Abstract
Objective
Ever since the first positive test was identified on January 21, 2020, Washington State has been on the frontlines of the coronavirus disease 2019 (COVID-19) pandemic. Using information obtained from Italian surgeons in Milan and given the concerns regarding the increasing case numbers in Washington State, we implemented new vascular surgery guidelines, which canceled all nonemergent surgical procedures and involved significant changes to our inpatient and outpatient workflow. The consequences of these decisions are not yet understood.
Methods
The vascular surgery division at Harborview Medical Center immediately instituted new vascular surgery COVID-19 practice guidelines on March 17, 2020. Subsequent clinic, operative, and consultation volume data were collected for the next 4 weeks and compared with the historical averages. The Washington State case and death numbers and University of Washington Medical Center (UW Medicine) hospital case volumes were collected from publicly available sources.
Results
Since March 10, 2020, the number of confirmed positive COVID-19 cases within the UW Medicine system has increased 1867%, with floor and intensive care unit bed usage increasing by 120% and 215%, respectively. After instituting our new COVID-19 guidelines, our average weekly clinical volume decreased by 96.5% (from 43.1 patients to 1.5 patients per week), our average weekly surgical volume decreased by 71.7% (from 15 cases to 4.25 cases per week), and our inpatient consultation volume decreased to 1.81 consultations daily; 60% of the consultations were completed as telemedicine “e-consults” in which the patient was never evaluated in-person. The trainee surgical volume has also decreased by 86.4% for the vascular surgery fellow and 84.8% for the integrated resident.
Conclusions
The COVID-19 pandemic has changed every aspect of “normal” vascular surgical practice in a large academic institution. New practice guidelines effectively reduced operating room usage and decreased staff and trainee exposure to potential infection, with the changes to clinic volume not resulting in an immediate increase in emergency department or inpatient consultations or acute surgical emergencies. These changes, although preserving resources, have also reduced trainee exposure and operative volume significantly, which requires new modes of education delivery. The lessons learned during the COVID-19 pandemic, if analyzed, will help us prepare for the next crisis.
Keywords: Coronavirus, COVID-19, Pandemic, Seattle, Washington
Washington State has been on the frontlines of the coronavirus disease 2019 (COVID-19) pandemic. The first positive test was identified on January 21, 2020, in Snohomish County, when a man presented to a local hospital with the typical symptoms and a history of recent travel to Wuhan, China. The power of the virus revealed itself several weeks later in a skilled nursing facility in Kirkland, Washington, a Seattle suburb located 11 miles from downtown and only 8 miles from the main campus of the University of Washington, when the first documented U.S. death occurred. At least 37 residents of the Life Health Center later died, and on March 11, 2020, Governor Jay Inslee restricted gatherings of >250 people in King, Snohomish, and Pierce counties. Two days later, he announced that all schools in the state would close for 6 weeks, and 2 days after that, with coronavirus infections and deaths still increasing, he revised his restrictions on gatherings to a 50-person maximum and ordered the temporary shutdown of all bars, restaurants, gyms, hair and nail salons, and other social gathering places to stop the spread of COVID-19.
Our vascular surgery group responded quickly to the evolving situation, implementing new COVID-19 vascular surgery guidelines given the increasing case numbers within our state. After discussions with Italian surgeons in Milan regarding the COVID-19 situation there, we issued a “Letter from Seattle” on March 20, 2020, warning surgeons all over America to cease all elective surgical procedures to increase hospital capacity in anticipation of the surge in patients with COVID-19 we expected.1 , 2 Washington State, due in part to the aggressive social distancing measures instituted early, has now been hailed as a model for “flattening the curve.”
The full effect of this pandemic and of our responses has yet to be understood. The purpose of our report, “fast tracked” by the editors, Drs Peter Lawrence and Peter Gloviczki, is to elevate the peer-to-peer communication for other vascular surgery groups who will face similar challenges in the coming days to weeks. Our intent is to present the lessons learned and provide guidelines for daily workflow and continued medical education during these unprecedented times.
