Abstract
BACKGROUND
Racial residential segregation is associated with higher rates of chronic hypertension, as well as greater risk of preterm birth and low birthweight. However, few studies have examined associations between segregation and hypertensive disorder of pregnancy (HDP).
METHODS
Electronic health records from 4,748 singleton births among non-Hispanic black women at Prentice Women’s Hospital in Chicago, IL (2009–2013) were geocoded to the census tract level. Residential segregation was measured using the Gi* statistic, a z-score measuring the extent to which each individual’s neighborhood composition deviates from the composition of the larger surrounding area. Segregation was categorized as low (z < 0), medium (z = 0–1.96) or high (z > 1.96). We estimated cross-sectional associations of segregation with HDP using multilevel logistic regression models with census tract random intercepts. Models adjusted for neighborhood poverty and maternal characteristics. We also examined effect modification by neighborhood poverty.
RESULTS
Overall, 27.2% of women lived in high segregation, high-poverty neighborhoods. Racial residential segregation was not associated as a main effect with HDP in models adjusting for neighborhood poverty and maternal characteristics. However, at higher levels of neighborhood poverty (>20%), women living in high- and medium-segregated neighborhoods had greater odds of HDP relative to those in low-segregation neighborhoods (P interaction: 0.002).
CONCLUSIONS
In this sample of non-Hispanic black women in Chicago, racial residential segregation was associated with greater prevalence of HDP among those living in higher poverty neighborhoods. Understanding sources of heterogeneity in the relationship between segregation and health will help refine targeted intervention efforts to reduce disparities.
Keywords: blood pressure, electronic health records, hypertension, hypertensive disorder of pregnancy, maternal health, neighborhood poverty, racial residential segregation
Hypertensive disorder of pregnancy (HDP), which affects approximately 10% of pregnancies, is an important risk factor for preterm birth, low birthweight, and perinatal mortality.1 Women with HDP are also at increased risk for developing chronic hypertension and cardiovascular disease in the future.2,3 Racial disparities in HDP exist, with non-Hispanic black women having a greater risk of developing HDP compared with women from other race/ethnic groups.4–6
Racial residential segregation, or the degree to which 2 or more racial groups live apart from one another,7 has been described as a fundamental cause of racial disparities in health outcomes.8 Segregation among African Americans as a result of discrimination in housing and lending practices has resulted in disproportionate exposure of African Americans to neighborhood disadvantage and poor physical and social environments relative to white Americans.8–12 Segregation may adversely influence health by limiting access by residents of segregated neighborhoods to health-promoting resources, limiting opportunities for economic advancement, and increasing psychosocial stress.9,10,13–15 Alternatively, living in segregated neighborhoods could be protective for health by increasing social support or reducing direct exposure to interpersonal experiences of discrimination.14,16,17
Segregation has been linked to adverse pregnancy outcomes including preterm birth and low birthweight.18–23 In addition, segregation has been found to be associated with greater risk of chronic hypertension.24,25 However, to our knowledge, only 1 prior study has examined associations between racial residential segregation and HDP.21 Grady and Ramírez found that HDP mediated the association between racial segregation and low birthweight among black women in New York City using birth certificate data.21 However, birth certificates have been found to underreport pregnancy-related medical conditions,26,27 limiting researchers’ ability to control for potential confounders and examine outcomes such as HDP. Electronic health records (EHRs), which contain more granular information on maternal health conditions than birth certificate data, are a promising data source for research examining associations of neighborhood characteristics and birth outcomes.
Our primary objective was to build on previous research by using EHR data to examine the association between racial residential segregation and HDP. Concentration of poverty in segregated neighborhoods has been noted as a particularly harmful consequence of racial residential segregation,28 but little is known regarding whether segregation and neighborhood poverty interact synergistically to increase risk of poor health outcomes.14 Thus, our second objective was to examine whether associations of segregation with HDP differed by level of neighborhood poverty.
