Coronavirus disease 2019 (COVID-19) is currently causing devastating impacts globally. As of March 31, 2020, a total of 857,165 COVID-19 cases have been confirmed around the world, and more than 42,100 people have died. The death rate is estimated at 5%, with older adults making up the vast majority of cases (>80%).
To address this situation and protect their populations, most countries have declared a state of emergency, and enforce or recommend physical distancing (of about 2 m), as well as voluntary quarantine. Strict guidelines for room or apartment confinement, including no unessential social or physical interaction, have been implemented for older adults, especially those who are frail and live in congregate apartments, assisted living settings, and long-term care, and those who are hospitalized. A poignant—but not unusual—example of this was an older couple on a cruise ship with a COVID-19 outbreak on board, who, on national television, talked about their experience being confined to a 200-square-foot cabin for more than a week.
Not surprisingly, studies show a decline in the number of pedometer steps taken per week by adults owing to restrictions put in place to mitigate COVID-19. European countries showed the most dramatic decline, ranging from a 7% to 38% reduction in steps between March 15 and 22, 2020.1 Hence, it is also important to keep in mind that inactivity is the fourth-leading cause of mortality according to the World Health Organization.2
Maintaining functional ability and coping with functional limitations for as long as possible are key health care challenges for independent living in institutionalized and hospitalized older adults. Thus, although COVID-19 restrictions aim to protect older adults, such social and physical distancing is also likely to negatively impact the physical and mental health of older adults.
Furthermore, long-term care residents are characterized by high prevalence of multimorbidity, prescription drug use, and dependency in activities of daily living. Hospitalization of older adults is also problematic as it leads to functional decline, also known as iatrogenic decline.3 In a 10-day hospitalization, an older patient typically loses 16% of muscle strength and 6% of muscle mass.4 Moreover, seniors recently discharged from hospital are at a particularly high risk of falls (34% within 3 months of discharge)5 , 6 and disability (33% will report functional decline 1 year after discharge).7 , 8 The vicious circle of frailty is accelerated by physical inactivity and further increases the need for health care services.
The negative consequences of hospitalization or living in long-term care are largely due to low physical activity. Older hospitalized patients are often confined to bed for 17 hours a day (not including sleep time)9 , 10 even if they are able to walk independently. Long-term care residents spend 90% of their time in sedentary positions (ie, sitting or lying) and rarely or never go outdoors, which further exacerbates their frailty and reduces cardiopulmonary reserve.11 , 12 Moreover, significant impact and stress on the health care system can be expected when older adults lose functional capacities, in addition to decreased quality of life and long life expectancy.
Overall, health care professionals are very concerned about the impacts of physical distancing on older adults, including multiple negative physical and mental health effects, in addition to loneliness and isolation. It is important that geriatric values are balanced with population safety when implementing actions to mitigate COVID-19 transmission. Furthermore, cardiopulmonary reserve (especially pulmonary reserve) is a key determinant of one's ability to survive COVID-19.
According to the World Health Organization, healthy aging is largely determined by the ability to maintain both mental and physical capacities.13 No medications currently exist that help maintain physical capacity, nor will any be commercialized in the foreseeable future. However, physical capacity can be maintained through physical stimulus via adapted physical activity. It is well known that physical activity is key for the health and well-being of people older than 85 years.14
Physical activity has been shown to protect against the incidence of activities of daily living disability, but also disability progression or severity.15 A meta-analysis of hospitalized older adults concluded that only supervised physical interventions, including those in continuous adaptation to the patient's capabilities, showed positive results on the patient's physical performance.16 Nevertheless, the solution to this problem requires pragmatism and an ecologic approach, as health care resources are limited and made available on a priority basis. In addition, this solution must also respect the COVID-19 guidelines.