Methods
The vascular surgery division at Harborview Medical Center immediately instituted new vascular surgery COVID-19 practice guidelines on March 17, 2020. These guidelines included ceasing all nonemergent operations, cancelling all clinic patients (except for those with wound-healing concerns), restructuring inpatient and outpatient services to minimize staff and trainee exposure to patients, and expanding the telemedicine capacity, including permitting remote “e-consults” when possible for new inpatient and emergency department consultations (Table I ).1 Subsequent clinic, operative, and consultation volume data were collected prospectively after institution of the guidelines for the next 4 weeks and were compared with the historical averages of the volumes from the previous 12 months. The trainee operative volume for the on-service vascular surgery fellow and integrated resident were also tracked prospectively and compared with the historical averages for each trainee.
Table I.
Harborview vascular surgery COVID-19 clinical practice guidelines
| General guidelines |
| All staff and trainees agree to comply with all UW Medicine and Harborview Medical Center COVID-19-specific policies and procedures |
| All guidelines are subject to change |
| Inpatient |
| The inpatient Harborview vascular surgery service will consist of 1 attending and 1 vascular surgery trainee (either resident or fellow), with a backup designated for each available should an exposure occur or if clinical needs require additional support |
| Outpatient |
| All routine in-person follow-up visits and new patient consultations will be cancelled |
| All patients will be offered a telemedicine visit |
| The only patients to be seen in clinic are those with surgical wound healing concerns or those who require staple or suture removal; same-day or next day clinic visits will be arranged to avoid the emergency room |
| The clinic will be formally staffed by the weekly on-call attending covering inpatient and outpatient issues |
| New inpatient and emergency department vascular surgery consultations |
| Vascular surgery will continue to respond to consultations at all times and will continue to be immediately available to help as needed |
| In the absence of a surgical emergency, all consultations will be reviewed by the on-call vascular trainee (resident or fellow) and vascular attending before an in-person evaluation of the patient; the patient will only be evaluated in-person by the vascular surgery team if deemed necessary by the on-call trainee and attending |
| In accordance with the COVID-19-specific vascular surgery operating room policy, only emergent operative cases will be performed; all nonemergent operations will be evaluated on a case-by-case basis, with nearly all deferred to the outpatient setting |
| Vascular surgery procedures and operating room usage |
| The following emergent procedures will be performed: ruptured abdominal aortic aneurysms, severe grade blunt aortic injuries, complicated type B aortic dissections, wet gangrene, and acute limb ischemia, depending on resources available |
| Other urgent procedures that will be considered according to the resources available include symptomatic aneurysms, mycotic aneurysms, symptomatic carotid disease, and moderate grade blunt aortic injuries |
| No elective procedures will be performed |
| The Harborview risk score for ruptured abdominal aortic aneurysms should be applied to all patients presenting with ruptured abdominal aortic aneurysms to predict the 30-day mortality before the patient is taken to the operating room3; any patient with a ≥69% mortality risk will not be offered transfer, and any patient with an ≥80% mortality risk will not be offered surgery3 |
| Transfer |
| Patients should only be transferred to Harborview Medical Center for vascular care if surgery is required and the procedure qualifies for scheduling as outlined in the “Vascular surgery procedures and operating room usage” section |
| Patients with uncomplicated type B aortic dissection should not be transferred; they should be treated at the local institution with anti-impulse control wherever possible; patients can be transferred if local resources for treatment are not available |
| Patients with a ruptured abdominal aortic aneurysm and a ≥69% expected 30-day mortality using the Harborview risk score (≥2 points) will not be transferred3 |
| Patients accepted for transfer to Harborview Medical Center and meeting the listed criteria for surgery should be taken directly to the operating room, bypassing the emergency department |
| COVID-19 screening questions will be asked by all accepting physicians |
| Consulting for COVID-19-positive patients |
| Before an in-person evaluation, the consultation will be discussed by the on-call vascular trainee and attending to determine whether an in-person evaluation is required; telehealth options will be used preferentially when available |
| If an in-person evaluation is required, the on-call trainee and attending should discuss whether the trainee and attending will examine the patient together or whether the trainee or attending will examine the patient alone—only 1 examination permitted |
| When evaluating a COVID-19-positive patient or person under investigation, the proper sequence for putting on and removing PPE will be followed4 |
| Staff who are pregnant, have chronic medical conditions, are aged >65 years, or are immunosuppressed will not come into contact with nor operate on any COVID-19-positive patient or person under investigation |
| Operating on COVID-19-positive patients |
| When operating on a COVID-19-positive patient or person under investigation, the proper sequence for putting on and removing PPE will be followed4 |
| Staff who are pregnant, have chronic medical conditions, are aged >65 years, or are immunosuppressed will not come into contact with nor operate on any COVID-19-positive patient or person under investigation |
| Redistribution of service responsibilities |
| All vascular surgery trainees agree to being reassigned to other services as needed to meet clinical need, as deemed necessary by the graduate medical education office and vascular surgery program director |
| The vascular surgery division can be asked to admit patients not usually admitted to our service in an attempt to conserve internal medicine resources (eg, patients with diabetic foot infections or cellulitis requiring intravenous antibiotics) |
PPE, Personal protective equipment; UW, University of Washington.
