Abstract
We present a 24-year-old male who developed an infected hematoma that resulted in sciatic nerve injury after he underwent an endoscopic sciatic nerve decompression. He underwent urgent hematoma evacuation and cultures speciated as Salmonella. At 4 months’ follow-up, the patient’s nerve had improved motor and sensory function. This case highlights the importance of obtaining appropriate hemostasis at the end of an endoscopic sciatic nerve decompression.
Deep gluteal syndrome (DGS) is a term used to describe sciatic nerve compression in the deep gluteal space that results in buttock pain.1 The sciatic nerve can be entrapped by numerous structures, including the piriformis, quadratus femoris, gemelli, obturator internus and externus, hamstrings, fibrous bands, and blood vessels. These patients are challenging to diagnose clinically, so it is imperative that surgeons keep a broad differential in mind when such patients present.
Initial conservative management of DGS typically includes an extra-articular injection of a corticosteroid and/or a local anesthetic plus a full course of physical therapy. If conservative management fails, decompression of the sciatic nerve can be done either open or via an endoscopic approach.2, 3, 4, 5 Endoscopic surgical decompression of the sciatic nerve has been shown to result in significant improvements in patient-reported outcomes.6,7 There is the peritrochanteric supine approach as well as the posterior approach to address DGS. Advantages of the posterior approach include the ability to treat hamstring pathology and ischial bursitis, allowing for more complete decompression of the sciatic nerve.4,5 As the use of endoscopic sciatic nerve decompression gains popularity, it is imperative that more literature be reported on the procedure to improve surgeons’ knowledge and to counsel patients appropriately. Currently, there is very little literature concerning the complications of endoscopic nerve decompression. We present the case of a 24-year-old patient who underwent an endoscopic sciatic nerve decompression for DGS that was complicated by an infected hematoma, resulting in significant sciatic nerve injury.
Case Report
A 24-year-old man presented with 1 year of right anterior, posterior and lateral hip pain after a ground-level fall 10 years earlier. Prior to presenting to our institution, the patient was diagnosed with bilateral labral tears and femoracetabular impingement and underwent bilateral arthroscopic labral repair and femoracetabular impingement resection. The operations left the patient free of anterior groin pain, but persistent lateral and buttock pain remained in the right hip. Prior to endoscopic sciatic nerve decompression, the patient underwent endoscopic trochanteric bursectomy by the senior author. Lysis of adhesions and scar tissue and partial iliotibial band release was performed. This successfully alleviated his lateral hip pain, but he continued to complain of debilitating posterior buttock pain.
The posterior pain radiated below the knee to the foot in the sciatic nerve distribution. This pain was unbearable and interfered with the activities of daily life. On examination, the patient had pain over his buttock and tenderness over the course of the sciatic nerve as well as radiating nerve pain and paresthesias in the sciatic nerve distribution down to the foot. Flexion, adduction, internal rotation, and flexion plus abduction and external rotation testing did not elicit hip pain. He had a diagnostic injection of his piriformis, which was equivocal with respect to pain relief. After extensive discussion, he decided the pain was not tolerable, given the activity goals of this young patient. His lumbar MRI and EMG were normal. He had no hamstring pathology, obvious sciatic nerve compression or piriformis pathology on the MRI of his pelvis. Because there was significant scarring of the peripheral lateral compartment after his initial fall, he was offered endoscopic exploration of the deep gluteal space to address scarring and potential fibrovascular bands of the sciatic nerve.
The patient was positioned prone, and portals were created along the gluteal crease. The ischial tuberosity was located using c-arm fluoroscopy. Triangulation was performed with the camera. First, ischial bursectomy was performed. The sciatic nerve was identified by following the posterior femoral cutaneous nerve; the sciatic nerve was decompressed up to the sciatic notch. Thick scarring and fibrovascular bands were identified in this area. The sciatic nerve was dissected and released from the piriformis and gemelli. At the time of surgical closure, there was no active bleeding inside the deep gluteal space.
After surgery, the patient was noted to be neurovascularly intact, with 5/5 strength and normal sensation in the right lower extremity. There was swelling on the operative buttock, but the swelling was not tense. Approximately 3 hours later, the patient walked to the bathroom and returned to the stretcher, when he suddenly lost sensation in the posterior leg and had profound weakness with dorsiflexion and plantarflexion. The patient complained of excruciating pain, and examination found weakness and loss of sensation in the sciatic nerve distribution on his right side. At that time, the patient’s differential diagnosis included a shifting nerve block versus hematoma. Due to his substantial pain and abnormal neurovascular examination, he was admitted to the hospital. An urgent CT scan was performed, and it showed a large hematoma compressing the sciatic nerve. A CT angiogram was also performed, and it did not show any active bleeding.
