the home environment for families of children with severe disabilities. Research in Developmental Disabilities, 23, 17–35. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ & Chandler MJ (1975). Reproductive risk and the continuum of caretaking casualty In Horowitz FD, et al. (Eds), Review of Child Development Research. University of Chicago Press: Chicago, IL. [Google Scholar]
- Semel E, Wiig EH, & Secord W (2003). Clinical Evaluation of Language Fundamentals Forth Edition San Antonio: TX: Psychological Corporation. [Google Scholar]
- Surowiecki VN, Sarant J, Maruff P, et al. (2002). Cognitive processing in children using cochlear implants: the relationship between visual memory, attention, and executive functions and developing language skills. Annals of Otology, Rhinology, and Laryngology, 189 (Suppl.), 119–126. [DOI] [PubMed] [Google Scholar]
- Taylor N, Donovan W, Miles S, et al. (2009). Maternal control strategies, maternal language usage and children’s language usage at two years. Journal of Child Language, 36, 381–404. [DOI] [PubMed] [Google Scholar]
- Teagle HRB & Eskridge H (2010). Predictors of success for children with cochlear implants: The impact of individual differences In Weiss A (Ed.), Perspectives on Individual Differences Affecting Therapeutic Change in Communication Disorders. Taylor & Francis/Psychology Press: New York. [Google Scholar]
- Vaccari C, & Marschark M (1997). Communication between parents and deaf children: Implications for social-emotional development. Journal of Child Psychology and Psychiatry, 38, 793–801. [DOI] [PubMed] [Google Scholar]
- Walker EA, McCreery RW, Spratford M, et al. (2015). Trends and predictors of longitudinal hearing aid use for children who are hard of hearing. Ear and Hearing, 36 (Suppl.), 38S–47S. [DOI] [PMC free article] [PubMed] [Google Scholar]