Abstract
This article updates the evidence base on outpatient behavioral treatments for adolescent substance use (ASU) since publication of the previous review completed for this journal by Hogue, Henderson, Ozechowski, and Robbins (2014). It first summarizes the Hogue et al. findings along with those from recent literature reviews and meta-analytic studies of ASU treatments. It then presents study design and methods criteria used to select 11 comparative studies subjected to Journal of Clinical Child and Adolescent Psychology level of support evaluation. These 11 studies are detailed in terms of their sample characteristics, methodological quality, and substance use outcomes. Cumulative level of support designations are then made for each identified treatment approach. These cumulative designations are virtually identical to those of the previous review: ecological family-based treatment, individual cognitive-behavioral therapy, and group cognitive-behavioral therapy remain well-established; behavioral family-based treatment and motivational interviewing remain probably efficacious; drug counseling remains possibly efficacious; and an updated total of 5 multicomponent treatments combining more than 1 approach (3 of which include contingency management) are deemed well-established or probably efficacious. Treatment delivery issues associated with evidence-based approaches are then reviewed, focusing on client engagement, fidelity and mediator, and predictor and moderator effects. Finally, to help accelerate innovation in ASU treatment science and practice, the article outlines promising horizons in improving youth identification and access, specifying and implementing pragmatic treatment in community settings, and leveraging emerging lessons from implementation science.
Identifying effective treatments for adolescent substance use (ASU) remains an urgent public health priority. ASU prevalence estimates from the most recent Monitoring the Future survey (Johnston, O’Malley, Bachman, & Schulenberg, 2016) indicate that 26% of eighth graders in the United States have tried alcohol, 16% have tried marijuana, and 21% have tried other illicit drugs. By 12th grade these rates more than double: 64% have tried alcohol, 45% marijuana, and 49% other illicit drugs.
As these prevalence rates attest, experimentation with alcohol and other substances is common during adolescence (Steinberg, 2007). A review by Hernandez, Lavingne, Wood, and Weirs (2015) concluded that substance use (SU) is typically initiated during adolescence, increases substantially across the teenage years, and decreases during the third decade of life. This pattern is remarkably consistent across countries and cultures, leading many to argue that SU disorders should be characterized as “developmental disorders” (Masten, Faden, Zucker, & Spear, 2008). Although substance experimentation is normative, about 5% of teenagers develop problems sufficient to meet psychiatric criteria for an SU disorder (Center for Behavioral Health Statistics and Quality, 2015). When adolescents with significant SU problems are left untreated, they face a cascade of far-reaching negative health outcomes that often persist into adulthood. Adverse health outcomes associated with ASU include sexually transmitted infections, unintended pregnancy, criminal involvement, school truancy, psychiatric disorders, and physical health problems (National Center on Addiction and Substance Abuse, 2011; Substance Abuse and Mental Health Services Administration [SAMHSA], 1999). Of immense concern, ASU is also associated with leading causes of death in this age cohort, including suicide, accidents, and violent crime (Keyes, Brady, & Li, 2015; Wong, Zhou, Goebert, & Hishinuma, 2013).
In recent years, the risks associated with ASU have received even greater attention due to national concerns about opioid misuse. Labeled a public health emergency by the president of the United States, opioid misuse— encompassing nonmedical use of prescription opioid-based medication (e.g., morphine, fentanyl) and use of illegal opiates (e.g., heroin)—has had a substantial impact on youth. Opioids are currently the most common cause of accidental death in the United States, and between 1999 and 2006 opioid overdoses increased more sharply among adolescents than any other age group (Edlund et al., 2015). At present, among 12th graders prescription and over-the-counter medications are the most commonly misused substances after alcohol, marijuana, and tobacco (Johnston et al., 2016), with one in every 100 youth between ages 12 and 17 reporting current opioid misuse (Center for Behavioral Health Statistics and Quality, 2016). Youth who use opioids are significantly more likely to use other substances as well (Johnston et al., 2016), and among youth younger than 21 who initiate heroin use, 80% had previously misused prescription and/or over-the-counter medication before the age of 18 (Cerdá, Santaella, Marshall, Kim, & Martins, 2015).
The pervasive negative consequences associated with ASU, and the high lethality of opioid misuse in particular, underscore a critical need to stay abreast of the latest evidence on effective ASU treatments. It is especially important to evaluate interventions delivered in outpatient settings, which host more than 80% of teenagers receiving ASU services (SAMHSA, 2014). A number of reviews and meta-analyses have analyzed the evidence supporting outpatient interventions for ASU, including two comprehensive reviews published in this journal (Hogue, Henderson, Ozechowski, & Robbins, 2014; Waldron & Turner, 2008). The goal of this article is to update the evidence since the review by Hogue et al. by evaluating comparative studies of outpatient behavioral treatments published between 2014 and 2017.