Results
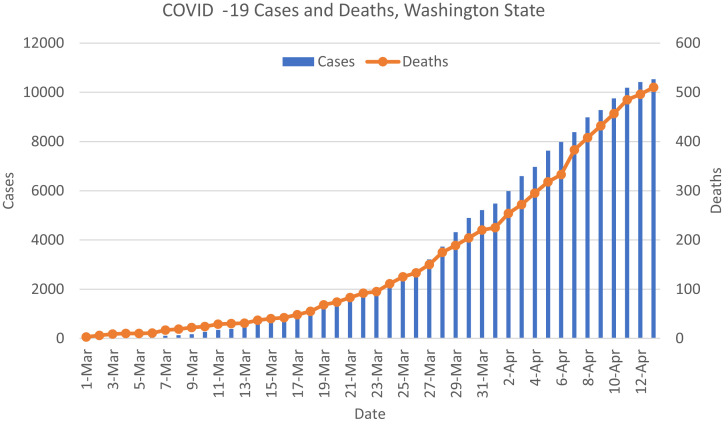
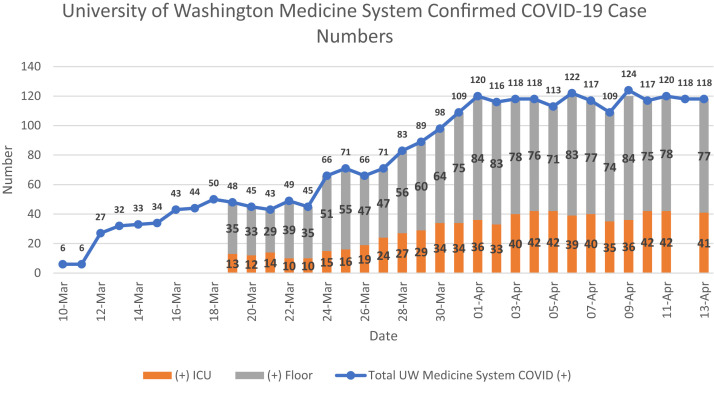
After the first several diagnosed cases of COVID-19 within Washington State, we began tracking the number of confirmed cases and deaths daily from the publicly available information from the Center for Systems Science and Engineering at Johns Hopkins University (Fig 1 ).5 Because the number of cases and deaths within Washington State have increased with time along a gradual, but exponential, scale, similar to trends seen elsewhere in the United States, the number of cases within the University of Washington Medical Center (UW Medicine) has also increased (Fig 2 ). Since the UW first started providing information on case numbers on March 10, 2020, the number of confirmed positive COVID-19 cases within the UW Medicine system has increased 1867%, from six cases to 118 cases. Similarly, the number of floor and intensive care unit beds required to treating these patients has increased by 120% for the floor beds (from 35 to 77) and 215% for intensive care unit beds (from 13 to 41).
Fig 1.
COVID-19 confirmed positive case (blue) and death (orange) trends in Washington State from March 1, 2020 to April 13, 2020.
Fig 2.