Innovative approaches using gerontechnology, such as exergames, are nowadays recognized to contribute to improving walking capacity in older adults.17 More specifically, previous research showed that Jintronix, an interactive exergames program, is feasible to apply, acceptable to all stakeholders, and improves functional capacities, including walking speed, in older adults in long-term care or posthospitalization.18 Interestingly, Barbosa Neves et al observed that the use of technology also increased the perceived social interaction with family and friends for participants with geographically distant relatives.19 Thus, technology can be used to avoid physical decline as well as decrease isolation and loneliness. Overall, exergames using (1) video consoles (eg, Wii, Wii-Fit, Xbox, or PlayStation fitness games), (2) interactive rehabilitation technologies (eg, Jintronix software), (3) tablet or smartphone (eg, Vivifrail application), (4) wearable sensor based (eg, FallSensing Exergames: OTAGO), or (4) virtual reality devices (eg, Box, Rendever, Sea Hero Quest using Oculus Go, HTC Vive; Samsung Gear)) should be brought forward to alleviate some of the challenges caused by COVID-19 restrictions, namely, physical distancing and isolation. Nevertheless, many components of this technology (Internet or materials or license access) are not yet available at hospitals or long-term care facilities. Thus, other solutions need to be found.
DVD-delivered physical activity intervention (eg, FlextoBa, OTAGO) is another efficient method to improve physical performance (flexibility and strength) or functional capacities (via, eg, the Short Physical Performance Battery [SPPB]; balance) in older adults because this technology can be used unsupervised and without individual Internet access. For example, Wójcicki et al20 concluded that physical activity programs using DVDs (ie, no need for Internet), specifically designed to target functional fitness in sedentary older adults, can produce clinically meaningful gains in physical function that are maintained beyond intervention cessation. Nevertheless, this method requires individual DVD disc and DVD reader on location. In addition, those scientifically validated have not all been adapted for the frail population, such as older adults living in long-term care or those hospitalized.
Recently, Ortiz-Alonso et al21 showed that simple supervised exercises (walking and rising from a chair for ∼20 minutes/d) decreased hospitalization-associated disability in very old hospitalized patients. However, even if this study demonstrated that simple exercises can improve functional capacities, this intervention has been done with supervision and cannot be replicated during COVID-19.
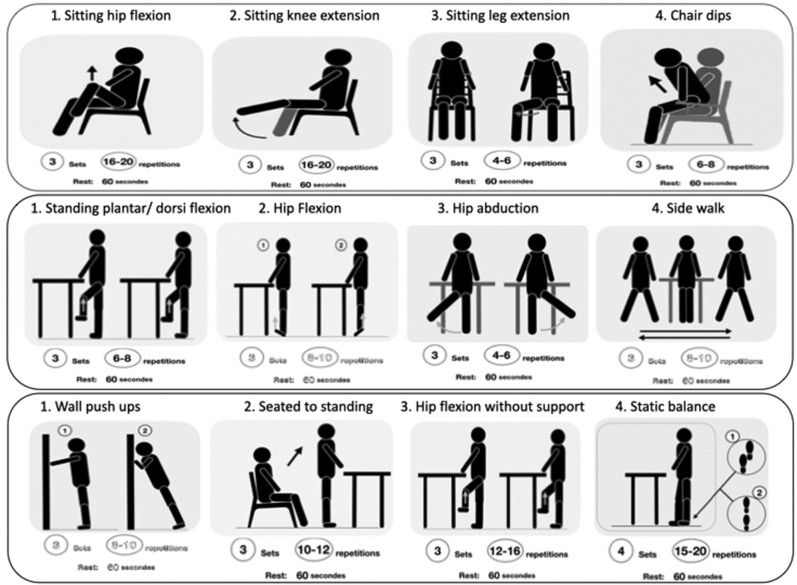
Thus, to counteract physical and functional declines during COVID-19, safe, efficient, and simple exercises that can be performed unsupervised are needed. We showed that specific physical activity programs adapted for home-based unsupervised use are efficient and safe (no fall reported) to improve functional capacity in older adults posthospitalization22 (Figure 1 ). But compared with previous studies, the novelty that facilitates its implementation is that the 27 specific programs are prescribed based on a pragmatic decisional tree.22
Fig. 1.
Example of 3 unsupervised PATH programs according to an individual's balance and strength profile.22 Each panel represents a different program; The figure represents reminder sheets that are designed to be placed on the patient's wall or refrigerator.
In addition, a pilot study tested unsupervised simple exercises in hospitalized older adults and demonstrated that it was not only feasible and acceptable23 but also an efficient way to improve a patient's functional capacity and physical activity practice (length of stay and discharge orientation).24
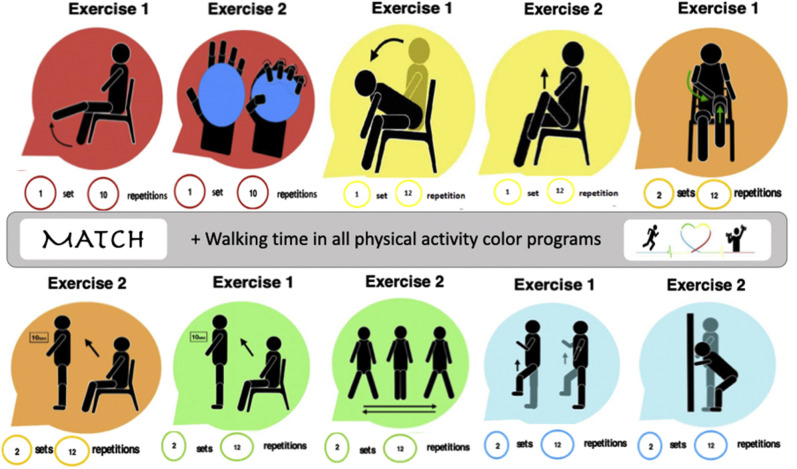
This simple physical activity program has been recently improved and can be easily and automatically prescribed using a pragmatic decisional tree (adapted from Carvalho et al22),24 and by adjusting simple unsupervised adapted physical activity programs (5 color levels) according to patient and clinician feedbacks.24 This new physical activity program (MATCH: Maintenance of Autonomy Through exercise Care during Hospitalization), available for notebook with optional and additional training video, has already been tested and implemented during this COVID-19 pandemic in geriatric hospital units and long-term care with no individual Internet access.
Regarding this program, the health care teams first need to complete the decisional tree. This decisional tree includes 3 simple tests: (1) 30-second chair test (numbers and used of arms), (2) SPPB balance (side by side and semitandem) tests (yes or no), and (3) SPPB 4-m walking speed.22 , 24 These 3 tests have been chosen because they are already implemented in geriatric practice, easy to perform (space and time), and do not require any specific materials. The score obtained using the first 2 tests prescribes the adapted and specific color of the physical activity program.22 , 24 The third test (walking speed) determined the walking time because the corridors and the common or free spaces are quite distinct in each structure.24
Each physical activity color program included 2 specific and adapted exercises (eg, seated knee extension, sit to stand, step aside, chair forward bend, bipedal and unipedal static balance, and wall squat) and walking time (Figure 1). All programs have been created to improve or at least maintain balance, strength, and also mobility and cardiopulmonary function (aerobic capacities). All programs are realized unsupervised, without materials (except room equipment: chair or wall), between 2 and 3 times per day, in a seated or standing position.
Thus, depending on the hospital and long-term care resources, a huge number of simple and adapted physical activity programs without specific materials and using notebook, TV screen, video, or Internet live video can be implemented to avoid bed rest and immobilization effects during the COVID-19 pandemic (eg, SPRINT; MATCH Vivifrail; LaterLifeTraining; Go4Life, and MOVE; see Table 1 ).
Table 1.