To accomplish this goal, the current review proceeds through several sections. First, we recap the findings from the prior two evidence base updates (EBUs) published in this journal, as well as results of literature reviews and meta-analytic studies of ASU outpatient treatment published since 2013. Next we detail the methods used to conduct the current review, including the scientific area of focus, search parameters, data extraction procedures, and evaluation criteria used to determine the Level of Support (Southam-Gerow & Prinstein, 2014) for each treatment approach. We then describe the 11 comparative trials selected for review and, using these, update the Level of Support designations presented in the 2014 EBU. We then review treatment delivery issues associated those approaches identified as Well-Established or Probably Efficacious, focusing on client engagement, fidelity and mediator, and predictor and moderator effects. Finally, we discuss promising areas of focus in ASU treatment science and practice.
PRIOR EVIDENCE BASE UPDATES
In the first EBU published in the Journal of Clinical Child and Adolescent Psychology (JCCAP), Waldron and Turner (2008) documented that protocol-based treatments for ASU were more effective than no treatment or usual care and classified discrete treatment models and broad treatment approaches into two categories of empirical support: Well-Established, which contained multidimensional family therapy (MDFT), functional family therapy (FFT), and group cognitive-behavioral therapy (CBT-G); and Probably Efficacious, which contained brief strategic family therapy (BSFT), behavioral family-based treatment (FBT-B), and multisystemic therapy (MST).
The more recent EBU by Hogue et al. (2014) updated Waldron and Turner via a cumulative review of studies published between 2007 and 2013, focusing on broad treatment approaches and refining the empirical support classifications. The revised Well-Established category included ecological family-based treatment (FBT-E), CBT-G, individual CBT (CBT-I), and two multicomponent treatments (i.e., treatment packages containing more than one evidence-based approach for ASU): motivational enhancement therapy + CBT (MET/CBT), and MET/CBT + FBT-B. The revised Probably Efficacious category included FBT-B, stand-alone motivational interviewing/MET (MI/MET), and two multicomponent treatments: FBT-E + contingency management (CM), and MET/CBT + FBT-B + CM. Finally, the category Possibly Efficacious was added to accommodate the drug counseling/12-step (DC/12) approach.
RECENT LITERATURE REVIEWS
Four ASU treatment literature reviews have been published since the 2014 EBU. Belendiuk and Riggs (2014) summarized approaches supported by two or more randomized trials. Several approaches were identified as “first-line” treatment: FBT-E, CBT, MI/MET, and CM. Brewer, Godley, and Hulvershorn (2017) reviewed ASU treatments as they applied to youth with co-occurring mental health disorders, concluding that multicomponent treatment combining FBT, DC/12, MI/MET, and CM was most effective for addressing ASU and comorbid disorders simultaneously. In both reviews, the authors lamented the posttreatment attenuation of the generally modest gains achieved during ASU treatment and emphasized the need for continuing care and other follow-up support services.
Carney, Myers, Louw, and Okwundu (2016) reviewed six studies of school-located MI-based interventions defined as brief interventions involving SU screening, data-based feedback, and efforts to increase personal responsibility for change. Results indicated no advantage of MI over information-only conditions and only moderate effectiveness for reducing cannabis and alcohol abuse/dependence when MI was compared to assessment only. The authors caution, however, that the quality of studies comparing MI versus assessment only was generally low. Stanger, Lansing, and Budney (2016) reviewed six studies of CM for decreasing adolescent cannabis use. Findings confirmed those in their prior review (Stanger & Budney, 2010) documenting CM effectiveness in reducing use during the course of treatment; however, posttreatment benefits were mixed, and the authors called for further research on the effects of specific CM incentive parameters (incentive magnitudes, targets, schedules, etc.).
META-ANALYTIC STUDIES
Seven ASU treatment meta-analyses have appeared since 2014: four focused on MI/MET, two focused on an FBT-E model, and one focused on culturally adapted treatment. Li, Zhu, Tse, Tse, and Wong (2016) analyzed 10 randomized trials comparing MI to standard practice among adolescents on measures of illicit SU, intention to use drugs, and attitudes toward ASU change. Findings indicated that MI did not result in reduced SU but might have impacted attitude change. Glass and colleagues (2015) analyzed 13 trials comparing alcohol-focused brief MI-based interventions (consisting of motivation building, counseling, and/or referral service) to standard procedures among adult and adolescent samples in medical settings. Findings indicated greater decreases in alcohol use among those in MI but insufficient evidence supporting MI utility for increasing linkage to treatment. Two other meta-analytic reviews of alcohol-focused, brief MI-based interventions widened the pool of studies to include both experimental and quasi-experimental research with adolescents and adults up to age 30; notably, only studies with nonactive comparison groups (i.e., no treatment, waitlist control, or standard care) were included. Tanner-Smith and Lipsey (2015) analyzed 185 studies (24 of which included adolescent samples) and found that MI was moderately effective in reducing alcohol consumption and related problems among adolescents, with effects maintained up to 1 year. MI with cognitive elements (e.g., goal setting, decisional balance exercises) produced stronger effects. Tanner-Smith and Risser (2016) analyzed 190 studies (26 with adolescent samples) and found that a calendar-based assessment approach (i.e., an interview-based process that permits the interviewer to boost the accuracy of participant reports by anchoring recall of SU consumption to specific calendar dates) was more sensitive than standard self-report strategies in detecting moderate-sized MI effects for alcohol use.
Two meta-analyses synthesized research on one FBT-E model, MDFT. Filges, Andersen, and Jørgensen (2015) examined five studies, including both experimental and quasi-experimental designs, containing youth enrolled in nonopioid treatment. Findings showed MDFT superior to various alternative treatments (CBT, peer group, multifamily educational therapy, usual care) in reducing ASU problem severity and frequency of use, though effects were small. Van der Pol and colleagues (2017) analyzed eight studies comparing MDFT to alternative treatments across a range of outcomes. Results showed generally small effects favoring MDFT. Moderator analyses demonstrated that youth with more severe ASU at intake benefitted to an even greater degree from MDFT than other treatments, evidenced by moderate effects for ASU.
Steinka-Fry and colleagues (2017) examined the effectiveness of culturally sensitive ASU treatment across eight studies. Half of the studies focused on FBT-E models, and some used quasi-experimental designs and/or were unpublished. Treatments that emphasized racial or ethnic-specific themes in their protocols (e.g., discrimination, acculturation, language barriers) were more effective for reducing SU overall, though effects did not emerge when comparing similar treatments that differed only on cultural elements.
CONTRIBUTIONS OF THE CURRENT REVIEW
These literature reviews and meta-analyses completed since the 2014 EBU reiterated the strength of FBT-E and CBT as Well-Established approaches for treating ASU. MI-based models received the most attention and continued their long-standing pattern of inconsistent performance as a stand-alone brief intervention across a variety of SU outcomes. This literature also highlights the need for further evaluation of culturally tailored interventions. The current review builds upon this prior literature as well as the 2014 EBU by (a) reviewing rigorous ASU treatment studies published since 2013; (b) updating research support designations for the full range of outpatient treatment approaches; (c) describing key factors that affect provision of ASU treatment, including a new focus on client engagement; and (d) describing promising horizons for the next generation of ASU treatment research.
METHOD
Study Inclusion Criteria
This EBU focuses on studies of outpatient behavioral treatment for ASU. The following parameters were used to delineate this area of treatment science. Adolescents were restricted to youth between the ages of 12 and 19. This age range was selected to exclude college students and older adolescents living independently, for whom there are context-specific educational and employment demands; sample characteristics of reviewed studies were vetted accordingly. Outpatient treatment was defined as care delivered in standard outpatient specialty and/or nonmedical settings, including treatment delivered by clinical practitioners in a school or court setting. We excluded studies conducted in residential, inpatient, emergency room, recreational, or foster care settings, as these settings have unique clinical workforce and milieu demands. Behavioral treatment included any nonpharmacological treatment approach designed explicitly to target acute SU. We excluded studies of continuum of care interventions such as Screening, Brief Intervention, and Referral to Treatment (SBIRT), as these primarily target linkage to treatment rather than SU reduction per se. We also excluded studies of follow-up care and adaptive treatment designs (e.g., Kaminer, Ohannessian, & Burke, 2017), as these focus primarily on posttreatment services retention and successive treatment episodes for those showing minimal initial benefits (Passetti, Godley, & Kaminer, 2016). Substance use was defined as consumption of alcohol or illicit drugs, or misuse of prescribed drugs, within the prior 30 days and/or presence of a diagnosable SU disorder. We excluded studies focused on tobacco or other nicotine products; nicotine cessation treatments constitute a large literature that features a variety of biological interventions and merits separate review.
In addition to the aforementioned criteria, studies had to meet the five methods criteria stipulated by JCCAP (see Table 1). These five criteria were interpreted as follows:
Group design: Adolescents needed to be randomly assigned to either the focal treatment condition or a logical comparison group (e.g., alternate treatment, assessment only, waitlist).
Independent variable defined: Manuals or a logical equivalent were used to implement the focal treatment condition.
Population clarified: As described previously, adolescents (ages 12–19) who used alcohol or illicit drugs at least once within the prior 30 days were the targets of intervention.
Outcomes assessed: Adolescents were assessed for SU at baseline prior to group assignment, using well-validated metrics. Adolescents were subsequently followed up for assessment at least 3 months after initiation of treatment.
Analysis adequacy: Each study condition contained at least 20 participants to ensure power to detect a reasonable effect. Attrition from each condition was reported and accounted for in study analyses using an intent-to-treat analytic approach.
TABLE 1.
Journal of Clinical Child and Adolescent Psychology Evidence Base Updates: Level of Support Evaluation Criteria
| Methods Criteria |
| M.1. Group design: Study involved a randomized controlled design |
| M.2. Independent variable defined: Treatment manuals or logical equivalent were used for the treatment |
| M.3. Population clarified: Conducted with a population, treated for specified problems, for whom inclusion criteria have been clearly delineated |
| M.4. Outcomes assessed: Reliable and valid outcome assessment measures gauging the problems targeted (at a minimum) were used |
| M.5. Analysis adequacy: Appropriate data analyses were used and sample size was sufficient to detect expected effects |
| Level 1: Well-Established Treatments |
| 1.1 Efficacy demonstrated for the treatment in at least two independent research settings and by two independent investigatory teams demonstrating efficacy by showing the treatment to be either: |
| 1.1.a. Statistically significantly superior to pill or psychological placebo or to another active treatment |
| OR |
| 1.1.b. Equivalent (or not significantly different) to an already well-established treatment in experiments |
| AND |
| 1.2. All five of the Methods Criteria |
| Level 2: Probably Efficacious Treatments |
| 2.1 There must be at least two good experiments showing the treatment is superior (statistically significantly so) to a waitlist control group |
| OR |
| 2.2 One or more good experiments meeting the Weil-Established Treatment level with the one exception of having been conducted in at least two independent research settings and by independent investigatory teams |
| AND |
| 2.3 All five of the Methods Criteria |
| Level 3: Possibly Efficacious Treatments |
| 3.1 At least one good randomized controlled trial showing the treatment to be superior to a waitlist or no-treatment control group |
| AND |
| 3.2 All five of the Methods Criteria |
| OR |
| 3.3 Two or more clinical studies showing the treatment to be efficacious, with two or more meeting the last four (of five) Methods Criteria, but none being randomized controlled trials |
| Level 4: Experimental Treatments |
| 4.1. Not yet tested in a randomized controlled trial |
| OR |
| 4.2. Tested in 1 or more clinical studies but not sufficient to meet Level 3 criteria. |
| Level 5: Treatments of Questionable Efficacy |
| 5.1. Tested in good group-design experiments and found to be inferior to other treatment group and/or waitlist control group; that is, only evidence available from experimental studies suggests the treatment produces no beneficial effect. |
Note. Adapted from Silverman and Hinshaw (2008) and Division 12 Task Force on Psychological Interventions’ reports (Chambless & Hollon, 1998; Chambless et al., 1996), from Chambless and Hollon (1998), and from Chambless and Ollendick (2001).
Search Strategy
To identify potentially eligible articles we conducted a literature search of Medline, PsycINFO, and the aggregated Social Sciences database on ISI Thompson’s Web of Knowledge. We created a set of search items based on a variety of addictive behaviors as well as addictive products such as alcohol, marijuana, cannabis, methamphetamine, and opiates/opioids. Another set of terms was formed to include different types of treatment models and approaches, including family therapy, motivational interviewing, cognitive-behavioral therapy, mindfulness/meditation, drug counseling, 12- step, seven challenges, and contingency management. We combined these two sets and limited the search to studies of outpatient ASU treatment published in English from 2013 onward (to cover publication lag for the 2014 EBU). The citation lists of identified articles were hand-searched to identify additional references (i.e., snowball sampling).
Article Review Procedures
Articles were subject to two rounds of review. Our primary goal was to identify new randomized comparative trials published since 2013. In addition, to capture the broadest evidence base, we included studies that extended the time window of follow-up assessment for a previously reviewed trial (e.g., a publication that reported 12-month outcomes for a trial that had previously had only 6-month outcomes reported). These follow-up studies were reviewed to extract new information but were not counted as new randomized trials when making determinations about the cumulative Level of Support for any given approach.
The first round of review was conducted by the first author and a professional librarian. Abstracts were hand-searched to identify randomized comparative trials focused on outpatient behavioral treatment for ASU, using the five JCCAP criteria. Abstracts that did not contain sufficient information to evaluate one or more criteria were automatically promoted to the second round. The second round of review was conducted by four reviewers (the study authors), with each article evaluated by two independent reviewers. Full articles were evaluated to ensure compliance with JCCAP criteria as defined in the Study Inclusion Criteria section. For those infrequent instances when paired raters disagreed on whether an article should be included, the article was discussed by all four authors until consensus was obtained.
Final Review Pool: Quality of Evidence and Level of Support Designations
For studies that passed both rounds of review and thereby entered the final review pool, each study’s methodological rigor was assessed using Nathan and Gorman’s (2002) Quality of Evidence criteria, which ranges from Type 1 (most rigorous) to Type 6 (least rigorous). Study inclusion criteria ultimately limited the final review pool to studies designated as Type 1 (those with random assignment, blinded assessment procedures, clear inclusion/exclusion criteria, replicable methods, sufficient power, sufficient follow-up period to judge durability of effects, and robust statistical methods) or Type 2 (some of the preceding methodological aspects missing but not considered fatally flawed). Level of Support designations were based on JCCAP criteria (listed in Table 1), which were shaped by Chambless et al. (1996), Chambless and Hollon (1998), and the Division 12 Task Force on Psychological Interventions.
