Abstract
Background
Leiomyomas are usually easily identifiable on routine imaging. However, there is increasing difficulty with diagnosing leiomyomas following degeneration. Subserosal leiomyomas that undergo cystic degeneration can imitate ovarian pathology.
Case
We present the case of a 39-year-old nulligravid woman who underwent surgery for a large pelvic mass originally suspected to be of ovarian origin. Intraoperatively, the mass was found to originate from the uterus and determined to be a large pedunculated, fluid-filled cyst arising from a fibroid which had undergone cystic degeneration. The mass was successfully removed laparoscopically through a single, two-centimeter port.
Conclusion
Gynecologists and radiologists should take into account this presentation when encountering suspected enlarged ovarian cysts without clearly identifying an origin. Laparoscopic intervention should be considered as the first line of management.
Keywords: Adnexal mass, Cystic degeneration, Degenerating fibroid, Pedunculated fibroid, Single-site port
Highlights
-
•
Degenerating leiomyomas are difficult to diagnose with routine imaging.
-
•
Subserosal leiomyomas with cystic degeneration can be mistaken for ovarian pathology.
-
•
Laparoscopic intervention should be considered first in pelvic masses of unknown origin.
1. Introduction
Uterine leiomyomas are the most prevalent pelvic tumor in women. Symptoms related to fibroids classically present in women aged thirty to forty, consistent with hormonal changes that occur during reproductive years [1]. There are a multitude of risk factors associated with developing leiomyomas including, but not limited to, race, parity, early menarche, hormonal contraception, hypertension, and genetics [1]. Leiomyomas, when symptomatic, commonly present with abnormal uterine bleeding, bulk-related symptoms or infertility [2,3]. Symptoms vary based on their location and size. The International Federation of Gynecology and Obstetrics (FIGO) developed a classification system for fibroids based on their location. They can be located or classified as submucosal (FIGO type 0, 1, 2), intramural (FIGO type 3, 4, 5), or subserosal (FIGO type 6, 7) [4]. Fibroids that are subserosal, more specifically Type 7, are pedunculated in character and can mimic ovarian pathology.
Fibroid degeneration typically occurs when a fibroid outgrows its vascular supply [5]. There are various processes of fibroid degeneration. The most common is hyaline degeneration, which accounts for about 60% of all degenerating fibroids. Other types include: myxomatous, calcification, mucoid, cystic, red and fatty degeneration [5]. Cystic degeneration occurs in approximately 4% of degenerating leiomyomas. Degenerating fibroids can be difficult to diagnose on routine imaging due to their varying morphology and appearance. Cystic degeneration of subserosal fibroids can be particularly difficult to diagnose due to its resemblance to unknown ovarian pathology. This can affect treatment planning and frequently leads to unnecessary, more invasive, exploratory laparotomy.
2. Case Report
A 39-year-old nulligravid, premenopausal woman presented to the emergency room with abdominal pain and distention. She had no significant medical or family history. She reported a history of increasing abdominal distention over the past year. She was noted on CT scan to have a large 25-cm simple “ovarian” cyst (Fig. 1). The mass was described as simple, cystic and unilocular in character. There were no solid components, septations or other suspicious findings concerning for malignancy. For this reason, no additional labs or imaging were performed.
Fig. 1.
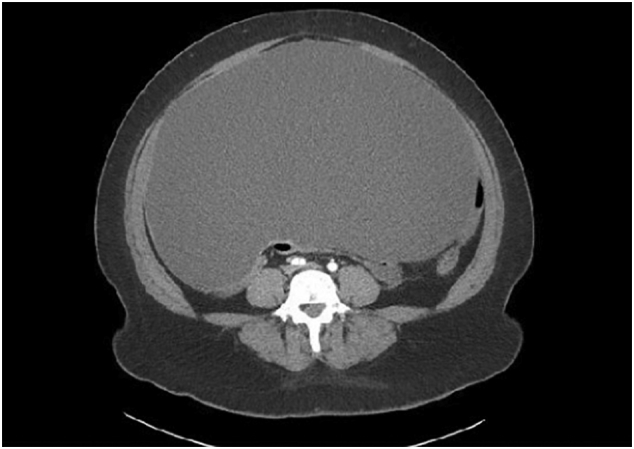
An axial non-enhanced computed tomography image of a 25 cm simple, cystic, unilocular mass, presumably of ovarian origin.
