Older adults in nursing homes have multiple risk factors for healthcare-associated infections including comorbid conditions, indwelling devices, frequent hospital visits, functional impairment, and increased use of medications including antibiotics.1 An estimated 2 million infections occur in US nursing homes each year, increasing mortality, antibiotic resistance, and healthcare costs.1–4 In healthcare settings, antibiotic-resistant bacteria are mainly spread by person-to-person contact, most often between healthcare personnel (HCP) and patients and/or residents, and by indirect contact with contaminated environmental surfaces and fomites. In Veterans Affairs (VA) nursing homes, enhanced barrier precautions (gowns and gloves) are recommended when performing direct care or touching the environment in rooms of residents colonized with select antibiotic-resistant bacteria including MRSA; however, gowns and gloves are generally not used outside resident rooms. To our knowledge, no previous studies have been done to characterize physical contact patterns between individuals and objects in nursing home common areas. In this study, our objective was to conduct observation of contact between staff, residents and the environment in nursing home common areas, where there is little guidance for infection prevention precautions.
Methods
This observational study was conducted over 15 months (February 2016 to April 2017) in 24 units in 8 VA nursing homes in 6 states (Miami, FL; Boston, MA; Ann Arbor, MI; Baltimore, MD; Perry Point, MD; Vancouver, WA; Kerrville, TX; and San Antonio, TX). Units included skilled nursing units, short-term rehabilitative care and long-term care. Hospice and palliative care–only units were excluded from observation. The VA Central Institutional Review Board deemed the study exempt human subjects research.
Trained research staff with no clinical responsibilities on the units randomly selected nursing home common areas from a pre-specified list standardized to be similar at each nursing home. Locations included dining hall, lounge/TV room, occupational therapy, physical therapy, recreation therapy or group activity room, and courtyard. All observers were trained in the use of the data collection tool and worked with a supervising local primary investigator. Each observation period lasted 15–30 minutes. Observers recorded the number of staff and residents present at the start and end of the observation period and tallied each time a staff member or resident had direct hand contact with another staff member, resident, or surfaces and objects in the environment. Hand hygiene and use of gloves were also recorded.
We calculated the average contacts as the total contacts observed divided by the median number of staff and residents observed in the room per hour of observation.
Results
A total of 1,726 observations over 531 hours were conducted over the study period. Most observations took place in the lounge/TV room (195 hours, 36.0%) and dining hall (179 hours, 33.4%).
On average, resident–staff contact occurred 5.8 times per hour and was highest in physical and occupational therapy (16.7 and 15.0 contacts per hour, respectively). Contact between residents and the environment was common (12.2 contacts per hour on average) and occurred most often in the dining hall (18.3 contacts per hour) and in physical therapy (17.4 contacts per hour), and least often was in the lounge/TV room (6.3 contacts per hour). There was little contact between residents (<1 contact per hour on average). Staff-environment contact was highest in physical and recreational therapy (26.6 and 25.8 contacts per hour, respectively). Staff donned gloves most often in occupational and physical therapy (3.2 and 2.7 times per hour respectively). Staff performed hand hygiene most often in occupational and physical therapy (2.9 and 2.2 times per hour respectively). Total contacts per hour are shown in Fig. 1.
Fig. 1.