RESULTS
Figure 1 depicts results of the review process, which adhered to guidelines of preferred reporting items for systematic reviews and meta-analyses (Moher, Liberati, Tetzlaff, Altman, & PRISMA Group, 2009). Eleven comparative studies composed the final review pool. Table 2 presents a detailed description of the study sample along with the Quality of Evidence (i.e., methodological strength) designation for each study. Table 3 presents the primary outcome measures and results of each study, including effect sizes (standardized indicators of the strength of the given effect) that were calculated for the main experimental comparison in each study. The following sections describe the SU outcomes reported by each study, specifying the primary substance(s) used and the SU metric (i.e., frequency, percentage of days abstinent, SU-related problems), as well as selected co-occurring behavioral health outcomes.
FIGURE 1.
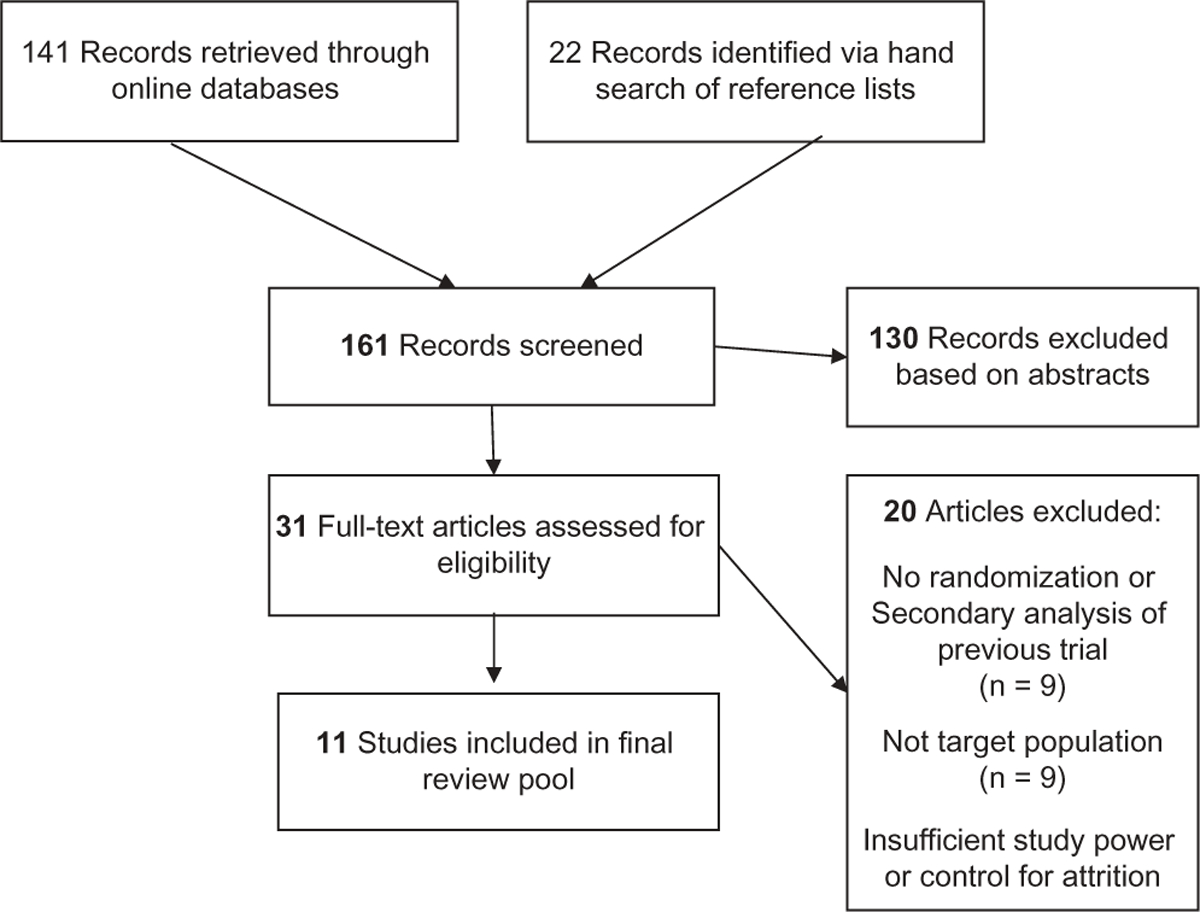
Flow chart of study selection.
TABLE 2.
Descriptive Information for the 11 Studies in the Current Review Pool
| Study | Substance Use Population | Demographic Characteristics | Treatment Conditions | Setting, Therapists, Training and Fidelity | Quality of Evidence |
|---|---|---|---|---|---|
| Cognitive-Behavioral Therapy | |||||
| Burrow-Sánchez et al, 2015 | Outpatient treatment; all met criteria for SUD | Age: 13–18 | Standard CBT-G (n = 36): 1.5 hr/week | Doctoral students trained by licensed psychologist. Therapists and supervisor reviewed videotaped sessions and completed adherence ratings. | 2 |
| Sex: 10% female | Culturally adapted CBT-G (n = 34): 1.5 hr/week | ||||
| Ethnicity: Hispanic 100%; 61% born in U.S.; 74% of mothers and 81% of fathers born in Mexico | |||||
| Henderson et al., 2016 | Adolescents under community supervision; 88% met criteria for SUD | Age: 12–17 | A-CRA (n = 63): weekly sessions of A-CRA over3–4 months followed by 12–14 weeks of continuing care | A-CRA: Trained and certified by model developers. Weekly supervision including audiotape review. | 1 |
| Sex: 26% female | UC (n = 63): variety of options ranging in intensity from drug education to weekly individual counseling | ||||
| Ethnicity: 79% White, 14% Hispanic, 6% African American | |||||
| Drug Counseling/12 Step | |||||
| Kelly et al., 2017 | Outpatient treatment; adolescents reported being abstinent for 35% of days in previous 90 | Age: 14–21 | DRC/12 (n = 29): 1 individual session followed by 8 group sessions | Weekly supervision with supervisor review of audio-recorded sessions. | 2 |
| Sex: 27% female | MET/CBT (n = 30): 2 individual MET sessions followed by 8 CBT-G sessions | ||||
| Ethnicity: 78% White, 8% African American, 5% Asian, 10% biracial | |||||
| Ecological Family-Based Treatment | |||||
| Dakof et al., 2015 | Juvenile drug court; all met criteria for SUD | Age: 13–18 | MDFT (n = 55): 2 sessions/week | MDFT: Trained and supervised by model developers. | 1 |
| Sex: 12% female Ethnicity: 59% Hispanic, 35% African American | CBT-G (n = 57): 3 sessions/week | CBT-G: Agency therapists. | |||
| Supervisors of both treatments reviewed all cases weekly. | |||||
| Horigian et al., 2015 | Outpatient treatment; 73% met criteria for SUD | Age: 13–17 | BSFT (n = 246): 12–16 sessions over 12 months | Community therapists randomized to condition. | 1 |
| Sex: 21% female | UC (n = 235): At least 1 session per week; expected to last 3–1 months | BSFT: Trained and supervised by model developers; 3-hr weekly group telephone supervision with BSFT supervisor. | |||
| Ethnicity: 31% White, 23% African American, 44% Hispanic | |||||
| Motivational Interviewing/Motivational Enhancement Therapy | |||||
| de Gee et al., 2014 | Non-treatment-seeking, cannabis-using adolescents in school/community settings; averaged 11.4 joints per week | Age: 14–21 | MI (n = 58): 2 sessions | Interventionists previously trained in MI. Received training in both conditions over 2 days. Single 20 min supervision session. | 2 |
| Sex: 26% female Ethnicity: 79% of Dutch descent | Information Only (n = 61): 1 session | ||||
| Walker et al., 2016 | School setting; average 37 days of cannabis use in previous 60 | Age: 14–18 | Both conditions received 2 sessions of MET | Lead author and clinical director provided training; ongoing individual and group supervision. Audiotaped sessions reviewed in group supervision. | 2 |
| Sex: 32% female | MI check-in (n = 128): 3 MET booster sessions | ||||
| Ethnicity: 59% White; 6% African American; 4% Asian; 20% multiracial | Assessment Only (n = 124): Assessments at same time points | ||||
| Winters et al., 2014 | School setting; 83% alcohol use disorder, 76% cannabis use disorder | Age: 13–17 | MI (n = 122): 2 sessions | Treatment provided in school setting. Supervision provided by model developer. Insufficient information provided on the frequency of supervision. | 1 |
| Sex: 54% female | MI + Parent Session (n = 114): 2 sessions + 1 parent session | ||||
| Ethnicity: 35% from ethnic minority groups | Attention control (n = 48): | ||||
| Multicomponent Models | |||||
| Letourneau et al., 2017 | Juvenile drug court; over 90% reported SU in previous 90 days, 31% testing SU positive at baseline | Age: 11–17 | FBT-E + CM + RR (n = 45): 6–7 months planned duration of family-based | Model developers provided FBT-E + CM + RR training and supervision. Weekly supervision with review of audiorecorded sessions. | 2 |
| Sex: 16% female Ethnicity: 33% White, 30% African American, 31% Hispanic | CM and family-based risk reduction UC (n = 60): 4 days/week first 12 weeks and 1–2 days/week second 12 weeks of group-based interventions | UC: No information given. | |||
| Rohde et al., 2014 | Outpatient treatment: comorbid SUD + depressive disorder | Age: 13–18 | FFT/CWD (n = 61): 12 sessions FFT followed by 12 sessions CWD | Model developers provided training. Weekly supervision with review of audiorecorded sessions. | 1 |
| Sex: 22% female | CWD/FFT (n = 56): 12 sessions CWD followed by 12 sessions FFT | ||||
| Ethnicity: 61% White, 28% Hispanic | Integrated FFT + CWD (n = 53): 4 family sessions followed by 10 weeks group and 2 additional sessions over 20 weeks | ||||
| Stanger et al., 2015 | Outpatient treatment: 100% met criteria for cannabis use disorder | Age: 12–18 | MET/CBT + FBT-B + CM (n = 51): 190-min session/week over 14 weeks + 1 parent training session per week | Model developers provided training. Weekly group supervision with review of videotaped sessions. | 1 |
| Sex: 11% female | MET/CBT + CM (n = 51): One 90-min session/week over 14 weeks with parents attending initial session. | ||||
| Ethnicity: 62% African American; 35% White | MET/CBT (n = 51): One 90-min session/week over 14 weeks with parents attending initial session. | ||||
Note. A-CRA = adolescent community reinforcement approach; BSFT = brief strategic family therapy; CBT = cognitive-behavioral therapy; CBT-G = group cognitive-behavioral therapy; CM = contingency management; DC/12 = drug counseling/12-step approach; FBT-B = behavioral family-based treatment; FBT-E = ecological family-based treatment; FFT = functional family therapy; MDFT = multidimensional family therapy; MET = motivational enhancement therapy; MI = motivational interviewing; SUD = substance use disorder; UC = usual care.
TABLE 3.
Main Findings from the 11 Studies in the Current Review Pool
| Study | Treatment Conditions | Substance Use Variables | Terminal Follow-Up Time Point and Effect Size: Small (s), Medium (m), Large (I) | Substance Use Key Findings | Other Notable Findings |
|---|---|---|---|---|---|
| Cognitive-Behavioral Therapy | |||||
| Burrow-Sánchez et al., 2015 | a. Standard CBT-G | TLFB: | 3-month FU: | Both conditions produced significant decreases in SU. No between-treatment differences. | Ethnic identity and familism moderated findings such that clients fared better with more culturally congruent models (e.g., adapted CBT-G more effective for teens with stronger ethnic identity, standard for teens with lesser ethnic identity). |
| b. Culturally adapted CBT-G | frequency of AOD use past 90 days | Between treatment: OR = 1.02s | |||
| Henderson et al., 2016 | a. A-CRA + ACC | GAIN: SFS (frequency AOD use past 90 days), SPS | 12-month FU: Between treatment: d = .39s/m (SFS); d = .98c (SPS) | Both conditions produced significant decreases in SU with. A-CRA + ACC showing more improvement. | None |
| b. UC | |||||
| Drug Counseling/12 Step | |||||
| Kelly et al, 2017 | a. DRC/12 | TLFB: %days of AOD abstinence past 90 | 9-month FU: Insufficient information provided to calculate effect sizes. | No between-treatment differences. | None |
| b. MET/CBT | |||||
| Ecological Family-Based Treatment | |||||
| Dakof et al., 2015 | a. MDFT | TLFB: | 24-month FU: | Both conditions produced significant decreases in SU. No between-treatment differences. | MDFT more effective for reducing externalizing symptoms, serious crimes, felony arrests. |
| b. CBT-G | Frequency of AOD use past 90 days | Between treatment: d=.01s | |||
| Horigian et al., 2015 | a. BSFT | TLFB: 30-day windows of frequency of AOD use over 1 year | 3- to 7-year FU: | No between-treatment differences. | BSFT lower externalizing symptoms, arrests, incarcerations. |
| b. UC | Between treatment: IRR = .095s | ||||
| Motivational Interviewing/Motivational Enhancement Therapy | |||||
| de Gee et al., 2014 | a. MI | Self-report: Mean weekly number of joints smoked in past 90 days | 3-month FU: | No between-treatment differences. | Those with heavier cannabis use showed greater CU reductions in MI than in control. |
| b. Information control | Between treatment: d = .03s,a | ||||
| Walker et al., 2016 | a. MI with boosters | GAIN: Days of cannabis use in past 60 | 15-month FU: | Both conditions produced significant decreases in SU. Boosters resulted in stronger effects at 6- month FU, but these not sustained through 15- month FU. | None |
| b. MI | Between treatment: d = .26s,b | ||||
| Winters et al., 2014 | a. MI | TLFB: Frequency of AOD use past 90 days | 12-month FU: | MI + Parent and MI associated with better SU outcomes than control; no differences found between the two experimental conditions. | Results mediated by client participation in additional services, motivation to change, and parenting practices. |
| b. MI + + Parent session | d = .23s | ||||
| c. Attention control | |||||
| Multicomponent Models | |||||