Number of confirmed positive cases within the University of Washington (UW) system (blue) and intensive care unit (orange) and floor (gray) bed usage. The number of cases within the UW system has increased over time, with an increase in both the number of floor and intensive care (ICU) beds used. Note ICU and floor bed information were only available beginning March 19, 2020, and no information on floor or ICU bed use was provided on April 12, 2020.
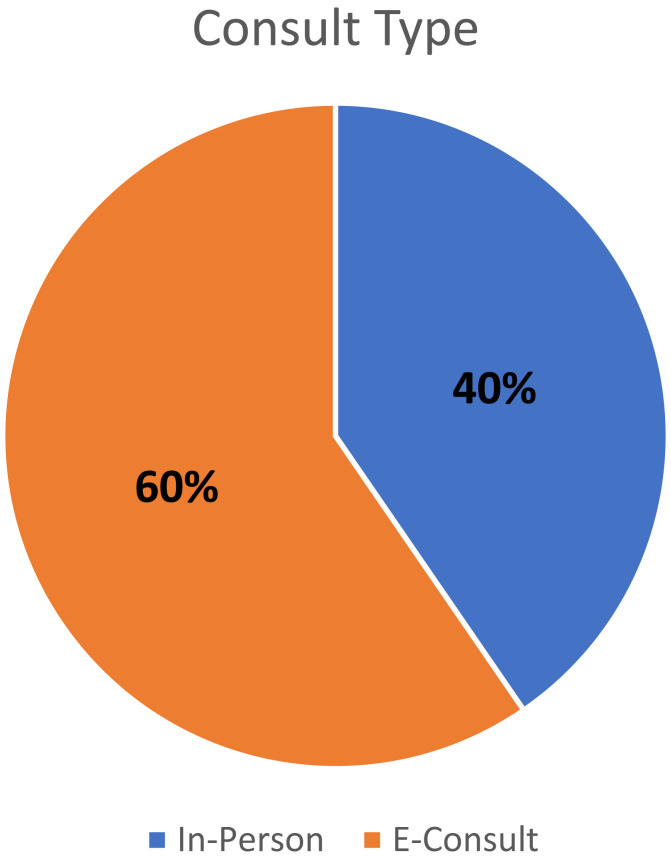
In response to these trends, our division immediately implemented our new vascular surgery COVID-19 guidelines on March 17, 2020 (Table I). In the 4 weeks after instituting these changes, the average weekly clinical volume decreased by 96.5% (from 43.1 patients to 1.5 per week), with the average weekly surgical volume decreasing by 71.7% (from 15 cases to 4.25 cases per week). The operative cases performed after institution of the guidelines are listed in Table II . The inpatient consultation volume also decreased to 1.81 consultations daily (47 consultations within 26 days), with 60% consisting of telemedicine “e-consults,” in which the patient was never evaluated in person (Fig 3 ). Of the 47 consultations, two involved a patient with confirmed COVID-19-positive infection and three involved a person under investigation whose test result later was negative. The trainee weekly surgical volume also decreased by 86.4% (from 12.9 cases weekly to 1.75) for the vascular surgery fellow and 84.8% (from 8.2 cases weekly to 1.25) for the postgraduate year 3 integrated resident.
Table II.
