Abstract
Background
Effective treatments are available for patients with inflammatory bowel disease (IBD); however, suboptimal outcomes occur and are often linked to patients’ limited disease knowledge. The aim of this analysis was to determine if delivery of educational messages through a telemedicine system improves IBD knowledge.
Methods
TELEmedicine for Patients with IBD (TELE-IBD) was a randomized controlled trial with visits at baseline, 6 months, and 12 months; patient knowledge was a secondary aim of the study. Patients were randomized to receive TELE-IBD every other week (EOW), weekly (TELE-IBD W), or standard of care. Knowledge was assessed at each visit with the Crohn’s and Colitis Knowledge (CCKNOW) survey. The primary outcome was change in CCKNOW score over 1 year compared between the TELE-IBD and control groups.
Results
This analysis included 219 participants. Participants in the TELE-IBD arms had a greater improvement in CCKNOW score compared with standard care (TELE-IBD EOW +2.4 vs standard care +1.8, P = 0.03; TELE-IBD W +2.0 vs standard care +1.8, P = 0.35). Participants with lower baseline CCKNOW scores had a greater change in their score over time (P < 0.01). However, after adjusting for race, site, and baseline knowledge, there was no difference in CCKNOW score change between the control and telemedicine arms.
Conclusions
Telemedicine improves IBD-specific knowledge through text messaging, although the improvement is not additive with greater frequency of text messages. However, after adjustment for confounding variables, telemedicine is not superior to education given through standard visits at referral centers. Further research is needed to determine if revised systems with different modes of delivery and/or frequency of messages improve disease knowledge.
Keywords: inflammatory bowel disease, health education, patient medical knowledge, telemedicine, text message
INTRODUCTION
Inflammatory bowel disease (IBD), comprised of ulcerative colitis (UC) and Crohn’s Disease (CD), is a chronic condition of the gastrointestinal (GI) tract and affects up to 1.6 million people in the United States.1 Although symptoms vary among patients, abdominal cramping, diarrhea, and GI bleeding are very common.2, 3 Symptoms tend to occur together in “flares” and are followed by symptom-free periods.3 Although effective treatments are available, suboptimal outcomes continue to occur with treatment and have been linked to many factors including patients’ limited knowledge of their disease.4
A number of studies have shown that patients are not knowledgeable about their IBD and that patients are dissatisfied with their lack of knowledge.4–11 For example, patients with IBD are generally unaware of their risks of colorectal cancer (CRC), although patients with UC have a better knowledge of this risk than patients with CD.7, 8 Many groups have explored the benefits of educational interventions on patient knowledge, including prior studies of workshops, lectures, handbooks, group sessions, and face-to-face instruction.12–17 One of the first studies, done across 9 communities in the United States, offered workshops with associated questionnaires and face-to-face sessions with patients and their families.4 Although less than 10% of participants completed all questionnaires, significant improvements were demonstrated in participants’ IBD knowledge, which were maintained for at least 3 months. Higher knowledge scores on validated IBD questionnaires have been associated with adaptive coping strategies,18, 19 patient satisfaction, and lower rates of medication nonadherence.20
More recently, telemedicine systems have been used to deliver education to IBD patients, with some success.21, 22 The primary aim of this secondary analysis was to determine if delivery of educational messages through a mobile telemedicine system for IBD can effectively improve patients’ disease-specific knowledge. We compared disease-specific knowledge of IBD over 1 year in patients receiving either standard care or 1 of 2 telemedicine interventions. We hypothesized that delivery of educational messages through a telemedicine system would improve patients’ knowledge of their disease over time and that higher frequency of interactions with the telemedicine system would augment that improvement.
