Abstract
According to data compiled by researchers at Johns Hopkins University in Baltimore, Maryland, more than two and half million cases of coronavirus disease 2019 (COVID-19), caused by a newly discovered virus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), have been confirmed on April 20, 2020 (Nature, 2020b). Since the emergence of this infectious disease in Asia (Wuhan, China) late last year, it has been subsequently span to every continent of the world except Antarctica (Rodríguez-Morales et al., 2020). Along with a foothold in every country, the current disease pandemic is disrupting practically every aspect of life all over the world. As the outbreak are continuing to evolve, several research activities have been conducted for better understanding the origin, functions, treatments, and preventions of this novel coronavirus. This review will be a summa of the key features of novel coronavirus (nCoV), the virus causing disease 2019 and the present epidemic situation worldwide up to April 20, 2020. It is expected that this record will play an important role to take more preventive measures for overcoming the challenges faced during this current pandemic.
Keywords: Novel coronavirus, Respiratory disease, Epidemic, Public health
Graphical abstract
Highlights
-
•
Novel coronavirus, SARS-CoV-2 is responsible for coronavirus disease 2019 (COVID-19).
-
•
SARS-CoV-2 has caused for human-to-human transmission worldwide.
-
•
Non-pharmaceutical interventions (NPIs) can reduce the transmission of COVID-19.
-
•
COVID-19 is a crisis for massive health hazard, big humanitarian and development.
-
•
The use of research-based evidence, global response and solidarity may be helpful.
1. Introduction
The most recent outbreak of corona virus disease 2019 (currently known as COVID-19), which can cause severe respiratory disease in humans, has been a potential threat to human health attracting worldwide attention after the 2003 severe acute respiratory syndrome (SARS) pandemic (WHO, 2004), followed by the 2012 middle east respiratory syndrome (MERS) (WHO, 2013). It was originated from the Wuhan city, the capital of China's Hubei province on December 29, 2019 (C. Huang et al., 2020; Zhou et al., 2020b; Zhu et al., 2020). Outside of China, the first case of the disease in Thailand (Joseph, 2020) and Japan (WHO, 2020j) was confirmed on January 13 and 16 respectively. In order to reduce its spreading outside China, Wuhan and other cities in the region were placed on lockdown on January 23 (BBC, 2020d). The disease causing virus has since spread to other regions in Asia, Europe, North America, South America, Africa, and Oceania, developing into a global 2019–2020 COVID-19 pandemic by March (Chan et al., 2020; JHU, 2020; M, 2020; Nature, 2020b; Reuters, 2020a; Reuters, 2020b; Rothe et al., 2020; S, 2020).
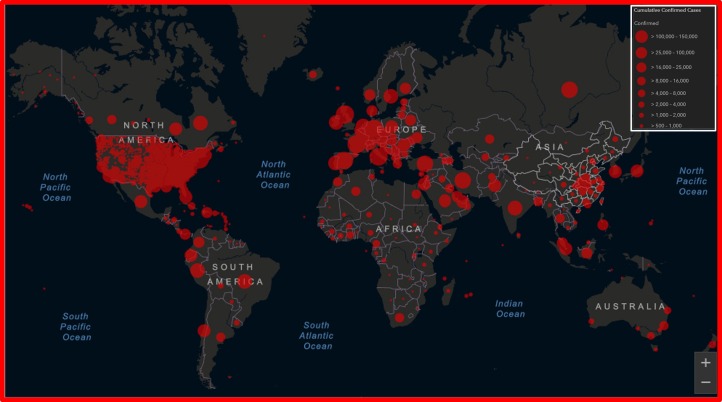
As one of the human corona viruses (HCoVs) is mainly responsible for this infectious disease, the novel virus has now been named as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the International Committee of Taxonomy of Viruses (ICTV) (Gorbalenya et al., 2020; WHO, 2020d). The virus was formerly known as 2019 novel coronavirus (2019-nCoV) named by World Health Organization (WHO). Due to its massive global outbreak followed by China, WHO designated the 2019-nCoV virus as sixth Public Health Emergency of International Concern on January 30 (Wee et al., 2020; WHO, 2020s). In February 2020, WHO announced the official name of this disease for public communications as COVID-19, where CO stands for corona, VI for virus, D for disease, and 19 is for the first outbreak year of that disease (WHO, 2020i). Based on the ongoing global COVID-19 contagion, the WHO declared it a pandemic on March 11, 2020 as there is no safe place from its effects (McKay et al., 2020; WHO, 2020t). According to figures compiled by U.S. based Johns Hopkins University, as of April 20, 2020, >2,480,506 total confirmed cases of COVID-19 have been reported in over 205 countries and territories, resulting in approximately 170,397 deaths whereas >646,330 people have since recovered (JHU, 2020). As of April 20, 2020, the overall rate of deaths per number of diagnosed cases is 6.87% based on Johns Hopkins University statistics (JHU, 2020; Worldometer, 2020a). Fig. 1 shows geographical distribution of current COVID-19 pandemic until April 20, 2020.
Fig. 1.
Geographic distribution of COVID-19 cases worldwide, as of April 20, 2020.
[Source: Adopted from Johns Hopkins University (JHU), Center for Systems Science and Engineering (CSSE): Coronavirus COVID-19 Global Cases, April 20, 2020].
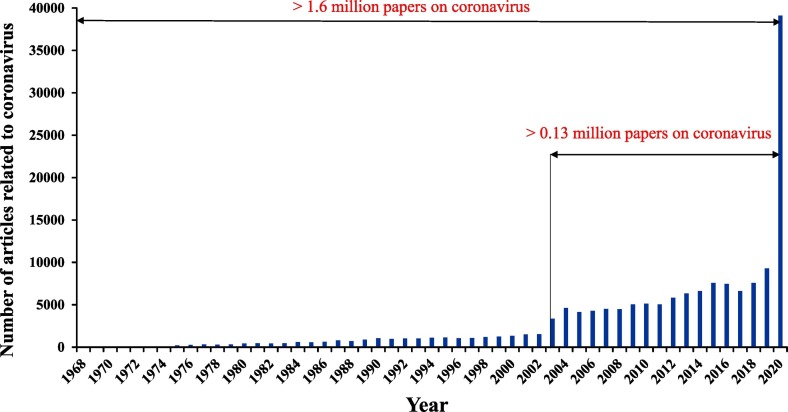
This novel virus is closely linked to the SARS virus (NCPERE, 2020). Although all the coronaviruses have the ability to infect human and develop severe respiratory syndrome, the novel virus has been considered as superior than other coronaviruses, i.e., SARS, MERS, and influenza. Because the number of confirmed infections of COVID-19 is higher than the total number of suspected SARS cases, the novel coronavirus is assumed to be more contagious than SARS with respect to community spread and severity (De Wit et al., 2016). Consequently, the novel CoV is currently spreading from continent to continent, which must be reduced to stop its potentially devastating impact on human. Besides, this epidemic driven to unpredictable future is causing anxiety among people. During this public health emergencies, a lots of information, news and health messages about coronavirus available online and offline when they are not misleading, can be overwhelming and confusing. Hence it is very important to stay informed during this outbreak. Moreover, this novel virus is new to the scientific world and many features of the virus are still not understandable due to its new strains (Qing and Gallagher, 2020). Hence, the worldwide researchers are now very active to explore the new insights of the virus in order to understand its biological character and mode of spreading. This real boost of research interest on the virus has actually started after the emergence of SARS and MARS, and subsequent COVID-19 (Fig. 2 ). According to google scholar search as of April 20, 2020, at least 39,100 English-language papers reporting coronavirus have been published since the outbreak (January 2020) (Stoye, 2020). Already, there are a number of review articles summarizing the epidemiology, pathogenesis, clinical characteristics, and management of COVID-19 (Z. Huang et al., 2020; Jin et al., 2020; Lai et al., 2020a; Lupia et al., 2020; Moriyama et al., 2020; Rodríguez-Morales et al., 2020; Rothan and Byrareddy, 2020; Shereen et al., 2020; Song and Karako, 2020; Vellingiri et al., 2020). However, the ongoing situation has urgently sought for constructive summary about the known features of COVID-19 attack, its current strength of infecting people and future predictions about long-run epidemic. In this review, all the very basic information related to the coronavirus causing infection are highlighted and the current global situation of the disease outbreak are discussed. The purpose of this study is to aggregate as well as present the existing information and the relevant global data on COVID-19 outbreak among vulnerable communities. In this current pandemic situation, this review is expected to be easily understandable and accessible to all categories of readers for providing continuous guidance and effective control for the future outbreaks.
Fig. 2.
The number of papers found in the Google scholar by the topic query “Coronavirus” as of April 20, 2020.
2. Human coronavirus at a glance
A virus is a submicroscopic infectious agent that replicates only inside the living cells of an organism (Wikipedia, 2020d). A complete virus particle is called virion. Viruses can infect all types of life forms, i.e., animals, plants, microorganisms (Koonin et al., 2006). There are millions of types of viruses in the environment (Breitbart and Rohwer, 2005). Among these, human corona viruses (HCoVs) are common in humans causing for around 30% of cases of the common cold (Mahy, 1980; Mesel-Lemoine et al., 2012). In 1968, coronaviruses were first discovered and named so due to their crown-like bulbous appearance (Latin “corona” means crown) in electron micrographs (Nature, 1968) as shown in Fig. 3 . The ubiquitous pathogens, coronaviruses (CoVs) can be found in vertebrates, i.e., birds, fish, amphibians, reptiles, and mammals (Brenda G. Hogue and Machamer, 2008). They are a large family of single-stranded ribonucleic acid (RNA) viruses (Yin and Wunderink, 2018), which can infect human and thus cause a variety of diseases, including respiratory infections, gastroenteritis, encephalitis, and hepatitis(Weiss and Navas-Martin, 2005) Usually, CoVs are enveloped, spherical lipid bilayer (approximately 120 nm in diameter), with a prominent fringe of 20-nm-long, petal shaped surface projections (spikes) composed of a heavily glycosylated type I glycoprotein, spike protein (Masters, 2006). In the structure of CoV, at least three structural (envelope) proteins like membrane (M), envelope (E) and spike (S) are coordinated with a positive-strand RNA genome of approximately 30 kilobases (kb) in length (Schoeman and Fielding, 2019). Some CoVs have additional envelope proteins like hemagglutinin-esterase (HE) and nucleocapsid (N) (Hogue and Machamer, 2008). The structure of CoV is responsible for its vibrant morphological, biological functions or reproductive modes in different environmental conditions.
Fig. 3.

Model of the virions of a coronavirus.
[Reused permission from Fig. 1, Lai and Cavanagh (1997), The Molecular Biology of Coronaviruses, Advances in Virus Research, 48, 1-100. Copyright (1997) Elsevier]
In terms of RNA genome, the four genera of CoVs are alpha-, beta-, gamma-, and delta-coronavirus (Yin and Wunderink, 2018). Among these four genera, alpha- and beta-CoV are mainly responsible for human infection. Till today, seven strains of human CoVs (HCoVs) have been specified causing respiratory tract infections in human (Table 1 ). However, the risk factor or rate of infection of coronaviruses vary significantly. In 1965, Tyrrell and Bynoe first identified a new group of human CoV-OC43 in the respiratory tract of an adult human showing common cold symptoms (Tyrrell and Bynoe, 1966). The SARS outbreak caused by SARS-CoV was emerged 18 years ago in Foshan, Guangdong, China in November 2002 and became epidemic till 2004 infecting over 8000 people and causing death of 774 people from 29 different countries (Businessinsider, 2020). Since 2002, the discovery of a number of SARS-CoVs has been continued from their natural reservoir host, bats. Like SARS-CoVs, MERS-CoV caused a severe respiratory syndrome in humans in 2012 in Middle East (De Groot et al., 2013). Lastly, the epidemic of SARS-CoV-2, a member of beta-coronaviruses, has started in China from December 2019 causing 198 confirmed infections with three fatal cases by January 20, 2020 (WHO, 2020k). In terms of risk factor, SARS-CoV-2 is distinct from SARS, MERS, and influenza (Yin and Wunderink, 2018). According to epidemiologists, the epidemic infectious disease caused by SARS-CoV-2 becomes a pandemic due to its new strains and current spreading from continents to continents (Gorbalenya et al., 2020; Lai et al., 2020b).
Table 1.