The patient underwent open surgical evacuation of the hematoma within 24 hours through a posterolateral approach. More than a liter of hematoma was evacuated from the deep gluteal space. The sciatic nerve was exposed and found to be intact. The patient was taken to recovery in stable condition. Although he had some improvement in pain and neurologic function, deficit remained.
Ten days after the hematoma evacuation, he felt recurrent fullness in his buttock with the associated vital signs and laboratory results: temperature of 101.2˚ F, heart rate of 110, white blood count of 15.1 × 103/uL, and 74% neutrophils. A postoperative MRI showed 2 recurrent hematomas; 1 displaced the sciatic nerve near the sciatic notch, and the other compressed the nerve from the level of the piriformis down the thigh. The patient underwent CT-guided aspiration and cultures with a cell count of the aspiration. A liter of hematoma was aspirated. Cultures grew Salmonella enteritidis.
Due to the uncommon pathogen, infectious-disease specialists investigated possible sources of infection. The patient mentioned travel outside of the country to Cuba, where he ate undercooked pork, and reported contact with an individual who had symptoms of infectious gastroenteritis approximately 1-2 months prior to surgery. The patient denied any gastrointestinal symptoms himself. After a 6-week regimen of cefpodoxime and Bactrim DS, the infection was eliminated as per infectious disease consultation.
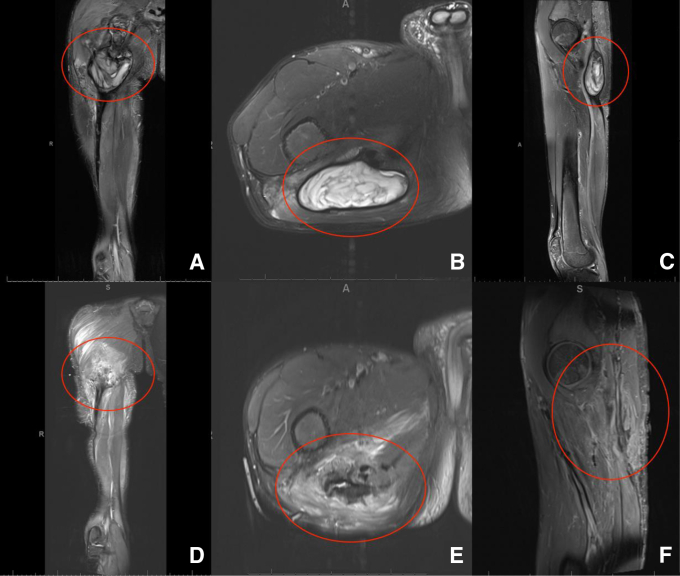
Two months later, the patient reported severe, constant deep pain in the right buttock that radiated to the posterior thigh, lower leg and foot. In addition, he mentioned lower-extremity, foot and groin numbness. An MRI demonstrated a recurrence of hematoma as well as posterior compartment muscular denervation (Fig 1).
Fig. 1.
The patient’s right-sided subgluteal hematoma, highlighted by the red graphics. Note the variable appearances on various MRI views, which were taken while the patient was positioned supine. T2 coronal (A), axial (B) and sagittal (C) MR images of the preoperative hematoma formation. Postoperative T2 coronal (D), axial (E) and sagittal (F) MR images showing interval resolution of the right subgluteal hematoma.
After consultation with a peripheral nerve specialist, the hematoma was surgically drained and a thorough sciatic neurolysis was performed using an open posterior approach. The hematoma was a thick gelatinous material and was abnormal looking, likely the sequalae of the S. enteritidis infection. Cultures from this operation showed no growth. Postoperatively, the patient complained of heaviness and pain in the right lower extremity, though MRI showed no recurrence of the hematoma. At the 4-month follow-up, he had the following physical examination findings: 1/5 extensor hallicus longus, 3/5 dorsiflexion, 3/5 ankle eversion, 4/5 plantarflexion, and sensation intact to light touch, with the exception of the dorsal and lateral foot. At follow-up, the patient reported improved sensation and motor function of the right lower extremity in the sciatic nerve distribution.
Discussion
This case is the first to report an infected hematoma with resultant sciatic nerve compression after endoscopic sciatic nerve decompression. In addition, we report the unique finding of recurrent hematomas, leading to 2 revision open sciatic nerve compressions with clinic manifestations of sciatic nerve compression. Endoscopic surgery in the deep gluteal space is an emerging field, and its complications need to be highlighted.
In the English literature, only minor complications have been associated with endoscopic sciatic nerve decompression.8 However, there has been a report of sciatic nerve compression due to hematoma secondary to iatrogenic injury of the inferior gluteal artery in the setting of a hip arthroscopy.9 Our patient took aspirin for deep vein thrombosis prophylaxis during his hospital stay, but aspirin is unlikely to have led to this recurrent hematoma formation.10 To our knowledge, this is the first report of an infected hematoma and sciatic nerve compression in the absence of a known arterial injury, coagulopathy or strong anticoagulative therapy.
S. enteritidis infection is a common cause of bacterial gastroenteritis but is a rare surgical-site infection. In some cases, this infection can spread hematogenously and seed in a distant site. Although this is extremely rare in an otherwise healthy patient, patients typically have symptoms of the index infection.11 A recent case report outlined the seeding of a prosthetic hip with S. enteritidis, which occurred weeks after the likely gastroenteritis and without detectable bacteremia.12 Our patient was probably exposed to the pathogen due to consumption of undercooked meat and contact with a symptomatic individual, but our patient denied any symptoms of gastroenteritis.
This case report presents a unique sequela of endoscopic sciatic nerve decompression. As indications for endoscopic sciatic nerve decompression continue to expand, it is important to understand and consider potential complications that can lead to long-term neurologic impairment.
Footnotes
All authors contributed equally.
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary data
References
- 1.McCrory P., Bell S. Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med. 1999;27:261–274. doi: 10.2165/00007256-199927040-00005. [DOI] [PubMed] [Google Scholar]
- 2.Benson E.R., Schutzer S.F. Posttraumatic piriformis syndrome: Diagnosis and results of operative treatment. J Bone Joint Surg Am. 1999;81:941–949. [PubMed] [Google Scholar]
- 3.Vandertop W.P., Bosma N.J. The piriformis syndrome: A case report. J Bone Joint Surg Am. 1991;73:1095–1097. [PubMed] [Google Scholar]
- 4.Martin H.D., Shears S.A., Johnson J.C., Smathers A.M., Palmer I.J. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011;27:172–181. doi: 10.1016/j.arthro.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Jackson T.J. Endoscopic sciatic nerve decompression in the prone position: An ischial-based approach. Arthros Tech. 2016;5:e637–e642. doi: 10.1016/j.eats.2016.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park M.S., Jeong S.Y., Yoon S.J. Endoscopic sciatic nerve decompression after fracture or reconstructive surgery of the acetabulum in comparison with endoscopic treatments in idiopathic deep gluteal syndrome. Clin J Sport Med. 2019;29:203–208. doi: 10.1097/JSM.0000000000000504. [DOI] [PubMed] [Google Scholar]
- 7.Ham D.H., Chung C., Jung D.U. Effectiveness of Endoscopic sciatic nerve decompression for the treatment of deep gluteal syndrome. Hip Pelvis. 2018;30:29–36. doi: 10.5371/hp.2018.30.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kay J., de Sa D., Morrison L., et al. Surgical management of deep gluteal syndrome causing sciatic nerve entrapment: A systematic review. Arthroscopy. 2017;33:2263–2278. doi: 10.1016/j.arthro.2017.06.041. [DOI] [PubMed] [Google Scholar]
- 9.Bruno M., Longhino V., Sansone V. A catastrophic complication of hip arthroscopy. Arthroscopy. 2011;27:1150–1152. doi: 10.1016/j.arthro.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 10.Azboy I., Barrack R., Thomas A.M., Haddad F.S., Parvizi J. Aspirin and the prevention of venous thromboembolism following total joint arthroplasty: Commonly asked questions. Bone Joint J. 2017;99-b:1420–1430. doi: 10.1302/0301-620X.99B11.BJJ-2017-0337.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rohilla R., Bhatia M., Gupta P., Singh A., Shankar R., Omar B.J. Salmonella osteomyelitis: A rare extraintestinal manifestation of an endemic pathogen. J Lab Physicians. 2019;11:164–170. doi: 10.4103/JLP.JLP_165_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dojode C.M.R., Hemingway J.S., Damodaran P., Shah N.N. Total hip arthroplasty infection caused by an unusual organism, Salmonella; its successful management and literature review. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-224792. bcr-2018-224792. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.