Operative cases performed since instituting COVID-19 vascular surgery guidelines (March 17, 2020-April 13, 2020)
| Pt. No. | Operation | Case notes | Hospital (ICU) LOS, days | Complications |
|---|---|---|---|---|
| 1 | Aortofemoral bypass for acute thrombosis of left common iliac artery | Intraoperative consultation; thrombosis occurred during spine exposure performed by general surgery | 4 (1) | None |
| 2a | Open repair of ruptured juxtarenal AAA with temporary abdominal closure | None | 13 (13) | Ischemic colitis, respiratory failure, myocardial infarction, death |
| 2a | Second-look exploratory laparotomy with sigmoid colectomy | None | NA | NA |
| 2a | Exploratory laparotomy, creation of sigmoid colostomy, abdominal closure | None | NA | NA |
| 3 | Lower extremity angiogram for chronic limb-threatening ischemia | Already inpatient at consultation, with open minor amputation already performed for wet gangrene by general surgery | 11 (0) | None |
| 4 | Carotid artery GSW repair using Dacron interposition graft | None | 8 (3) | None |
| 5 | Above-the-knee amputation for wet gangrene | None | 6 (0) | None |
| 6 | Intraoperative consultation for arterial hemorrhage during orthopedic surgery | None | 7 (0) | None |
| 7 | Endovascular repair of ruptured AAA | None | 4 (1) | None |
| 8 | Femoral artery repair after VA-ECMO decannulation | Already inpatient at consultation | Remained an in-patient | None |
| 9 | Brachial artery GSW repair with GSV interposition graft | None | 4 (2) | None |
| 10 | Brachial artery GSW repair with GSV interposition graft | None | 3 (1) | None |
| 11 | Subclavian angiogram and removal of CVC from SCA with balloon angioplasty for hemostasis | COVID-19 positive | Remained an in-patient | None |
| 12 | Infected AV graft ligation and excision | None | Remains inpatient | None |
| 13b | SFA GSW repair with GSV interposition graft, 4 compartment fasciotomies | None | 4 (1) | None |
| 13b | Fasciotomy washout and closure | None | None | None |
| 14 | Radial artery injury primary repair with thrombectomy | None | 2 (0) | None |
AAA, Abdominal aortic aneurysm; AV, atrioventricular; CVC, central venous catheter; GSV, greater saphenous vein; GSW, gunshot wound; ICU, intensive care unit; LOS, length of stay; NA, not applicable; Pt. No., patient number; SCA, subclavian artery; SFA, superficial femoral artery; VA-ECMO, venoarterial extracorporeal membrane oxygenation.
Patient 2 underwent three separate procedures.
Patient 13 underwent two separate procedures.
Fig 3.
Distribution of telemedicine (“e-consults”) versus in-person consultations; 60% of consultations were performed as e-consults and did not require an in-person evaluation.
Discussion
The COVID-19 pandemic has changed every aspect of “normal” practice in a large academic institution. As vascular surgeons we are looked on to be leaders and the so-called firemen of the hospital, responding to urgent intraoperative consultations and requests from our medicine and surgical colleagues. Our practice consists of treating the highest risk patients with both cutting edge, minimally invasive techniques and large open procedures. Our patients require the use of personnel, equipment (eg, gowns, gloves, masks), and hospital space for their recovery. Most of our patients are elderly, who often require other medical specialties to assist in their care both before and after a procedure. On March 12, 2020, our department announced that elective cases should be postponed in an effort to create the capacity needed for the expected surge of patients with COVID-19. We quickly mobilized and created our list of nonelective procedures and planned on treating abdominal aortic aneurysms (AAAs) measuring >5.5 cm, chronic limb-threatening ischemia with tissue loss, dialysis access, and acute limb ischemia. We rescheduled all other cases and decreased the number of our clinic patients in accordance with these parameters. However, as stated, in discussion with our Italian colleagues (Drs Pierantonio Rimoldi and Germano Melissano), who were a few weeks ahead of us in the pandemic, we quickly adopted their plan of performing only emergent procedures.2 We used the following philosophy: if a patient had been seen in the clinic and scheduled for a procedure in the future, the procedure was elective. Our mindset, therefore, changed, and although it was not a comfortable feeling among our surgeons, we recognized that even a patient with CLTI or AAA seen in the clinic will not usually have surgery scheduled emergently. Instead the surgery was usually scheduled after appropriate risk stratification has been performed.
After adopting this philosophy, we created a method to perform our duties and assist as possible in our system. To our surprise, most of our patients understood our reasoning, and many were relieved to hear that they did not need to enter the hospital and potentially be exposed. In addition, because our hospital imposed a strict visitation policy, many of our patients would have been entering the hospital without family support available during their recovery. We enacted teleconferencing and telemedicine protocols to maintain our communication with patients and for our division (Table I) and found that, after using these methods, we have not been flooded with acute cases or patients requiring amputations at this point. Our clinical volume has decreased significantly, and many of our consultations have been able to be performed with telehealth.
