Abstract
Objective: Hematologic abnormalities are the most common complications of human immunodeficiency virus (HIV) infection being more pronounced during the late stages of the disease, thereby indicating the progressive nature of the disease. Anemia is the most frequent hematologic abnormality in HIV. However, leukopenia, lymphopenia, and thrombocytopenia have also been observed. We undertook this study to evaluate the hematologic abnormalities in HIV patients and their relationship with the CD4 cell counts. Materials and methods: This is an analytical cross-sectional study that was carried out among patients in Jammu, India for the three years from 2015 to 2018. Data collection pro-forma has two parts. Firstly, socio-demographic details such as age, gender, marital status, and occupation were noted. Secondly, investigations such as HIV testing, complete blood counts and CD4 counts were considered. The Statistical Package for Social Sciences (SPSS) software version 20 was used for data entry and analysis. One way analysis of variance (ANOVA) was applied as appropriate to examine differences between quantitative variables. Results: Anaemia was present in 72.5% of cases in our study. Leukopenia, lymphopenia and thrombocytopenia were observed in 18.33%, 49.17%, and 15.83% of the cases, respectively. We found statistically significant relationships of anemia, absolute lymphocyte count, and thrombocytopenia with the CD4 counts (P<0.0001, =0.018 and =0.044, respectively). However, CD4 counts at the time of presentation were not significantly related to the total leukocyte count and absolute neutrophil count. Conclusions: Anemia was the most frequent hematologic abnormality in HIV patients followed by lymphopenia, leukopenia, and thrombocytopenia. A significant relationship was observed between the anemia, absolute lymphocyte count, and thrombocytopenia with the CD4 counts. We recommend routine hematologic investigations and timely treatment for all the hematologic derangements in HIV patients.
Keywords: Hematologic abnormality, HIV, AIDS, anemia, CD4 counts
Introduction
Human Immunodeficiency virus (HIV) infection is characterized by progressive weakening of the immune system attributed to the decrease in the number of circulating CD4+ T-helper cells. This predisposes HIV patients to a variety of opportunistic infections and neoplastic disorders. The most severe phase of HIV infection leads to Acquired Immunodeficiency syndrome (AIDS) where the CD4+ cell count drops below 200/mm3. It is marked by the appearance of particular opportunistic infections [1].
HIV infection leads to a multisystem disease with prevailing hematological abnormalities. Hematological aberrancies become more severe during the late stages of the disease signifying the importance of active virus replication and high levels of viremia in the causation of disease [2,3]. They include defective haematopoiesis, cytopenias affecting various cell lineages, and abnormalities of coagulation. These abnormalities are due to diverse reasons which include immune-mediated destruction of cells, direct cytopathic effects of the virus, secondary to various infections and neoplasms, and drug toxicity [4]. The most prevalent haematological disorder observed in children and adults with HIV infection is anemia. Incidences of anemia are particularly high in patients with late stages of the disease and a reduced CD4 cell count. Anemia has been linked with the advancement of the disease and increase in mortality [5-7].
Leukopenia is also a common occurrence, especially in patients with advanced stages of the disease [8-10]. Neutropenia has been observed in all stages of the disease. Lymphopenia primarily involves CD4 T-helper cells and is considered the classic hallmark of the disease. Lymphopenia worsens with the progression of the disease [11]. HIV-infected patients frequently present with dysplastic changes in neutrophils which includes bizarre nuclei, high N:C ratio, hypogranularity, and nuclear fragmentation [12]. Thrombocytopenia is found in all the stages of HIV; the prevalence being highest in the late stages of disease and with low CD4 cell counts [13-16]. Myelodysplastic changes have been observed in a large number of HIV patients and these changes can be detected in all the stages of the disease. Most common infectious agents involving the bone marrow in patients with AIDS are mycobacteriosis, histoplasmosis, and toxoplasmosis [17,18].
This study is an analytical cross-sectional study to assess the hematological abnormalities in HIV/AIDS patients and to correlate these abnormalities with the CD4 cell counts.
Methodology
The present study is an analytical cross-sectional study and was implemented on the patients registered at Dr. Bhardwaj’s Diagnostic Laboratory, Jammu, India. A retrospective data of three years from March, 2015 to February, 2018 was retrieved from the files of the patients. Dr. Bhardwaj’s Diagnostic Laboratory received blood samples for various hematological investigations from HIV-positive patients registered at the Voluntary Counselling and Testing Centre (VCTC), Government Medical College Hospital, Jammu. Exclusion criteria of the study include: suffering from malignancy not related to HIV/AIDS, pregnancy, and <16 years of age. The total number of patients validated for the study was 120. The research was conducted after ethical approval from Jammu and Kashmir State AIDS Control Society (Approval no: JKSACS/Adm/19/171). The de-identified data were collected from files of patients. Hence, the ethical committee of Jammu and Kashmir State AIDS Control Society exempted the authors from the necessity to obtain informed consent.
Data collection pro-forma has two parts. Firstly, socio-demographic details such as age, gender, marital status, and occupation were noted and secondly, investigations such as HIV testing, complete blood counts, CD4 counts were recorded. Case was defined as AIDS if it met criteria as specified by the National AIDS control society (NACO, 2007) [19].
Investigations
1. HIV detection tests: Comb Test (COMBAIDS for detecting HIV1 & 2) and ELISA Tests (GENEDIA HIV 1/2 RAPID 3.0 kits) were employed for diagnosing HIV infection.
2. Complete haematological evaluation was done first at the time of presentation. Blood collection and processing was done as per guidelines of National AIDS Control Organisation (NACO, India). The haematological investigations comprised of: a) Complete Blood Counts (CBC) by automated cell counter. This included the haemoglobin estimation, total erythrocyte count, total leukocyte count, differential leukocyte count, and platelet count; b) Peripheral blood examination after staining the blood film by Romanowsky stains; and c) Erythrocyte sedimentation rate (ESR) measurement was done by Westergren’s method [20].
3. CD4 cell counts: BD FACSCOUNT flow cytometer (Becton Dickenson and Company, California, USA) was used for CD4 cell counts.
4. Other routine investigations included routine urine examination, renal function tests, liver function tests, and chest X-rays. All patients were screened for associated sexually transmitted diseases (STD), i.e., for HCV, HBsAg, and VDRL.
5. Investigations like bone marrow aspiration/marrow trephine biopsy, USG abdomen, Mantoux test, and sputum for AFB were done as and when needed.
HIV patients were categorized into three clinical categories: Category A, B, and C based on the revised CDC classification system (1993). The three CD4+ T-lymphocyte categories are as follows: Category 1: greater than or equal to 500 cells/µL; Category 2: 200-499 cells/µL; and Category 3: less than 200 cells/µL [21].
Data analysis
The Statistical Package for Social Sciences (SPSS) software version 20 was used for data entry and analysis. Descriptive statistics were presented as frequency (numbers; n), percentage and mean ± SD. P values <0.05 was considered as statistically significant. Analysis of Variance (ANOVA) was used to examine differences between quantitative variables.
Results
In our study, male preponderance (57.5%) was observed. Male: female ratio was 1.35:1. Majority of the patients (72.5%) were in the age group ≤40 years. We found that 90% of the patients were married, 7.5% divorced or widowed and only 2.5% were unmarried. Sexual mode of transmission was the predominant mode of spread in our study and was found in 87.5% cases. 90 patients (80.83%) were on regular HAART treatment while HBV/HCV coinfection was found in 17 (14.17%) of cases (Table 1).
Table 1.
Socio-demographic and disease characteristics (n=120)
| Variable | n (%) | |
|---|---|---|
| Age group (in years) | <40 | 87 (72.5) |
| >40 | 33 (27.5) | |
| Gender | Male | 69 (57.5) |
| Female | 51 (42.5) | |
| Marital status | Unmarried | 3 (2.5) |
| Married | 108 (90) | |
| Divorced/Widow | 9 (7.5) | |
| Mode of transmission | Sexual | 105 (87.5) |
| Blood | 5 (4.17) | |
| Unknown | 10 (8.33) | |
| On regular HAART | 97 (80.83) | |
| Presence of HBV/HCV Co-infection | 17 (14.17) | |
Data are presented as frequencies; n and (%).
Anemia presented in 87 cases (72.5%). Leukopenia was observed in 22 patients (18.33%) and lymphopenia in 59 cases (49.17%). We found thrombocytopenia in 15.83% of the cases while neutropenia was observed only in 5% of the cases (Table 2).
Table 2.
Hematological abnormalities in HIV infected patients (n=120)
| Variable | n (%) |
|---|---|
| Leukopenia | 22 (18.33) |
| Lymphopenia | 59 (49.17) |
| Neutropenia | 6 (5.0) |
| Anemia | 83 (69.17) |
| Thrombocytopenia | 19 (15.83) |
In terms of the clinical categories, 47 patients were in the category A (4 patients in A1, 35 in A2, and 8 patients in A3); 43 patients in category B (4 patients in B1, 26 in B2, and 13 patients in B3); and 30 patients in category C (3 patients in C1, 4 in C2, and 23 patients in C3). With regard to CD4 counts, only 11 patients from all clinical categories had CD4 counts >500/µL, 65 patients had CD4 counts between 200-499/µL, and 44 patients had CD4 counts <200/µL (Table 3).
Table 3.
Clinical categories (CDC 1993 Revised classification system) of the HIV patients
| CD4+ T-cell categories | Clinical categories | Total | ||
|---|---|---|---|---|
|
| ||||
| A (Asymptomatic) | B (symptomatic) | C (AIDS indicator conditions) | ||
| >500/µL | 04 (A1) | 04 (B1) | 03 (C1) | 11 |
| 200-499/µL | 35 (A2) | 26 (B2) | 04 (C2) | 65 |
| <200/µL | 08 (A3) | 13 (B3) | 23 (C3) | 44 |
Data shown are n.
Hb levels and RBC counts were statistically significant when associated with CD4 counts (P<0.0001 and = 0.009, respectively). However, statistical significance was not observed with the TLC and ANC parameters. We observed lymphopenia in 59 cases (49.17%) and a statistical significant relation was found between ALC and CD4 counts (P=0.018). We observed thrombocytopenia in 19 cases (15.83%) and it was significantly related to CD4 counts (P=0.044) (Table 4).
Table 4.
Relationship of haematological parameters with CD4 counts of the HIV patients
| CD4 count (cells/µL) | <200 (n=44) | 200-499 (n=65) | ≥500/µL (n=11) | P | |||
|---|---|---|---|---|---|---|---|
| Hb (g/dL) | 9.23 | ±1.21 | 10.82 | ±1.84 | 11.77 | ±1.58 | <0.001* |
| RBC count (×106/mm3) | 3.69 | ±0.41 | 3.91 | ±0.39 | 4.02 | ±0.54 | 0.009* |
| TLC (/mm3) | 6850.59 | ±2133.71 | 7078.95 | ±2355.67 | 7180.91 | ±1281.64 | 0.835 |
| Neutrophils (%) | 64.69 | ±7.01 | 62.93 | ±6.47 | 59.29 | ±8.13 | 0.059 |
| Lymphocytes (%) | 30.27 | ±6.12 | 32.75 | ±6.96 | 36.12 | ±8.13 | 0.024* |
| Monocytes (%) | 2.18 | ±0.54 | 2.17 | ±0.34 | 2.05 | ±0.42 | 0.657 |
| Eosinophils (%) | 2.86 | ±0.78 | 2.53 | ±0.95 | 2.54 | ±0.87 | 0.150 |
| ANC cells/µL | 4350.12 | ±1385.35 | 4658.59 | ±1890.03 | 4489.97 | ±1685.12 | 0.649 |
| ALC cells/µL | 1823.38 | ±559.01 | 2036.98 | ±531.35 | 2332.23 | ±778.6 | 0.018* |
| Platelets (×103/µL) | 189.23 | ±32.3 | 208.31 | ±45.1 | 213.82 | ±49.2 | 0.048* |
Statistically significant (P<0.05).
Data shown are mean ± SD and P value.
Discussion
Hematological abnormalities are quite commonly observed in all the stages of HIV infection. In view of the resource constraints in developing countries like India, measurement of the hematological parameters assumes paramount importance. These measurements can be used as prognostic markers predicting the progression of the disease. We undertook this study to evaluate the haematological derangements in HIV patients and to correlate these derangements with the CD4 counts. Our study showed a predominance of males (57.5%), with male: female ratio of 1.35:1. Male predominance was observed by Dikshit et al., De Santis et al., and Parinithia and Kulkarni in 67.5%, 68%, and 61.6% of their cases, respectively [2,22,23]. Majority of our patients (72.5%) aged ≤40 years. In the study of Enawgaw et al. [16], it was found that 90% of their patients were <45 years old, whereas DeSantis et al. [22] found a mean age <42 years. In our study, the majority of the patients were married (90%). Enawgaw et al. found that 14.5% of the patients were single, whereas the other patients were married, widow or divorced. We found that sexual mode of transmission was the most common (87.5%). De Santis et al. found sexual transmission in 73.7% of cases [22]. Dikshit et al. found unprotected heterosexual exposure in 93.5% of their cases [2].
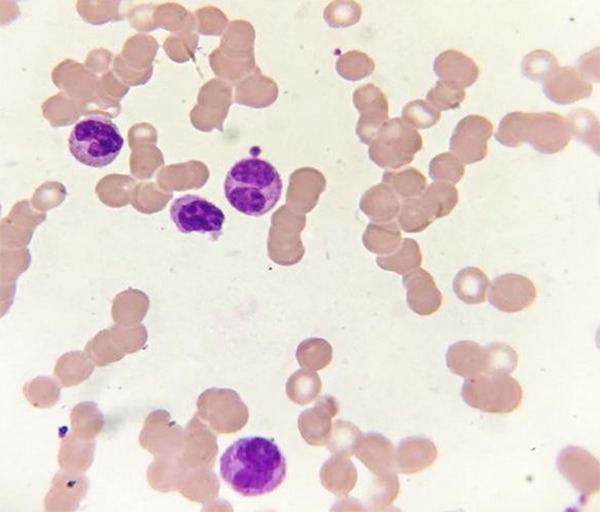
Hematologic abnormalities have been found to be strong prognosticators of morbidity and mortality in HIV patients [24]. Hematological abnormalities are mostly observed in the category 2 and 3 HIV patients but anemia and thrombocytopenia have been reported even in the early stage of HIV infection [25]. One of the most frequently occurring hematologic complications in HIV patients is the development of anemia, which is associated with decreased survival, increased disease progression, and deterioration in the quality of life. Factors contributing towards the development of anemia in HIV patients include sex and race of the patient, low CD4 counts, anti-HIV medications, and high viral load [26]. Opportunistic infections and myelosuppression by drugs also plays a dominant role in the pathogenesis of anemia [5,27]. Anemia being the most common haematological abnormality in HIV patients is more prevalent in advanced stages of the disease [28]. The prevalence of anemia varies widely ranging from as low as 22.2% to as high as 90.9% in the studies done in different population groups [29,30]. Anaemia was present in 72.5% cases in our study. Prevalence of anemia was found to be higher in the various studies done in India, as has been reported by Panwar et al. [31] in 86.4% of cases, Tripathi et al. [17] in 90% of cases, and Pandey A et al. [32] in 74.7% of the cases. Dikshit et al. found anemia in 65.5% of their patients [2]. The most common type of anemia observed in our study was normocytic normochromic anemia accounting for about 42.34% of cases (Figure 1). Panwar et al. found normocytic normochromic anemia in 46% of cases [31]. Kasthuri et al. [33] and Tripathi et al. [17] also reported “normocytic normochromic” as the most common type of anemia in HIV patients.
Figure 1.

Peripheral blood smear shows the presence of normocytic normochromic anemia in a HIV patient (Leishman stain 100×).
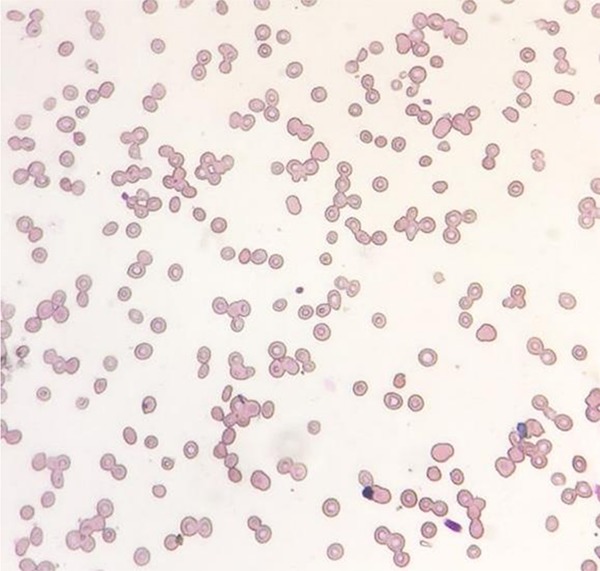
Leukopenia in AIDS patients has been attributed to defective granulopoiesis, infections, malignancies, and anti-granulocyte antibodies [34]. Toxicity of the drugs used to treat HIV infection also plays an important role in the pathogenesis of leukopenia [35]. The pathogenetic factors which account for neutropenia encompass direct cytopathic effects, myelodysplasia, drug toxicity, infections, and malignancies (Figure 2). Lymphopenia, especially involving CD4 T-helper cells, is predominantly due to the direct cytopathic effects of the virus [11]. In our study, leukopenia was observed in 18.33% patients and lymphopenia in 49.17% of the cases. Similar observations were made by Tripathi et al., Parinitha and Kulkarni, Thulasi et al., and Treacy et al. [17,23,35,36].
Figure 2.
Peripheral blood smear showing presence of hypolobulated neutrophils and a bilobed neutrophil in a HIV patient (Leishman stain 100×).
The prevalence of thrombocytopenia in HIV patients ranges from 3.74-40% in different studies (Figure 3). Different mechanisms responsible for thrombocytopenia include the immune mediated and non-immune mediated mechanisms [37,38]. We found thrombocytopenia in 15.83% of the cases. Many other studies have found thrombocytopenia in the range of 13 to 18% such as those conducted by Parinitha and Kulkarni [23], Patwardhan et al. [39], and Costello C [40].
Figure 3.
Peripheral blood smear shows the decrease in the number of platelets (thrombocytopenia) in a HIV patient (Leishman stain 100×).
In our study, severe anemia was observed in the HIV patients with lowered CD4 counts in contrast to the patients having higher CD4 counts. The RBC parameters, like Hb and RBC counts, were significantly related to CD4 counts (P<0.0001 and P=0.009 respectively). Parinitha and Kulkarni also found that the number of cases of anemia increased with decreasing CD4 counts and it was statistically significant [23]. Dikshit B et al. [2], De Santis et al. [22], Thulasi et al. [35], and Vanker et al. [41] found an increased incidence of anemia with decreasing CD4 counts.
We did not observe a significant relationship when CD4 counts were correlated with the total leukocyte count and absolute neutrophil count. Devi CS et al. observed lower TLC and ANC counts with decreasing CD4 cell counts, but did not find significant correlations between them [42]. Dikshit et al. did not find any cases of neutropenia in their study conducted on 200 HIV patients. Moreover, they did not find a significant relationship between CD4 counts and the total leucocyte count [2]. However, Parinitha and Kulkarni found significant correlations of CD4 count with total leukocyte count where lowered CD4 counts lead to lowered total leucocyte counts [23]. Vanker et al. found a statistically significant relationship between declining CD4+ counts and TLC and neutrophil counts [41].
In our study, lymphopenia was observed in 49.17% of the cases. The relationship between the absolute lymphocyte count and CD4 counts was statistically significant (P=0.018). Parinitha and Kulkarni found a significant relation between CD4 count and each of lymphopenia and absolute lymphocyte counts [23].
Thrombocytopenia was observed in 15.83% of the cases in our study and the relationship with the CD4 count was statistically significant (P=0.044). Enawgaw et al. found a significant increase in thrombocytopenia cases with decrease in CD4 counts (P=0.007). De Santis et al. [22] and Katemba et al. [43] also found a significant association between decreasing CD4+ cell counts and thrombocytopenia. However, some of the authors failed to find a significant relationship between thrombocytopenia and CD4 counts [35,41]. Dikshit et al. [2] and Parinitha and Kulkarni [23] found thrombocytopenia in 7% and 18% of their patients, respectively but did not find a significant relation with CD4 counts.
Conclusions
Derangements in the hematological profile are frequent in HIV patients. The most frequent hematological abnormality is anemia followed by lymphopenia, leukopenia and thrombocytopenia. A statistically significant relationship was noted between the anemia and the declining CD4 counts. Absolute lymphocyte count and thrombocytopenia also showed a significant association with CD4 counts thereby implying the adverse effect of lowered CD4 counts on the disease progression. We recommend routine haematological investigations as reliable and cheap prognostic indicators in HIV patients and appropriate treatment for all the haematological derangements.
Disclosure of conflict of interest
None.
Abbreviations
- HIV
Human immunodeficiency virus
- AIDS
Acquired immunodeficiency syndrome
- CBC
Complete blood counts
- ESR
Erythrocyte sedimentation rate
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HAART
Highly active antiretroviral therapy
- RBC
Red blood cell
- TLC
Total leucocyte count
- ANC
Absolute neutrophils count
- ALC
Absolute lymphocyte count
References
- 1.HIV/AIDS. https://www.cdc.gov/hiv/basics/whatishiv.html. Published March 1, 2019.
- 2.Dikshit B, Wanchu A, Sachdeva RK, Sharma A, Das R. Profile of hematological abnormalities of Indian HIV infected individuals. BMC Blood Disord. 2009;9:5. doi: 10.1186/1471-2326-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirchhoff F, Silvestri G. Is Nef the elusive cause of HIV-associated hematopoietic dysfunction? J Clin Invest. 2008;118:1622–5. doi: 10.1172/JCI35487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comprehensive, up-to-date information on HIV/AIDS treatment and prevention from the University of California San Francisco. HIV Transmission and Prevention in Adolescents. http://hivinsite.ucsf.edu/InSite?page=kb-04-01-09. Accessed March 6, 2019.
- 5.Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW. Epidemiology of anemia in human immunodeficiency virus (HIV)-infected persons: results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood. 1998;91:301–308. [PubMed] [Google Scholar]
- 6.O’Brien ME, Kupka R, Msamanga GI, Saathoff E, Hunter DJ, Fawzi WW. Anemia is an independent predictor of mortality and immunologic progression of disease among women with HIV in Tanzania. J Acquir Immune Defic Syndr. 2005;40:219–225. doi: 10.1097/01.qai.0000166374.16222.a2. [DOI] [PubMed] [Google Scholar]
- 7.Semba RD, Shah N, Klein RS, Mayer KH, Schuman P, Vlahov D Human Immunodeficiency Virus Epidemiology Research Study Group. Prevalence and cumulative incidence of and risk factors for anemia in a multicenter cohort study of human immunodeficiency virus infected and -uninfected women. Clin Infect Dis. 2002;34:260–266. doi: 10.1086/338151. [DOI] [PubMed] [Google Scholar]
- 8.Evans RH, Scadden DT. Haematological aspects of HIV infection. Baillieres Best Pract Res Clin Haematol. 2000;13:215–230. doi: 10.1053/beha.1999.0069. [DOI] [PubMed] [Google Scholar]
- 9.Frontiera M, Myers AM. Peripheral blood and bone marrow abnormalities in the acquired immunodeficiency syndrome. West J Med. 1987;147:157–160. [PMC free article] [PubMed] [Google Scholar]
- 10.Castella A, Croxson TS, Mildvan D, Witt DH, Zalusky R. The bone marrow in AIDS. A histologic, hematologic and microbiologic study. Am J Clin Pathol. 1985;84:425–432. doi: 10.1093/ajcp/84.4.425. [DOI] [PubMed] [Google Scholar]
- 11.Lim ST, Levine AM. Hematological aspects of human immunodeficiency syndrome. In: Lichtman MA, Beutler E, Kipps TJ, Seligsoha U, Kaushansky K, Prchal JT, editors. William’s Hematology. 7th edition. New York: McGraw Hill Medical; 2006. pp. 1109–34. [Google Scholar]
- 12.Bain BJ. The haematological features of HIV infection. Br J Haematol. 1997;99:1–8. doi: 10.1046/j.1365-2141.1997.2943111.x. [DOI] [PubMed] [Google Scholar]
- 13.Mathews SE, Srivastava D, Balayadav R, Sharma A. Association of hematological profile of human immunodeficiency virus-positive patients with clinicoimmunologic stages of the disease. J Lab Physicians. 2013;5:34–37. doi: 10.4103/0974-2727.115929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sloand EM, Klein HG, Banks SM, Vareldzis B, Merritt S, Pierce P. Epidemiology of thrombocytopenia in HIV infection. Eur J Haematol. 1992;48:168–172. doi: 10.1111/j.1600-0609.1992.tb00591.x. [DOI] [PubMed] [Google Scholar]
- 15.Firnhaber C, Smeaton L, Saukila N, Flanigan T, Gangakhedkar R, Kumwenda J, La Rosa A, Kumarasamy N, De Gruttola V, Hakim JG, Campbell TB. Comparisons of anemia, thrombocytopenia, and neutropenia at initiation of HIV antiretroviral therapy in Africa, Asia, and the Americas. Int J Infect Dis. 2010;14:1088–1092. doi: 10.1016/j.ijid.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Enawgaw B, Alem M, Addis Z, Melku M. Determination of hematological and immunological parameters among HIV positive patients taking highly active antiretroviral treatment and treatment naïve in the antiretroviral therapy clinic of Gondar University Hospital, Gondar, Northwest Ethiopia: a comparative cross-sectional study. BMC Hematol. 2014;14:8. doi: 10.1186/2052-1839-14-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tripathi AK, Kalra P, Misra R, Kumar A, Gupta N. Study of bone marrow abnormalities in patients with HIV disease. J Assoc Physicians India. 2005;53:105–10. [PubMed] [Google Scholar]
- 18.Brook MG, Ayles H, Harrison C, Rowntree C, Miller RF. Diagnostic utility of bone marrow sampling in HIV positive patients. Genitourin Med. 1997;73:117–121. doi: 10.1136/sti.73.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naco.gov.in. 2019. [online] Available at: http://www.naco.gov.in/sites/default/files/Guidelines%20for%20Prevention%20and%20Management%20of%20common%20opportunistic%20infections.pdf [Accessed 24 Jun. 2019]
- 20.Bain BJ, Bates I, Laffan M, Lewis SM, editors. Dacie and Lewis Practical Haematology. 11th edition. Edinburgh: Churchill Livingstone; 2011. pp. 36–104. [Google Scholar]
- 21.1993 revised classification system for HIV infection and expandedsurveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep. 1992;41:1–19. [PubMed] [Google Scholar]
- 22.De Santis GC, Brunetta DM, Vilar FC, Brandão RA, de Albernaz Muniz RZ, de Lima GM, Amorelli-Chacel ME, Covas DT, Machado AA. Hematological abnormalities in HIV-infected patients. Int J Infect Dis. 2011;15:e808–811. doi: 10.1016/j.ijid.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Parinitha S, Kulkarni M. Haematological changes in HIV infection with correlation to CD4 cell count. Australas Med J. 2012;5:157–162. doi: 10.4066/AMJ.20121008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anastos K, Shi Q, French AL, Levine A, Greenblatt RM, Williams C, DeHovitz J, Delapenha R, Hoover DR. Total lymphocyte count, hemoglobin, and delayed-typehypersensitivity as predictors of death and AIDS illness in HIV-1-infected women receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2004;35:383–392. doi: 10.1097/00126334-200404010-00008. [DOI] [PubMed] [Google Scholar]
- 25.Basu A, Ghosh K, Banerjee K. Bone marrow involvement in HIV infection: light, electron and immuno electron microscopic studies. Indian J Hematol Blood Transf. 1999;17:76–86. [Google Scholar]
- 26.Volberding PA, Levine AM, Dieterich D, Mildvan D, Mitsuyasu RandSaag M Anemia in HIV Working Group. Anemia in HIV infection: clinical impact and evidence-based management strategies. Clin Infect Dis. 2004;38:1454–63. doi: 10.1086/383031. [DOI] [PubMed] [Google Scholar]
- 27.Moyle G. Anaemia in persons with HIV infection: prognostic marker and contributor to morbidity. AIDS Rev. 2002;4:13–20. [PubMed] [Google Scholar]
- 28.Geletaw T, Tadesse MZ, Demisse AG. Hematologic abnormalities and associated factors among HIV infected children pre- and post-antiretroviral treatment, North West Ethiopia. J Blood Med. 2017;8:99–105. doi: 10.2147/JBM.S137067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mihiretie H, Taye B, Tsegaye A. Magnitude of anemia and associated factors amongpediatric HIV/AIDS patients attending Zewditu Memorial Hospital ART clinic, Addis Ababa, Ethiopia. Anemia. 2015;2015:479329. doi: 10.1155/2015/479329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Totin D, Ndugwa C, Mmiro F, Perry RT, Jackson JB, Semba RD. Iron deficiency anemia is highly prevalent among human immunodeficiency virus-infected and uninfected infants in Uganda. J Nutr. 2002;132:423–9. doi: 10.1093/jn/132.3.423. [DOI] [PubMed] [Google Scholar]
- 31.Panwar A, Sharma SC, Kumar S, Sharma A. A study of anemia in human immunodeficiency virus patients: estimating the prevalence, analyzing the causative effect of nutritional deficiencies, and correlating the degree of severity with CD4 cell counts. Med J DY PatilUniv. 2016;9:312–8. [Google Scholar]
- 32.Pande A, Bhattacharyya M, Pain S, Ghosh B, Saha S, Ghosh A, Banerjee A. Anemia in antiretroviral naïve HIV/AIDS patients: a study from Eastern India. Online J Health Allied Scs. 2011;10:4. [Google Scholar]
- 33.Kasthuri A, Sanjeevan S, Kar P. A study of hematological manifestations of HIV infection. Indian J Sex Transm Dis. 2006;27:9–16. [Google Scholar]
- 34. Donald W. Northfelt, MD, Mayo Clinic, Scottsdale, Arizona. Hematologic Manifestations of HIV. http://hivinsite.ucsf.edu/InSite?page=kb-04-01-09. (Published February 1998)
- 35.Thulasi R, Manimaran D, Hemanathan G, Afroz T, Sagar R. Hematological abnormalities in HIV infected individuals in correlation to CD4 counts and ART status. AJMS. 2016;7:14–8. [Google Scholar]
- 36.Treacy M, Lai L, Costello C, Clark A. Peripheral blood and bone marrow abnormalities in patients with HIV related disease. Br J Haematol. 1987;65:289–94. doi: 10.1111/j.1365-2141.1987.tb06855.x. [DOI] [PubMed] [Google Scholar]
- 37.Li Z, Nardi MA, Karpatkin S. Role of molecular mimicry to HIV-1 peptides in HIV-1-related immunologic thrombocytopenia. Blood. 2005;106:572–576. doi: 10.1182/blood-2005-01-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alexaki A, Wigdahl B. HIV-1 infection of bone marrow hematopoietic progenitor cells and their role in trafficking and viral dissemination. PLoS Pathog. 2008;4:e1000215. doi: 10.1371/journal.ppat.1000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patwardhan MS, Gowlikar AS, Abhyankar JR, Atre MC. Hematologic profile of HIV positive patients. Int J Pathol Microbiol. 2002;45:147–50. [PubMed] [Google Scholar]
- 40.Costello C. Haematological abnormalities in human immunodeficiency virus (HIV) disease. J Clin Pathol. 1988;41:711–15. doi: 10.1136/jcp.41.7.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vanker NandIpp H. The use of the full blood count and differential parameters to assess immune activation levels in asymptomatic, untreated HIV infection. S Afr Med J. 2013;104:45–8. doi: 10.7196/samj.6983. [DOI] [PubMed] [Google Scholar]
- 42.Devi CS, Satish S, Gupta M. A study of haematological profile in human immune deficiency virus infection: correlation with CD4 cell count. Ann Pathol Lab Med. 2016;5:484–489. [Google Scholar]
- 43.Katemba C, Muzoora C, Muwanguzi E, Mwambi B, Atuhairwe C, Taremwa IM. Hematological abnormalities in HIV-antiretroviral therapy naïve clients as seen at an immune suppression syndrome clinic at Mbarara Regional Referral Hospital, southwestern Uganda. J Blood Med. 2018;9:105–110. doi: 10.2147/JBM.S157148. [DOI] [PMC free article] [PubMed] [Google Scholar]