Examples of Physical Activity Resources Available and Specific to Older Adults to Avoid COVID-19 Restrictions
| Name | Details and Source URL | Type of Resource |
|---|---|---|
| Specific, simple, and adapted program for older adults | ||
| Otago | https://www.livestronger.org.nz/assets/Uploads/acc1162-otago-exercise-manual.pdf | Notebook, DVD |
| Vivifrail | http://vivifrail.com | Notebook, applications |
| SPRINT/MATCH/PATH | https://physioimpact.files.wordpress.com/2013/12/protocole-sprint-decc81cembre-2013.pdf | Notebook, website video |
| General physical activity program for older adults | ||
| LaterLifeTraining | https://www.laterlifetraining.co.uk | Notebook Facebook Live daily classes |
| Go4Life | https://go4life.nia.nih.gov | Free video |
| MovesCanada | https://www.movescanada.ca/ | Notebook, website video |
| Active Aging Canada | https://www.youtube.com/c/ActiveAgingCanada | Notebook, website video |
| Active Ageing Australia | https://activeageing.org.au | Notebook, website video |
| Move50+ | https://move50plus.ca/bougez/#tout | Notebook, website video |
Such approaches also have the advantage of being in compliance with the currently imposed physical and social distancing. Finally, as COVID-19 restrictions vary by country for older adults, research and data collection must be encouraged around the world. A collective effort could help to monitor the changes in physical function and to determine which physical activity practice more effectively limits the number of deaths as well as iatrogenic decline during the COVID-19 pandemic. Such efforts could help provide clear public health recommendations to better prepare the health care system in the event of a future pandemic.
In conclusion, to our knowledge, these simple, adapted, specific daily physical activities that include strength, balance, and walk exercises (eg, Vivifrail; see Figures 1 and 2 ) can be considered as the best solution to care for frail older adults during the COVID-19 pandemic.
Fig. 2.
The MATCH color programs. These 5 unsupervised, simple, but specific exercise programs are prescribed based on a patient's decisional tree score. The figure represents a combination of the reminder graphics for the red (lowest level), yellow, orange, green, and blue (highest level) programs. Each color graphic is designed to be fixed on the head of the patient's bed.
Footnotes
M.A.-L. is supported by the Fonds de Recherche du Québec - Santé (FRQS).
The authors declare no conflicts of interest.
References
- 1.FitBit staff The impact of coronavirus on physical activity all over the world. https://blog.fitbit.com/covid-19-global-activity Available at:
- 2.World Health Organization . WHO; Geneva: 2010. Global Recommendations on Physical Activity for Health. chap. 2.1. [PubMed] [Google Scholar]
- 3.Van Ancum J.M., Scheerman K., Jonkman N.H. Change in muscle strength and muscle mass in older hospitalized patients: A systematic review and meta-analysis. Exp Gerontol. 2017;92:34–41. doi: 10.1016/j.exger.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 4.Kortebein P., Ferrando A., Lombeida J. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA. 2007;297:1772–1774. doi: 10.1001/jama.297.16.1772-b. [DOI] [PubMed] [Google Scholar]
- 5.Mahoney J., Sager M., Dunham N.C., Johnson J. Risk of falls after hospital discharge. J Am Geriatr Soc. 1994;42:269–274. doi: 10.1111/j.1532-5415.1994.tb01750.x. [DOI] [PubMed] [Google Scholar]
- 6.Sherrington C., Lord S.R., Close J.C. A simple tool predicted probability of falling after aged care inpatient rehabilitation. J Clin Epidemiol. 2011;64:779–786. doi: 10.1016/j.jclinepi.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 7.Gill T.M., Allore H.G., Holford T.R., Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 8.Buurman B.M., Hoogerduijn J.G., de Haan R.J. Geriatric conditions in acutely hospitalized older patients: Prevalence and one-year survival and functional decline. PLoS One. 2011;6:e26951. doi: 10.1371/journal.pone.0026951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown C.J., Redden D.T., Flood K.L., Allman R.M. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57:1660–1665. doi: 10.1111/j.1532-5415.2009.02393.x. [DOI] [PubMed] [Google Scholar]