Other important consequences of these changes include the potentially damaging effects that a decreased volume can have on a training program. At our institution, we take great pride in providing our trainees with high volumes of complex procedures, which has been reduced 71.7% by the present crisis. To combat the lack of procedures, we have added more electronic educational events, including daily recorded lectures, and have continued to work on scholarly activities and research, all of which can be accomplished remotely. By concentrating on areas of productivity, we have been maintaining trainee morale and education, with the assumption that the operative volume will return once the pandemic surge has ended. However, just as for any program, the lack of procedures will be a lingering concern as we are asked to do less in the operating room.
During these unprecedented times, we have also found ourselves rapidly adjusting to new hospital policy, with changes occurring daily as resources become available and institutional knowledge of this new pathogen improves. As our institutional practices have changed, from testing only symptomatic patients to now testing all patients requiring admission to the hospital, our operating room policies have also changed and now include testing of all surgical patients preoperatively. Although emergent cases with test results pending had originally been performed using full airborne precautions, this quickly became unsustainable. Thus, our operating room policy has shifted to using full airborne precautions only for those with pending test results who are unable to give a reliable history—in contrast to those patients who have a pending test result but are able to deny any symptoms of infection. For the latter patients, full airborne precautions are only maintained during the 30 minutes after intubation and extubation and the anesthesia provider is the only person present in the operating room. Internal reports have noted previously that during these 30 minutes, circulation within the operating room will clear >99% of air particles. Thus, our institution has adopted the policy of proceeding with standard precautions after the 30-minute recirculation period for those patients with pending test results who are asymptomatic and thus deemed of low risk.
In our division, we believe that our role is to conserve personal protective equipment, to protect our patients and personnel, and to increase hospital bed capacity. If we consider even our emergent case of the open ruptured juxtarenal AAA, we can see the resources required. During that procedure, the patient's colon appeared potentially threatened; thus, a temporary abdominal closure was performed. A subsequent colectomy and repeat laparotomy and closure was required, with the patient developing respiratory failure postoperatively with computed tomography findings concerning for COVID-19 infection. The patient was, therefore, transferred to a COVID-19 unit until the results of testing were negative. In addition, the patient experienced a myocardial infarction during recovery, necessitating percutaneous coronary intervention. This all occurred during the restricted visitation policy; thus, the family of the patient, who could not visit in person, were updated remotely. Ultimately, the patient was transitioned to comfort care measures only after he had failed to progress. Although it is difficult to understand whether this patient's outcome would have been different in “normal” situations, what is clear is that the number of resources required for this emergent procedure would likely not be available during a true crisis.
Conclusions
Ultimately, every vascular surgeon's practice will be affected by COVID-19, and we believe everyone needs to look to their local hospital leadership for direction. We were one of the early cities in the United States to be affected by the pandemic, and we have been through several iterations of practice modification, as described. Our guidelines will continue to be malleable as the situation requires, and we are starting to plan for a return of capabilities as our situation in Seattle allows. We believe in our system and understand we might have a unique perspective, and that other locations could be in a different stage of this pandemic. We look forward to the future, when this pandemic is behind us, and understand that we have likely developed tools that will make us more nimble and efficient when faced with the next crisis.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Kay B. Prominent Seattle hospital issues COVID-19 clinical practice guidelines for vascular surgery. Vascular Specialist. https://vascularspecialistonline.com/prominent-washington-hospital-issues-covid-19-clinical-guidelines/ Available at:
- 2.Starnes B.W., Singh N. Letter from Seattle: amid COVID-19 pandemic, time to act is long past due. Vascular Specialist. https://vascularspecialistonline.com/letter-from-seattle-amid-covid-19-pandemic-time-to-act-is-long-past-due/ Available at:
- 3.Garland B.T., Danaher P.J., Desikan S., Tran N.T., Quiroga E., Singh N. Preoperative risk score for the prediction of mortality after repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 2018;68:991–997. doi: 10.1016/j.jvs.2017.12.075. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention CDC Proper Sequence for Putting on and Removing PPE. https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf Available at: Accessed March 27, 2020.
- 5.Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Available at: