Abstract
In order to manage the urgent psychological need for support in response to the anticipated reaction of the population to the COVID-19 pandemic, we developed a new psychological crisis intervention model by implementing a centralised psychological support system for all of Tunisia. We set up a helpline which is accessible throughout the country, including those without access to Internet. This model integrates medical students, child and adolescent psychiatrists, psychiatrists, psychologists and social services to provide psychological intervention to the general population and medical staff. It will make a sound basis for developing a more effective psychological crisis intervention response system.
Keywords: COVID-19, Psychological support, Algorithm
The World Health Organization declared the current outbreak of COVID-19 a pandemic on March 11th, 2020 (WHO, 2020). Seeing the world data and especially taking into account the effect of COVID-19 on Mediterranean countries such as France and Italy (to which Tunisia is close to in proximity), the Tunisian government has taken several in-phase anticipatory measures to prevent the progression of the pandemic within the nation (Tunisian Republic Presidency, 2020).
As in other countries, the rapidly increasing numbers of confirmed cases and deaths resulted in both medical staff and the public experiencing psychological problems, including anxiety, depression, and stress (Araújo et al., 2020; Brooks et al., 2020).
In order to better manage the urgent psychological need for support, we developed a psychological crisis intervention model by implementing a centralised psychological assistance for all of Tunisia. We provided a helpline present throughout the Tunisian territory. The Strategic Health Operations Center (Shoc room) along with the psychological support unit (CAP) called into action this intervention on March 14th.
The Shoc Room is a unit belonging to the Ministry of Health whose mission is to coordinate health interventions in emergency situations. The first time Tunisia implemented a psychological crisis intervention was after the terrorist attack in Bardo in 2015 (Bouasker, 2015), and was reinstated several times as a response to terrorist attacks, natural disasters, and major accidents. On December 20th, 2016, a ministerial decree defined the function of the CAP, its composition, and its regional consultant for north, centre and south region.
1. Protocol Methods for preparing the implementation of the Psychological crisis intervention: the Process from March 14th to March 30th 2020
1.1. First step: discussion between the Shoc Room and the CAP about the implementation of a work algorithms and a technical platform
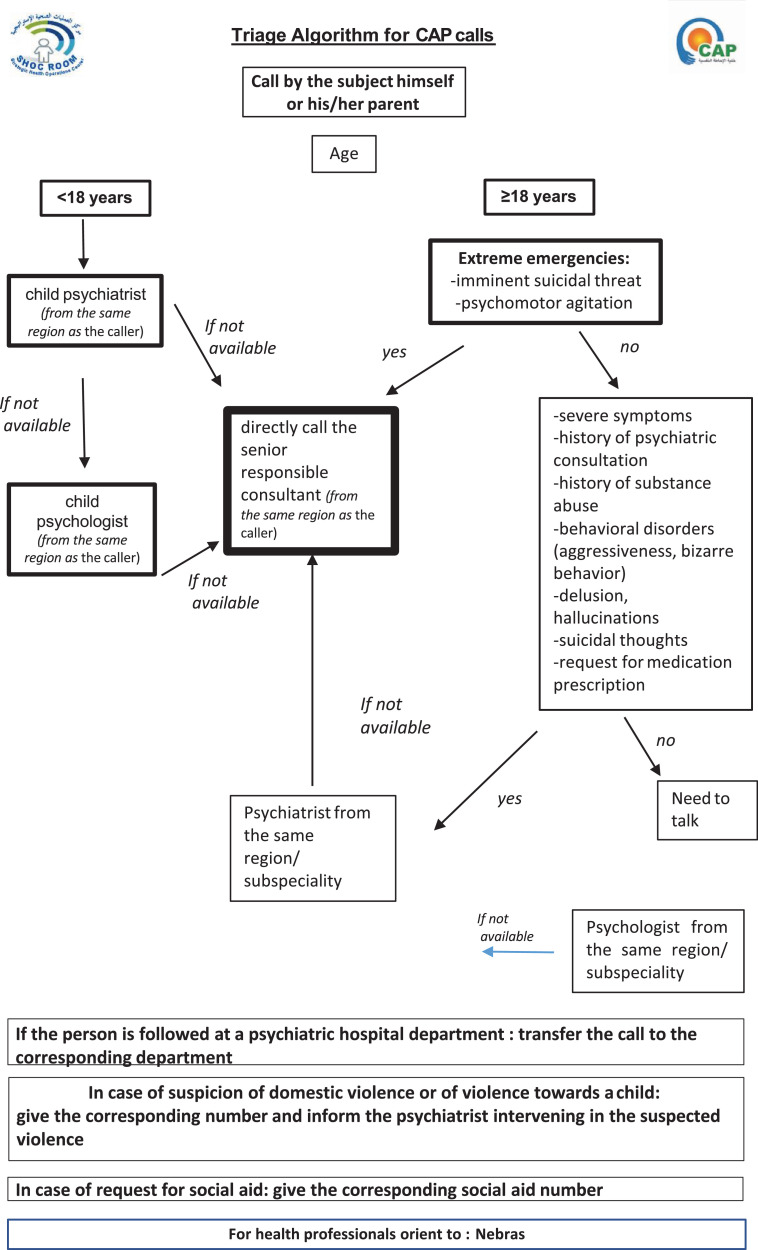
A virtual meeting was conducted between the Shoc Room and the consultants of the CAP to discuss the psychiatric needs of the general population, health professionals and different technicalities. This was followed by several virtual meetings between the consultants of the CAP for elaboration on the algorithm of the triage during the reception of a call and the management of beneficiaries (see figure 1 ). We solicited the national telephone operator; the result being the installation of a helpline accessible to all citizens free of charge. We also needed to establish the necessary facilities for the operation of the technical assistance centre: for this we resorted to a call center subject to Convention 108 of the protection of the personal data, and which has voluntarily made available essential protective measures (hydroalcoholic gel, mask), logistics and technology. In addition, we solicited the Tunisian institute for rehabilitation NEBRAS for the care of health professionals. A meeting with the Shoc Room and the CAP was held to finalize the procedure of the intervention and discuss the progress of the technicalities
Fig. 1.
Triage Algorithm for CAP calls
1.2. Second step: Recruitment of therapists willing to volunteer: psychiatrists, child psychiatrists and psychologists from all over Tunisia
The helpline was announced in professional social groups, and each regional consultant personally contacted the fellow colleagues of their specialty throughout Tunisia. This approach was possible given the limited number of mental health specialists and due to the openness of Tunisian culture. Ultimately, we had 200 volunteers the first week and 240 the second week. The psychological care of health professionals was initiated in collaboration with the Nebras Institute and the CAP. The telephone number of the Nebras Institute was broadcast in the media and in hospitals.
1.3. Third step: Coordination between the Tunisian Medical Student's Association (Associa-Med), the Tunisian Red Crescent, the Shoc Room and the CAP for training of receivers and handlers of the calls from the general population
The students were trained on the psychological impact of quarantine, the technical platform, the call sorting algorithms, and the different difficulties to anticipate when receiving calls. A representative of the teleoperator volunteers was appointed. Additionally, a method of communication for the group of volunteers was agreed up on: students are asked to fill out their availability to ensure sufficient distribution of receivers throughout the day.
1.4. Fourth step: Modelling of the process of the contact between a subject and a therapist (see figure 1)
Before the beginning of each week, each volunteer therapist indicates his availability throughout the day and week, with specification of his or her residing area and his or her subspecialty as addictology, suicidology or victimology. The student receiving the call completes a form with the subject identification, age, gender, COVID-19 risk status, psychiatric and somatic history, and current complaints. Depending on the algorithm, they transfer the call to a therapist after verifying their availability. A CAP consultant, who guides them in case of an uncertainty while applying the call triage algorithm, supervises the students. The therapist receiving the call receives in parallel an email containing the information collected by the student. At the end of the intervention, the therapist is invited to fill an intervention sheet which includes: the clinical symptoms, the reason for the call, the psychiatric interview data and the intervention methods such as: social orientation, psychiatric emergencies orientation, referral to the attending psychiatrist, psychoeducation about anxiety, relaxation training, recommendation, if necessary, for parental consultation when the call is concerning their child. Several media appearances were made to inform the general population of the CAP availability and to raise awareness about the psychological effects of quarantine.