METHODS
Study population
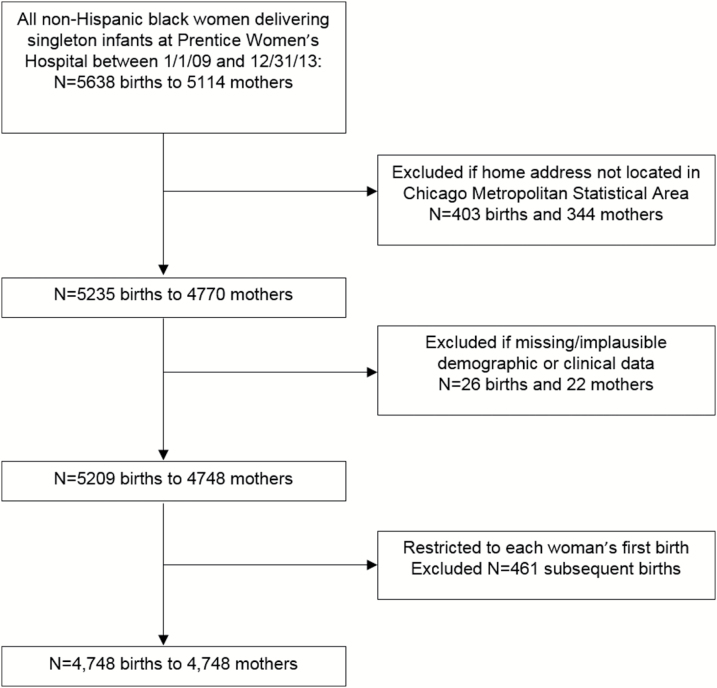
We conducted a retrospective cohort study using data from the Northwestern Medicine Enterprise Data Warehouse, a repository of EHRs. We extracted records for all non-Hispanic black women delivering singleton infants at Prentice Women’s Hospital in Chicago, IL between 1 January 2009 and 31 December 2013 (N = 5,638 births to 5,114 mothers). We used ArcMap version 10.5 (Environmental Systems Research Institute, Redlands, CA) to geocode patient addresses at the time of birth. Our sample was limited to women whose home address was located within the Chicago-Joliet-Naperville, IL-IN-WI Metropolitan Statistical Area (Chicago MSA), which included 5,235 births to 4,770 mothers. We then excluded 26 births (<1%) with missing/implausible demographic or clinical information and restricted the analysis to each woman’s first birth during the study period, for a final total of 4,748 included births (study flow chart shown in Figure 1). Mothers ranged in age from 13 to 53 years old. A total of 137 births (2.9%) were to mothers less than 18 years.
Figure 1.
Study flow diagram.
Racial residential segregation
Neighborhood-level racial residential segregation was measured using the local Getis-Ord Gi* statistic29 using 2010 US Census tracts to define neighborhoods. For each tract, the Gi* statistic outputs a z-score representing the degree to which the racial composition (i.e., percent non-Hispanic black) of that tract and its neighboring tracts differs from the mean racial composition of a larger area unit (in this case, the Chicago MSA). Tracts were considered neighboring if they shared an edge with the focal tract. Segregation was categorized as follows: low (z < 0), medium (z = 0–1.96), high (z > 1.96). At the α = 0.05 level, a Gi* value of 1.96 indicates statistically significant over-representation of black residents relative to the larger MSA, while scores near 0 indicate that the racial composition of the tract is comparable with that of the larger area and negative scores indicate a lower than expected percent of black residents. These cutoffs have been used in previous segregation studies of adverse pregnancy outcomes.20
Hypertensive disorder of pregnancy
HDP was determined using problem lists and diagnostic codes with the EHR. Women who had documentation of a diagnosis of gestational hypertension or pre-eclampsia during the included pregnancy were classified as having HDP.
Covariates
Individual-level covariates were extracted from the EHR, including age at delivery, insurance type (none, private, or public), multiparity, smoking in pregnancy, pregestational or gestational diabetes in the current pregnancy, and chronic hypertension. Neighborhood poverty was defined as the percentage of individuals within the mother’s census tract with household income below the federal poverty threshold, based on data from the 2009 to 2013 US Census American Community Survey.