METHODS
Study Design
Our study analyzed a secondary aim of the larger, previously described TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD) trial.23 Participants were enrolled in a multicenter, randomized controlled trial conducted over 1 year. Enrollment occurred from 2013 to 2015, with the last participant visit conducted in September 2016. There were 2 intervention arms, weekly telemedicine (TELE-IBD W) and biweekly telemedicine (TELE-IBD EOW), and a standard care arm. Participants completed a self-assessment of symptoms and side effects and measured body weight weekly or every other week in the TELE-IBD W and TELE-IBD EOW arms, respectively. However, participants received more frequent educational messages. In the TELE-IBD W arm, participants received 2 educational text messages per week, whereas in the TELE-IBD EOW arm, participants received 1 educational text message per week. In the standard care arm, participants received educational materials at clinic appointments at the discretion of their provider. Participants had disease knowledge assessed at the baseline and 6-month and12-month visits.
Study Setting
Patients were recruited from 3 IBD referral centers, University of Maryland (UM), University of Pittsburgh Medical Center (UPMC), and Vanderbilt University (VU).
Study Participants—Inclusion Criteria
Patients were included in the study if diagnosed with IBD based on the usual criteria,24 if they experienced at least 1 flare of IBD in the last 2 years, defined as IBD symptoms warranting a change in current medical therapy, and if they were aged 18 years or older.
Study Participants—Exclusion Criteria
Patients who met any of the following criteria were excluded from the study: Inability to communicate in English, inability to comply with the study as determined by investigators, GI surgeries that may preclude the ability to accurately calculate bowel movements (ileostomy, colostomy, ileoanal pouch anastomosis, or ileorectal anastomosis), pending or imminent surgery, history of short bowel syndrome, uncontrolled medical or psychiatric disease, or pregnancy.
TELE-IBD Intervention
The TELE-IBD trial has previously been described in detail.23 Briefly, the TELE-IBD system consists of a mobile telephone for participants and a web-based platform for providers and research staff. The system was developed by the UM IBD Program and CircleLink Health, LLC. Interaction between patients, TELE-IBD, and research staff was facilitated through text messages driven by a decision support server.
TELE-IBD Educational Intervention
An educational curriculum was developed based on materials from the Crohn’s and Colitis Foundation. Participants randomized to TELE-IBD W received 2 educational text messages per week, whereas participants randomized to TELE-IBD EOW received 1 message per week. Examples of text messages delivered to participants are shown in Figure 1. Participants in both intervention arms received the same message content, but the frequency of text messages between intervention arms differed, as previously described. Additional “pragmatic” educational messages were sent periodically to all participants in the intervention groups at the discretion of the principal investigator (R.K.C.). The standard care arm did not receive educational text messages but instead received educational materials at the time of routine clinic visits at the discretion of their provider.
FIGURE 1.
Examples of educational messages delivered to participants with the TELE-IBD system.
Data Collection
Study visits were completed at baseline, 6 months, and 12 months. Routine clinic visits were continued without interruption. Demographic and clinical characteristics were assessed at the baseline visit. Disease activity in participants with CD was assessed with the Harvey Bradshaw Index (HBI), with a cutoff value of 5 or higher indicating active disease.25 UC participant disease activity was measured with the Simple Clinical Colitis Activity Index (SCCAI), with a cutoff value of 3 or higher indicating active disease.26 Locus of control (LOC) was measured by Rotter’s LOC scale, also known as the I-E scale.27 LOC refers to an individual’s perception of who or what is responsible for events that happen to them. Those with an external locus of control perceive that events that occur are driven by circumstances outside of their control, whereas those with an internal locus of control believe that they are personally responsible (through effort, skills, and abilities) for important events that occur in their lives. Self-efficacy, defined as one’s ability to accomplish a task, was measured with the general self-efficacy (GSE) scale.28, 29 Higher GSE scores are associated with increased confidence in one’s ability to accomplish a given task.
Assignment of Exposure
Participants were randomly assigned 1:1:1 at the baseline study visit to either receive 2 weekly educational text messages, 1 weekly educational text message, or no educational text messages.
