Abstract
Purpose
To discuss the effects of the severe acute respiratory syndrome coronavirus 2 betacoronavirus on ambulatory ophthalmology practices, the value proposition of telemedicine, teleophthalmology implementation methodologies, and the accelerated future of telemedicine.
Design
Review of the current telehealth landscape including usage, policies, and techniques for ambulatory practice integration.
Methods
We provide author-initiated review of recent trends in telehealth, governmental recommendations for health care delivery during the COVID-19 pandemic, and a PubMed Central query for telemedicine in ophthalmology or teleophthalmology. In addition, the authors' comprehensive experience in telemedicine design and implementation is provided.
Results
We provide a summary describing the present state of telehealth, teleophthalmology modeling, care delivery, and the proposed impact of telehealth surges on the future of ophthalmology practice.
Conclusion
Recent patient and provider interest in telemedicine, the relaxation of regulatory restrictions, increased remote care reimbursement, and ongoing social distancing practices compel many ophthalmologists to consider virtualizing services.
The global severe acute respiratory syndrome coronavirus 2 betacoronavirus pandemic and the accompanying social distancing policies are tremendously impacting the world's economy, governments, and health care delivery. Hospitals are desperately searching for supplies and physicians to treat patients in particularly burdened areas. Less widely discussed, ambulatory practices face issues supporting patient care and business operations during the crisis. The current health care crisis and need for social distancing to protect our providers, affiliate staff, and patients has necessitated the need to consider new methodologies for ophthalmic evaluation, coding, and reimbursement.
Telemedicine may offer solutions; however, ophthalmology's telehealth experience is historically store-and-forward using a hub-and-spoke model, similar to radiology. The Centers for Disease Control and Prevention is now recommending telemedicine in lieu of live clinic visits in anticipation of an extended period of social distancing.1 Patients themselves are looking for digital care, evidenced by recent surges reported by telehealth companies.2 , 3 Before social distancing mandates, 74% of patients were unaware of a telemedicine option in their physicians' practices.4 The COVID-19 pandemic has transformed this scenario, such that some leading telehealth platforms now report virtual patient visits have increased between 257% and 700%. This surge correlates with the regional impact of coronavirus infection.5 Payers are expanding coverage and privacy restrictions have been relaxed.6 Whether these changes signal more permanent reforms in legislative, regulatory, and local hospital requirements and restrictions remains to be seen.
At present, the New York–based authors recognized the need for emergent telemedicine implementation at New York Eye and Ear Infirmary of Mount Sinai's walk-in eye clinic to reduce novel coronavirus exposure to the physicians, staff, and congregating patients. We describe guidelines to help practices implement telemedicine. We also explore the COVID-19 related telemedicine surge as it accelerates a paradigm shift for how patients access medical care.
Define the Scope of your Telemedicine Goals
The current issues in ophthalmology practices are how to use staff, offering triage, and how to maintain patient–physician engagement. An office may decide to use telemedicine tools for different purposes. There are good reasons to address the following objectives/use cases: triage acute problems,7 medication reconciliation to improve adherence,8 reassurance,9 , 10 follow-up of chronic conditions,11 reassess care plans,12 reschedule upcoming appointments or procedures,13 and advertising telehealth service to patients.14 , 15 Offices may choose to focus on one or a few of these objectives rather than attempt to completely virtualize.
Telemedicine can be offered through scheduled telephone calls or video visits (VVs). One may bill either service, but guidelines vary between these modalities and by states. VVs are advantageous for triage because of the video component but can be used for any of the above objectives. Telephone calls are routine for physicians and are often not billed. To bill, there must be proper documentation and the patient must be informed. The physician may find it awkward to return an emergent call and inform the patient they will bill for the call. Patient-requested nonurgent calls could be scheduled as a visit by the office, documented, and submitted for reimbursement. Remote patient monitoring is also available and billable but is not yet scaled.16 Patient-generated image interpretation17 and patient portal correspondence6 are also separately reimbursable services but are not discussed in detail here.
Process Changes
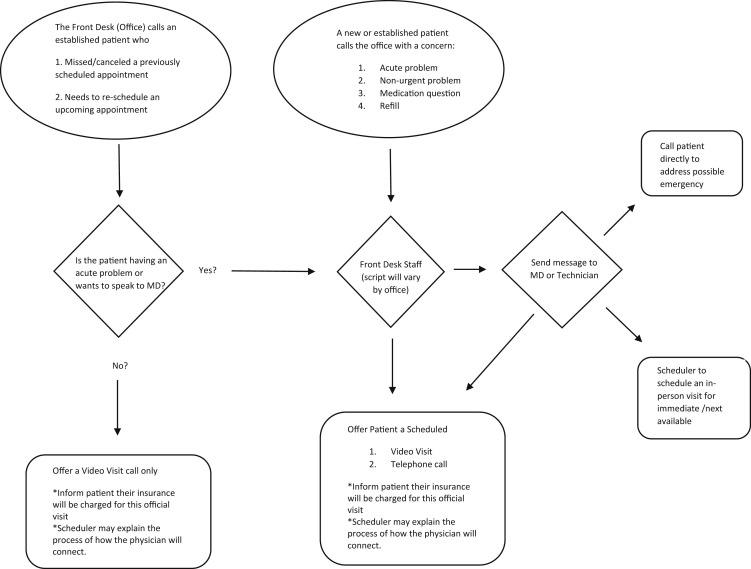
In tackling the processes needed to quickly construct a live ophthalmology telemedicine program, we were motivated by saving lives through social distancing in a hyperendemic area (New York City) while also staying available to provide care for needy patients. Regulatory and billing issues were important albeit secondary considerations. Using workflow diagrams (Figure ) to map the entire visit cycle in the practice helps to ensure that a new service integrates well. By adding or changing only the parts of the workflow required to incorporate telemedicine, the new offering becomes seamlessly delivered in daily operations. We addressed one use case at a time, with plans to grow with each success facilitating adoption. Many practices may first start by looking for a mobile platform and then adapting their workflow to the technology. The authors advocate for the alternative approach of conceptualizing the desired future state first and then finding the right technology for the workflow. Some options are large platforms branded with the practice's name, while others are a simple link to join a visit. Technology is replaceable; however, a robust process to integrate that technology allows a program to thrive.
Figure.
A workflow diagram that maps the ophthalmology telehealth visit cycle is depicted.
Some important considerations and lessons learned to reinforce process change include the creation of scripts for the staff who will support the new program and ensuring appropriate network connectivity and hardware. Furthermore, we found it better to use of large screens to more readily visualize the patient (tablets instead of mobile phones for conducting VVs, for example). VVs can be converted to a telephone call if the video connection is unsuccessful. In addition, the team has found value in involving the provider when deciding if the patient can be scheduled for a VV, telephone call, or if they need to be seen emergently. We find that the process change is iterative, but with time, becomes integrated.
A Telehealth Visit Life Cycle
Scheduling
The front desk staff is critical to direct patients. For patients who call the office, the scheduler may offer a scheduled VV, a scheduled telephone call, or let the physician decide which type of visit is appropriate. One may choose to offer telehealth to either established or new patients; it is particularly important to recognize the limitations of new patient visits. When the office calls the patients, the front desk may offer scheduled VVs, but not telephone calls.17 Emergent calls should be handled immediately.
History
William Osler's statement from the late 1800s (“Just listen to your patient(s), he is telling you the diagnosis”) is still true.18 The importance of taking a detailed history cannot be overstated. The technician or provider can gather and document the required elements to support the evaluation and management (E/M) coding. Some telehealth platforms allow customizable dynamic questionnaires for the patient to fill out before the VV.
Visual Acuity
The technician or provider can guide the use of Amsler grids or visual acuity measurement via mobile app or printed chart as many options are available. Printed charts are easier to validate because the provider can see the figures displayed on the chart while the patient reads. There are mobile and online refraction tools that can also be incorporated. None of these methods are as accurate as in-office testing. Using the same method to check visual acuity each time allows the provider to trend the measured vision, which becomes more useful data. Certainly, there is now an urgent need to validate remote assessment of this most basic of ophthalmic vital signs using the myriad of functional tools that are available. Ultimately, if a visual acuity cannot be obtained for the telehealth visit, there are still many other pieces of valuable information one can ascertain to complete the visit.
Intraocular Pressure
The iCare Tonometer and the Sensimed Triggerfish contact lens are available for at-home tonometry but they are expensive and not widely tested in terms of accuracy in the home environment.19 , 20 Finger tensions performed by the patient are also an option21 and patients may be encouraged to describe how hard the eye feels in terms of familiar objects like a piece of fruit. In our experience this requires patience in instructing patients how to properly self-perform finger tensions and the subjective response of the patients need to be judged on a case-by-case basis. Patients may also be offered intraocular pressure measurements at an alternate care location to minimize in-office exposure, such as a parking lot. but such an approach to tonometric measurement is largely untested. Overall, major gaps exist in the performance of remote tonometric measurements.
Ancillary Testing
Previous test results can be reviewed for established patients. There are online and app-based perimeters available, such as Peristat (Keep Your Sight Foundation, Los Angeles, California).22, 23, 24 For evaluation of macular diseases there are apps and devices to monitor the central 10° including the commercially available preferential hyperacuity perimeter ForSee device (Notal Vision) and discrimination apps such as mVT (Vital Art and Science) application.16 Smartphone retinal imaging is available, but not yet designed for patients to use at home.25, 26, 27 Overall, home-based remote monitoring is still relatively premature and not widely available. As an alternative to at-home testing, one may establish clinics for specific tests to be performed while few or no other patients are in the office to maintain social distancing. The results of these tests can be forwarded to the physician for an upcoming VV or phone call.
Examination
VVs will allow for basic psychologic and neurologic, external adnexal, pupil, motility, alignment, anterior segment, iris, and corneal light reflexes (with the latter performed using an external light source supplied by the patient and used under the direction of the physician). It is recommended to ask the patient to move toward a window or to stay in a well-lit area. Both the patient and physician must work in spaces with high internet connectivity. While handheld devices are often the most convenient and accessible for both the patient and physician, the use of larger devices with higher-resolution screens may be preferable to maximize the quality of image acquisition and viewing.
Interventions and Planning
Medication changes, care plan modifications, recommended referrals, consenting for upcoming previously planned procedures, revising surgical dates based on disease severity, and establishing following telehealth or testing visits are all examples of care interventions that could be conducted during a VV.
Documentation, Billing, and Compliance for Ambulatory Ophthalmology Telehealth
The reimbursement policies for telehealth were expanded on March 13, 2020 under the Coronavirus Preparedness and Response Supplemental Appropriations Act.28 Many telehealth restrictions related to licensing, reimbursable services, and Health Insurance Portability and Accountability Act compliance were relaxed under the 1135 waiver. It is unlikely that one could obtain all the information necessary to submit an eye code. Low level E/M codes are recommended. The authors recommend checking Centers for Medicare and Medicaid Services and the Academy of Ophthalmology resources for up-to-date billing changes because billing requirements are in a constant state of flux. Briefly, there are 3 main types of reimbursable visits6:
-
1.
Telehealth visit: VVs with supporting documentation for established patients and, under the waiver, new patient visits.
-
2.
Virtual check-in: Telephone calls with supporting documentation. The phone encounter cannot be tied to an office visit within the last 7 days nor can it result in an in-office appointment within the next 24 hours or next available.
-
3.
Digital encounters: A patient-initiated communication through a Health Insurance Portability and Accountability Act–compliant portal used to perform E/M services, normally done during a face-to-face communication. These services may be billed once during a 7-day cumulative period. This does not include global periods and is available for established patients.
Verbal consent, duration of the visit, the type of visit (telehealth), diagnosis codes, and patient and provider location are all required documentation to support billing for all telehealth services. The verbal consent should delineate what telehealth entails, the benefits and risks of using telehealth to perform a limited examination, and any other state-designated requirements. The fact that this examination is not live and thereby incomplete should be highlighted. If charging the insurance company, the patient must be informed.
The Future of Virtual Ophthalmology
Social distancing has pushed industries into remote operations, and many speculate if there will be a “new normal” after this pandemic. For medicine, that would involve telehealth. Even though the technology for remote ophthalmic monitoring is not scalable or ready, it seems that our patients are willing to adopt this approach. This crisis will likely spur innovation that will transform care delivery. For ophthalmology that could mean scalable and more accurate home testing. There may be improved near focus on smartphone cameras or attachments for self-photography. Remotely controlled slit-lamp devices, nonmydriatic fundus cameras, and optical coherence tomography machines may become more available in public areas. Perhaps the ophthalmologist will routinely have scheduled telephone calls and VVs with patients to review test results, check on medication adherence, or triage patients.
It is important to recognize that some subspecialties are more amenable to live telehealth visits than others. Specialties such as oculoplastics, neuro-ophthalmology, and pediatrics may be better suited for VVs because much of these examinations can be performed externally. Anterior segment pathology is more difficult to address via telehealth unless the pathology is grossly obvious on external evaluation. For glaucoma, VVs are particularly useful for medicine reconciliation and assessment of glaucoma medication tolerance. Retinal telehealth is best supported by store-and-forward asynchronous models that are already well-established in some settings.29 , 30 For retinal subspecialists, VVs may be helpful in the assessment of macula function of selected diabetic retinopathy and age-related macula disease patients.
While ophthalmology waits for new innovations to become widely available, the current interest and efforts to implement telehealth will likely have lasting effects. Reimbursement structures have already changed in remarkable ways and the policies surrounding the telehealth support its growth more than ever. Patients who are elderly or chronically ill have a heightened awareness of its utility as they currently use it to reduce their exposure. Previously, teleophthalmology was more reserved for rural or underserved areas. During this pandemic, everyone became remote and underserved, making telehealth mainstream. We may soon observe teleophthalmology finding a more permanent role.
CRediT authorship contribution statement
Sophia Mirza Saleem: Conceptualization, Project administration, Writing - original draft, Writing - review & editing. Louis R. Pasquale: Conceptualization, Project administration, Writing - review & editing. Paul A. Sidoti: Project administration, Writing - review & editing. James C. Tsai: Conceptualization, Project administration, Resources, Writing - review & editing.
Acknowledgments
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest. Funding/Support: Administrative support by the New York Eye and Ear Infirmary of Mount Sinai under the leadership of Dr James C. Tsai. Financial Disclosures: Dr Pasquale is a consultant to Eyenovia, Bausch+Lomb, Nicox, Emerald Bioscience, and Verily. Dr Tsai is a consultant to Eyenovia, ReNetX Bio, and Smartlens and receives research support from his Delafield-Rodgers Professorship. Drs Saleem and Sidoti have no financial conflicts of interest. Conceptualization (S.M.S., L.R.P., J.C.T.); Project administration (S.M.S., L.R.P., P.A.S., J.C.T.); Resources (J.C.T.); Writing - original draft (S.M.S.); Writing - review & editing (S.M.S., L.R.P., P.A.S., J.C.T.). All authors attest that they meet the current ICMJE criteria for authorship.
Footnotes
Supplemental Material available at AJO.com.
Supplemental Data
Dr Sophia Mirza Saleem is double board-certified in Ophthalmology, with Uveitis sub-specialty training, and Clinical Informatics. In addition to practicing ophthalmology, Dr Saleem has served as the Associate Medical Information Officer for New York Eye and Ear Infirmary as well as a Director of Telemedicine and Teleconsults for the Mount Sinai Hospital Health System. She works to improve patient care coordination with primary care partners, such as through her design, implementation, and support of a multi-facility tele-retina program which has completed thousands of screenings. Her interests remain at the cross section between informatics, telehealth, and ophthalmology.
References
- 1.Centers for Disease Control and Prevention Get your clinic ready for coronavirus disease 2019 (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinic-preparedness.html Available at:
- 2.Healthcare IT News Telemedicine during COVID-19: benefits, limitations, burdens, adaptation. https://www.healthcareitnews.com/news/telemedicine-during-covid-19-benefits-limitations-burdens-adaptation Available at:
- 3.Patients overwhelm telehealth services amid coronavirus pandemic - STAT. https://www.statnews.com/2020/03/17/telehealth-services-overwhelmed-amid-coronavirus-pandemic/ Available at:
- 4.Truex G. As telehealth technology and methodologies mature, consumer adoption emerges as key challenge for providers. https://www.youtube.com/watch?v=Ez1DvKAlULU Available at:
- 5.Forbes.com The coronavirus has created a surge of telemedicine demand. GoodRx now lets consumers compare services. https://www.forbes.com/sites/leahrosenbaum/2020/03/26/the-coronavirus-has-created-a-surge-of-telemedicine-demand-goodrx-now-lets-consumers-compare-services/#164bc9947f50 Available at:
- 6.Center for Medicaid and Medicare Services Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Available at:
- 7.Marsden J. An evaluation of the safety and effectiveness of telephone triage as a method of patient prioritization in an ophthalmic accident and emergency service. J Adv Nurs. 2000;31(2):401–409. doi: 10.1046/j.1365-2648.2000.01285.x. [DOI] [PubMed] [Google Scholar]
- 8.Rose A.J., Fischer S.H., Paasche-Orlow M.K. Beyond medication reconciliation the correct medication list. JAMA. 2017;317(20):2057–2058. doi: 10.1001/jama.2017.4628. [DOI] [PubMed] [Google Scholar]
- 9.Dawn A.G., Lee P.P. Patient expectations for medical and surgical care: a review of the literature and applications to ophthalmology. Surv Ophthalmol. 2004;49(5):513–524. doi: 10.1016/j.survophthal.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 10.The secret to a satisfied patient. https://www.reviewofophthalmology.com/article/the-secret-to-a--satisfied-patient Available at:
- 11.American Academy of Ophthalmology 4 ways to boost patient satisfaction. https://www.aao.org/eyenet/article/4-ways-to-boost-patient-satisfaction?december-2018 Available at:
- 12.Chalk D., Smith M. Guidelines on glaucoma and the demand for services. Br J Heal Care Manag. 2013;19(10):476–481. [Google Scholar]
- 13.National Collaborating Centre for Acute Care . Methods, evidence & guidance. National Collaborating Centre for Acute Care (UK); London: 2009. Glaucoma. Diagnosis and managenement of chronic open angle glaucoma and ocular hypertension. [PubMed] [Google Scholar]
- 14.Rotvold G.H., Knarvik U., Johansen M.A., Fossen K. Telemedicine screening for diabetic retinopathy: staff and patient satisfaction. J Telemed Telecare. 2003;9(2):109–113. doi: 10.1258/135763303321327984. [DOI] [PubMed] [Google Scholar]
- 15.Sreelatha O.K., Ramesh S.V.S. Teleophthalmology: Improving patient outcomes? Clin Ophthalmol. 2016;10:285–295. doi: 10.2147/OPTH.S80487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holekamp N.M. Moving from clinic to home: what the future holds for ophthalmic telemedicine. Am J Ophthalmol. 2018;187:xxviii–xxxv. doi: 10.1016/j.ajo.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Center for Medicaid and Medicare Services Final policy, payment, and quality provisions changes to the medicare physician fee schedule for calendar year 2019. https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year Available at:
- 18.Sturdy S. William Osler: a life in medicine. BMJ. 2000;321:1087. [Google Scholar]
- 19.Chen E., Quérat L., Åkerstedt C. Self-tonometry as a complement in the investigation of glaucoma patients. Acta Ophthalmol. 2016;94(8):788–792. doi: 10.1111/aos.13129. [DOI] [PubMed] [Google Scholar]
- 20.Tan S., Yu M., Baig N., Hansapinyo L., Tham C.C. Agreement of patient-measured intraocular pressure using rebound tonometry with Goldmann applanation tonometry (GAT) in glaucoma patients. Sci Rep. 2017;7:42067. doi: 10.1038/srep42067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Philippin H., Shah P., Burton M. Detecting possible glaucoma with only limited equipment: a crucial first step. Community Eye Health J. 2012;25(79–80):48–49. [PMC free article] [PubMed] [Google Scholar]
- 22.Lowry E.A., Hou J., Hennein L. Comparison of peristat online perimetry with the humphrey perimetry in a clinic-based setting. Transl Vis Sci Technol. 2016;5:4. doi: 10.1167/tvst.5.4.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vingrys A.J., Healey J.K., Liew S. Validation of a tablet as a tangent perimeter. Transl Vis Sci Technol. 2016;5:3. doi: 10.1167/tvst.5.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gan K., Liu Y., Stagg B., Rathi S., Pasquale L.R., Damji K. Telemedicine for glaucoma: guidelines and recommendations. Telemed J E Health. 2020;26(4):551–555. doi: 10.1089/tmj.2020.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lord R.K., Shah V.A., San Filippo A.N., Krishna R. Novel uses of smartphones in ophthalmology. Ophthalmology. 2010;117(6):1274–1274.e3. doi: 10.1016/j.ophtha.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 26.Muiesan M.L., Salvetti M., Paini A. Ocular fundus photography with a smartphone device in acute hypertension. J Hypertens. 2017;35(8):1660–1665. doi: 10.1097/HJH.0000000000001354. [DOI] [PubMed] [Google Scholar]
- 27.Ademola-Popoola D.S., Olatunji V.A. Retinal imaging with smartphone. Niger J Clin Pract. 2017;20(3):341–345. doi: 10.4103/1119-3077.201428. [DOI] [PubMed] [Google Scholar]
- 28.Coronavirus Preparedness and Response Supplemental Appropriations Act. 2020. Pub L No. 116-123, 134 Stat 146. [Google Scholar]
- 29.Tozer K., Woodward M.A., Newman Casey P.A. Telemedicine and diabetic retinopathy: review of published screening programs. J Endocrinol Diabetes. 2015;2(4):1–18. doi: 10.15226/2374-6890/2/4/00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams S.L., Wang L., Kane S.A. Telemedical diagnosis of retinopathy of prematurity: accuracy of expert versus non-expert graders. Br J Ophthalmol. 2010;94(3):351–356. doi: 10.1136/bjo.2009.166348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Dr Sophia Mirza Saleem is double board-certified in Ophthalmology, with Uveitis sub-specialty training, and Clinical Informatics. In addition to practicing ophthalmology, Dr Saleem has served as the Associate Medical Information Officer for New York Eye and Ear Infirmary as well as a Director of Telemedicine and Teleconsults for the Mount Sinai Hospital Health System. She works to improve patient care coordination with primary care partners, such as through her design, implementation, and support of a multi-facility tele-retina program which has completed thousands of screenings. Her interests remain at the cross section between informatics, telehealth, and ophthalmology.