Statistical analysis
Distributions of maternal and geographic characteristics were examined by level of racial residential segregation using means and SDs for continuous variables and proportions for categorical variables. We used multivariable multilevel logistic regression to estimate odds ratios of HDP associated with racial residential segregation category (high vs. low, medium vs. low). Models included random intercepts for census tracts to reflect clustering of mothers within neighborhoods. Models were first adjusted for neighborhood poverty and maternal age at delivery. Subsequent models were additionally adjusted for insurance type, smoking during pregnancy, pregestational diabetes, gestational diabetes, and chronic hypertension. To examine potential effect modification of the association between segregation and HDP by neighborhood poverty, we included an interaction term between segregation and neighborhood poverty in a second set of models. We plotted odds ratios of HDP comparing women in high- and medium-segregated neighborhoods to low-segregated neighborhoods across levels of neighborhood poverty. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Out of 4,748 women included in this study, 62.7% lived in a highly segregated neighborhood, 16.7% lived in a medium-segregated neighborhood, and 20.8% lived in a low-segregated neighborhood. Selected characteristics by neighborhood segregation level are shown in Table 1. Women in highly segregated neighborhoods were more likely to have public insurance than women in medium- or low-segregation neighborhoods. Women in highly segregated neighborhoods were more likely to be multiparous and to have pregestational diabetes than women in low- or medium-segregation areas. Highly segregated areas had a higher percent of residents below the poverty threshold (31%) compared with medium-segregation neighborhoods (25%) and low-segregation neighborhoods (15%).
Table 1.
Characteristics of African American mothers at Prentice Women’s Hospital by category of racial residential segregation, 2009–2013 (N = 4,748)
| Characteristic | High segregation N = 2,975 (62.7% of births) | Medium segregation N = 791 (16.7% of births) | Low segregation N = 982 (20.8% of births) | P valuea |
|---|---|---|---|---|
| Mother characteristics | ||||
| Age at delivery, mean (SD) | 29.3 (6.4) | 27.7 (6.4) | 27.9 (6.3) | <0.0001 |
| Insurance status, % | <0.0001 | |||
| Private | 42.8 | 45.4 | 56.5 | |
| Public | 56.5 | 53.2 | 42.8 | |
| None/self pay | 0.7 | 1.4 | 0.7 | |
| Multiparous, % | 50.2 | 47.8 | 42.9 | 0.0004 |
| Prevalent diabetes, % | 1.9 | 1.3 | 1.5 | 0.4 |
| Gestational diabetes. % | 6.1 | 4.6 | 7.2 | 0.06 |
| Smoking during pregnancy, % | 3.9 | 4.6 | 2.1 | 0.01 |
| Prevalent hypertension | 3.6 | 3.4 | 2.9 | 0.5 |
| Hypertensive disorder of pregnancy,b % | 9.4 | 9.1 | 8.6 | 0.7 |
| Geographic characteristics | ||||
| G* statistic, mean (SD)c | 4.58 (1.10) | 0.74 (0.52) | −0.90 (0.48) | <0.0001 |
| Neighborhood poverty, mean (SD)d | 0.31 (0.14) | 0.25 (0.15) | 0.15 (0.09) | <0.0001 |
a P values from chi-squared tests for categorical variables and one-way analysis of variance for continuous variables.
bDefined as gestational hypertension or pre-eclampsia.
cLevels of racial residential segregation categorized into high, medium, and low based on the value of the local Gi* statistic, which measures the deviation of the racial composition of the census tract from the larger area. Segregation levels based on a Gi* statistic z-score of less than 0, 0–1.96, and greater than 1.96, represent low, medium, and high categories, respectively.
dProportion of individuals within the census tract with household income below the federal poverty threshold based on data from the 2009 to 2013 US Census American Community Survey.
Table 2 presents the distribution of women in our analysis according to segregation category and neighborhood poverty category. The highest proportion of women lived in neighborhoods with high segregation and high neighborhood poverty (27.2%). Few women (1.0%) lived in neighborhoods with high poverty and low segregation.
Table 2.
Percentage of African American mothers at Prentice Women’s Hospital, by level of racial residential segregation and neighborhood poverty, 2009–2013 (N = 4,748)
| Segregation category,a % | Neighborhood poverty categoryb | ||
|---|---|---|---|
| High | Medium | Low | |
| High | 27.2 | 22.3 | 13.2 |
| Medium | 5.2 | 4.8 | 6.7 |
| Low | 1.0 | 6.3 | 13.4 |
aLevels of racial residential segregation categorized into high, medium, and low based on the value of the local Gi* statistic, which measures the deviation of the racial composition of the census tract from the larger area. Segregation levels based on a Gi* statistic z-score of less than 0, 0–1.96, and greater than 1.96, represent low, medium, and high categories, respectively.
bLevels of neighborhood poverty categorized into high, medium, and low based on tertiles of the percentage of neighborhood residents living in poverty.
In models adjusted for maternal age at delivery and neighborhood poverty, racial residential segregation was not associated with significantly higher odds of HDP (Table 3; high vs. low: odds ratio: 1.11, 95% confidence interval: 0.84–1.47; medium vs. low: odds ratio: 1.09, 95% confidence interval: 0.78–1.53). Results were unchanged after further adjustment for additional maternal characteristics.
Table 3.
Odds ratios of hypertensive disorder of pregnancya associated with racial residential segregation among African American mothers at Prentice Women’s Hospital, 2009–2013 (N = 4,748)
| Characteristic | Model 1, OR (95% CI) | Model 2, OR (95% CI) |
|---|---|---|
| Segregation category (vs. low)b | ||
| High | 1.11 (0.84–1.47) | 1.10 (0.82–1.46) |
| Medium | 1.09 (0.78–1.53) | 1.09 (0.77–1.54) |
| Neighborhood povertyc | 1.01 (0.94–1.09) | 1.01 (0.93–1.09) |
| Mother’s age at delivery | 1.02 (1.01–1.04) | 1.01 (0.99–1.03) |
| Insurance (vs. private) | ||
| None/self pay | — | 1.10 (0.33–3.63) |
| Public | — | 1.12 (0.89–1.41) |
| Multiparous | — | 0.75 (0.61–0.94) |
| Gestational diabetes | — | 1.61 (1.12–2.32) |
| Prevalent diabetes | — | 2.16 (1.22–3.84) |
| Prevalent hypertension | — | 6.17 (4.33–8.78) |
| Smoking during pregnancy | — | 0.83 (0.48–1.46) |
Abbreviations: CI, confidence interval; OR, odds ratio.
aCombined outcome including both gestational hypertension and pre-eclampsia.
bSegregation categories determined by G* statistic of mother’s census tract of residence using the following cut points: >1.96 = high segregation, 0–1.96 = medium segregation, <0 = low segregation.
cOdds ratio of hypertensive disorder of pregnancy for each 10% increase in neighborhood poverty.
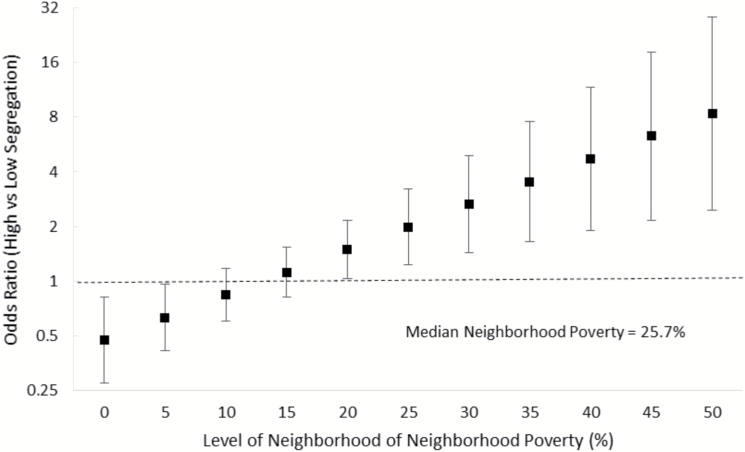
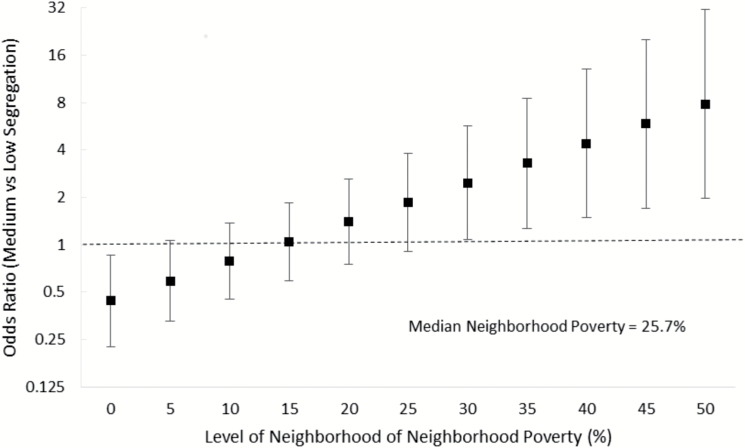
However, associations of segregation and HDP varied by level of neighborhood poverty (P interaction: 0.002). Figures 2 and 3 display the odds of HDP comparing high- and medium-segregation neighborhoods to low-segregation neighborhoods across varying levels of neighborhood poverty. At low levels of neighborhood poverty (<15%), racial residential segregation was associated with lower odds of HDP (Figures 2 and 3). This direction of the association reversed at the 20th percentile of neighborhood poverty and strengthened as neighborhood poverty percentile increased. For women in neighborhoods with the median poverty level (25.7%) or greater, medium and high segregation were associated with significantly greater odds of HDP.
Figure 2.
Association of high racial residential segregation (vs. low) with hypertensive disorder of pregnancy across levels of neighborhood poverty.
Figure 3.
Association of medium racial residential segregation (vs. low) with hypertensive disorder of pregnancy across levels of neighborhood poverty.
DISCUSSION
In this analysis of EHR data, we found that racial residential segregation was associated with higher odds of HDP in areas with higher neighborhood poverty rates only. While prior studies of segregation and birth outcomes have not focused on HDP as an outcome, prior research suggests that segregation is associated with greater risk of preterm birth and low birthweight.18–23 Our results, as well as those from a previous study among women in New York City that examined HDP as a mediator for the association of segregation and low birthweight,21 suggest HDP as a pathway through which segregation may influence disparities in other adverse pregnancy outcomes (e.g., preterm birth). In addition, as HDP is associated with increased risk that a woman develops chronic hypertension later in life,2,3 this outcome has important implications for racial disparities in cardiovascular disease.
In our study, segregation was associated with lower odds of HDP in lower poverty neighborhoods and higher odds of HDP in higher poverty neighborhoods. Neighborhoods with both high levels of segregation and poverty may lack access to health-promoting amenities such as grocery stores and health care providers.30,31 In addition, these neighborhoods may have higher rates of psychosocial stressors such as crime.32–34 The “weathering hypothesis” suggests that repeated exposures to adverse social and economic conditions result in chronic dysregulation of the immune and neuroendocrine systems, which may contribute to deterioration in health among African American women in early and midadulthood.35 This process may be related to development of hypertension, both chronic and during pregnancy, through inflammation and endothelial dysfunction.36,37 Supporting this idea, prior studies have found neighborhood crime38 and physical disorder (e.g., graffiti, trash, abandoned buildings)39,40 to be associated with greater likelihood of HDP.
In contrast, some aspects of segregation have been hypothesized to have a protective effect through increasing social support among black communities.14,16,17 Several prior studies have found protective association of elements of segregation with birth outcomes. For example, Bell et al.16 reported risk of preterm birth and low birthweight to be reduced with clustering of predominantly black neighborhoods, which may enhance social support and social networks. In addition, Pickett et al.17 found that African American women living in Chicago census tracts that were both predominantly African American, and wealthier relative to tracts lived in by other women with comparable educational attainment, had lower rates of preterm birth. In this context, our results suggest that the adverse influence of segregation on HDP may be magnified in the presence of neighborhood poverty but that more highly segregated neighborhoods may have health-promoting aspects if they are of low poverty. However, more research in this area is needed.