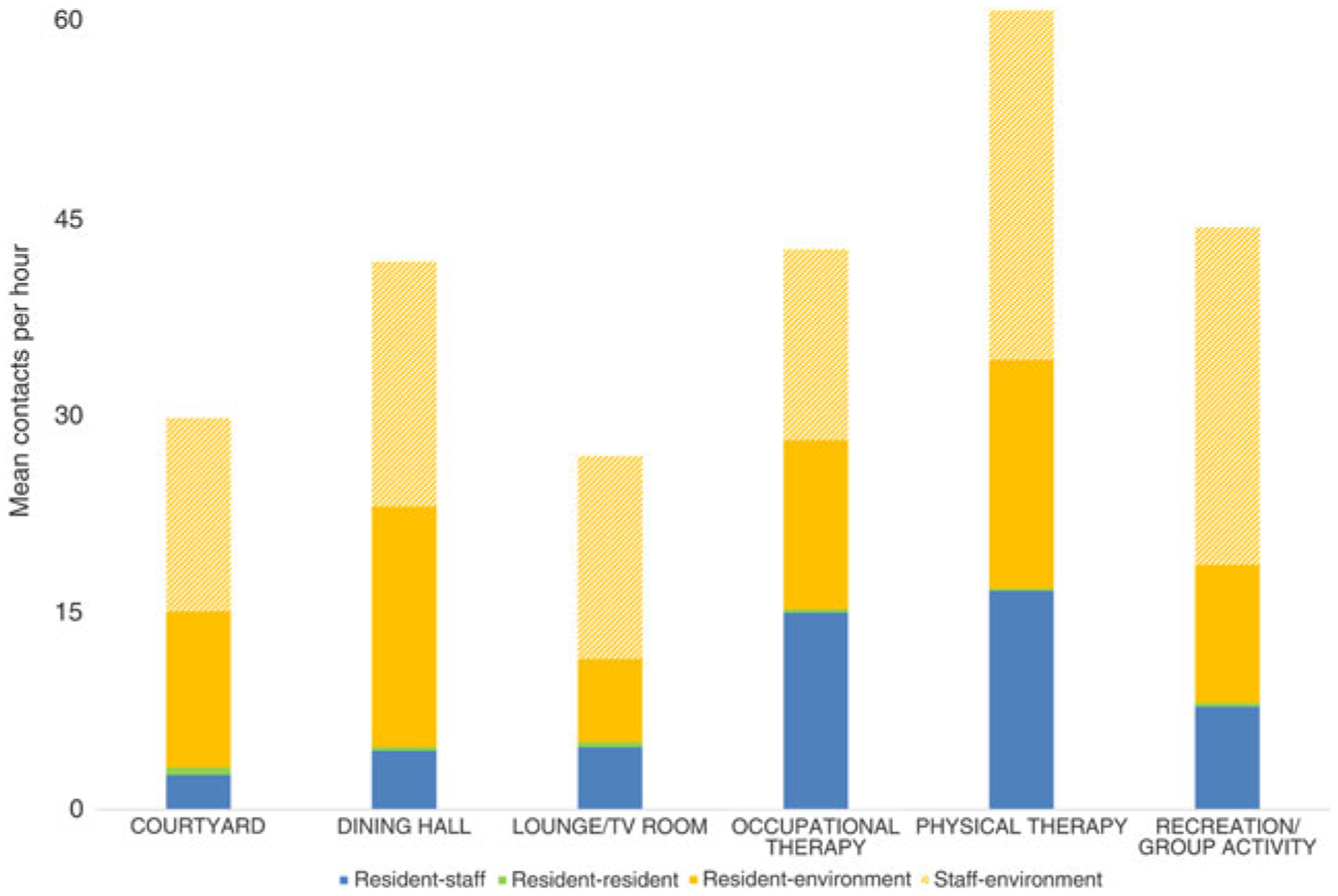
Frequency of contact per hour in common areas between nursing home residents and other residents, staff, and the environment across 8 long-term care facilities.
Discussion
Across 8 LTCFs in 6 states with >500 hours of observation, nursing home residents had frequent contact with staff and the environment outside of their rooms but rarely had contact with other residents.