Types of HCoVs responsible for health hazard (Yin and Wunderink, 2018).
| Genera of Coronavirus (CoV) | Human Coronavirus (HCoV) | Health hazard | Year of identification |
|---|---|---|---|
| alpha-CoV | HCoV-NL63 | Mild symptoms of common cold | 2004 (Abdul-Rasool and Fielding, 2010) |
| HCoV-229E | Since 1960s (Lim et al., 2016) | ||
| beta-CoV | HCoV-OC43 | Since 1960s (Tyrrell and Bynoe, 1966) | |
| HCoV-HKU1 | 2005 (Lau et al., 2006) | ||
| Severe acute respiratory syndrome-CoV (SARS-CoV) | Potentially severe, respiratory tract infections | 2002 (Thiel, 2007; WHO, 2003) | |
| Middle East respiratory syndrome-CoV (MERS-CoV) | 2012 (De Groot et al., 2013) | ||
| Severe acute respiratory syndrome-CoV 2 (SARS-CoV-2) | January 2020 (Hui et al., 2020) | ||
| gamma-CoV | Unknown | ||
| delta-CoV | Unknown |
3. Basics of coronaviruses
3.1. Origin of infection
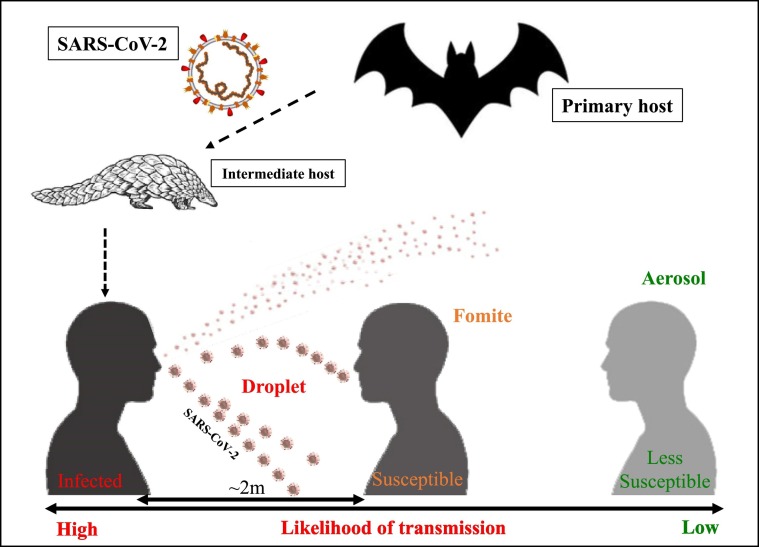
The actual natural reservoir hosts of CoVs remains obscure for centuries. However, the bodies of animals are considered to be the common origin for about 60% of newly emerging and re-emerging pathogens (CDC, 2020c). Recently, it has been reported that most alpha- and beta-CoVs originates from bats (Woo et al., 2012; Woo et al., 2006). Furthermore, several virologic and genetic studies indicated that the origin of SARS-CoV (Li et al., 2005) and MERS-CoV (Ithete et al., 2013) is supposed to be bats, whereas the intermediary hosts before dissemination to humans are palm civets and dromedary camels respectively. The first discovered place of the novel coronavirus (SARS-CoV-2) was reported as a wet market named Huanan Seafood Market, Wuhan, China (Zhu et al., 2020), where there is a chance of transmission of pathogens from wild animals to humans. Like SARS, SARS-CoV-2 has close genetic similarity to bat coronaviruses suggesting its emergence from a bat-borne virus (Benvenuto et al., 2020; N. Chen et al., 2020; Perlman, 2020; Zhou et al., 2020a). Therefore, the most likely natural reservoir of SARS-CoV-2 is bats as recommended by WHO (WHO, 2020r). In addition, pangolin is assumed to be involved as an intermediate animal reservoir for the transmission of novel virus to humans causing COVID-19 (C, 2020; WHO, 2020k).
3.2. Transmission of coronavirus
3.2.1. Transmission from animal to human
The main routes of transmission of SARS and MERS viruses from animal to human were reported to be direct contact with intermediary host animals or consumption of milk, urine, or uncooked meat (Yin and Wunderink, 2018). The intermediate hosts of SARS-CoV-2 are predicted to be the unknown wild animals like pangolins sold at the seafood market of Wuhan in China (N. Chen et al., 2020).
3.2.2. Transmission from human to human
The main routes of transmission of SARS-CoV from human to human was reported to be nosocomial, i.e., hospitals (Jennifer et al., 2016; KoreaCDC, 2015; May et al., 2004). Transmission of MERS and SARS cases between family members was also reported to occur (Kang et al., 2017; Yin and Wunderink, 2018). The COVID-19 pandemic has also been driven due to human-to-human transmission, especially during close contact of people (within 1–2 m) as well as via respiratory droplets produced during when an infected person coughs or sneezes (within a range of about 2 m) (CDC, 2020c; CDC, 2020h; WHO, 2020q). Fig. 4 presents the possibility of COVID-19 transmission from respiratory droplets. It is mostly contagious by symptomatic COVID-19 cases (CDC, 2020c). It is noted that the viral RNA has also been found in stool samples of infected people (Holshue et al., 2020). However, whether the infectious nature of the virus in stool or the risk of transmission of COVID-19 is unknown.
Fig. 4.
Infographic illustration: coronavirus transmission
3.2.3. Indirect transmission via contaminated surfaces and aerosols
Other possible route for transmission of COVID-19 is fomite exposure (CDC, 2020b), which involves an inanimate object to carry a pathogen from one susceptible person to another during touching the surface, followed by eyes, nose, or mouth (Fig. 4). It was reported that the virus can remain viable and infectious for hours in air and for days on surfaces (Van Doremalen et al., 2020). Van Doremalen et al. (2020)) analyzed the stability of human coronaviruses, SARS-CoV-1 (Wu et al., 2020) and SARS-CoV-2 in aerosols and on various surfaces, i.e., plastic, stainless steel, copper, and cardboard. The viability of the coronavirus in aerosols, plastic, stainless steel, copper and cardboard were found to be 3, 72, 72, 4 and 24 h respectively (Van Doremalen et al., 2020).
3.2.4. Transmission due to environmental factors
It was reported that the combination of low humidity, low temperature, lack of sunlight, deficiency of vitamin D may lead to the increased exposure to the respiratory viruses during winter season in temperate regions (Abu-Amer and Bar-Shavit, 1993; Eng et al., 2015; Kokolus et al., 2013; Leigh et al., 2015; Yellon et al., 1999). Due to this fact, the local and systemic antiviral defense mechanisms can be weakened (Moriyama et al., 2020). However, the relation between the mechanisms of respiratory viral infections and the seasonal environmental factors has been causing controversy for many years (Moriyama et al., 2020). These all issues have been discussed by Moriyama et al. (2020), who focused on the linking evidence of outdoor and indoor climates with the seasonality of respiratory viral infections. Therefore, it was suggested that the transmission rate and stability of novel coronavirus (i.e., SARS-CoV-2) can be varied with different environmental parameters, i.e., temperature, humidity, sunlight etc. (Kuiken et al., 2003; Luo et al., 2020; Ma et al., 2020; Peiris et al., 2003). However, there is no strong evidence about decreased transmission rates of SARS-CoV-2 in temperate regions like African countries (Martinez-Alvarez et al., 2020).
3.2.5. Transmission of human to animal
According to World Organization for Animal Health (OIE) and WHO, pet dogs, or cats are not reported to be infected by coronavirus. On April 6, 2020, the first infected animal by coronavirus was reported to have been a tiger in New York City's Bronx Zoo of USA, which might be due to transmission of virus from an asymptomatic zookeeper (BBC, 2020c). This human-to-animal transmission of coronavirus is a matter of warning and could pose a threat to some wildlife like the great apes like wild gorillas, chimps, and orangutans. This issue is still an ongoing study by OIE.
3.3. Record of transmission from COVID-19 patients
According to WHO, the COVID-19 transmission may occur from symptomatic, pre-symptomatic, and asymptomatic people infected with COVID-19. Symptomatic transmission takes place from a person experiencing symptoms. Pre-symptomatic transmission occurs before symptom of COVID-19 onset. Whereas asymptomatic transmission occurs from a person with no symptoms of COVID-19.
On April 2, 2020, WHO provided a brief overview of available evidence on transmission by COVID-19 virus, which is discussed here (WHO, 2020c). It has been reported that COVID-19 has been primarily transmitted from symptomatic people by direct contact or close contact through respiratory droplets, or by indirect contact with contaminated objects and surfaces (Burke et al., 2020; Chan et al., 2020; Jiaye et al., 2020; Ong et al., 2020; WHO, 2020c). A small number of case reports and studies have been found for pre-symptomatic transmission through contact tracing efforts and enhanced investigation of clusters of confirmed cases (R. Huang et al., 2020; W.E. Wei et al., 2020; Yu et al., 2020; Zhen-Dong et al., 2020). Where the contact tracing is a process of identifying persons who may have come in contact with an COVID-19 infected person and subsequent collection of further information about these contacts (Wikipedia, 2020a). To April 20, 2020, there has been no documented asymptomatic transmission (WHO, 2020c). However, this does not mean zero possibility of asymptomatic transmission.
3.4. Symptoms for infection
The COVID-19 infected person (host) may be symptomatic, pre-symptomatic, and asymptomatic (WHO, 2020c). For a symptomatic COVID-19 case, signs and symptoms compatible are developed. A pre-symptomatic case lies on the time between exposure to the virus (becoming infected) and symptom onset. If the host is an asymptomatic carrier, there is no signs or symptoms of infection. In the symptomatic case, flu-like symptoms will be developed (N. Chen et al., 2020; MT, 2020). Table 2 summarizes the signs and symptoms of COVID-19. According to previous studies, mild symptoms are observed in most cases, whereas complicated and very-complicated symptoms are reported for approximately 14% and 5% respectively (NCPERE, 2020; WHO, 2020f). The complicated symptoms include sepsis and septic shock, multi organ failure, including acute kidney injury, and cardiac injury (WHO, 2020f). COVID-19 cases for children are usually less severe than that for adults while co-infection has been observed for children (Cai et al., 2020; WHO, 2020f; Xia et al., 2020). COVID-19 cases for infants are reported to be few with mild illness (M. Wei et al., 2020). It should be noted that COVID-19 symptoms for pregnant and non-pregnant women are almost identical (WHO, 2020f). Moreover, if mild or emergency symptoms of COVID-19 are present, immediate medical attention is advised (CDC, 2020d).
Table 2.
Signs and symptoms of COVID-19.
| Category | Symptoms | Reference |
|---|---|---|
| Asymptomatic | No symptom | (CDC, 2020d) |
| Common/mild symptoms | Fever, cough, and shortness of breath | (CDC, 2020k) |
| Complications/emergency symptoms | Pneumonia and acute respiratory distress syndrome (ARDS) | (CDC, 2020d) |
| Difficulty breathing, persistent chest pain or pressure, confusion, difficulty waking, and bluish face or lips; | (CDC, 2020d) | |
| Other symptoms | Muscle pain, sputum production, diarrhea, sore throat, loss of smell (anosmia), and abdominal pain. | (CDC, 2020d; Hopkins, 2020; Iacobucci, 2020; Palus, 2020) |
| Nausea, vomiting, and diarrhea | (C. Huang et al., 2020; Lai et al., 2020b) | |
| Chest tightness and palpitations | (Zheng et al., 2020) | |
| Less common symptoms | Upper respiratory symptoms, such as sneezing, runny nose, or sore throat | (CDC, 2020k) |
3.5. Mechanism of coronavirus infection and replication cycle
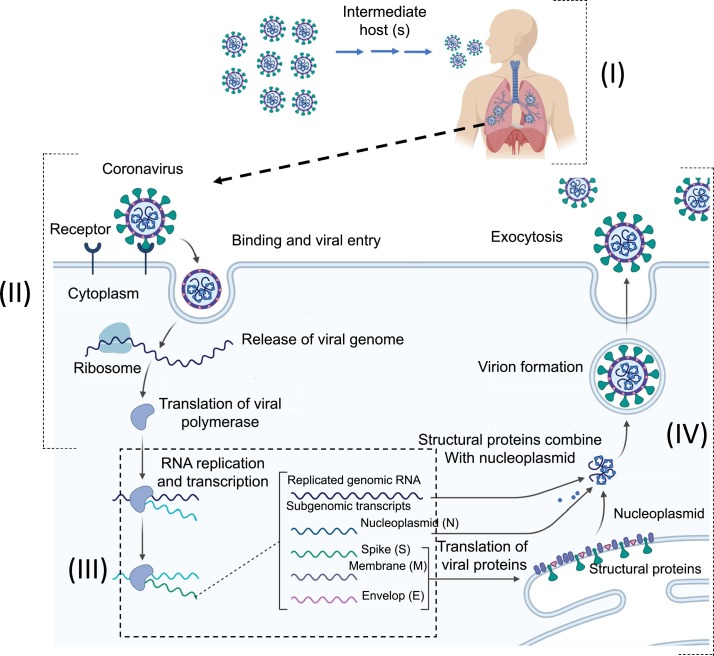
The most affected organ of an infected person (host) due to coronavirus is the lungs in severe cases. The enzyme named, angiotensin converting enzyme 2 (ACE2) is most abundant in the type II alveolar cells of the lungs (Hogan, 2011). The alveoli are hollow cup-shaped little cavities found in the lung structure where gas exchange of breathing process takes place. Type II cells are the most numerous cells in the alveoli. Fig. 5 depicts the coronavirus infection and replication cycle. The infection may proceed in the following way (Letko et al., 2020):
-
I.