Assessment of Outcome
Participant knowledge was assessed with the Crohn’s and Colitis Knowledge (CCKNOW) survey; the CCKNOW is a 30-item questionnaire, with 1 point given for each correct answer. A total of 24 questions are used to calculate a final score, ranging from 0 to 24.5 The outcome was defined as the difference in CCKNOW score between baseline and the 12-month study visit.
Statistical Methods
Baseline demographic and disease-related data for each exposure group were compared. The outcome (knowledge score difference between baseline and 12-month visit) was analyzed as a continuous variable, with a range from 0 to 24. Knowledge gain or loss over time was assessed between groups using a standard t test. Potential covariates that may predict the outcome were identified a priori. These included demographic characteristics such as age, race, and insurance status, and disease-related characteristics, like baseline disease activity and disease duration. These were compared between groups defined by the assigned exposure and the measured outcome. One-way analysis of variance (ANOVA) and Pearson’s chi-square were used to compare covariate distributions between exposure and outcome groups. To assess for effect measure modification, stratum-specific estimates from 1-way ANOVA were compared for qualitative differences between strata. We assessed for confounding by individually adjusting for each covariate in a linear regression model, with educational messages as the independent variable and change in CCKNOW score as the dependent variable. Percent changes in beta coefficient estimates were calculated with a value of 10% being used as the threshold for significance.
Ethical Considerations
The study was approved by the UM Human Research Protection Office, UPMC Office of Research, and VU Human Research Protection Program. A Data Safety and Monitoring Board (DSMB) was created to monitor adherence to all protocols, consistent with National Institutes of Health (NIH) guidelines.
RESULTS
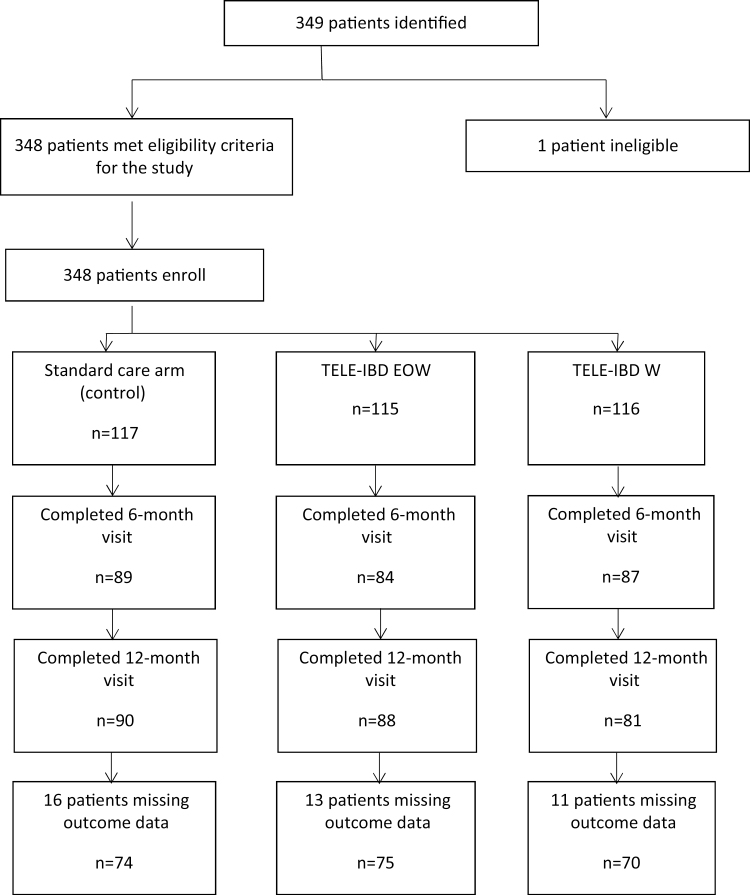
Three hundred forty-eight patients were enrolled in the trial. Forty-eight patients withdrew from the study, 10 from the standard care arm, 16 from the TELE-IBD EOW, and 22 from TELE-IBD W. Because participants without a completed CCKNOW survey at baseline and 12 months were excluded, we assessed a total of 219 patients (Fig. 2).
FIGURE 2.
Participant flow in the TELE-IBD trial.
Demographic and Clinical Characteristics of Participants in the TELE-IBD Trial
Participant demographic and disease-related characteristics are summarized in Table 1. Among all participants, mean age at enrollment was 38.5 ± 12.3 years, 92% were white, and 58% were women. The majority of the participants were enrolled at UM (n = 121), followed by UPMC (n = 69) and VU (n = 29). A little over half the patients (n = 120) had commercial insurance. Forty-four percent of the patients (n = 96) had active disease at the baseline visit. Demographics and clinical characteristics, including age, race, and disease activity at baseline, were not significantly different among exposure groups for all enrolled patients at baseline (n = 348). However, when analyzing only the 219 patients with CCKNOW scores at baseline and the 12-month visit, there were significant differences in age (P < 0.01), race (P = 0.04) and disease activity (P = 0.01) among the arms, whereas other demographics and disease-related covariates did not differ significantly. Twelve percent of the patients in the standard care arm were not white (n = 9), compared with 5% (n = 4) and 6% (n = 4) in the TELE-IBD EOW and W arms, respectively (P = 0.04). A larger number of patients had active disease at the baseline study visit in the standard care arm (n = 40, 54%) compared with TELE-IBD EOW (n = 31, 41%) and TELE-IBD W (n = 25, 36%; P = 0.01).
TABLE 1:
Demographic and Clinical Characteristics of Participants Enrolled in the TELE-IBD Trial With a Baseline and 12-Month CCKNOW Score
| Variable | Overall (n = 219) | Standard Care (n = 74) | Once Weekly Message (n = 75) | Twice Weekly Messages (n = 70) |
|---|---|---|---|---|
| Age, mean ± SD* | 38.5 ± 12.3 | 39.2 ± 12.1 | 39.5 ± 13.4 | 36.9 ± 11.2 |
| Sex, No. (%) | ||||
| Male | 93 (42) | 32 (43) | 30 (40) | 31 (44) |
| Female | 126 (58) | 42 (57) | 45 (60) | 39 (56) |
| Race, No. (%)* | ||||
| White | 202 (92) | 65 (88) | 71 (95) | 66 (94) |
| Other | 17 (8) | 9 (12) | 4 (5) | 4 (6) |
| Baseline knowledge, mean ± SD | 12.6 ± 4.4 | 12.4 ± 4.4 | 12.8 ± 4.9 | 12.5 ± 3.8 |
| Rotter’s locus of control, mean ± SD | 9.9 ± 3.8 | 9.9 ± 3.9 | 9.8 ± 3.9 | 10.1 ± 3.5 |
| General self-efficacy score, mean ± SD | 32.2 ± 4.0 | 32.1 ± 3.9 | 32.3 ± 4.3 | 32.1 ± 3.7 |
| MHI-5 score, mean ± SD | 74.7 ± 17.4 | 73.9 ± 17.9 | 75.4 ± 18.0 | 74.9 ± 16.2 |
| Site, No. (%) | ||||
| UM | 121 (55) | 38 (51) | 44 (59) | 39 (56) |
| UPMC | 69 (32) | 24 (32) | 21 (28) | 24 (34) |
| VU | 29 (13) | 12 (17) | 10 (13) | 7 (10) |
| Insurance status, No. (%) | ||||
| Commercial | 120 (55) | 38 (51) | 45 (60) | 37 (53) |
| Other | 99 (45) | 36 (49) | 30 (40) | 33 (47) |
| Disease activity, No. (%)* | ||||
| Remission | 123 (56) | 34 (46) | 44 (59) | 45 (64) |
| Active disease | 96 (44) | 40 (54) | 31 (41) | 25 (36) |
Locus of control was measured by Rotter’s LOC scale. Self-efficacy was measured by the GSE. Mental health was measured using the mental health inventory-5 subscale of the short form-36. Disease activity was measured by the HBI for patients with CD, and the SCCAI for patients with UC.
*P value between groups is less than 0.05.
Association of Frequency of Educational Messages With Change in CCKNOW Scores
Differences of crude associations between number of weekly educational messages and change in knowledge score are shown in the first column of Table 2. Patients in both intervention arms had improvements in knowledge scores (+2.4 in TELE-IBD EOW, +2.0 in TELE-IBD W) when compared with standard care (+1.8; P = 0.03 for TELE-EOW vs standard care and P = 0.35 for TELE-W vs standard care).
TABLE 2:
Unadjusted and Adjusted Values of CCKNOW Score Change After Controlling for Race, Site, and Baseline Knowledge
| Variable | CCKNOW Mean Difference, Mean, SD | Adjusted Estimate, Beta Coefficient, SE | P After Adjustment |
|---|---|---|---|
| Education | |||
| Standard care | 0.0 | 0.0 (ref) | |
| Once-weekly messages | +0.6, 0.5 | +0.66, 0.45 | 0.15 |
| Twice-weekly messages | +0.2, 0.5 | +0.20, 0.46 | 0.67 |
| Race | |||
| White | +2.1, 0.7 | +2.5, 0.73 | <0.01 |
| Other | 0.0 | 0.0 (ref) | |
| Site | |||
| UMB | 0.0 | 0.0 (ref) | |
| UPMC | +0.6, 0.4 | +0.51, 0.43 | 0.24 |
| VU | +2.1, 0.7 | +1.9, 0.57 | <0.01 |
| Baseline knowledge | |||
| 0–7 | +3.1, 0.7 | +3.3, 0.63 | <0.01 |
| 8–15 | +1.8, 0.4 | +2.0, 0.43 | <0.01 |
| 16–24 | 0.0 | 0.0 (ref) | |
There were significant differences in change in mean CCKNOW scores among strata of disease-related covariates (Table 2). Specifically, patients with lower baseline CCKNOW scores had greater improvement in the CCKNOW score over the course of the study (P < 0.01). Patients whose baseline score was in the lowest tertile experienced a gain of +3.7 points, compared with +2.4 for those in the middle tertile and 0.6 for those in the highest tertile. CCKNOW score change also varied significantly across study sites (P < 0.01), with participants from VU having the greatest improvement in knowledge score (+3.7 points), followed by UPMC (+2.2 points) and UM (+1.6 points). Participants of different races had significantly different changes in CCKNOW scores (P < 0.01), with white patients having a mean gain of +2.2 points and other races having a mean gain of +0.1 points.
Assessment for Effect Measure Modification and Confounding
Age, race, insurance type, and disease duration were found to be potential effect measure modifiers in the twice-weekly message exposure level when compared with standard care. However, there were no effect measure modifiers in the once-weekly message level. No effect measure modifiers were found to change the association in both exposure levels, and as such, no effect measure modifiers were included in the final model.
Race, site, and baseline knowledge were all potential confounders due to their change of the association between exposure and outcome and were subsequently included in the final model (Table 2). After adjusting for race, site, and baseline knowledge, once-weekly text messages to participants over 1 year were associated with an increase in CCKNOW score by 0.66, and twice-weekly text messages to participants over 1 year were associated with an increase in CCKNOW score by 0.20. Neither of these differences was statistically significant (P = 0.15 and P = 0.67, respectively).
DISCUSSION
Participants from the TELE-IBD study with at least a baseline and 12-month CCKNOW score experienced modest increases in disease-specific knowledge. Participants that received once- or twice-weekly educational messages experienced a numerical increase in knowledge scores compared with standard care participants; however, the difference was not significant after adjustment for likely confounders. Participants with lower baseline CCKNOW scores had a greater change in their knowledge score over time. The estimates of differences in change in CCKNOW score over time between the telemedicine and standard care arms after adjusting for race, site, and baseline knowledge remained nearly the same, although the differences were no longer statistically significant (standard care vs once-weekly messages +0.66, P = 0.15; standard care vs twice-weekly messages +0.20, P = 0.67).
The observed improvement of CCKNOW score in the education groups is consistent with findings from prior studies.6, 13, 30 Eaden et al.5 noted that patients who received an IBD guidebook showed better knowledge of their UC at 1 month compared with controls, an effect that was maintained after 9 months. A 3-hour workshop done across 9 communities in the United States open to IBD patients and their families increased CCKNOW score by 4 points, an improvement that was maintained when patients were resurveyed 3 months later.4 An educational curriculum in a telemedicine-driven pilot program for a small group of patients with UC showed improvement of CCKNOW scores from 9 to 12.21 Although most increases in CCKNOW score after formal educational interventions are on the order of 1.5–3 points,4, 12, 13, 19 patients enrolled in a randomized controlled trial by Waters et al.31 reported a greater increase of 8 points compared with a 4-point increase in controls. In that particular study, the investigators evaluated the effects of ad hoc physician education over 8 weeks as opposed to written educational materials or a formal curriculum. A clinically important improvement in disease-specific knowledge is difficult to ascertain, although a college education increases mean CCKNOW score by about 3 points.30 Our study demonstrated increases in disease-specific knowledge similar to prior studies, albeit with more frequent interactions with trial participants. To put this change in knowledge over time in a clinical context, participants across all 3 groups at baseline answered 12 questions out of 24 correctly; after frequent educational messages over 1 year, participants answered 2 more questions correctly on average.
This study has a number of strengths. Our sample size was large, and the study design was a randomized controlled trial. To our knowledge, this is the first randomized trial to evaluate a formal educational curriculum using a text messaging platform. With almost 3 billion people around the world using a mobile phone,32 use of text messaging taps into technology that is widely available, easily accessible, and requires minimal or no training to use. One limitation of our study is that all the patients came from IBD referral centers led by experts in the field. These patients may not be representative of the general IBD population; their disease may be more difficult to treat, and their derived benefit from the intervention may not be generalizable to patients in the community. Additionally, due to the nature of these IBD referral centers, the “standard care” arm may not be representative of an IBD patient’s usual care in the community. The referral centers in the study incorporate trainees, midlevel providers, nurse coordinators, social workers, psychologists, and sometimes patient volunteers in the care of their patients with IBD. All of these additional team members interacting with the participant may diminish the true effect of the educational intervention arms. Also, as trainees, midlevel providers, and other staff members often obtain a history and complete documentation of the visit, the attending physician is able to spend more time teaching and educating the patient than what is possible in other settings. Despite these possible advantages, participants at baseline only answered 50% of questions correctly, suggesting that participant knowledge of disease is limited. Another potential limitation is the incomplete assessment of disease knowledge at baseline and follow-up for participants. This could have introduced bias, although we do not suspect that the bias would be differential. As a result of a lower sample size, there were some differences in participant characteristics at baseline; however, these variables were either not associated with the outcome or were adjusted for in the multivariate analysis.
How should our results be interpreted? It is possible that delivery of educational messages via text message does not improve disease knowledge in patients with IBD. This seems to be the case at least in IBD referral centers that have multidisciplinary teams in place to assist in the care of patients. Whether education via text messaging is effective in other settings is speculative. It is also possible that education is effective but that the effect of the intervention is not reflected in the knowledge survey used in this study. Further research is needed to determine if improved and/or up-to-date surveys are needed to assess patients’ disease-specific knowledge. Furthermore, research is needed to define a meaningful change in disease knowledge. The study team is currently performing qualitative interviews on participants from the TELE-IBD trial to determine the participants’ perspective on the educational intervention, including the mode and frequency of delivery of the messages. Our results suggest that a number of baseline factors are important to consider before considering an educational intervention including low baseline knowledge. Thus, it is plausible that targeting patients with low IBD understanding may improve the effect of the intervention on disease knowledge.
In summary, telemedicine interventions can improve patients’ disease-specific knowledge of IBD through text messaging, although the improvement is not additive with greater frequency of text messages. Patients who have lower baseline knowledge about their disease demonstrate the greatest improvement from this intervention. However, when adjusting for possible confounding variables, educational messages delivered via text messaging did not improve disease-specific knowledge compared with standard care provided at IBD referral centers. Further research is needed to assess the effect of similar interventions outside of referral centers and to determine if other survey instruments are needed to measure disease-specific knowledge.
Conflicts of interest: None.
Supported by: the Agency for Healthcare Research and Quality (1R01HS018975-01A1) and the University of Maryland General Clinical Research Centers Program. Ameer Abutaleb and Kenechukwu Chudy-Onwugaje were supported by T32 training grant DK067872.
REFERENCES
- 1. Molodecky NA, Soon IS, Rabi DM, et al. . Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.e42; quiz e30. [DOI] [PubMed] [Google Scholar]
- 2. Mahadev S, Young JM, Selby W, et al. . Quality of life in perianal Crohn’s disease: what do patients consider important?Dis Colon Rectum. 2011;54:579–585. [DOI] [PubMed] [Google Scholar]
- 3. Romberg-Camps MJ, Bol Y, Dagnelie PC, et al. . Fatigue and health-related quality of life in inflammatory bowel disease: results from a population-based study in the Netherlands: the IBD-South Limburg cohort. Inflamm Bowel Dis. 2010;16:2137–2147. [DOI] [PubMed] [Google Scholar]
- 4. Quan H, Present JW, Sutherland LR. Evaluation of educational programs in inflammatory bowel disease. Inflamm Bowel Dis. 2003;9:356–362. [DOI] [PubMed] [Google Scholar]
- 5. Eaden JA, Abrams K, Mayberry JF. The Crohn’s and colitis knowledge score: a test for measuring patient knowledge in inflammatory bowel disease. Am J Gastroenterol. 1999;94:3560–3566. [DOI] [PubMed] [Google Scholar]
- 6. Butcher RO, Law TL, Prudham RC, et al. . Patient knowledge in inflammatory bowel disease: CCKNOW, how much do they know?Inflamm Bowel Dis. 2011;17:E131–E132. [DOI] [PubMed] [Google Scholar]
- 7. Baars JE, Siegel CA, van’t Spijker A, et al. . Inflammatory bowel disease-patients are insufficiently educated about the basic characteristics of their disease and the associated risk of colorectal cancer. Dig Liver Dis. 2010;42:777–784. [DOI] [PubMed] [Google Scholar]
- 8. Lopez A, Collet-Fenetrier B, Belle A, et al. . Patients’ knowledge and fear of colorectal cancer risk in inflammatory bowel disease. J Dig Dis. 2016;17:383–391. [DOI] [PubMed] [Google Scholar]
- 9. Gumidyala AP, Plevinsky JM, Poulopoulos N, et al. . What teens do not know can hurt them: an assessment of disease knowledge in adolescents and young adults with IBD. Inflamm Bowel Dis. 2017;23:89–96. [DOI] [PubMed] [Google Scholar]
- 10. Bernstein KI, Promislow S, Carr R, et al. . Information needs and preferences of recently diagnosed patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:590–598. [DOI] [PubMed] [Google Scholar]
- 11. Selinger CP, Carbery I, Warren V, et al. . The relationship between different information sources and disease-related patient knowledge and anxiety in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2017;45:63–74. [DOI] [PubMed] [Google Scholar]
- 12. Kennedy A, Robinson A, Hann M, et al. ; North-West Region Gastrointestinal Research Group A cluster-randomised controlled trial of a patient-centred guidebook for patients with ulcerative colitis: effect on knowledge, anxiety and quality of life. Health Soc Care Community. 2003;11:64–72. [DOI] [PubMed] [Google Scholar]
- 13. Benchimol EI, Walters TD, Kaufman M, et al. . Assessment of knowledge in adolescents with inflammatory bowel disease using a novel transition tool. Inflamm Bowel Dis. 2011;17:1131–1137. [DOI] [PubMed] [Google Scholar]
- 14. Neilson K, Ftanou M, Monshat K, et al. . A controlled study of a group mindfulness intervention for individuals living with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:694–701. [DOI] [PubMed] [Google Scholar]
- 15. Robinson A, Thompson DG, Wilkin D, et al. . Guided self-management and patient-directed follow-up of ulcerative colitis: a randomised trial. Lancet. 2001;358:976–981. [DOI] [PubMed] [Google Scholar]
- 16. Sephton M, Kemp K, Ridgway V. An evaluation study of a pilot group education programme for inflammatory bowel disease. Frontline Gastroenterol. 2016;7:135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schmidt S, Herrmann-Garitz C, Bomba F, et al. . A multicenter prospective quasi-experimental study on the impact of a transition-oriented generic patient education program on health service participation and quality of life in adolescents and young adults. Patient Educ Couns. 2016;99:421–428. [DOI] [PubMed] [Google Scholar]
- 18. Wardle RA, Mayberry JF. Patient knowledge in inflammatory bowel disease: the Crohn’s and Colitis Knowledge Score. Eur J Gastroenterol Hepatol. 2014;26:1–5. [DOI] [PubMed] [Google Scholar]
- 19. Moradkhani A, Kerwin L, Dudley-Brown S, et al. . Disease-specific knowledge, coping, and adherence in patients with inflammatory bowel disease. Dig Dis Sci. 2011;56:2972–2977. [DOI] [PubMed] [Google Scholar]
- 20. Waters BM, Jensen L, Fedorak RN. Effects of formal education for patients with inflammatory bowel disease: a randomized controlled trial. Can J Gastroenterol. 2005;19:235–244. [DOI] [PubMed] [Google Scholar]
- 21. Cross RK, Finkelstein J. Feasibility and acceptance of a home telemanagement system in patients with inflammatory bowel disease: a 6-month pilot study. Dig Dis Sci. 2007;52:357–364. [DOI] [PubMed] [Google Scholar]
- 22. Elkjaer M, Shuhaibar M, Burisch J, et al. . E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided ‘Constant-care’ approach. Gut. 2010;59:1652–1661. [DOI] [PubMed] [Google Scholar]
- 23. Cross RK, Jambaulikar G, Langenberg P, et al. . TELEmedicine for patients with Inflammatory Bowel Disease (TELE-IBD): design and implementation of randomized clinical trial. Contemp Clin Trials. 2015;42:132–144. [DOI] [PubMed] [Google Scholar]
- 24. Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–6; discussion 16. [DOI] [PubMed] [Google Scholar]
- 25. Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1:514. [DOI] [PubMed] [Google Scholar]
- 26. Walmsley RS, Ayres RC, Pounder RE, et al. . A simple clinical colitis activity index. Gut. 1998;43:29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rotter JB. Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr. 1966;80:1–28. [PubMed] [Google Scholar]
- 28. Schwarzer R, Jerusalem M. Generalized self-efficacy scale, causal and control beliefs. In: Johnston M, Wright S, Weinman J, eds. Measures in Health Psychology: A User’s Portfolio. Windsor, England: NFER-NELSON; 1995:35–37. [Google Scholar]
- 29. Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol. 2005;139:439–457. [DOI] [PubMed] [Google Scholar]
- 30. Hou JK, Turkeltaub JA, McCarty III TR, et al. . Assessment of disease specific knowledge and health-related quality of life among United States military veterans with inflammatory bowel disease. World J Gastroenterol. 2015;21:6001–6007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Waters BM, Jensen L, Fedorak RN. Effects of formal education for patients with inflammatory bowel disease: a randomized controlled trial. Can J Gastroenterol. 2005;19:235–244. [DOI] [PubMed] [Google Scholar]
- 32. Quinn CC, Clough SS, Minor JM, et al. . WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther. 2008;10:160–168. [DOI] [PubMed] [Google Scholar]