The use of EHR data is a strength of this study, as EHRs are more reliable than birth certificates to capture the presence of HDP and potential confounding covariates such as maternal conditions. However, this study was also subject to several limitations. First, the study was conducted in 1 urban hospital and may not generalize to all populations. Second, EHR data are still limited in terms of the variables captured, as these systems were designed for clinical practice as opposed to research. The EHR did not contain information on health behaviors like diet and physical activity that may mediate associations of segregation with HDP. As maternal body mass index and gestational weight gain were missing for a large proportion of women, we could not include this variable in the analysis. The EHR also did not contain information on mothers’ marital status, employment status, or education. In addition, while we controlled for chronic hypertension as a covariate in an attempt to distinguish HDP from prevalent hypertension preceding the pregnancy, it is possible that some women classified as having HDP actually had pre-existing undiagnosed chronic hypertension. Also, we lacked information on pregnancies that had been terminated due to HDP. Finally, we defined segregation based on women’s addresses at the time of delivery. However, we were unable to account for how long women had lived at that address.
Racial residential segregation was associated with higher odds of HDP among non-Hispanic black women living in neighborhoods with a greater percentage of residents living below the poverty threshold. Understanding sources of heterogeneity in the relationship between segregation and health will help refine targeted intervention efforts to reduce disparities.
DISCLOSURE
The author(s) declared no conflict of interest.
ACKNOWLEDGMENTS
This research was supported by an NHLBI Training Grant in Cardiovascular Epidemiology and Prevention (T32HL069771).
REFERENCES
- 1. Lo JO, Mission JF, Caughey AB. Hypertensive disease of pregnancy and maternal mortality. Curr Opin Obstet Gynecol 2013; 25:124–132. [DOI] [PubMed] [Google Scholar]
- 2. McDonald EG, Dayan N, Pelletier R, Eisenberg MJ, Pilote L. Premature cardiovascular disease following a history of hypertensive disorder of pregnancy. Int J Cardiol 2016; 219:9–13. [DOI] [PubMed] [Google Scholar]
- 3. Valdiviezo C, Garovic VD, Ouyang P. Preeclampsia and hypertensive disease in pregnancy: their contributions to cardiovascular risk. Clin Cardiol 2012; 35:160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ghosh G, Grewal J, Männistö T, Mendola P, Chen Z, Xie Y, Laughon SK. Racial/ethnic differences in pregnancy-related hypertensive disease in nulliparous women. Ethn Dis 2014; 24:283–289. [PMC free article] [PubMed] [Google Scholar]
- 5. Miranda ML, Swamy GK, Edwards S, Maxson P, Gelfand A, James S. Disparities in maternal hypertension and pregnancy outcomes: evidence from North Carolina, 1994–2003. Public Health Rep 2010; 125:579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shen JJ, Tymkow C, MacMullen N. Disparities in maternal outcomes among four ethnic populations. Ethn Dis 2005; 15:492–497. [PubMed] [Google Scholar]
- 7. Massey DS, Denton NA. The dimensions of residential segregation. Soc Forces 1988; 67:281–315. [Google Scholar]
- 8. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 2001; 116:404–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Borrell LN, Kiefe CI, Diez-Roux AV, Williams DR, Gordon-Larsen P. Racial discrimination, racial/ethnic segregation, and health behaviors in the CARDIA study. Ethn Health 2013; 18:227–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Landrine H, Corral I. Separate and unequal: residential segregation and black health disparities. Ethn Dis 2009; 19:179–184. [PubMed] [Google Scholar]
- 11. Massey DS, Fischer MJ. How segregation concentrates poverty. Ethn Racial Stud 2000; 23:670–691. [Google Scholar]
- 12. Nuru-Jeter AM, LaVeist TA. Racial segregation, income inequality, and mortality in US metropolitan areas. J Urban Health 2011; 88:270–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bahr PR. Race and nutrition: an investigation of Black-White differences in health-related nutritional behaviours. Sociol Health Illn 2007; 29:831–856. [DOI] [PubMed] [Google Scholar]