First, the virus particle uses its special surface, glycoprotein (spike) to connect to ACE2 of the lungs and thus enters the host cell (Fig. 5a).
-
II.
The virus particle is then uncoated, and its RNA genome enters the cell cytoplasm and attach to the host cell's ribosome by its 5′ methylated cap and 3′ polyadenylated tail. The host ribosome forms a long polyprotein by translating the virus genome and the polyprotein is subsequently cleaved into multiple nonstructural proteins. (Fig. 5b).
-
III.
Then the nonstructural proteins coalesce and form a multi-protein replicase-transcriptase complex (RTC) named RNA-dependent RNA polymerase (RdRp). RdRp synthesizes positive-sense genomic RNA as progeny viruses by replication and positive-sense sub genomic RNA as gene transcripts or messenger RNA (mRNA) by transcription.
-
IV.
The host's ribosomes translate the mRNAs into the structural proteins and a number of accessory proteins inside the endoplasmic reticulum. Then the viral structural proteins (S, E, and M) are combined with nucleocapsid by protein-protein interactions. Finally, the progeny viruses are then released from the host cell.
Fig. 5.
Mechanism of coronavirus infection and replication cycle
The density of ACE2 in each tissue correlates with the severity of the COVID-19 disease in that tissue. As the disease progresses, respiratory failure and consequent death may occur (Xu et al., 2020). ACE2 is also attached to the outer surface of cells in the arteries, heart, kidney, and intestines. As a result, COVID-19 may cause multi-organ failure in extremely severe cases (CDC, 2020d).
3.6. Incubation period for infected cases
Incubation period is the time elapsed between exposure and symptom onset to a pathogenic organism. During this incubation period, an organism can be multiplied and reach a threshold limit, which is necessary to produce symptoms in the host (Wikipedia, 2020b). In order to determine the most likely exposure time for an outbreak of a typical infectious disease, it is very important to know the average as well as range of incubation period (CDC, 2020l). Currently, the incubation period of novel coronavirus is generally between two and fourteen days (Lombardi et al., 2020), with an average of five days (CDC, 2020k). Lauer et al. (2020) estimated the length of the incubation period of COVID-19 for 181 confirmed cases outside Hubei province, China. It was monitored that >97% of people exposed to SARS-CoV-2 were showing symptoms within 11.5 days of exposure whereas the average incubation period was approximately 5 days, which is as similar as SARS. However, longer monitoring periods are suggested to be justified in extreme cases. Therefore, if a person travelled to an ongoing COVID-19 infected area within the previous 14 days, is at high risk and must follow quarantine rules (CDC, 2020c; Jiaye et al., 2020).
3.7. Laboratory tests for coronavirus
3.7.1. Nucleic acid amplification tests (NAAT)
Routine confirmation of cases of COVID-19 is based on the nucleic acid amplification tests (NAAT) by detecting unique sequences of viral RNA (WHO, 2020g). This test can be performed by real-time reverse transcription polymerase chain reaction (RT-PCR) technique. Real-time RT-PCR is a popular technique in molecular biology (Freeman et al., 1999) for monitoring the amplification of a targeted DNA molecule in real time. Whereas RT-PCR combines reverse transcription of RNA into DNA and PCR amplification of the DNA followed by readout using fluorescence (Bustin et al., 2009). The test is done by collecting respiratory or blood samples. The respiratory samples are obtained by a nasopharyngeal swab (Fig. 6 ). The nasopharyngeal swab is a collection method of clinical test sample of nasopharyngeal secretions from the back of the nose and posterior pharynx (WHO, 2020g). The swab used for nasopharyngeal collection is a narrow stick made of a short plastic rod that is covered, at one tip, with adsorbing material such as sterile Dacron or rayon and ensuring viral transport media (WHO, 2020a). The test results are generally available within a few hours to two days. Blood samples can be collected two times in two weeks apart and the results have little immediate value (CDC, 2020j). It is a matter of hope that the country-based genetic sequences of RNA strains of the novel coronavirus have already been isolated and reported (Sah et al., 2020; Wu et al., 2020).
Fig. 6.
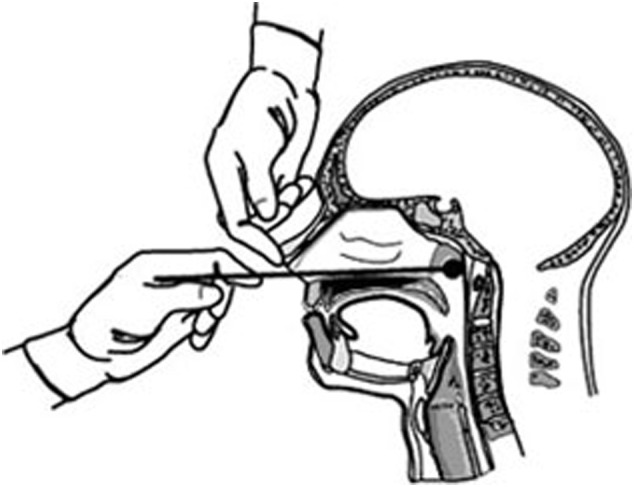
Collection of a clinical test sample of nasopharyngeal secretions (Nasopharyngeal swab).
[Source: Adopted from Fig. 1, Faulkner et al., Chapter 10, Manual for the Surveillance of Vaccine-Preventable Diseases, Centers for Disease Control and Prevention (CDC) United States, 2015]
3.7.2. Serological testing
In cases, where NAAT assays are found to be negative but there is still a strong epidemiological connection to COVID-19 infection with consideration of past events or situations, serological surveys can be used for testing for investigation of the ongoing outbreak (WHO, 2020g). For this purpose, paired serum samples could support diagnosis once validated serology tests are available (WHO, 2020g). Some studies with COVID-19 serological data on clinical samples have been published (Bai et al., 2020; Xiao et al., 2020).
3.7.3. Viral sequencing
Monitoring of the viral genomic mutations is important for better performance of medical countermeasures. Therefore, regular sequencing of novel CoV viral gene are clinically appreciated (WHO, 2020g).
3.7.4. Chest imaging
Chest radiography typically shows patchy or diffuse asymmetric airspace opacities, similar to other causes of corona virus pneumonias in symptomatic patients (Ai et al., 2020). Characteristic imaging features on computerized tomography (CT) scans of the chest of symptomatic patients are useful even before symptom occur (Ai et al., 2020; Salehi et al., 2020). However, this test should not be used to screen for or as a first-line test to diagnose COVID-19 recommended by the American College of Radiology (ACR, 2020).
3.8. Treatments for coronavirus infection
As of April 20, 2020, there is no vaccine (Spinney, 2020), or specific antiviral treatment approved for COVID-19 (WHO, 2020q). However, primary treatment of this disease is symptomatic and supportive therapy (McCreary et al., 2020). The mild symptoms of COVID-19 may be relieved by taking regular over-the-counter medications, drinking fluids, and resting (CDC, 2020i). Whereas severe cases of COVID-19 may require oxygen therapy, conservative fluid managements, breathing support and supporting other affected vital organs (BMJ, 2020; Cheng and Shan, 2020; J, 2020; Liu et al., 2020; Pennsylvania, 2020; Wang et al., 2020; WHO, 2020a). Research toward development of vaccine and testing of existing medication approved for treatment of other viral diseases are ongoing in treating COVID-19 patients (McCreary et al., 2020). The vaccine against novel coronavirus is not expected to become available until 2021 at the earliest (Grenfell, 2020). WHO has provided interim guidance for timely, effective and safe supportive management of patients with suspected and confirmed COVID-19 (WHO, 2020a). The treatment methods of COVID-19 patients recommended by WHO are compiled in the following:
For mild COVID-19 cases
-
√
Patients with mild disease do not require hospital interventions; but isolation is necessary to contain virus transmission and will depend on national strategy and resources.
-
√
Patient with mild COVID-19 require symptomatic treatment such as antipyretics for fever and monitoring.
-
√
Patients with mild COVID-19 should be counseled about signs and symptoms of complicated disease. If they develop any of these symptoms, they should seek urgent care through national referral systems.
For severe COVID-19 cases
-
√
Supplemental oxygen should be provided to the patients immediately.
-
√
Patients with COVID-19 for signs of clinical deterioration, such as rapidly progressive respiratory failure and sepsis should be closely monitored to respond immediately with supportive care interventions.
-
√
The patient's co-morbid condition(s) should be understandable to tailor the management of critical illness.
For severe COVID-19 cases along with co-infections
-
√
Empiric antimicrobials should be given to treat all likely pathogens causing sepsis as soon as possible, within 1 h of initial patient assessment for patients with sepsis.
-
√
Empiric therapy should be de-escalated on the basis of microbiology results and clinical judgment.
For critical COVID-19 cases with acute respiratory distress syndrome (ARDS)
-
√
Severe hypoxemic respiratory failure should be recognized when a patient with respiratory distress is failing standard oxygen therapy and advanced oxygen/ventilatory support should be prepared to provide.
-
√
Endotracheal intubation should be performed by a trained and experienced provider using airborne precautions. Endotracheal intubation is a procedure by which a tube is inserted through the mouth down into the trachea (the large airway from the mouth to the lungs).
3.9. Interventions for prevention of COVID-19
There are mainly two types of approaches to limit the spread of any infectious disease.
-
a.
Pharmaceutical interventions (PIs):
PIs are drug interventions, such as vaccines and anti-viral medications. It is well known that the primary and most effective PI of any infectious disease is vaccination (NIAID, 2016; Orenstein et al., 1985). A vaccine typically contains an agent of the disease-causing microorganism in its weakened or killed forms (Wikipedia, 2020c). After getting vaccination, the antigenic agent stimulates the body's immune system to recognize the agent of the respective disease as a threat and subsequently destroys it. Vaccines for coronaviruses are mostly based on targeting the main antigenic component of the virus, which is S protein. Several strategies have been used that encode the S protein. The most popular strategies are DNA vaccines, subunit vaccines, and attenuated recombinant viruses (ClinicalTrials, 2019; M., 2019). Recently, China and Australia have successfully grown 2019-nCoV to help develop new strategies to combat the pathogen (J., 2020). According to the prior studies related to coronaviruses like SARS and MERS, a genetic platform called mRNA-1273 (messenger RNA) was used to develop the investigational vaccine and examined in human on trial basis (NIAID, 2020). However, there has not yet been approved vaccine and anti-viral medications for SARS-CoV-2 (Grenfell, 2020; Spinney, 2020). This may be because it is highly unlikely that a well-matched vaccine will be available when a pandemic begins unless a vaccine with broad cross-protection is developed (CDC, 2007).
-
b.
Non-pharmaceutical interventions (NPIs):
It is important to take speedy and coordinated public health actions as protective measures, which are known as NPIs. The NPIs have been reporting to be applied for reduction of the chance of COVID-19 transmission and infection among high-risk populations (CDC, 2020i; S. Chen et al., 2020; Horowitz, 2020; Prem et al., 2020; Shao, 2020). Because the individual and population-based preventive measures can minimize the burden of diseases and associated risk factors. In addition, if proper NPI-like counter measures are not taken during a pandemic, the healthcare system could be overwhelmed by severe COVID-19 infected cases and thus the situation cannot be handled effectively (CDC, 2020i; Noreen Qualls et al., 2017).
Fig. 7 shows the effect of taking preventive measures on COVID-19 outbreak indicating that proper counter measures can flatten” the curve of infection and reduce the acute burden on healthcare systems and workers (Qualls et al., 2017). As shown in Fig. 7, if adequate protection is not taken, a fast upswing of COVID-19 infected cases may take place. As a result, the number of infected persons requiring hospitalization may go beyond the capacity of a nation's health-care facilities. On the other hand, protective measures can lower the epidemic peak of COVID-19 cases to the extent possible (CDC, 2007). Therefore, it is highly appreciated to apply protective measures like NPI during this pandemic until the epidemic peak goes down. Different strategies of NPIs for combating COVID-19 are briefly discussed in the following:
-
a.
Individual protection
Fig. 7.
Flattening the COVID-19 Epidemic Curve.
Strategies for self-protection include overall good personal hygiene, washing hands, avoiding touching the eyes, nose, or mouth with unwashed hands, social distancing and avoid travelling (CDC, 2020i). Among all, frequent hand washing is the most powerful preventive measure for an individual to fight the infectious virus. The recommended time for hand washing along with soap and water is at least 20 s (CDC, 2020i). When soap and water are not readily available outside, especially in a public place, hand sanitizer is used as an alternative to soap (CDC, 2020i). Because alcohol-based hand sanitizer containing at least 60% alcohol can disinfect hands by taking a little amount on hand and rubbing them until getting dry (CDC, 2020i). It is advisable not to touch the eyes, nose, or mouth with unwashed hands, which is a major source of infection without proper hand hygiene (CDC, 2020i). During the outbreak, one should avoid close contact with people who are sick.
-
b.