Despite relatively high rates of multidrug-resistant organism (MDRO) colonization and infection in nursing homes, there is little research to guide nursing home infection prevention. Most infection control interventions in long-term care focus on standard precautions, including hand hygiene, which should be applied regardless of MDRO status. However, precautions for MDROs are usually limited to direct elements of care within a resident’s room. In its 2006 MDRO guideline, the Centers for Disease Control and Prevention (CDC) recommended that the resident’s clinical condition guide the decision for whether to employ contact precautions in LTCF; however, this recommendation lacks guidance about infection prevention outside resident rooms.5 This study was performed within the VA, which has a nationwide policy of glove and gown use for direct care of residents with methicillin-resistant Staphylococcus aureus (MRSA) colonization or infection, but this protocol is applied inside the resident’s room, not in common areas.6
Within these same 8 nursing homes, in our previous study, residents were visited relatively frequently within their rooms (4.3 visits per hour overall). Although barrier precautions were required for direct care within the room, compliance was low, with 58% of HCP using gloves and 34% using gowns.7 The frequency of contact with the patient or environment within the room was not monitored, so numbers between these 2 studies are not directly comparable. Therefore, we could not estimate the total amount of contact between residents and staff inside of rooms versus outside the rooms, but direct contact with staff was considerable in common areas, especially in rehabilitation. Staff performed hand hygiene and used gloves most often in the areas where contact with other residents and the environment were highest.
The role of the environment in the cross transmission of MDROs in long-term care facilities has been identified as an area of needed research.8 We found that residents had frequent contact with the environment of common areas, indicating that this maybe an important focus for frequent cleaning to prevent transmission.
The scope of this study was limited in that it was an exempt observational study. We were not able to collect information about which residents observed in common areas were on enhanced barrier precautions in their rooms. Additionally, although we excluded hospice and palliative care units, units we were not able to identify individual resident status as long-term, rehabilitation, etc. Finally, although staff were not told what the observers were doing, we cannot rule out the Hawthorne effect, which may have caused staff to modify their behavior.
In summary, residents of LTCFs had frequent contact with staff and the environment outside their rooms, areas that are not typically included in the nursing home’s infection control policies. In outbreak settings, environmental cleaning could be enhanced in areas with the most environmental contact. Guidance for infection control in long-term care must consider the need to balance the home-like environment for patients along with the reality that substantial contact occurs outside a resident’s room.
Acknowledgments.
We would like to thank the study coordinators Jwan Mohammadi (OR), Diana Sams (MI), Melissa Hibner (TX), Carol Ramos (FL), Alexandra Rochman (MA), Corey Lonberger (MA), Makaila Decker (MA), and Georgia Papaminas (MD). The contents do not represent the views of the US Department of Veterans Affairs or the United States Government.
Financial support.
This work was supported by Collaborative Research to Enhance and Advance Transformation and Excellence (CREATE) Initiative (grant no. HX-12-018) and Merit Review (grant no. I01 HX001128) from the United States Department of Veterans Affairs Health Services Research and Development Service (HSR&D).
Footnotes
Potential conflicts of interest.
All authors report no conflicts of interest relevant to this article.
References
- 1.Montoya A, Mody L Common infections in nursing homes: a review of current issues and challenges. Aging Health 2011;7:889–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cassone M, Mody L Colonization with multi-drug resistant organisms in nursing homes: scope, importance, and management. Curr Geriatr Rep 2015;4:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dantes R, Mu Y, Belflower R, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 2013;173:1970–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herzig CTA, Dick AW, Sorbero M, et al. Infection trends in US nursing homes, 2006–2013. J Am Med Dir Assoc 2017;18:635.e9–635.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siegel JD, Rhinehart E, Jackson M, Chiarello L, Health Care Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control 2007;35(10 suppl 2):S65–S164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Veterans Affairs. Revised Guideline for Implementation ofthe VHA MRSA Prevention Initiative in Community Living Centers. Washington, DC: Department of Veterans Affairs; 2013. [Google Scholar]
- 7.Pineles L, Petruccelli C, Perencevich EN, et al. The impact of isolation on healthcare worker contact and compliance with infection control practices in nursing homes. Infect Control Hosp Epidemiol 2018;39:683–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evans CT, Jump RL, Krein SL, et al. Setting a research agenda in prevention of healthcare-associated infections (HAIs) and multidrug-resistant organisms (MDROs) outside of acute care settings. Infect Control Hosp Epidemiol 2018;39:210–213. [DOI] [PMC free article] [PubMed] [Google Scholar]