- 14. Kramer MR, Hogue CR. Is segregation bad for your health?Epidemiol Rev 2009; 31:178–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schulz AJ, Kannan S, Dvonch JT, Israel BA, Allen A III, James SA, House JS, Lepkowski J. Social and physical environments and disparities in risk for cardiovascular disease: the healthy environments partnership conceptual model. Environ Health Perspect 2005; 113:1817–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med 2006; 63:3030–3045. [DOI] [PubMed] [Google Scholar]
- 17. Pickett KE, Collins JW Jr, Masi CM, Wilkinson RG. The effects of racial density and income incongruity on pregnancy outcomes. Soc Sci Med 2005; 60:2229–2238. [DOI] [PubMed] [Google Scholar]
- 18. Masi CM, Hawkley LC, Piotrowski ZH, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc Sci Med 2007; 65:2440–2457. [DOI] [PubMed] [Google Scholar]
- 19. Mehra R, Boyd LM, Ickovics JR. Racial residential segregation and adverse birth outcomes: a systematic review and meta-analysis. Soc Sci Med 2017; 191:237–250. [DOI] [PubMed] [Google Scholar]
- 20. Salow A, Pool LR, Grobman WA, Kershaw KN. Association of neighborhood-level racial residential segregation with adverse pregnancy outcomes. Am J Obstet Gynecol 2018; 218:S69–S69. [DOI] [PubMed] [Google Scholar]
- 21. Grady SC, Ramírez IJ. Mediating medical risk factors in the residential segregation and low birthweight relationship by race in New York City. Health Place 2008; 14:661–677. [DOI] [PubMed] [Google Scholar]
- 22. Ncube CN, Enquobahrie DA, Albert SM, Herrick AL, Burke JG. Association of neighborhood context with offspring risk of preterm birth and low birthweight: a systematic review and meta-analysis of population-based studies. Soc Sci Med 2016; 153:156–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Culhane JF, Elo IT. Neighborhood context and reproductive health. Am J Obstet Gynecol 2005; 192:S22–S29. [DOI] [PubMed] [Google Scholar]
- 24. Kershaw KN, Albrecht SS. Racial/ethnic residential segregation and cardiovascular disease risk. Curr Cardiovasc Risk 2015; 9:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and black-white disparities in hypertension. Am J Epidemiol 2011; 174:537–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Reichman NE, Hade EM. Validation of birth certificate data. A study of women in New Jersey’s HealthStart program. Ann Epidemiol 2001; 11:186–193. [DOI] [PubMed] [Google Scholar]
- 27. Roohan PJ, Josberger RE, Acar J, Dabir P, Feder HM, Gagliano PJ. Validation of birth certificate data in New York State. J Community Health 2003; 28:335–346. [DOI] [PubMed] [Google Scholar]
- 28. Massey DS. American apartheid: segregation and the making of the underclass. Am J Sociol 1990; 96:329–357. [Google Scholar]
- 29. Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geogr Anal 1992; 24:189–206. [Google Scholar]
- 30. Bower KM, Thorpe RJ Jr, Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med 2014; 58:33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gaskin DJ, Dinwiddie GY, Chan KS, McCleary RR. Residential segregation and the availability of primary care physicians. Health Serv Res 2012; 47:2353–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Peterson RD, Krivo LJ. Racial segregation, the concentration of disadvantage, and black and white homicide victimization. Sociol Forum 1999; 14:465–493. [Google Scholar]
- 33. Velez MB, Krivo LJ, Peterson RD. Structural inequality and homicide: an assessment of the black-white gap in killings. Criminology 2003; 41:645–672. [Google Scholar]
- 34. O’Flaherty B, Sethi R. Crime and segregation. J Econ Behav Organ 2007; 64:391–405. [Google Scholar]
- 35. Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health 2006; 96:826–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med 1993; 153:2093–2101. [PubMed] [Google Scholar]
- 37. Pickering TG. Stress, inflammation, and hypertension. J Clin Hypertens (Greenwich) 2007; 9:567–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mayne SL, Pool LR, Grobman WA, Kershaw KN. Associations of neighbourhood crime with adverse pregnancy outcomes among women in Chicago: analysis of electronic health records from 2009 to 2013. J Epidemiol Community Health 2018; 72:230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Messer LC, Vinikoor-Imler LC, Laraia BA. Conceptualizing neighborhood space: consistency and variation of associations for neighborhood factors and pregnancy health across multiple neighborhood units. Health Place 2012; 18:805–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vinikoor-Imler LC, Messer LC, Evenson KR, Laraia BA. Neighborhood conditions are associated with maternal health behaviors and pregnancy outcomes. Soc Sci Med 2011; 73:1302–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]