Protecting Population in a community
Fig. 8 is an infographic illustration describing how to prevent the spread of COVID-19 in a community. Strategies for protecting others in a community comprise coughing or sneezing into a tissue and putting the used tissue directly into a waste container; covering one's mouth when coughing; maintaining distance from other people (social distancing); closing of schools, workplaces, stadiums, theatres, or shopping malls; wearing a surgical mask in public place to limit the volume and travel distance of expiratory droplets dispersed when talking, sneezing, and coughing (CDC, 2020a; CDC, 2020i). Among all of these measures, social or physical distancing is intended to slow the spread of disease in a community or country effectively, by minimizing close contact between individuals (approximately 2 m), remaining out of crowded public places, avoiding mass gatherings and working from home (CDC, 2020i). During the outbreaks like COVID-19, people sometimes use the terms quarantine and isolation interchangeably, where there is an important distinction between quarantine and isolation (CDC, 2020i). For example, when there is a possibility of exposure of people to COVID-19, they are put in quarantine to help stopping the spread of the disease. On the contrary, the confirmed COVID-19 patients are put into isolation by completely separating them from others to stop the spreading of the disease into others.
Fig. 8.
Infographic: preventive measures for COVID-19.
[Source: Adapted from Prevention & Treatment, Centers for Disease Control and Prevention (CDC), United States, 15 February 2020]
Having a mask on could cut down on the number of transmissions from asymptomatic people. Because new data cited by Centre for Disease Prevention and Control (CDC) has shown the high rates of transmission by people who are infected but don't know it yet (CDC, 2020c). An infected person can be contagious for 48 h before developing symptoms, if they get them at all. CDC is now considering whether to recommend more people — perhaps everybody — wearing a mask when out in public (NewWorkTimes, 2020). Furthermore, self-isolation at home has been recommended for infected patients by COVID-19 and suspected persons (CDC, 2020g; CDC, 2020m). The suspected persons are those who may have been exposed to someone with COVID-19 and those who have recently travelled to an affected country or region. Hence the suspected persons are advised to self-quarantine for 14 days from the time of last possible exposure. Governments of many countries have already imposed self-quarantine for entire populations living in affected areas (BBC, 2020a; Horowitz, 2020; P et al., 2020; Sattenspiel and Herring, 2003; Zhou, 2020).
-
c.
Prevention on National and International level
Efforts to prevent the virus spreading on national and international level include travel restrictions; screening at airports and train stations; quarantines, curfews, workplace hazard controls, event postponements and cancellations; facility closures; (Beaubien, 2020; Marsh, 2020; Nikel, 2020; P et al., 2020; Shao, 2020; Zhou, 2020) outgoing passenger travel bans (CDC, 2020f; Deerwester and Gilbertson, 2020; NewYorkTimes, 2020). It is also recommended to clean and disinfect the frequently touched surfaces used in public places daily. The contaminated surfaces of public places may be decontaminated with a number of solutions (within one minute for a stainless steel surface), including 62–71% ethanol, 50–100% isopropanol, 0.1% sodium hypochlorite, 0.5% hydrogen peroxide and 0.2–7.5% povidone‑iodine. Other solutions such as benzalkonium chloride and chlorhexidine gluconate are less effective (CDC, 2020i).
-
d.
Using personal protective equipment
Personal protective equipment (PPE), which is designed to protect the wearer's body from infection, may be worn for job-related occupational safety and health purposes to reduce exposure of employee to the current hazards (transmission of coronavirus) to acceptable levels, especially in healthcare settings when performing procedures that can generate aerosols, such as intubation or hand ventilation (Cheung et al., 2020). During the current pandemic, CDC outlines the specific guidelines for the use of personal protective equipment (PPE). The recommended gear includes N95 respirator, facemask, face shields, gown, medical gloves, and eye protective googles.
-
e.
Nonpharmaceutical interventions during winter
NPIs are gaining attention to achieve better prevention of respiratory viral infections during winter (Moriyama et al., 2020). The tips of NPIs applied during winter were reported previously (Moriyama et al., 2020) and revised in Table 3 . However, these actions may also be practiced during other seasons to minimize the magnitude of the current pandemic.
Table 3.
Tips for limiting respiratory virus transmission in winter.
| Tips | Related reference(s) |
|---|---|
| Humidification of indoor air to maintain humidity to 40–60% relative humidity at room temperature | (Lester, 1948; Lowen and Palese, 2009; Lowen et al., 2007; Reiman et al., 2018; Yang et al., 2012) |
| Ventilation of indoor air | (Schulman and Kilbourne, 1962) |
| Wearing face mask to keep the nose warm and moist | (Foxman et al., 2015; Foxman et al., 2016; Kudo et al., 2019; Williams et al., 1996) |
| Vitamin D supplement to compensate for short daylight–induced Vitamin D deficiency | (Abu-Amer and Bar-Shavit, 1993; Lee and Shah, 2012; Rondanelli et al., 2018; Yellon et al., 1999) |
| Sleeping >7 h/day | (Besedovsky et al., 2019) |
| Washing hands to prevent indirect contact transmission | (Lee and Shah, 2012; Warren-Gash et al., 2013) |
[Reused permission from Table 2, Moriyama et al. (March 16, 2020) (Moriyama et al., 2020) Copyright (03 March 2020) Springer Nature].
4. Epidemiology of COVID-19
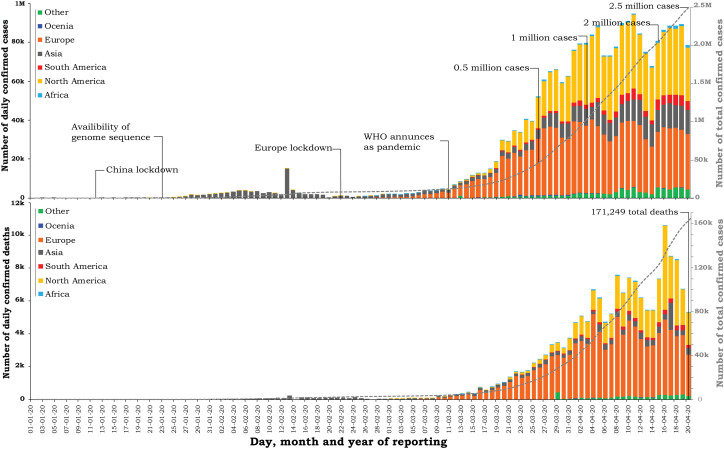
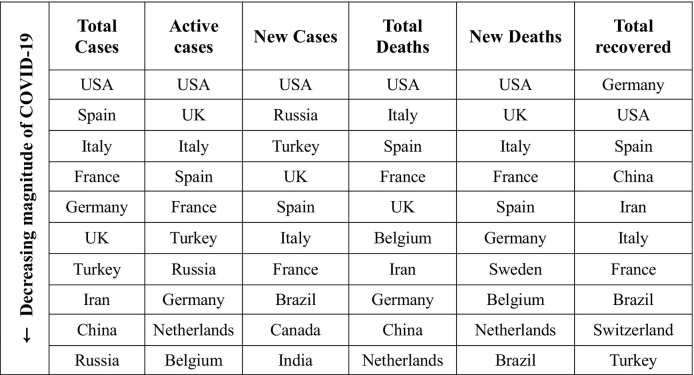
This section includes countries and territories affected by and their responses to the coronavirus responsible for the ongoing COVID-19 up to April 20, 2020. Fig. 9 is the statistical chart by continents showing daily and total confirmed cases and deaths of COVID-19 by date of case reporting through April 20, 2020, which can be used to visualize the onset and progression of the COVID-19 outbreak. It has been observed that how the total number of confirmed cases, and the number of daily new confirmed deaths have changed since December 31, 2019. The higher magnitude of COVID-19 infection has been obtained for Europe and America than that for Asia, while Europe and America show almost similar strength of infection [Fig. 9 (top)]. In case of Asia, the strength of COVID-19 infection is slightly increasing from 25 March 2020. Europe and America have the highest numbers of deaths among all of the continents while Europe has positioned on the top [Fig. 9 (Bottom)]. In order to obtain an epidemic peak, it is assumed that the most likely time period of the current disease exposure that led to the outbreak will probably be the next couple of weeks. Table 4 shows the current trend of total/new/active cases and total/new deaths and total recovered for top ten countries, where cases refer to the numbers of people who have been tested positive for COVID-19 according to official protocols (WHO, 2020g).
Fig. 9.
Distribution of COVID-19 a) confirmed cases and b) deaths worldwide, by continent, as of April 20, 2020 (according to the applied case definition and testing strategies in the affected countries).
[Source: European Centre for Disease Prevention and Control, Situation update worldwide, as of April 20, 2020, https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases]
Table 4.
The list of most affected countries (top 10) having critical trend of COVID-19 outbreak as of April 20, 2020.
[Data are collected from Johns Hopkins University (JHU) (JHU, 2020) and Worldometer (Worldometer, 2020b)].
4.1. Asia
The 2019–20 coronavirus pandemic began in Asian region, China, which eventually spread to the rest of China (CGTN, 2020) and subsequently throughout the continent. As of April 20, 2020, the most affected Asian countries after China were Turkey, Iran, India, Israel, Saudi Arabia, Japan, South Korea etc. It should be mentioned that South Korea, a vibrant capitalist democracy, along with Taiwan and Singapore, has managed the virus with transparency, efficiency and solidarity, while preserving freedom of movement (Cave and May, 2020). The total number of confirmed COVID-19 cases for the top ten most affected countries in the Asian region decreased in the order as (April 20, 2020) (JHU, 2020): Turkey (95,591) > Iran (84,802) > China (82,758) > India (20,080) > Israel (13,942) > Saudi Arabia (11,631) > Japan (11,512) > South Korea (10,683) > Pakistan (9565) > Singapore (9125).
4.2. Europe
Europe was considered as the active centre of COVID-19 after the situation improved in China (WHO, 2020b). Initial cases in Europe were reported in France (WHO, 2020m), Germany (WHO, 2020n), and Finland (WHO, 2020o) with a relatively low number of cases. As of March 13, 2020, some countries of Europe, i.e., Italy, France, Germany, and Spain showed doubling every 2 to 4 days (Roser et al., 2020). However, all countries within Europe have been affected by a confirmed case of COVID-19, with Montenegro, the last European country to report at least one case (Twitter, 2020). As of April 20, 2020, the total number of cases in Montenegro was 313 (IPH, 2020). The most affected European country was Italy till April 2, 2020 update, which had the second-highest fatality rate as of April 20, 2020 (WHO, 2020c). The large outbreak reported in Italy was on 21 February, mostly in the north near Milan city, which is the second-most populous city in Italy after Rome. As of April 20, 2020, Spain was the most affected European country, which had the world's third-highest number of fatalities (JHU, 2020) (Table 4). As of April 20, 2020, there were 21,282 confirmed deaths in Spain. Cases grew rapidly as the outbreak spread across Europe. The total number of confirmed COVID-19 cases for the top ten most affected countries in the Europe region decreased in the order as (April 20, 2020) (JHU, 2020): Spain (204,178) > Italy (183,957) > France (158,050) > Germany (148,453) > United Kingdom (129,044) > Russia (52,763) > Belgium (40,956) > Netherlands (34,134) > Switzerland (28,063) > Portugal (21,379).
4.3. North America
Until April 20, 2020, all North American countries reported for COVID-19 infections. The first case in North America was reported in the United States on January 23, 2020 (WHO, 2020l). As of April 20, 2020, the United States nationally was in the acceleration phase of the pandemic with largest number of confirmed coronavirus cases in the world (Table 4) along with first ranking in the number of total deaths from the virus (JHU, 2020; McNeil and Donald, 2020). All the 50 states of U.S. have reported cases of COVID-19 to Centers for Disease Control and Prevention (CDC). Until April 20, 2020, Canada and Mexico were the second and third most affected countries by COVID-19 respectively, in North America (JHU, 2020). The total number of confirmed COVID-19 infection cases of the top ten most affected North American countries decreased in the order as (April 20, 2020) (JHU, 2020): USA (818,744) > Canada (38,422) > Mexico (8772) > Dominican Republic (5044) > Panama (4658) > Cuba (1137) > Costa Rica (669) > Honduras (494) > Guatemala (294).
4.4. South America
The COVID-19 virus was first reported in South America in São Paulo, Brazil on February 26 (Worldometer, 2020b). The total number of confirmed COVID-19 cases for the top ten most affected South American countries decreased in the order as (April 20, 2020) (JHU, 2020): Brazil (43,079) > Peru (17,837) > Chile (10,832) > Ecuador (10,398) > Colombia (4149) > Argentina (3144) > Bolivia (598) > Uruguay (543) > Venezuela (288) > Paraguay (208).
4.5. Africa
The COVID-19 pandemic was confirmed to have spread to Africa on February 14, 2020 as the first confirmed in Egypt on February 13, 2020 (BBC, 2020a; Egypt, 2020) whereas the first identified case in sub-Saharan Africa was in Nigeria on February 27, 2020 (Adepoju, 2020; BBC, 2020e). As of April 20, 2020, confirmed cases were found in most African nations, whereas three African sovereign states have yet to report a case of COVID-19: Comoros, Lesotho, and São Tomé and Príncipe. There have been no reported cases in the territory of Saint Helena, Ascension and Tristan da Cunha. Most of the identified cases have arrived from Europe and the United States rather than from China (Maclean, 2020). The total number of confirmed COVID-19 cases for the top ten most affected African countries decreased in the order as (April 20, 2020) (JHU, 2020): Egypt (3490) > South Africa (3465) > Morocco (3209) > Algeria (2811) > Cameroon (1163) > Ghana (1042) > Djibouti (945) > Ivory Coast (916) > Tunisia (901) > Niger (782). It is a matter of warning about the effects of COVID-19 pandemic spreading to Africa due to the challenging facts (Ahmed, 2020; Maclean, 2020) availed in that region for a long time like inadequate healthcare systems (lack of equipment, lack of funding, insufficient training of healthcare workers, and inefficient data transmission); challenging hand washing, physical distancing as well as lockdowns; prevalence of ongoing diseases (BBC, 2020b) such as malaria, HIV, tuberculosis, and cholera. Following these facts, many countries on the African continent have already been provided laboratory set up facilities for COVID-19 testing by WHO (Braubien, 2020) along with many preventive measures, i.e., travel restrictions, flight cancellations, event cancellations, school closures, and border closures.
4.6. Oceania
The COVID-19 pandemic was confirmed to have reached Oceania in January 2020 with first confirmed case in Melbourne, Victoria, Australia on 25 January 25 (AGDH, 2020b). On March 1, it was reported that a 78-year-old man from Western Australia, who was a passenger on the Diamond Princess, had become the first person to die from coronavirus in Australia (AGDH, 2020a; Daoud, 2020). The total number of new cases in Australia (AGDH, 2020a) grew exponentially and then leveled out at about 360 per day since March 22. Cases have been reported in all Oceanian sovereign states except Kiribati, Marshall Islands, Federated States of Micronesia, Nauru, Palau, Samoa, Solomon Islands, Tonga, Tuvalu and Vanuatu, and have not been reported in the associated states of Cook Islands and Niue. Many small Pacific island nations have thus far avoided the outbreak by closing their borders. No cases have been reported in the Autonomous Region of Bougainville, Norfolk Island, Wallis and Futuna, Tokelau, Pitcairn Islands, and American Samoa. The total number of confirmed COVID-19 cases for the Oceanian countries decreased in the order as (April 20, 2020) (JHU, 2020): Australia (6645) > New Zealand (1445) > French Polynesia (57) > New Caledonia (18) > Fiji (18) > Papua New Guinea (7).
4.7. Countries free of COVID-19
A handful of countries worldwide have escaped from COVID-19 outbreak so far, at least apparently. As of April 20, 2020, around ten countries - some from Pacific nations and others from the Africa and Asia region have no confirmed cases (Aydogan, 2020; JHU, 2020). The Asian countries free of COVID-19 are Turkmenistan, Tajikistan, and North Korea whereas the African countries like Lesotho have not reported any COVID-19 cases until April 20, 2020. The popular tourist destinations during normal times are Pacific Island nations, some of which are apparently untouched by the coronavirus. These countries and regions include Tonga, Samoa, Vanuatu, the Cook Islands, Niue, and Tuvalu. The reasons behind this free of coronavirus cases could be considered of their strong isolation and remoteness. Therefore, island nations are assumed to be the original self-isolators in the current perspective.
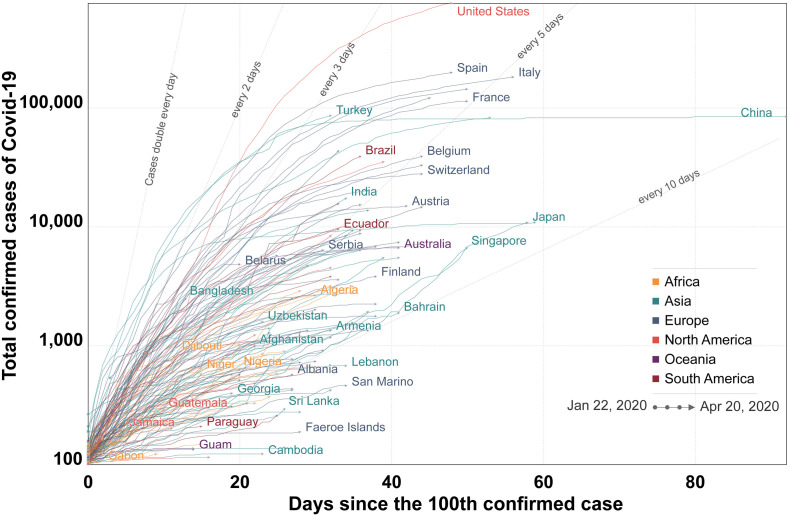
4.8. Statistical research on COVID-19 epidemic
As it is currently noticed that different parts of the globe are seeing different levels of COVID-19 effects. Because the duration and severity of each pandemic phase can vary depending on the characteristics of the virus and the public health response (CDC, 2020e). Roser et al. (2020) reviewed the existing global data sources and global statistics published by the European Center for Disease Prevention and Control (ECDC). According to the statistical data of ECDC, Fig. 10 was revised in this study for showing the speed of increasing the number of cases in each country since the 100th confirmed cases (from January 22 to April 20, 2020) (Roser et al., 2020). The straight grey lines in Fig. 10 indicate trajectories for a doubling time of 2 days, 3 days, 5 days, and 10 days, where the “trajectory” is the standard starting place for each line on the graph. According to Fig. 10, if a country's line is higher than those lines, then its number of cases is doubling faster than that (Roser et al., 2020). For example, the trajectory of China had a particular faster rise than other countries like Singapore and Japan. Whereas China and South Korea have showed rapid initial rise. However, this has become plateau after implementing preventive measures and new daily confirmed deaths have been declined. Thus, this graph would be useful to know whether cases in a country now would grow faster, slower, at the same speed as of other countries when it had a similar number.
Fig. 10.
The speed of increasing the number of COVID-19 cases in each country since the 100th confirmed case (from January 22 to April 20, 2020).
[Source: European Center for Disease Control, Updated April 20, 2020, 12.00 (London time) https://ourworldindata.org/coronavirus]
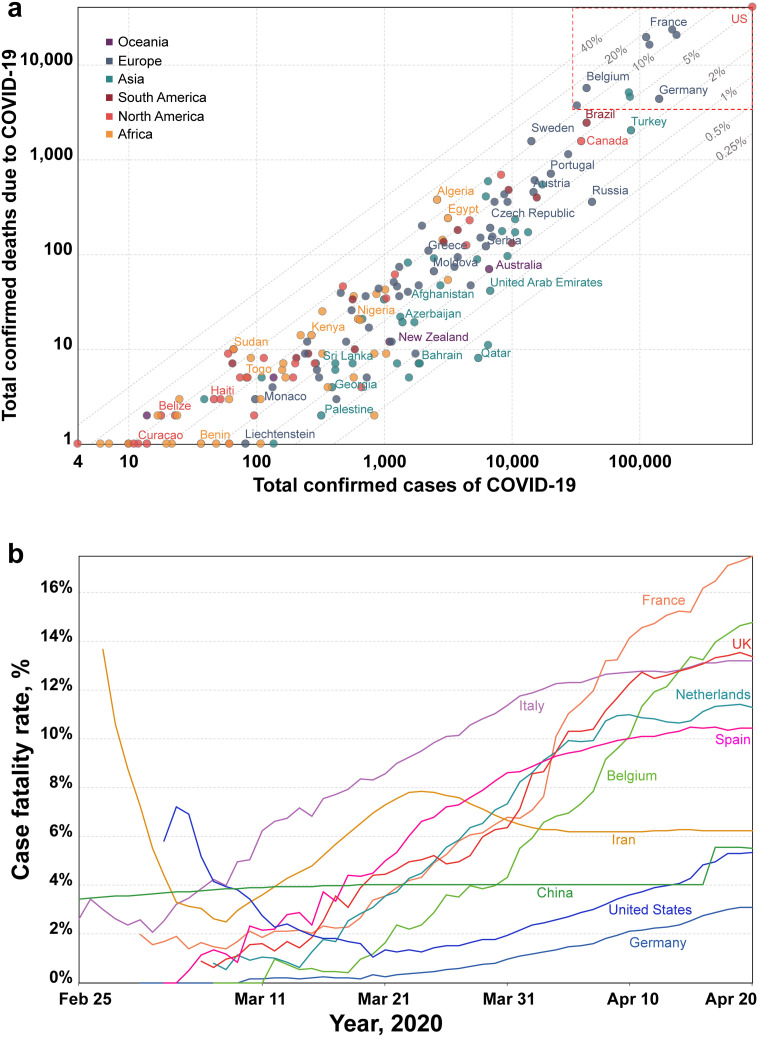
In order to understand the mortality risk of a country, case fatality rate (CFR) can be used as an effective tool, which can be obtained by the number of deaths divided by the number of confirmed cases. CFR can change with time, location, number of testing, demography, characteristics of heath care facilities, and other unknown factors. When there is a relatively large number of confirmed cases, CFR can be informative about the severity of the disease and thus proper actions can be implemented in order to minimize the strength of the outbreak. The current CFR of COVID-19 in all continents presented by Roser et al. (2020)) was reviewed in Fig. 11 . Fig. 11a shows the comparison of CFR values among countries up to April 20, 2020, where the grey lines are the range of CFR values from 0.25% to 10%. Countries lain along these lines indicate their CFR values. For example, a country lies along the 0.25% line indicating that it has a CFR of 0.25%. The highest CFRs have been observed for those countries falling on the uppermost lines. Based on the number of deaths, the points with red dotted boundary correspond to the ten most affected countries by COVID-19 worldwide.
Fig. 11.
Current case fatality rate of COVID-19: a) Comparison of CFR values with number of confirmed cases and deaths in the affected countries up to April 20, 2020; b) CFR over time (from February 25 to April 20, 2020) for ten top countries having higher CFR on April 20, 2020.
[Source: European Center for Disease Control, Updated April 20, 2020, 12.00 (London time) https://ourworldindata.org/coronavirus]
Fig. 11b shows the CFR from February 25 to April 20, 2020 for top ten countries with comparatively higher CFR. It has been observed that CFR has changed over time in these countries. The CFR > 5% has been obtained for six countries and decreased in the following order: France > Belgium > UK > Italy > Netherlands > Spain > Iran. It should be noted that CFR is a poor metric to understand the mortality risk for relatively small number of confirmed cases. The major contributing factors for high fatality of COVID-19 cases across the whole world may be higher population density or higher rate of international travel. Additionally, a recent study found that coronavirus mortality rates are higher in countries, i.e., Italy, Spain, France, and Germany where the level of air pollutant like nitrogen dioxide (NO2) is high (Ogen, 2020). Because long-term exposure to NO2 may weaken the lungs of people living in air-polluted areas and thus result in potential fatality caused by the COVID-19 virus.
4.9. Suggestive strategies to respond to COVID-19
As the world is in initial stage facing COVID-19, the global health community are trying hard to afford this situation. There are post-haste priorities during this outbreak suggested by Experts of CDC (CDC, 2020b):
-
1.
Vaccine development: As vaccines can dramatically slow the spread of a disease, it should be the first priority. However, it will take at least a year to develop the vaccine for SAR-CoV-2.
-
2.
Genome sequence: The identification of genome sequence for RNA strains of SAR-CoV-2 can be implemented in the laboratories across the world to develop PCR-based tests independently in order to analyze infection caused by the virus.
-
3.
Finding treatments: Research and tests of possible antiviral medications should be performed for treatment options.
-
4.
Expansion of diagnostic capacity: In order to identify the COVID-19 cases quickly, rapid diagnostic kits should be developed.
-
5.
Boosting of hospital readiness: The health facilities, i.e., infection control procedures, training of health workers, available stock of gowns, and gloves should be enriched.
-
6.
Communication: All features related to COVID-19 pandemic must be shared clearly with the public, and resisted the temptation to withhold bad news.
5. Current and upcoming challenges
In the COVID-19 pandemic scenario, it has already been noticed that all the countries affected by COVID-19 are racing to slow the spread of the virus by testing and treating patients, carrying out contact tracing, limiting travel, quarantining citizens, and cancelling large gatherings such as sporting events, concerts, and schools (UNDP, 2020a). In this ongoing situation, there may be a possibility of disruption to critical supply markets, i.e., surgical masks, N95 masks, gloves, goggles, and face shields, where demand outpaces global supply. Furthermore, the COVID-19's increased demand for medicines, vaccines, diagnostics and reagents, could create opportunities for ill-intended persons to distribute falsified medical products (WHO, 2020e). As a result, there are growing number of falsified medical products available that claim to prevent, detect, treat, or cure COVID-19. Due diligence is required from consumers, healthcare professionals, and health authorities in the procurement, use and administration of medical products, in particular those affected by the current crisis of, or related to, COVID-19 (WHO, 2020e). As no pharmaceutical products have yet been shown to be safe and effective for the treatment of COVID-19 (WHO, 2020p), doctors should not prescribe medications that have not been approved for this disease. The use of licensed medicines for indications that have not been approved by a national medicines regulatory authority is considered “off-label” use (WHO, 2020p). The prescription of medicines for off-label use by doctors may be subject to national laws and regulations. Unnecessary stockpiling and the creation of shortages of approved medicines that are required to treat other diseases should be avoided. Besides, all hospitals of every continent should be prepared during this outbreak for identifying and managing COVID-19 patients (Jansson et al., 2020).
Since early of 2020, people have been staying indoors across the world for being safe from getting infected or spreading the virus. Almost all the cities of affected countries are seemed to be turn into ghost-cities. Small island nations, which are significantly dependent on tourism, have now their hotels customer-less and beaches without people (UNDP, 2020a). Factories are closing and thus people are losing their jobs as well as income every day. The International Labour Organization estimates that 25 million jobs could be lost, which could lose at least US$220 billion in income in developing countries (ILO, 2020). Hence, the living conditions in the world has been turning into hostile environment for human being. Countries already in crisis because of conflicts, natural disasters, and climate change are most at risk (Maxmen, 2020). Furthermore, countries with fragile institutions and weak health systems, huge numbers of people could die in the short term, (Maxmen, 2020) including many of the millions of vulnerable people living in unruly and under-resourced refugee camps (Berglof, 2020). One of the most stressful situations is the unpredictability of the situation and the uncertainty of when to control the disease and the seriousness of the risk (Zandifar and Badrfam, 2020). As a result, factors like uncertain future, travel bans, social distancing, home quarantine, possibility of COVID-19 infections, and isolation of patients etc. during the current outbreak has caused public panic and mental health stress (Bao et al., 2020). Moreover, it is realizable from the current ongoing situation that the current COVID-19 pandemic is the greatest challenge we have faced since World War II (Two). As confirmed COVID-19 cases are increasing every day in many countries, it has become much more than a global health crisis, which is thus creating a global stress with devastating mental, social, economic, and political crises while reversing development gains achieved over the last 20 years.
Now, every country needs to act immediately to prepare, respond, and recover for the current pandemic. The national and international public and private organizations must join the current COVID-19 fight in order to eradicate poverty, reduce inequalities, and build resilience to crises and shocks (Gonçalves-Sá, 2020). Already, several international organizations have started to support the COVID-19 affected countries. For example, WHO encourages the sharing of data for better understanding to manage the COVID-19 outbreak, and to develop countermeasures (WHO, 1948). In addition, WHO Operation Support and Logistics (OSL) continues to monitor critical markets and in partnership with the Pandemic Supply Chain Network (WHO, 2020c). Since the beginning of the outbreak, OSL has shipped >8,00,000 surgical masks, 54,000 N95 masks, 8,73,000 gloves, 15,000 goggles and 24,000 face shields to 75 countries and also COVID-19 testing kits to 126 countries (WHO, 2020c). United Nations Development Programme (UNDP) has been supporting countries since the very early stages of this crisis, donating more than two million surgical masks and providing life supporting medical equipment, such as X-ray machines, infrared thermometers, infusion pumps, protective suits, gloves, and hand sanitizer (UNDP, 2020a). UNDP is also supporting health systems in countries including Bosnia, Herzegovina, Djibouti, El Salvador, Eritrea, Iran, Kyrgyzstan, Madagascar, Nigeria, Paraguay, Panama and Ukraine (UNDP, 2020a). Additionally, United Nations Secretary-General António Guterres has launched a US$2 billion global humanitarian response plan in the most vulnerable (UNDP, 2020b). The World Bank, which has a long record of supporting health care, has announced an initial package of up to $12 billion in immediate support to affected countries (WorldBank, 2020).
The fastest exchange of scientific knowledge with scientific journals has already been observed in human history due to the current pandemic (Berglof, 2020). An effective global strategy must support the effort to develop and distribute a vaccine. For starters like COVID-19 pandemic, vaccination could be the primary preventive measure of the disease (Berglof, 2020). However, there is no guarantee that other novel virus will not emerge in future, for which millions may die before developing respective vaccines (Berglof, 2020; UNDP, 2020a). Therefore, the use of research-based evidence (Nature, 2020a; Yang and Wang, 2020) and coping with steep learning curves may strengthen the weakest links in an individual hospital, a local community, a country, or the world during this current pandemic (Berglof, 2020). At the same time, the weak health-care systems must be shored up for the worst-case scenario. Lastly, fast and large-scale efforts must be designed as well as considered to handle not only the imminent flood of cases but also pandemic recurring and future waves of similar viruses (Berglof, 2020). Because, weaker health education can be as damaging as the virus itself and thereby, improved health education is one of the important tools to fight the unknown pathogens like novel viruses. Assuming this view, the Director-General of WHO has stated that the world is fighting an epidemic as well as infodemic” (WHO, 2020h).
6. Conclusion
COVID-19 is not only a massive health crisis but also a humanitarian and development crisis. The pandemic is moving like a wave leaving in deaths, damaging immune systems, and weakening economies globally. There is, actually, no way of knowing when all the situation will come back to normal life. Now all the countries are in uncharted territory due to global threat of the current COVID-19 pandemic. To overcome this dark period, a global response as well as solidarity must be an investment in our future in order to support the most vulnerable countries, which cope with this unfolding crisis. Because, from climate change to the next pandemic, global response and solidarity could lay the groundwork for a new, nimbler alliance of multiple countries for handling future challenges. These extra efforts will pay off when the next one strikes. Therefore, it can be assumed that the performance of the current world leaders will be reviewed by the future historians in addressing the COVID-19 pandemic. It is time for government of every country to emphasis and invest more on research and development to overcome this pandemic and prevent any future crisis like this.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This research work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2017R1D1A1B03032189). Authors are thankful to Dr. Tahmeed Ahmed and Dr. Mustafa Mahfuz of International Centre for Diarrhoeal Disease Research, Bangladesh (icddr'b) for their valuable comments about the importance of this study.
Editor: Jianmin Chen
References
- Abdul-Rasool S., Fielding B.C. Understanding human coronavirus HCoV-NL63. Open. Virol. J. 2010;4:76–84. doi: 10.2174/1874357901004010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu-Amer Y., Bar-Shavit Z. Impaired bone marrow-derived macrophage differentiation in vitamin D deficiency. Cell. Immunol. 1993;151:356–368. doi: 10.1006/cimm.1993.1245. [DOI] [PubMed] [Google Scholar]
- ACR . American College of Radiology; 2020. ACR Recommendations for the Use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. [Google Scholar]
- Adepoju P. 2020. Nigeria Responds to COVID-19; First Case Detected in Sub-Saharan Africa, Nature Medicine (News Feature) [DOI] [PubMed] [Google Scholar]
- AGDH . Australian Government Department of Health; 2020. Coronavirus (COVID-19) Current Situation and Case Numbers. [Google Scholar]
- AGDH . 2020. First Confirmed Case of Novel Coronavirus in Australia. [Google Scholar]
- Ahmed K. The Guardian; 2020. World’s Most Vulnerable in ‘third Wave’ for Covid-19 Support, Experts Warn. [Google Scholar]
- Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aydogan M. Anadolu Agency; 2020. World, Health, Latest on Coronavirus Outbreak: Some Countries Still Without Confirmed Virus Cases. [Google Scholar]
- Bai S.L., Wang J.Y., Zhou Y.Q., Yu D.S., Gao X.M., Li L.L. Analysis of the first cluster of cases in a family of novel coronavirus pneumonia in Gansu Province. Chin. J. Prev. Med. 2020;54:e005. doi: 10.3760/cma.j.issn.0253-9624.2020.0005. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC . BBC News; 2020. Beijing Orders 14-Day Quarantine for All Returnees. [Google Scholar]
- BBC . BBC News; 2020. Coronavirus: Could African Countries Cope With an Outbreak? [Google Scholar]
- BBC . 2020. Coronavirus: Tiger at Bronx Zoo Tests Positive for Covid-19, BBC News (US and Canada) [Google Scholar]
- BBC . BBC; United Kingdom: 2020. Lockdowns Rise as China Tries to Control Virus. [Google Scholar]
- BBC . BBC News; 2020. Nigeria Confirms First Coronavirus Case. [Google Scholar]
- Beaubien J. Nevada Public Radio; 2020. Coronavirus Update: Masks and Temperature Checks in Hong Kong. [Google Scholar]
- Benvenuto D., Giovanetti M., Ciccozzi A., Spoto S., Angeletti S., Ciccozzi M. The 2019-new coronavirus epidemic: evidence for virus evolution. J. Med. Virol. 2020;92:455–459. doi: 10.1002/jmv.25688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berglof E. Project Syndicate; USA: 2020. A Pandemic Strategy As Global as COVID-19. [Google Scholar]
- Besedovsky L., Lange T., Haack M. The sleep-immune crosstalk in health and disease. Physiol. Rev. 2019;99:1325–1380. doi: 10.1152/physrev.00010.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BMJ Overview of novel coronavirus (2019-nCoV)—summary of relevant conditions. The BMJ Best Practice. 2020 [Google Scholar]
- Braubien J. NPR; 2020. African Countries Respond Quickly to Spread of COVID-19. [Google Scholar]
- Breitbart M., Rohwer F. Here a virus, there a virus, everywhere the same virus? Trends Microbiol. 2005;13:278–284. doi: 10.1016/j.tim.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Burke R.M., Midgley C.M., Dratch A. 2020. Active Monitoring of Persons Exposed to Patients with Confirmed COVID-19 — United States, January–February 2020; pp. 245–246. (Morb. Mortal. Wkly. Rep. 69). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Businessinsider . 2020. How SARS Terrified the World in 2003, Infecting More than 8,000 People and Killing 774 Businessinsider. [Google Scholar]
- Bustin S.A., Benes V., Garson J.A., Hellemans J., Huggett J., Kubista M. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin. Chem. 2009;55:611–622. doi: 10.1373/clinchem.2008.112797. [DOI] [PubMed] [Google Scholar]
- C S. Deutsche Welle; 2020. Coronavirus: From Bats to Pangolins, how Do Viruses Reach us? [Google Scholar]
- Cai J., Xu J., Lin D., Yang Z., Xu L., Qu Z. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cave D., May T. Now the Tables Are Turned. 2020. World feared China over coronavirus. [Google Scholar]
- CDC . Centers for Disease Control and Prevention; US: 2007. Interim Pre-pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States: Early, Targeted, Layered Use of Nonpharmaceutical Interventions. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); United States: 2020. 2019-nCoV: What the Public Should Do. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); United State: 2020. 2019 Novel Coronavirus (2019-nCoV) [Google Scholar]
- CDC . Centers for Disease Control and Prevention(CDC); United States: 2020. Coronavirus Disease 2019 (COVID-19)—Transmission. [Google Scholar]
- CDC . Centers for Disease Control and Prevention; United States: 2020. Coronavirus Disease 2019 (COVID-19) Symptoms. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); United States: 2020. Coronavirus Disease 2019 (COVID-19): Situation Summary. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); United States: 2020. Coronavirus Disease 2019 Information for Travel. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); United States: 2020. COVID-19 Travel Precautions. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); U.S: 2020. How COVID-19 Spreads. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); United States: 2020. Prevention & Treatment. (Accessed 15 February 2020) [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); U.S: 2020. Real-Time RT-PCR Panel for Detection 2019-Novel Coronavirus. [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); U.S: 2020. Symptoms of Novel Coronavirus (2019-nCoV) [Google Scholar]
- CDC . Centers for Disease Control and Prevention; United States: 2020. Using an Epi Curve to Determine Most Likely Period of Exposure (Quick Learn Lessons) [Google Scholar]
- CDC . Centers for Disease Control and Prevention (CDC); United States: 2020. What to Do if you Are Sick with COVID-19. [Google Scholar]
- CGTN . CGTN; 2020. 27 Cases of Viral Pneumonia Reported in Central China’s Wuhan City. [Google Scholar]
- Chan J.F.-W., Yuan S., Kok K.-H., To K.K.-W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Yang J., Yang W., Wang C., Bärnighausen T. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395:764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Z.J., Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020;48:155–163. doi: 10.1007/s15010-020-01401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung J.C.-H., Ho L.T., Cheng J.V., Cham E.Y.K., Lam K.N. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ClinicalTrials . US National Library of Medicine; 2019. A Clinical Trial to Determine the Safety and Immunogenicity of Healthy Candidate MERS-CoV Vaccine (MERS002) [Google Scholar]
- Daoud E. Western Australian man becomes first person in Australia to die from coronavirus. 7news. 2020 (Accessed 1 March 2020) [Google Scholar]
- De Groot R.J., Baker S.C., Baric R.S., Brown C.S., Drosten C., Enjuanes L. Middle East respiratory syndrome coronavirus (MERS-CoV): announcement of the Coronavirus Study Group. J. Virol. 2013;87:7790–7792. doi: 10.1128/JVI.01244-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deerwester J., Gilbertson D. USA Today; 2020. Coronavirus: US Says ‘Do Not Travel’ to Wuhan, China, as Airlines Issue Waivers, Add Safeguards. [Google Scholar]
- Egypt Egypt announces first Coronavirus infection. Egypt Today. 2020 [Google Scholar]
- Eng J.W.L., Reed C.B., Kokolus K.M., Pitoniak R., Utley A., Bucsek M.J. Housing temperature-induced stress drives therapeutic resistance in murine tumour models through β2-adrenergic receptor activation. Nat. Commun. 2015;6:6426. doi: 10.1038/ncomms7426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foxman E.F., Storer J.A., Fitzgerald M.E., Wasik B.R., Hou L., Zhao H. Temperature-dependent innate defense against the common cold virus limits viral replication at warm temperature in mouse airway cells. Proc. Natl. Acad. Sci. U. S. A. 2015;112:827–832. doi: 10.1073/pnas.1411030112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foxman E.F., Storer J.A., Vanaja K., Levchenko A., Iwasaki A. Two interferon-independent double-stranded RNA-induced host defense strategies suppress the common cold virus at warm temperature. Proc. Natl. Acad. Sci. U. S. A. 2016;113:8496–8501. doi: 10.1073/pnas.1601942113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman W.M., Walker S.J., Vrana K.E. Quantitative RT-PCR: pitfalls and potential. BioTechniques. 1999;26:112–125. doi: 10.2144/99261rv01. [DOI] [PubMed] [Google Scholar]
- Gonçalves-Sá J. In the fight against the new coronavirus outbreak, we must also struggle with human bias. Nat. Med. 2020;26:305. doi: 10.1038/s41591-020-0802-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A. bioRxiv; 2020. Severe Acute Respiratory Syndrome-Related Coronavirus: The Species and Its Viruses – A Statement of the Coronavirus Study Group. 2020.02.07.937862. [DOI] [Google Scholar]
- Grenfell R.D.T. Science Alert; 2020. Here’s Why It’s Taking So Long to Develop a Vaccine for the New Coronavirus. [Google Scholar]
- Hogan C.M. Respiration. In: McGinley Mark, Cleveland C.J., editors. Encyclopedia of Earth. National council for Science and the Environment; Washington, D.C: 2011. [Google Scholar]
- Hogue Brenda G., Machamer C.E. 2008. Chapter 12: Coronavirus Structural Proteins and Virus Assembly. Nidoviruses. [DOI] [Google Scholar]
- Holshue M.L.D.C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 Novel Coronavirus in the United States. N. Engl. J. Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins C. 2020. Loss of Sense of Smell as Marker of COVID-19 Infection, Ear, Nose and Throat Surgery Body of United Kingdom. [Google Scholar]
- Horowitz J. 2020. Italy Announces Restrictions Over Entire Country in Attempt to Halt Coronavirus. [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang R., Xia J., Chen Y., Shan C., Wu C. A family cluster of SARS-CoV-2 infection involving 11 patients in Nanjing, China. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30147-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z., Zhao S., Li Z., Chen W., Zhao L., Deng L. The Battle against coronavirus disease 2019 (COVID-19): emergency management and infection control in a radiology department. J. Am. Coll. Radio. 2020 doi: 10.1016/j.jacr.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui D.S., Azhar E.I., Madani T.A., Ntoumi F., Kock R., Dar O. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—the latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacobucci G. Sixty seconds on … anosmia. BMJ. 2020;368 doi: 10.1136/bmj.m1202. [DOI] [PubMed] [Google Scholar]
- ILO . International Labour Organization; 2020. Almost 25 Million Jobs Could Be Lost Worldwide as a Result of COVID-19, Says ILO: COVID-19: Protecting Workers in the Workplace (Press Release) [Google Scholar]
- IPH . Institut Za Javno Zdravlje Crne Gore: Acts of the Institute of Public Health of Montenegro; 2020. Situation in Montenegro on Tuesday. [Google Scholar]
- Ithete N.L., Stoffberg S., Corman V.M., Cottontail V.M., Richards L.R., Schoeman M.C. Close relative of human Middle East respiratory syndrome coronavirus in bat, South Africa. Emerging Infect. Dis. 2013;19:1697–1699. doi: 10.3201/eid1910.130946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- J F . EMCrit; USA: 2020. COVID-19—The Internet Book of Critical Care (Digital) (Reference Manual) [Google Scholar]
- J. A Australian lab cultures new coronavirus as infections climb. The Scientist. 2020 [Google Scholar]
- Jansson M., Liao X., Rello J. Strengthening ICU health security for a coronavirus epidemic. Intens. Crit. Care Nur. 2020;57 doi: 10.1016/j.iccn.2020.102812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennifer C.H., Duc T.N., Bashir A., Zyad Al B., Wafa Al D., Kheir Abu E. Transmission of Middle East respiratory syndrome coronavirus infections in healthcare settings, Abu Dhabi. Emerging Infect. Dis. 2016;22:647. doi: 10.3201/eid2204.151615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JHU . Center for Systems Science and Engineering (CSSE), Johns Hopkins University (JHU); 2020. Coronavirus COVID-19 Global Cases. [Google Scholar]
- Jiaye L., Xuejiao L., Shen Q., Jing Y., Fuxiang W., Yingxia L. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerging Infect. Dis. 2020;26 doi: 10.3201/eid2606.200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y., Yang H., Ji W., Wu W., Chen S., Zhang W. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12:372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph A. Boston Globe Media; StatNews: 2020. Woman with Novel Pneumonia Virus Hospitalized in Thailand — The First Case Outside China. [Google Scholar]
- Kang C.K., Song K.-H., Choe P.G., Park W.B., Bang J.H., Kim E.S. Clinical and epidemiologic characteristics of spreaders of Middle East respiratory syndrome coronavirus during the 2015 outbreak in Korea. J. Korean Med. Sci. 2017;32:744–749. doi: 10.3346/jkms.2017.32.5.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokolus K.M., Capitano M.L., Lee C.-T., Eng J.W.L., Waight J.D., Hylander B.L. Baseline tumor growth and immune control in laboratory mice are significantly influenced by subthermoneutral housing temperature. Proc. Natl. Acad. Sci. U. S. A. 2013;110:20176–20181. doi: 10.1073/pnas.1304291110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koonin E.V., Senkevich T.G., Dolja V.V. The ancient virus world and evolution of cells. Biol. Direct. 2006;1:29. doi: 10.1186/1745-6150-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KoreaCDC Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong. Public Health Res. Perspect. 2015;6:269–278. doi: 10.1016/j.phrp.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo E., Song E., Yockey L., Rakib T., Wong P., Homer R. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc. Natl. Acad. Sci. U. S. A. 2019;116 doi: 10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiken T., Fouchier R.A.M., Schutten M., Rimmelzwaan G.F., van Amerongen G., van Riel D. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet. 2003;362:263–270. doi: 10.1016/S0140-6736(03)13967-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai M.M.C., Cavanagh D. The Molecular Biology of Coronaviruses. In: Maramorosch K., Murphy F.A., Shatkin A.J., editors. Advances in Virus Research. Vol. 48. Academic Press; 1997. pp. 1–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.-C., Liu Y.H., Wang C.-Y., Wang Y.-H., Hsueh S.-C., Yen M.-Y. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. J. Microbiol., Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.-C., Shih T.-P., Ko W.-C., Tang H.-J., Hsueh P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau S.K.P., Woo P.C.Y., Yip C.C.Y., Tse H., H-w Tsoi, Cheng V.C.C. Coronavirus HKU1 and other coronavirus infections in Hong Kong. J. Clin. Microbiol. 2006;44:2063–2071. doi: 10.1128/JCM.02614-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R. The incubation period of Coronavirus Disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee B.Y., Shah M. Prevention of influenza in healthy children. Expert Rev. Anti-Infect. Ther. 2012;10:1139–1152. doi: 10.1586/eri.12.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh N.D., Kokolus K.M., O’Neill R.E., Du W., Eng J.W.L., Qiu J. Housing temperature-induced stress is suppressing murine graft-versus-host disease through β2-adrenergic receptor signaling. J. Immunol. 2015;195:5045–5054. doi: 10.4049/jimmunol.1500700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester W., Jr. The influence of relative humidity on the infectivity of air-borne influenza A virus, PR8 strain. J. Exp. Med. 1948;88:361–368. doi: 10.1084/jem.88.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letko M., Marzi A., Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat. Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Shi Z., Yu M., Ren W., Smith C., Epstein J.H. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310:676. doi: 10.1126/science.1118391. [DOI] [PubMed] [Google Scholar]
- Lim Y.X., Ng Y.L., Tam J.P., Liu D.X. Human coronaviruses: a review of virus-host interactions. Diseases. 2016;4:26. doi: 10.3390/diseases4030026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Fang Y.-Y., Deng Y., Liu W., Wang M.-F., Ma J.-P. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. 2020 doi: 10.1097/CM9.0000000000000744. (Publish Ahead of Print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardi A., Bozzi G., Mangioni D., Muscatello A., Peri A.M., Taramasso L. Duration of quarantine in hospitalized patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a question needing an answer. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A., Palese P. Transmission of influenza virus in temperate zones is predominantly by aerosol, in the tropics by contact: a hypothesis. PLoS Curr. 2009;1:RRN1002. doi: 10.1371/currents.rrn1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A.C., Mubareka S., Steel J., Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo W., Majumder M.S., Liu D., Poirier C., Mandl K.D., Lipsitch M. medRxiv; 2020. The Role of Absolute Humidity on Transmission Rates of the COVID-19 Outbreak. 2020.02.12.20022467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupia T., Scabini S., Mornese Pinna S., Di Perri G., De Rosa F.G., Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J. Global Antimicrob. Resist. 2020;21:22–27. doi: 10.1016/j.jgar.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- M. A Safety, tolerability and immunogenicity of vaccine candidate MVA-MERS-S. ClinicalTrials. 2019 [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclean R. Africa braces for coronavirus, but slowly. The New York Times. 2020 [Google Scholar]
- Mahy B.W.J. Coronavirus come of age. Nature. 1980;288:536–537. doi: 10.1038/288536a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh S. The Guardian; 2020. Four Cruise Ship Passengers Test Positive in UK—As it Happened. [Google Scholar]
- Martinez-Alvarez M., Jarde A., Usuf E., Brotherton H., Bittaye M., Samateh A.L. COVID-19 pandemic in West Africa. Lancet Glob. Health. 2020 doi: 10.1016/S2214-109X(20)30123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters P.S. Advances in Virus Research. Vol. 66. Academic Press; 2006. The molecular biology of coronaviruses; pp. 193–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxmen A. How poorer countries are scrambling to prevent a coronavirus disaster. Nature, News. 2020 doi: 10.1038/d41586-020-00983-9. [DOI] [PubMed] [Google Scholar]
- May R.M., McLean A.R., Pattison J., Weiss R.A., Anderson R.M., Fraser C. Epidemiology, transmission dynamics and control of SARS: the 2002–2003 epidemic. Philos. Trans. R. Soc. B. 2004;359:1091–1105. doi: 10.1098/rstb.2004.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreary E.K., Pogue J.M., on behalf of the Society of Infectious Diseases P COVID-19 treatment: a review of early and emerging options. Open Forum Infect. Dis. 2020 doi: 10.1093/ofid/ofaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay B., Calfas J., T A. 2020. Coronavirus Declared Pandemic by World Health Organization. [Google Scholar]
- McNeil J., Donald G. The U.S. now leads the world in confirmed coronavirus cases - following a series of missteps, the nation is now the epicenter of the pandemic. The New York Times. 2020 [Google Scholar]
- Mesel-Lemoine M., Millet J., Vidalain P.-O., Law H., Vabret A., Lorin V. A human coronavirus responsible for the common cold massively kills dendritic cells but not monocytes. J. Virol. 2012;86:7577–7587. doi: 10.1128/JVI.00269-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu. Rev. Virol. 2020 doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- MT H. Elsevier Connect; 2020. Novel Coronavirus Information Center: Expert Guidance and Commentary. [Google Scholar]
- Nature Virology: coronaviruses. Nature. 1968;220:650. doi: 10.1038/220650b0. [DOI] [Google Scholar]
- Nature Coping with COVID-19. Nat. Geosci. 2020;13:257. [Google Scholar]
- Nature Coronavirus latest: confirmed cases cross the one-million mark. Nature (News) 2020 [Google Scholar]
- NCPERE T Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) – China. China CDC Weekly. 2020;2:113–122. [PMC free article] [PubMed] [Google Scholar]
- NewWorkTimes It may be time for everyone to mask up, Corona virus briefing. The New Work Times. 2020 [Google Scholar]
- NewYorkTimes Coronavirus live updates: Europe prepares for pandemic as illness spreads from Italy. The New York Times. 2020 [Google Scholar]
- NIAID . United States National Institute of Allergy and Infectious Diseases (NIAID), Wayback Machine; 2016. NIAID Biodefense Research Agenda for Category B and C Priority Pathogens: “Vaccines Are the most Effective Method of Protecting the Public against Infectious Diseases.”. [Google Scholar]