She was referred for outpatient follow-up with her gynecologist. She was counseled that the features of this cyst are highly suggestive of a benign process. However, she was also counseled on the low risk of malignancy and sequelae of surgical spillage in the setting of malignancy. She was offered conservative versus surgical management and after shared decision-making, the decision was made to proceed with laparoscopic exploration. The patient was consented, scheduled and taken to the operating room. A 2-cm single-site port was placed and the abdomen was inspected. Upon entry into the abdomen, the cystic mass was easily visualized. A purse-string stitch was placed and the cyst was incised and drained. Incision and drainage of the cyst revealed a yellow-colored fluid (Fig. 2A).
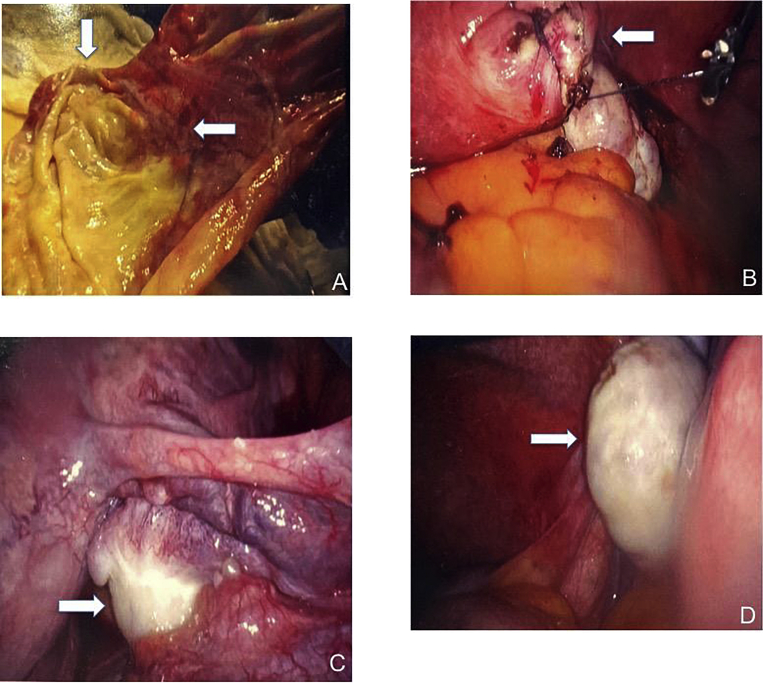
Fig. 2.
Intraoperative images at time of laparoscopic exploration. A: Image shows cystic degenerating fibroid status-post incision and drainage (arrows). Yellow fluid contained within the cyst is visible exteriorly. B. Laparoscopic closure of the base of the pedunculated fibroid (arrow) following myomectomy. C. Normal appearing, unaffected right ovary (arrow). D. Normal appearing, unaffected left ovary (arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Once the drainage was mostly completed, the suture was tied. Upon further inspection of the base of the cyst, it was noted to originate from the uterus (Fig. 2B). The ovaries were visualized bilaterally and determined to be unaffected and normal in appearance (Fig. 2C & D). The cyst wall, along with the fluid, was removed from the abdomen and sent for pathology. The final specimen measured 21.0 × 11.5 × 0.7 cm. Pathology revealed that the cyst arose from an intrauterine pedunculated smooth muscle tumor with a cavitated center. A rim of compressed tumor cells was seen at the edges of the cyst wall fragments. The solid component showed intersecting smooth muscle fascicles. The tumor showed nuclear enlargement, overlapping nuclei and mild cytologic atypia. The mitotic count was 3 per 10 high-power fields. These findings were consistent with a mitotically active cellular uterine leiomyoma with cystic degeneration.
3. Discussion
Leiomyomas, or uterine fibroids, are the most commonly diagnosed pelvic tumor in women [1]. Fibroids typically are slow growing throughout a woman's life. However, they may sometimes outgrow their blood supply, resulting in degeneration. There are various processes of fibroid degeneration. The most common is hyaline degeneration, which accounts for about 60% of all degenerating fibroids. Other types include: myxomatous, calcification, mucoid, cystic, red and fatty degeneration [3]. Cystic degeneration occurs in approximately 4% of degenerating leiomyomas.
Common imaging modalities include ultrasonography, CT scan and MRI for evaluating uterine and ovarian pathology. Depending on a patient's clinical history and presentation, one or more may be utilized in uncovering a diagnosis and deciding a treatment plan. In our case, the patient presented to the emergency room with abdominal pain and distention, so a CT scan was performed. The CT scan for our patient was highly consistent with an enlarged ovarian cyst measuring approximately 25 cm. The cyst was characterized as simple and unilocular. There were no septations, solid components, thickened walls, ascites or evidence of lymph node enlargement. As a result, no further laboratory (i.e CA-125) or imaging modalities were performed. She followed up with her gynecologist and elected for fertility-sparing surgical removal of the presumed ovarian cyst. A very important component of her visit involved counseling on the small risk of malignancy and consequences of spillage from the procedure. We recommend that all patients undergo thorough counseling before proceeding with minimally invasive management in these settings.
