Abstract
Background
Although older adults with predialysis chronic kidney disease are at higher risk for falls, the prognostic significance of a serious fall injury prior to dialysis initiation has not been well described in the end-stage renal disease population.
Methods
We examined the association between a serious fall injury in the year prior to starting hemodialysis and adverse health outcomes in the year following dialysis initiation using a retrospective cohort study of U.S. Medicare beneficiaries ≥ 67 years old who initiated dialysis in 2010–2012. Serious fall injuries were defined using diagnostic codes for falls plus an injury (fracture, joint dislocation, or head injury). Health outcomes, defined as time-to-event variables within the first year of dialysis, included four outcomes: a subsequent serious fall injury, hospital admission, post-acute skilled nursing facility (SNF) utilization, and mortality.
Results
Among this cohort of 81,653 initiating hemodialysis, 2,958 (3.6%) patients had a serious fall injury in the year prior to hemodialysis initiation. In the first year of dialysis, 7.6% had a subsequent serious fall injury, 67.6% a hospitalization, 30.7% a SNF claim, and 26.1% died. Those with versus without a serious fall injury in the year prior to hemodialysis initiation were at higher risk (hazard ratio, 95% confidence interval) for a subsequent serious fall injury (2.65, 2.41–2.91), hospitalization (1.11, 1.06–1.16), SNF claim (1.40, 1.30–1.50), and death (1.14, 1.06–1.22).
Conclusions
For older adults initiating dialysis, a history of a serious fall injury may provide prognostic information to support decision making and establish expectations for life after dialysis initiation.
Keywords: Accidental falls, Chronic kidney failure, Geriatric nephrology
Falls that result in a serious injury, such as a fracture, joint dislocation, or brain injury are common among older adults and a harbinger of functional decline, nursing home placement, and death (1,2). While fatal falls do occur, the association of fall injuries with mortality is often attributed to the underlying illness burden, diminished physical resilience, postfall complications, and poor recovery (3–6). For these reasons, eliciting a history of an injurious fall may be clinically helpful for assessing prognosis.
Several studies have shown that falls are common among older adults with predialysis chronic kidney disease (7–9). Among Medicare beneficiaries, the rate of serious fall injuries has been shown to increase in the year preceding dialysis initiation (10). By the time patients reach end-stage renal disease (ESRD), the rate may be as high as 100 serious fall injuries per 1,000 person years. Despite higher rates of serious fall injuries among older adults approaching ESRD, the prognostic significance of a serious fall injury prior to dialysis initiation for outcomes in the year following dialysis has not been well described.
The purpose of the current study was to examine the association between a serious fall injury in the year prior to starting hemodialysis and adverse health outcomes in the year following dialysis initiation. In addition to mortality, we determined the association of a serious fall injury preceding hemodialysis initiation with a subsequent fall injury, hospitalization, and need for skilled-nursing facility (SNF) care.
Methods
Study Population and Data Sources
The study was approved by the Emory University Institutional Review Board. Data from Medicare ESRD eligibility (CMS-2728) forms and Part A (inpatient) and Part B (outpatient) claims were obtained from the U.S. Renal Data System (USRDS) (11). This retrospective cohort included patients initiating dialysis in 2010–2012, with follow-up through 2013. A total of 152,092 patients aged 67–100 years (such that all patients had Medicare coverage and related claims prior to the start of dialysis), who started dialysis between January 1, 2010 and December 31, 2012, were identified. Of these, 148,049 had Medicare eligibility form data, and 121,744 patients started treatment on hemodialysis and stayed on hemodialysis for at least 60 days. Because Medicare Part B includes emergency department (ED) coverage, we further limited our cohort to those with Part B coverage, defined as at least one outpatient claim in the 0–6 months prior to dialysis, plus at least one outpatient claim in the 6–12 months prior to dialysis (n = 81,653). For the SNF analysis only, we further limited the cohort to 71,368 patients without SNF claims in the 100 days prior. This was based on the Medicare benefit which provides 100 days of SNF care per benefit period and allowed us to identify need for new SNF care rather than a return to SNF following dialysis initiation.
Study Variables
Exposure
Our exposure of interest was a serious fall injury in the year prior to dialysis start. Serious fall injuries were identified in the 12 months prior to dialysis initiation and defined by ICD-9 codes in combined claims data from inpatient and emergency encounters using a previously published claims-based algorithm (8,12,13). Emergency encounters were defined as those outpatient encounters in which either the place of service or the type of provider was identified as an ED. Serious fall injuries were attributed to claims with a fall-related E code (8800–8889) and an injury code for nonpathological skull, facial, cervical, clavicle, humeral, forearm, pelvic, hip, fibula, tibia, or ankle fractures (80000–80619, 8070–8072, 8080–8089, 81000–81419, 8180–8251, or 8270–8291), brain injury (85200–85239), or dislocation of the hip, knee, shoulder, or jaw (8300–83219, 83500–83513, or 83630–83660). For claims without a fall-related E code, claims for the serious injuries listed above were defined as a serious fall injury in the absence of a motor vehicle accident E code (8100–8199). A serious fall injury was defined as yes (at least one serious fall injury claim) versus no (no serious fall injury claims) in the year prior to dialysis start.
Outcomes
Outcomes were defined as time-to-event variables within the first year of dialysis for four outcomes. Subsequent serious fall injuries were defined as above for history of serious fall injuries. Time-to-event was calculated as the difference between the date of the first claim for a postdialysis initiation serious fall injury and dialysis start date. Times to first hospital admission, first SNF claim, and death were defined similarly. Hospital admission rates were defined as number of admissions in the first year of dialysis divided by the follow-up time (time from dialysis start to 365 days or date of death, excluding time spent in the hospital).
Other variables
Incident age, sex, treatment modality history, and date of dialysis start were obtained from the USRDS standard analytic files. Race/ethnicity, smoking status, body mass index, history of comorbid conditions, and functional status indicators (inability to ambulate, inability to transfer, needing assistance with activities of daily living, and institutionalization) were all provider-reported and obtained from the Medicare ESRD eligibility form (CMS-2728).
Statistical Analysis
Patient characteristics were summarized overall and by whether patients had at least one serious fall injury in the year preceding dialysis initiation. Continuous and categorical characteristics were compared by fall status by t and χ2 tests, respectively. Cox proportional hazards models were used to obtain hazard ratios (HRs) for the association with a history of serious fall injuries. Time-to-event outcomes were censored for transplantation, switch to peritoneal dialysis, loss to follow-up (including uncertain dialysis modality, withdrawal from dialysis, and recovery of renal function), death (for outcomes excluding mortality), or end of study follow-up (365 days from dialysis start). Mortality events began at 60 days after dialysis start due to the exclusion of patients who were not on hemodialysis at least 60 days. Adjustment was performed for potential confounding demographic and clinical characteristics, with further adjustment for potentially mediating factors, including measures of functional status and healthcare access. Sensitivity analyses included (i) examination of incidence rate ratios (IRRs) for hospital admissions rates using negative binomial models (with an offset of log[follow-up time]); (ii) stratification of models of SNF utilization by whether patients had SNF claims in the year prior to dialysis start; and (iii) adjustment of mortality models for serious fall injuries after dialysis start, as a time-varying covariate in an extended Cox model. All analyses were performed with Stata v 14.2 (College Station, TX) and the statistical significance threshold was set at α = 0.05.
Results
Patient Characteristics
The mean age in this cohort of U.S. patients aged 67–100 years initiating hemodialysis in 2010–2012 was 76.8 years; about half (47.2%) were female and about two-thirds (65.5%) were non-Hispanic white (Table 1). More than half (54.9%) of the patients had comorbid diabetes, and most (87.8%) had comorbid hypertension. Overall, one-quarter (24.9%) had any (at least one) functional limitation; 9.9% were unable to walk at dialysis start, 18.2% needed assistance with activities of daily living, and 13.6% were institutionalized. Those who had a recent history of a serious fall injury were older, more likely to be female and white, and more likely to have an inpatient dialysis start and functional limitations, compared to those without serious fall injuries in the year prior to hemodialysis initiation; these patients were also less likely to have pre-ESRD nephrology care (Table 1). Any functional limitation at dialysis start was reported for 38.5% versus 24.4% (p < .001) of those with vs. without history of serious fall injuries.
Table 1.
Characteristics of U.S. Patients Aged 67–100 y Initiating Hemodialysis in 2010–2012, Overall and by Recent History of a Serious Fall Injury
| Characteristic at Dialysis Start | Overall | History of Serious Fall Injury | ||
|---|---|---|---|---|
| Yes | No | p* | ||
| N (%) | 81,653 | 2,958 (3.6%) | 78,695 (96.4%) | – |
| Demographics | ||||
| Mean (SD) age, years | 76.8 (6.5) | 78.1 (6.7) | 76.7 (6.5) | <.001 |
| Female, % | 47.2% | 57.7% | 46.8% | <.001 |
| Race/ethnicity, % | ||||
| Non-Hispanic white | 65.5% | 73.5% | 65.2% | <.001 |
| Non-Hispanic black | 20.5% | 12.4% | 20.8% | |
| Hispanic | 9.1% | 9.5% | 9.1% | |
| Other | 5.0% | 4.2% | 5.0% | |
| Clinical | ||||
| Received pre-ESRD nephrology care, % | 72.7% | 67.8% | 72.9% | <.001 |
| Inpatient dialysis start, % | 69.4% | 71.7% | 69.3% | .006 |
| Mean BMI (SD), kg/m2 | 28.3 (7.2) | 27.4 (7.1) | 28.3 (7.2) | <.001 |
| Comorbid conditions, % | ||||
| Diabetes | 54.9% | 56.0% | 54.9% | .2 |
| Atherosclerotic cardiovascular disease | 28.3% | 28.4% | 28.3% | .9 |
| Cerebrovascular disease | 11.8% | 14.4% | 11.7% | <.001 |
| Peripheral vascular disease | 16.8% | 17.9% | 16.7% | .08 |
| Hypertension | 87.8% | 86.3% | 87.9% | .009 |
| Congestive heart failure | 41.4% | 45.5% | 41.3% | <.001 |
| Functional status, % | ||||
| Inability to ambulate | 9.9% | 17.8% | 9.6% | <.001 |
| Inability to transfer | 5.5% | 10.3% | 5.3% | <.001 |
| Needs assistance with daily activities | 18.2% | 27.2% | 17.8% | <0.001 |
| Institutionalized | 13.6% | 23.9% | 13.2% | <.001 |
Note: Only patients with Part B coverage in the year prior to dialysis start are included. BMI = Body mass index; ESRD = End-stage renal disease.
N = 81,653 for all except: pre-ESRD care (N = 71,056), inpatient start (N = 72,902), and BMI (N = 81,039).
*By t (continuous variables) or chi-square (categorical variables) test.
Health Outcomes
Subsequent serious fall injuries
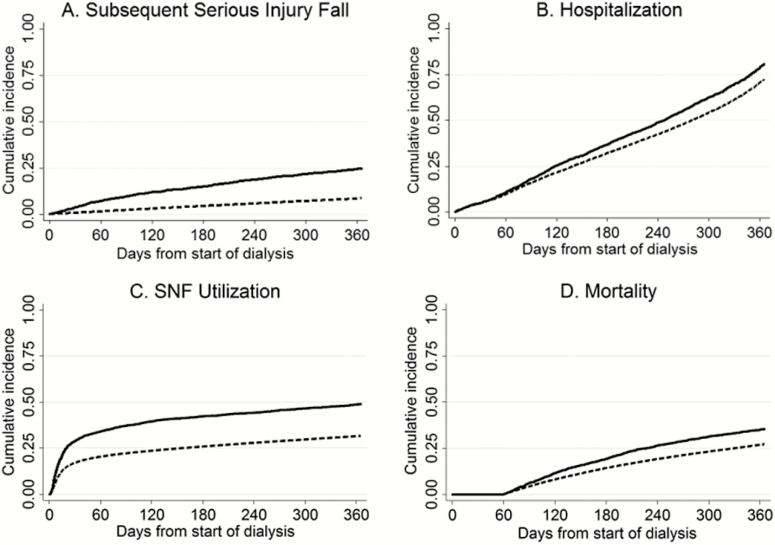
A total of 6,235 patients (7.6%) had a serious fall injury in the year after hemodialysis start. Patients with a history of serious fall injuries had more than three times the crude cumulative incidence of subsequent serious fall injuries in the first year of dialysis as patients without a history of serious fall injury (Figure 1A). With full adjustment for, patients with a serious fall injury had 2.7-fold higher rates of serious fall injuries in the year after dialysis start (Table 2). This association was of greater magnitude than any association of included covariates with subsequent serious fall injuries (Supplementary Table 1).
Figure 1.
Kaplan–Meier curves showing 1-year cumulative incidence of (A) serious fall injury, (B) hospital admission, (C) post-acute skilled nursing facility utilization, and (D) mortality, by history of serious fall injury. Solid lines, history of serious fall injury, dashed lines, no history of serious fall injury. SNF = Skilled nursing facility. p < .001 by log-rank test for all.
Table 2.
Associations of History of a Serious Fall Injury With Outcomes in the Year After Dialysis Start, Among U.S. Patients Aged 67–100 y Initiating Hemodialysis in 2010–2012
| Health Outcome | Hazard ratio (95% CI) for outcomes in the year after dialysis start, by history of serious fall injury (yes vs no), adjusted* for: | ||||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Serious fall injury | 2.96 (2.72–3.22) | 2.94 (2.71–3.20) | 2.89 (2.66–3.15) | 2.67 (2.44–2.94) | 2.65 (2.41–2.91) |
| Hospitalization | 1.22 (1.17–1.27) | 1.20 (1.15–1.26) | 1.16 (1.11–1.21) | 1.11 (1.06–1.17) | 1.11 (1.06–1.16) |
| Post-acute SNF utilization | 1.66 (1.56–1.77) | 1.62 (1.52–1.73) | 1.47 (1.38–1.57) | 1.38 (1.29–1.48) | 1.40 (1.30–1.50) |
| Mortality | 1.30 (1.22–1.39) | 1.28 (1.20–1.37) | 1.19 (1.12–1.27) | 1.15 (1.07–1.24) | 1.14 (1.06–1.22) |
Note: SNF = Skilled nursing facility. N = 62,583 for all except post-acute SNF utilization (N = 54,331).
Model 1 = age, sex, race.
Model 2 = Model 1 + history of diabetes, history of stroke, and history of congestive heart failure.
Model 3 = Model 2 + functional impairment defined as yes vs. no, any of inability to walk, transfer, or independently carry out activities of daily living, or being institutionalized.
Model 4 = Model 3 + nephrology access defined as pre-ESRD nephrology care and inpatient dialysis start.
Model 5 = Model 4 + body mass index, categorized as underweight (<18.5), normal weight (18.5–24.9; referent), overweight (25.0–29.9), and obese (≥30.0).
*Demographics=Clinical=history of diabetes, history of stroke, and history of congestive heart failure.
Hospital admissions
Most patients (n = 55,216 or 67.6%) had at least one hospital admission in year 1 of hemodialysis treatment. Cumulative incidence of hospital admissions was higher in those with versus without history of serious fall injury (Figure 1B). Fully-adjusted models showed 1.1-fold higher incidence of hospital admission among those with versus without history of serious fall injuries (Table 2); the magnitude of this effect was higher than that of most covariates and was similar to that of history of congestive heart failure in the same model (Supplementary Table 1). When rates of hospital admissions were examined (including all admissions, not just the first admission, in year 1), crude rates of hospital admissions were 3.3 versus 2.5 per person-year in those with versus without history of serious fall injury. Fully-adjusted models showed 1.2-fold higher rates of hospital admissions among those with history of serious fall injuries (incidence rate ratio = 1.16, 95% confidence interval [CI]: 1.10–1.22).
SNF utilization
Among the 71,368 patients without SNF utilization in the 100 days prior to dialysis start, 21,874 (30.7%) had at least one SNF claim in the year after dialysis. Cumulative incidence of SNF utilization was much higher among those with history of serious fall injuries; however, this effect was driven primarily by differences in the first ~2 months after dialysis start (Figure 1C). With full adjustment, those with history of serious fall injuries remained at 1.4-fold higher risk of SNF utilization in year 1 of dialysis treatment than those without these falls (Table 2), a higher magnitude of effect than any covariate except for functional impairment (Supplementary Table 1). In stratified analyses, history of serious fall injuries was associated with higher risk of SNF claims among patients without SNF claims prior to dialysis initiation (HR = 1.38 , 95% CI: 1.27–1.50) but not among patients with SNF claims prior to dialysis initiation (HR = 0.98, 95% CI: 0.85–1.13; pinteraction < .001).
Mortality
More than one-quarter (n = 21,339 or 26.1%) of patients died in the first year of dialysis. Cumulative mortality (after 60 days) was higher in those with versus without a history of a serious fall injury (Figure 1D). Fully-adjusted models showed 1.1-fold risk of mortality for those who had a serious fall injury in the year prior to dialysis, compared to those who did not (Table 2). This effect was less than that of older age, history of congestive heart failure, and functional impairment (Supplementary Table 1). When serious fall injuries after dialysis start were added as a time-varying exposure to the fully-adjusted model, the magnitude of the effect of history of serious fall injury on mortality was attenuated (HR = 1.02, 95% CI: 0.95–1.10). However, the occurrence of a serious fall injury after dialysis was associated with more than twice the risk of mortality in this same model (HR = 2.23, 95% CI: 2.11–2.34).
Discussion
Among older U.S. adults, a history of a serious fall injury in the year prior to hemodialysis initiation was associated with a higher risk of adverse health outcomes in the first year of dialysis. The associations of a recent history of a serious fall injury with a subsequent fall injury, hospitalization, need for SNF care, and death were all robust to adjustment for demographic and clinical characteristics and remained statistically significant after adjustment for potential mediating factors such as access to care, functional impairment, and body mass index. The magnitude of these associations was greatest for subsequent serious fall injuries and post-acute SNF utilization, suggesting that a serious fall injury provides important prognostic information in this population. Assessing prognosis for older adults initiating dialysis in terms of both mortality and functional decline may be improved by taking into account a history of a serious fall injury.
Older hemodialysis patients experience a high burden of functional impairment, health care utilization, and limited life-expectancy (14–16). Because of the considerable variability in outcomes and survival seen in this population (17), it is important to have prognostic markers that can be used to stratify risk. However, comorbidity indices or disease-specific markers that are routinely available in clinical and administrative databases, may not adequately capture this heterogeneity or be helpful for predicting risk for function-related outcomes (18). Geriatric or “nondisease-specific” problems have been shown to be associated with both mortality and functional decline. For example, among older adults who received post-acute care following dialysis initiation, the presence of multiple nondisease-specific problems identified shortly after dialysis initiation (falls, cognitive impairment, depressive symptoms, exhaustion, impaired mobility, and polypharmacy) were associated with death, need for nursing home placement, and functional impairment (14). The current study extends these findings in an important way by showing that an administrative claims-based algorithm for identifying serious fall injuries in the year before dialysis initiation can be used to assess risk for health outcomes following dialysis initiation.
Identifying the higher risk for adverse health outcomes after dialysis initiation associated with a recent serious fall injury may have important clinical implications. While geriatric conditions, such as impairments in mobility or function, have been shown to be significant prognostic markers, they are not reliably available in administrative data or electronic health records (9,14,19). Serious fall injuries, are more likely to be captured in both sources and thus be available to providers. A geriatric approach to patient care that identifies serious fall injuries can inform clinical care in two ways. First, recognizing a history of a serious fall injury can provide important prognostic information (20,21). Assessing and communicating prognosis to patients and their caregivers is especially important when making clinical decisions where the most appropriate treatment may vary by prognosis. Prognostic information is also helpful for anticipating care needs after a change in health status. Around the time of dialysis initiation, knowledge of a serious fall injury may facilitate patient-centered communication about prognosis both for making treatment decisions and predicting patients’ postdialysis initiation healthcare needs. Additionally, we found that a serious fall injury after dialysis was associated with more than twice the risk of mortality when considered a time-varying exposure. A serious fall injury after dialysis initiation may provide prognostic information needed for reevaluating goals of care.
Second, knowledge of a serious fall injury can be used to target patients for interventions to improve outcomes. Our findings suggest a nearly threefold higher risk of serious fall injuries in the year after dialysis in patients who had a fall injury in the prior year. Additionally, falls in the year after starting dialysis were associated with a higher risk of death. Well-designed multicomponent fall prevention interventions have been shown to be effective in the general population (22–24). Interventions that address known fall risk factors, alone or in combination with strategies to reduce dialysis-related symptoms that could lead to falls, should be tested and if found to be effective, made routinely available for ESRD patients, especially those with falls in the year prior to stating dialysis.
The current analysis had several strengths, including a large sample of older patients with available data on serious fall injuries in the year preceding dialysis initiation. Known limitations must also be considered. Because we used administrative claims data to identify falls which requires a patient experience an injury associated with the fall, we did not have available data on falls without injury. Additionally, we were interested in outcomes following dialysis initiation and accordingly limited our study cohort to those who started dialysis. However, it is possible that many older adults with advanced chronic kidney disease may experience serious fall injuries and die before progressing to kidney failure or choose not to start dialysis. Findings from the current study may not be generalizable to older chronic kidney disease patients who do not start dialysis. Finally, data on frailty components are not available; thus, assessment of the validity of serious fall injuries as potential markers of frailty is not possible in this study.
In conclusion, among older adults starting dialysis, a serious fall injury in the year prior to dialysis initiation was associated with a higher risk for an additional serious fall injury, hospitalization, SNF admission, and mortality. In this population, a history of a serious fall injury may provide prognostic information to support decision making and establishing expectations for life after dialysis initiation.
Supplementary Material
Supplementary data is available at The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences online.
Funding
Support was provided through a Career Development Award from the U.S. Department of Veterans Affairs (IK2CX000856) to C.B.B., an award from the Extramural Grant Program (EGP) by Satellite Healthcare, a not-for-profit renal care provider, to L.P., and additional support (KL2TR001115) to R.H.
Conflict of Interest
None reported.
Acknowledgments
L.P. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The data reported here have been supplied by the U.S. Renal Data System (USRDS). The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the U.S. government.
References
- 1. Gill TM, Murphy TE, Gahbauer EA et al. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol. 2013;178:418–425. doi:10.1093/aje/kws554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–1284. doi:10.1056/NEJM199710303371806 [DOI] [PubMed] [Google Scholar]
- 3. Gill TM, Murphy TE, Gahbauer EA et al. The course of disability before and after a serious fall injury. JAMA Intern Med. 2013;173:1780–1786. doi:10.1001/jamainternmed.2013.9063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dunn JE, Rudberg MA, Furner SE et al. Mortality, disability, and falls in older persons: the role of underlying disease and disability. Am J Public Health. 1992;82:395–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Roche JJ, Wenn RT, Sahota O et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. doi:10.1136/bmj.38643.663843.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vestergaard P, Rejnmark L, Mosekilde L. Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int. 2007;18:1583–1593. doi:10.1007/s00198-007-0403-3 [DOI] [PubMed] [Google Scholar]
- 7. Bowling CB, Booth JN 3rd, Gutierrez OM et al. Nondisease-specific problems and all-cause mortality among older adults with CKD: the REGARDS Study. Clin J Am Soc Nephrol. 2014;9:1737–1745. doi:10.2215/CJN.00880114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bowling CB, Bromfield SG, Colantonio LD et al. Association of reduced eGFR and albuminuria with serious fall injuries among older adults. Clin J Am Soc Nephrol. 2016:1236–1243. doi:10.2215/CJN.11111015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hall RK, Haines C, Gorbatkin SM et al. Incorporating geriatric assessment into a nephrology clinic: preliminary data from two models of care. J Am Geriatr Soc. 2016;64:2154–2158. doi:10.1111/jgs.14262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Plantinga LC, Patzer RE, Franch HA et al. Serious fall injuries before and after initiation of hemodialysis among older ESRD patients in the United States: a Retrospective Cohort Study. Am J Kidney Dis. 2017:76–83. doi:10.1053/j.ajkd.2016.11.021 [DOI] [PubMed] [Google Scholar]
- 11. U.S. Renal Data System: USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and and End-Stage Renal Disease in the United State, 2013 ed, Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; 2013 [Google Scholar]
- 12. Shimbo D, Barrett Bowling C, Levitan EB et al. Short-term risk of serious fall injuries in older adults initiating and intensifying treatment with antihypertensive medication. Circ Cardiovasc Qual Outcomes. 2016;9:222–229. doi:10.1161/CIRCOUTCOMES.115.002524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tinetti ME, Han L, Lee DS et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588–595. doi:10.1001/jamainternmed.2013.14764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bowling CB, Plantinga L, Hall RK et al. Association of nondisease-specific problems with mortality, long-term care, and functional impairment among older adults who require skilled nursing care after dialysis initiation. Clin J Am Soc Nephrol. 2016;11:2218–2224. doi:10.2215/CJN.01260216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jassal SV, Chiu E, Hladunewich M. Loss of independence in patients starting dialysis at 80 years of age or older. N Engl J Med. 2009;361:1612–1613. doi:10.1056/NEJMc0905289 [DOI] [PubMed] [Google Scholar]
- 16. Kurella Tamura M, Covinsky KE, Chertow GM et al. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361:1539–1547. doi:10.1056/NEJMoa0904655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tamura MK, Tan JC, O’Hare AM. Optimizing renal replacement therapy in older adults: a framework for making individualized decisions. Kidney Int. 2012;82:261–269. doi:10.1038/ki.2011.384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cheung KL, Montez-Rath ME, Chertow GM et al. Prognostic stratification in older adults commencing dialysis. J Gerontol A Biol Sci Med Sci. 2014;69:1033–1039. doi:10.1093/gerona/glt289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kurella M, Covinsky KE, Collins AJ et al. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med. 2007;146:177–183. [DOI] [PubMed] [Google Scholar]
- 20. Bao Y, Dalrymple L, Chertow GM et al. Frailty, dialysis initiation, and mortality in end-stage renal disease. Arch Intern Med. 2012;172:1071–1077. doi:10.1001/archinternmed.2012.3020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kutner NG, Zhang R, Huang Y et al. Falls among hemodialysis patients: potential opportunities for prevention?Clin Kidney J. 2014;7:257–263. doi:10.1093/ckj/sfu034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49. doi:10.1056/NEJMcp020719 [DOI] [PubMed] [Google Scholar]
- 23. Tinetti ME, Baker DI, McAvay G et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331:821–827. doi:10.1056/NEJM199409293311301 [DOI] [PubMed] [Google Scholar]
- 24. Heung M, Adamowski T, Segal JH et al. A successful approach to fall prevention in an outpatient hemodialysis center. Clin J Am Soc Nephrol. 2010;5:1775–1779. doi:10.2215/CJN.01610210 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.