- NIAID . National Institute of Allergy and Infectious Diseases (NIAID), New releases, U.S. Department of Health & Human Services; 2020. NIH Clinical Trial of Investigational Vaccine for COVID-19 Begins. [Google Scholar]
- Nikel D. Denmark closes border to all international tourists for one month. Forbes. 2020 [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA, J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orenstein W.A., Bernier R.H., Dondero T.J., Hinman A.R., Marks J.S., Bart K.J. Field evaluation of vaccine efficacy. Bull. World Health Organ. 1985;63:1055–1068. [PMC free article] [PubMed] [Google Scholar]
- P J., AW S., T C. Reuters; 2020. Coronavirus: Poland to Close Borders to Foreigners, Quarantine Returnees. [Google Scholar]
- Palus S. The key stat in the NYTimes’ piece about losing your sense of smell was wrong. Slate Magazine. 2020 [Google Scholar]
- Peiris J.S.M., Lai S.T., Poon L.L.M., Guan Y., Yam L.Y.C., Lim W. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennsylvania . Penn Libraries; 2020. COVID19—Resources for Health Care Professionals. [Google Scholar]
- Perlman S. Another decade, another coronavirus. N. Engl. J. Med. 2020;382:760–762. doi: 10.1056/NEJMe2001126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qing E., Gallagher T. SARS coronavirus redux. Trends Immunol. 2020;41:271–273. doi: 10.1016/j.it.2020.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualls Noreen, Levitt Alexandra, Kanade Neha, Wright-Jegede Narue, Dopson Stephanie, Biggerstaff Matthew. Community mitigation guidelines to prevent pandemic influenza — United States, 2017. Morb. Mortal. Wkly Rep. 2017;66:1–34. doi: 10.15585/mmwr.rr6601a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman J.M., Das B., Sindberg G.M., Urban M.D., Hammerlund M.E.M., Lee H.B. Humidity as a non-pharmaceutical intervention for influenza A. PLoS One. 2018;13 doi: 10.1371/journal.pone.0204337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuters . 2020. Algeria Confirms Two more Coronavirus Cases. [Google Scholar]
- Reuters . 2020. Ecuador Confirms Five New Cases of Coronavirus, all Close to Initial Patient. [Google Scholar]
- Rodríguez-Morales A.J., MacGregor K., Kanagarajah S., Patel D., Schlagenhauf P. Going global – travel and the 2019 novel coronavirus. Trav. Med. Infect. Dis. 2020;33 doi: 10.1016/j.tmaid.2020.101578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rondanelli M., Miccono A., Lamburghini S., Avanzato I., Riva A., Allegrini P. Self-care for common colds: the pivotal role of vitamin D, vitamin C, zinc, and Echinacea in three main immune interactive clusters (physical barriers, innate and adaptive immunity) involved during an episode of common colds-practical advice on dosages and on the time to take these nutrients/botanicals in order to prevent or treat common colds. Evid. Based Complement. Alternat. Med. 2018;2018:5813095. doi: 10.1155/2018/5813095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roser Max, Ritchie H., Ortiz-Ospina E. Ourworldindata; 2020. Coronavirus Disease (COVID-19) – Statistics and Research. [Google Scholar]
- Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- S K. Coronavirus: Singapore reports first cases of local transmission; 4 out of 6 new cases did not travel to China. The Straits Times. 2020 [Google Scholar]
- Sah R., Rodriguez-Morales A.J., Jha R., Chu D.K.W., Gu H., Peiris M. Complete genome sequence of a 2019 novel coronavirus (SARS-CoV-2) strain isolated in Nepal. Microbiol. Resour. Announc. 2020;9 doi: 10.1128/MRA.00169-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. Am. J. Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- Sattenspiel L., Herring D.A. Simulating the effect of quarantine on the spread of the 1918–19 flu in Central Canada. Bull. Math. Biol. 2003;65:1–26. doi: 10.1006/bulm.2002.0317. [DOI] [PubMed] [Google Scholar]
- Schoeman D., Fielding B.C. Coronavirus envelope protein: current knowledge. Virol. J. 2019;16:69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulman J.L., Kilbourne E.D. Airborne transmission of influenza virus infection in mice. Nature. 1962;195:1129–1130. doi: 10.1038/1951129a0. [DOI] [PubMed] [Google Scholar]
- Shao P. medRxiv; 2020. Impact of City and Residential Unit Lockdowns on Prevention and Control of COVID-19. 2020.03.13.20035253. [DOI] [Google Scholar]
- Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song P., Karako T. COVID-19: real-time dissemination of scientific information to fight a public health emergency of international concern. Bio Sci. Trends. 2020;14:1–2. doi: 10.5582/bst.2020.01056. [DOI] [PubMed] [Google Scholar]
- Spinney L. Coronavirus vaccine: when will it be ready? The Guardian. 2020 [Google Scholar]
- Stoye E. China coronavirus: how many papers have been published. Nature, news. 2020 doi: 10.1038/d41586-020-00253-8. [DOI] [PubMed] [Google Scholar]
- Thiel V. 1st ed. Caister Academic Press; 2007. Coronaviruses: Molecular and Cellular Biology. [Google Scholar]
- Twitter Two COVID-19 cases confirmed in Montenegro. twitter.com/MeGovernment. 2020 [Google Scholar]
- Tyrrell D.A.J., Bynoe M.L. Cultivation of viruses from a high proportion of patients with colds. Lancet. 1966;287:76–77. doi: 10.1016/S0140-6736(66)92364-6. [DOI] [PubMed] [Google Scholar]
- UNDP . United Nations Development Programme; 2020. COVID-19 Pandemic: Humanity Needs Leadership and Solidarity to Defeat the Coronavirus: UNDP Response. [Google Scholar]
- UNDP . United Nations Development Programme; New York, NY 10017 USA: 2020. Statement by UNDP Administrator Achim Steiner on UN COVID-19 Global Humanitarian Response Plan. [Google Scholar]
- Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellingiri B., Jayaramayya K., Iyer M., Narayanasamy A., Govindasamy V., Giridharan B. COVID-19: a promising cure for the global panic. Sci. Total Environ. 2020;725:138277. doi: 10.1016/j.scitotenv.2020.138277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T., Du Z., Zhu F., Cao Z., An Y., Gao Y. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020;395:e52. doi: 10.1016/S0140-6736(20)30558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren-Gash C., Fragaszy E., Hayward A.C. Hand hygiene to reduce community transmission of influenza and acute respiratory tract infection: a systematic review. Influenza Other Respir. Viruses. 2013;7:738–749. doi: 10.1111/irv.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wee S.L., McNeil D.G., Jr., JC H. W.H.O. declares global emergency as Wuhan coronavirus spreads. The New York Times. 2020 [Google Scholar]
- Wei M., Yuan J., Liu Y., Fu T., Yu X., Zhang Z.-J. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA, J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei W.E., L Z., Chiew C.J., Yong S.E., Toh M.P., Lee V.J. Presymptomatic transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. Morb. Mortal. Wkly Rep. 2020 doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss S.R., Navas-Martin S. Coronavirus pathogenesis and the emerging pathogen severe acute respiratory syndrome coronavirus. Microbiol. Mol. Biol. Rev. 2005;69:635–664. doi: 10.1128/MMBR.69.4.635-664.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, 1948. World Health Organization.
- WHO . World Health Organization (WHO); 2003. Severe Acute Respiratory Syndrome (SARS) – Multi-Country Outbreak – Update 6. [Google Scholar]
- WHO . World Health Organization (WHO); 2004. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003. [Google Scholar]
- WHO . World Health Organization (WHO); 2013. Middle East Respiratory Syndrome Coronavirus (MERSCoV) [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Clinical Management of Severe Acute Respiratory Infection when Novel Coronavirus (nCoV) Infection Is Suspected: Interim Guidance. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Coronavirus Disease 2019 (COVID-19): Situation Report – 53. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Coronavirus Disease (COVID-2019) Situation Report-73. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Coronavirus Disease (COVID-2019) Situation Reports. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Falsified Medical Products, Including In Vitro Diagnostics, that Claim to Prevent, Detect, Treat or Cure COVID-19: Rolling Updates on Coronavirus Disease (COVID-19) [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Interim Guidance: Clinical Management of Severe Acute Respiratory Infection when COVID-19 Is Suspected. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Laboratory Testing for Coronavirus Disease (COVID-19) in Suspected Human Cases: Interim Guidance. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Munich Security Conference. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Naming the Coronavirus Disease (COVID-19) and the Virus that Causes it. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Novel Coronavirus– Japan (ex-China) [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Novel Coronavirus (2019-nCoV): Situation Report- 22. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Novel Coronavirus (2019-nCoV): Situation Report - 3. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Novel Coronavirus (2019-nCoV): Situation Report - 5. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Novel Coronavirus (2019-nCoV): Situation Report - 8. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Novel Coronavirus (2019-nCoV): Situation Report - 10. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Off-Label Use of Medicines for COVID-19. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Q&a on Coronaviruses. [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) [Google Scholar]
- WHO . World Health Organization (WHO); 2020. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV) (Press release) [Google Scholar]
- WHO . World Health Organization (WHO); 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. (Press release) [Google Scholar]
- Wikipedia . 2020. Contact Tracing. [Google Scholar]
- Wikipedia . 2020. Incubation period. [Google Scholar]
- Wikipedia . 2020. Vaccine. [Google Scholar]
- Wikipedia . 2020. Virus. [Google Scholar]
- Williams R., Rankin N., Smith T., Galler D., Seakins P. Relationship between the humidity and temperature of inspired gas and the function of the airway mucosa. Crit. Care Med. 1996;24 doi: 10.1097/00003246-199611000-00025. [DOI] [PubMed] [Google Scholar]
- Woo P.C.Y., Lau S.K.P., Li K.S.M., Poon R.W.S., Wong B.H.L., H-w Tsoi. Molecular diversity of coronaviruses in bats. Virology. 2006;351:180–187. doi: 10.1016/j.virol.2006.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo P.C.Y., Lau S.K.P., Lam C.S.F., Lau C.C.Y., Tsang A.K.L., Lau J.H.N. Discovery of seven novel mammalian and avian coronaviruses in the genus deltacoronavirus supports bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavirus. J. Virol. 2012;86:3995–4008. doi: 10.1128/JVI.06540-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WorldBank . The World Bank; 2020. World Bank Group Announces up to $12 Billion Immediate Support for COVID-19 Country Response (Press Release) [Google Scholar]
- Worldometer . 2020. Coronavirus (COVID-19) Mortality Rate. [Google Scholar]
- Worldometer . 2020. COVID-19 coronavirus pandemic. [Google Scholar]
- Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27:325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia W., Shao J., Guo Y., Peng X., Li Z., Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr. Pulm. 2020 doi: 10.1002/ppul.24718. (n/a) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao S.-Y., Wu Y., Liu H. Evolving status of the 2019 novel coronavirus infection: proposal of conventional serologic assays for disease diagnosis and infection monitoring. J. Med. Virol. 2020;92:464–467. doi: 10.1002/jmv.25702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Zhong L., Deng J., Peng J., Dan H., Zeng X. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci. 2020;12:8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang P., Wang X. COVID-19: a new challenge for human beings. Cell. Mol. Immunol. 2020 doi: 10.1038/s41423-020-0407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Elankumaran S., Marr L.C. Relationship between humidity and influenza A viability in droplets and implications for influenza’s seasonality. PLoS One. 2012;7 doi: 10.1371/journal.pone.0046789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yellon S.M., Fagoaga O.R., Nehlsen-Cannarella S.L. Influence of photoperiod on immune cell functions in the male Siberian hamster. Am. J. Phys. 1999;276:R97–R102. doi: 10.1152/ajpregu.1999.276.1.R97. [DOI] [PubMed] [Google Scholar]
- Yin Y., Wunderink R.G. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology. 2018;23:130–137. doi: 10.1111/resp.13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu P., Zhu J., Zhang Z., Han Y. A familial cluster of infection associated with the 2019 Novel coronavirus indicating possible person-to-person transmission during the incubation period. J. Infect. Dis. 2020 doi: 10.1093/infdis/jiaa077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhen-Dong T., An T., Ke-Feng L., Peng L., Hong-Ling W., Jing-Ping Y. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerging Infect. Dis. 2020;26 doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y.-Y., Ma Y.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020 doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou V. Coronavirus: Shanghai neighbour Zhejiang imposes draconian quarantine. South China Morning Post. 2020 [Google Scholar]
- Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W. Discovery of a novel coronavirus associated with the recent pneumonia outbreak in humans and its potential bat origin. bioRxiv. 2020 doi: 10.1101/2020.01.22.914952. 2020.01.22.914952. [DOI] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]