Our case report highlights the uncommon diagnosis and management of a pedunculated fibroid that underwent cystic degeneration presenting as an ovarian cyst. Gynecologists and radiologists should always take into account this presentation when encountering a suspected enlarged ovarian cyst or neoplasm. In our case, only CT scan was utilized for imaging. The combination of ultrasonography and MRI has proved to be more successful in correctly diagnosing cystic degeneration of fibroids. This is due to the ability to identify a stalk originating from the uterus and characteristic signal intensities seen on MRI [6]. However, despite utilization of multiple imaging modalities, the diagnosis is still frequently missed [7]. Based on presumed diagnostic suspicion for an ovarian cyst or neoplasm, exploratory laparotomy is frequently performed followed by definitive hysterectomy.
Unless there is a clear indication for exploratory laparotomy, a minimally invasive approach should be considered to further characterize the adnexal mass and if clinically appropriate, excise the mass laparoscopically. If necessary, the surgeon could then convert to laparotomy without significantly increasing operative time or morbidity. Upon review of case reports and case series of degenerating cystic pedunculated leiomyomas, exploratory laparotomy is most commonly performed as the first-line intervention, frequently followed by definitive hysterectomy. Few cases of minimally invasive approaches have been reported. There have been reports of CT-guided aspiration being used; however, this only seems to provide a temporary measure as the fluid reaccumulates. In one case, following CT-guided aspiration one year earlier, the patient returned with abdominal distention and imaging findings consistent with recurrence. She subsequently underwent exploratory laparotomy and total abdominal hysterectomy [8]. A second report concerned the use of CT-guided aspiration to successfully reduce the size of the mass so that a total laparoscopic hysterectomy could be performed outpatient [9]. Our case is the first reported in the literature of a cystic degenerating fibroid that was successfully treated with fertility-sparing laparoscopic removal. We were able to completely excise the degenerated fibroid using a single, two-centimeter port at the umbilicus. As a result, the patient was able to obtain definitive removal of the degenerating fibroid, while simultaneously avoiding a laparotomy and definitive hysterectomy.
Acknowledgments
Contributors
Christopher Walker contributed to the writing and editing of the manuscript, and collected and formatted the images.
Kaitlyn Banning contributed to the writing and editing of the manuscript.
Courtney Ritchie contributed to the writing and editing of the manuscript.
Christopher Kliethermes was responsible for patient recruitment, was the primary surgeon, and edited the manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
No funding from an external source supported the publication of this case report.
Patient Consent
Obtained.
Provenance and Peer Review
This case report was peer reviewed.
References
- 1.Steward E.A., Cookson C.L., Gandolfo R.A. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124(10):1501–1512. doi: 10.1111/1471-0528.14640. [DOI] [PubMed] [Google Scholar]
- 2.Bulun S.E. Uterine fibroids. N. Engl. J. Med. 2013;369(14):1344–1345. doi: 10.1056/NEJMra1209993. [DOI] [PubMed] [Google Scholar]
- 3.Baird D.D., Dunson D.B., Hill M.C. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am. J. Obstet. Gynecol. 2003;188(1):100–107. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 4.Steward E. Uterine fibroids. N. Engl. J. Med. 2015;372:1646–1655. doi: 10.1056/NEJMcp1411029. [DOI] [PubMed] [Google Scholar]
- 5.Persaud V., Arjoon P.D. Uterine leiomyoma. Incidence of degenerative change and a correlation of associated symptoms. Obstet. Gynecol. 1970;35(3):432–436. [PubMed] [Google Scholar]
- 6.Kubik-Huch R., Weston M., Nougaret S. European Society of Urogenital Radiology (ESUR) guidelines: MR imaging of leiomyomas. Eur. Radiol. 2018;28:3125–3137. doi: 10.1007/s00330-017-5157-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayer D., Shipilov V. Ultrasonography and magnetic resonance imaging of uterine fibroids. Obstet. Gynecol. Clin. N. Am. 1995;22:667–725. [PubMed] [Google Scholar]
- 8.Tomimatsu T., Sugihara M., Nakamura T. Massive cystic degeneration of a uterine leiomyoma in a patient with autosomal dominant polycystic kidney disease. Gynecol. Obstet. Investig. 2015;79:168–171. doi: 10.1159/000369996. [DOI] [PubMed] [Google Scholar]
- 9.Arnolds K., Senderey E., Sprague M. Giant cystic degeneration of a uterine leiomyoma in a patient with autosomal dominant polycystic kidney disease. Case Rep. Women’s Health. 2016;10:1–3. doi: 10.1016/j.crwh.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]