1.5. March 30 th, the beginning of the activity
In the Arabic word, we didn't find a same scientific study. We quickly installed an intervention protocol and adapted it to the Tunisian population, as it was suggested that psychological interventions “should be targeted and adapted as appropriate” (Duan & Zhu, 2020). Our country demonstrates widespread telephone accessibility, although the internet is lacking or scarcely used in some regions. Furthermore, the fact that the number is free of charge allows a greater number of distressed people to receive care without having to worry about cost. The centralisation of the calls is also a strong suit of our model; meanwhile several countries have done local or institutionalized interventions (Liu et al., 2020). This aspect was possible due to the ethnic and cultural homogeneity between Tunisian regions as well as help from the health ministry.
We included therapists for children and adults in order to account for the different sections of the population in terms of age and profession, as well as a service accessible to quarantined subjects and specific to health professionals who necessitate appropriate care in this time of crisis, as described by various other authors (Neto et al., 2020).
Globally, several interventions are based on teleconsultation using new technology and mobile applications (Orrù et al., 2020).
In addition, seeing the emergence of the many psychiatric emergencies during the COVID-19 pandemic (Tian et al., 2020), Artificial Intelligence, by means of applications such as We Chat, Weibo, and Tik Tok, has offered interventions for psychological crises and support to people that are suffering (Liu et al., 2020). In our model however, we prioritized human contact that first takes place during the triage done by the students, and later with the therapists.
The intervention methods are adapted, ranging from simple psychoeducation to specialized care by therapists competent in victimology, suicidology or addictology. These offers are carried out immediately and on demand.
We have also taken into consideration the complications linked to confinement such as the resurgence of violence or the increase in social assistance care in our country classified as low middle income. However, it is important to note that these complaints are not specific to Tunisia and have been described throughout the course of this COVID-19 pandemic (Lima et al., 2020; Mukhtar, 2020).
2. Conclusion
We present a good model of medico-economic-social volunteering ranging from CAP members, volunteer therapists, medical students, Red Crescent psychologists and the facilitator of the technical platform. At the time of the submission of this protocol, psychosocial crises and requests are growing, which leave us thinking about how to further improve our intervention, especially to provide access for prescription medication and to begin teleconsultation. We hope this model will make a sound basis for developing a more effective psychological crisis intervention response system that is applicable for urgent social and psychological problems.
Authors’ contributions
Yosra Zgueb and Soumaya Bourgou designed the review.
Anissa Bouasker, Aida Neffeti, Badii Amamou, Jaweher masmoudi, Naoufel Somrani and Henda Chebbi reviewed the study protocol and provided substantial input to the manuscript. All authors critically reviewed drafts and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
The authors would like to thank all the members of the strategic health operations center, the volunteers of the CAP and the facilitator of the technical platform.
References
- WHO, 2020. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020.
- Araújo F.J., de O., de Lima L.S.A., Cidade P.I.M., Nobre C.B., Neto M.L.R. Impact of Sars-Cov-2 And Its Reverberation In Global Higher Education And Mental Health. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouasker A. Bardo Terrorist attack : Psychological support units : Assessment and Recommendations 9 months after. La Tunisie Medicale. 2015;93(12):733–736. http://latunisiemedicale.com/article-medicale-tunisie_2942_fr [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it : Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima N.N.R., de Souza R.I., Feitosa P.W.G., Moreira J.L., de S., da Silva C.G.L., Neto M.L.R. People experiencing homelessness: Their potential exposure to COVID-19. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.-T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukhtar S. Preparedness and proactive infection control measures of Pakistan during COVID-19 pandemic outbreak. Research in Social & Administrative Pharmacy. 2020 doi: 10.1016/j.sapharm.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neto M.L.R., Almeida H.G., Esmeraldo J.D., Nobre C.B., Pinheiro W.R., de Oliveira C.R.T., Sousa I.da C., Lima O.M.M.L., Lima N.N.R., Moreira M.M., Lima C.K.T., Júnior J.G., da Silva C.G.L. When health professionals look death in the eye : The mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orrù G., Gemignani A., Conversano C. Psychological intervention measures during the COVID-19 pandemic. Clinical Neuropsychiatry. 2020;17(2):76–79. doi: 10.36131/CN20200208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunisian Republic Presidency, 2020. President activities during March 2020. http://www.carthage.tn/?q=ar/event-created/month/2020-03.