- 10.Pedersen M.M., Bodilsen A.C., Petersen J. Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol. 2013;68:331–337. doi: 10.1093/gerona/gls165. [DOI] [PubMed] [Google Scholar]
- 11.De Souto Barreto P., Demougeot L., Vellas B., Rolland Y. How much exercise are older adults living in long-term cares doing in daily life? A cross-sectional study. J Sports Sci. 2015;33:116–124. doi: 10.1080/02640414.2014.928828. [DOI] [PubMed] [Google Scholar]
- 12.Martin J.L., Webber A.P., Alam T. Daytime sleeping, sleep disturbance, and circadian rhythms in the nursing home. Am J Geriatr Psychiatry. 2006;14:121–129. doi: 10.1097/01.JGP.0000192483.35555.a3. [DOI] [PubMed] [Google Scholar]
- 13.Beard J.R., Officer A., de Carvalho I.A. The world report on ageing and health: A policy framework for healthy ageing. Lancet. 2016;387:2145–2154. doi: 10.1016/S0140-6736(15)00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Izquierdo M., Morley J.E., Lucia A. Exercise in people over 85: Advanced age is no barrier to the benefits of tailored exercise. BMJ. 2020;368:m402. doi: 10.1136/bmj.m402. [DOI] [PubMed] [Google Scholar]
- 15.Tak E., Kuiper R., Chorus A., Hopman-Rock M. Prevention of onset and progression of basic ADL disability by physical activity in community dwelling older adults: A meta-analysis. Ageing Res Rev. 2013;12:329–338. doi: 10.1016/j.arr.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Scheerman K., Raaijmakers K., Otten R.H.J. Effect of physical interventions on physical performance and physical activity in older patients during hospitalization: A systematic review. BMC Geriatr. 2018;18:288. doi: 10.1186/s12877-018-0965-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corregidor-Sánchez A.I., Segura-Fragoso A., Rodríguez-Hernández M. Can exergames contribute to improving walking capacity in older adults? A systematic review and meta-analysis. Maturitas. 2020;132:40–48. doi: 10.1016/j.maturitas.2019.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Lauzé M., Martel D., Aubertin-Leheudre M. Feasibility and effects of a physical activity program using gerontechnology in assisted living communities for older adults. J Am Med Dir Assoc. 2017;18:1069–1075. doi: 10.1016/j.jamda.2017.06.030. [DOI] [PubMed] [Google Scholar]
- 19.Barbosa Neves B., Franz R., Judges R. Can digital technology enhance social connectedness among older adults? A feasibility study. J Appl Gerontol. 2019;38:49–72. doi: 10.1177/0733464817741369. [DOI] [PubMed] [Google Scholar]
- 20.Wójcicki T.R., Fanning J., Awick E.A. Maintenance effects of a DVD-delivered exercise intervention on physical function in older adults. J Gerontol A Biol Sci Med Sci. 2015;70:785–789. doi: 10.1093/gerona/glu188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ortiz-Alonso J., Bustamante-Ara N., Valenzuela P.L. Effect of a simple exercise programme on hospitalisation-associated disability in older patients: a randomised controlled trial. J Am Med Dir Assoc. 2020;21:531–537.e1. doi: 10.1016/j.jamda.2019.11.027. [DOI] [PubMed] [Google Scholar]
- 22.Carvalho L.P., Kergoat M.J., Bolduc A., Aubertin-Leheudre M. A systematic approach for prescribing posthospitalization home-based physical activity for mobility in older adults: The PATH Study. J Am Med Dir Assoc. 2019;20:1287–1293. doi: 10.1016/j.jamda.2019.01.143. [DOI] [PubMed] [Google Scholar]
- 23.Juneau A., Bolduc A., Nguyen P. Feasibility of implementing an exercise program in a geriatric assessment unit: The SPRINT Program. Can Geriatr J. 2018;21:284–289. doi: 10.5770/cgj.21.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aubertin-Leheudre M, Peyrusqué E, Buckinx F, et al. Potential efficacy of pragmatic exercise program (SPRINT) during hospitalization in older adults on health care and physical performance: A pilot study. Paper presented at: International Conference on Frailty and Sarcopenia Research (ICFSR 2020); March 11-13, 2020; Toulouse, Occitanie, France. [DOI] [PubMed]