| Letourneau et al., 2017 | a. FBT-E + CM + RR | TLFB: Frequency of AOD use past 90 days | 12-month FU: | No between-treatment differences. | No between-treatment differences in risky sexual behavior. |
| b. UC | Between treatment: OR = .14m | ||||
| Rohde et al., 2014 | a. CWD/FFT | TLFB: % of days of AOD use in past | 12-month FU: Between treatment (FFT/CWD vs. | FFT/CWD produced better SU outcomes than FFT + CWD. CWD/FFT produced intermediate outcomes. | All conditions associated with decreased depressive symptoms. No between-treatment differences. |
| b. FFT/CWD | 90 | FFT+CWD): d = .52m,a | |||
| c. FFT + CWD | Between treatment (CWD/FFT vs. FFT +CWD): d = .52m,a | ||||
| Stanger et al, 2015 | a. MET/CBT + FBT-B | TLFB: % days cannabis abstinence past 90 | 12-month FU: | All conditions produced significant decreases in SU. MET/CBT + CM was associated with better outcomes than MET/CBT alone. | No between-treatment differences in externalizing symptoms or parenting outcomes. |
| b. MET/CBT + CM | Insufficient information provided to calculate effect sizes. | ||||
| c. MET/CBT | |||||
Note. A-CRA = adolescent community reinforcement approach; AOD = alcohol and other drug; BSFT = brief strategic family therapy; CBT = cognitive-behavioral therapy; CBT-G = group cognitive-behavioral therapy; CM = contingency management; CU = cannabis use; DC/12 = drug counseling/12-step approach; FBT-B = behavioral family-based treatment; FBT-E = ecological family-based treatment; FFT = functional family therapy; FU = follow-up; GAIN = global appraisal of individual needs; IRR = incidence rate ratio; MDFT = multidimensional family therapy; MET = motivational enhancement therapy; MI = motivational interviewing; OR = odds ratio; SFS = substance frequency scale; SPS = substance problem scale; TLFB = timeline follow-back interview; SU = substance use; UC = usual care.
Effect size calculated by subtracting mean score at terminal assessment of the comparison treatment from the mean score of the experimental treatment and dividing the resulting value by the standard deviation averaged across conditions.
Effect size calculated by dividing deviation from average linear slope for experimental group (assuming comparison coded 0 and experimental coded 1) by baseline standard deviation (Feingold, 2009).
Cognitive-Behavioral Therapy
Two studies examined CBT, one a CBT-I approach and the other CBT-G, both of which were designated Well-Established in the 2014 EBU. Henderson and colleagues (2016) completed an independent replication of Adolescent Community Reinforcement Approach (A-CRA), a CBT-I model that was tested against usual care provided to youth under community supervision by juvenile probation. Youth randomized to A-CRA also received 3 months of assertive continuing care (Godley, Godley, Dennis, Funk, & Passetti, 2002) following treatment. A-CRA was superior to usual care in decreasing SU-related problems and had moderate effects for frequency of alcohol and other drug (AOD) use at 1-year follow-up (FU). This replication study newly qualifies A-CRA as a Well-Established treatment model, a notable achievement previously reached by two FBT-E models (MDFT, FFT). Burrow-Sánchez, Minami, and Hops (2015) tested a CBT-G intervention incorporating cultural accommodations for Hispanic youth in the juvenile justice system against the standard CBT-G intervention from which it was developed. Both conditions produced significant decreases in frequency of AOD use at 3-month FU. Results were moderated by culturally relevant variables: The treatments were most effective when implemented in a culturally congruent manner. Hispanic youth with a stronger degree of ethnic identity, and families with higher self-ratings of familism, responded better to the culturally accommodated CBT-G intervention. However, the converse was also true in that youth with a lesser degree of ethnic identity, and families with lower self-ratings of familism, responded better to standard CBT-G.
Ecological Family-Based Treatment
Three trials evaluated FBT-E models. Dakof and colleagues (2015) tested MDFT against usual care featuring the CBT-G approach in a juvenile drug court setting. Treatments showed comparable decreases in AOD frequency and SU-related problems at 2-year FU. MDFT was superior in decreasing externalizing symptoms and serious delinquent activity (based on self-report and arrest records). Rohde, Waldron, Turner, Brody, and Jorgensen (2014) recruited substance-using youth with co-occurring depressive disorders and randomly assigned them to one of three outpatient treatment conditions: FFT delivered first, followed by an evidence-based group treatment for depression; depression treatment delivered first, followed by FFT; and FFT and depression interventions delivered simultaneously. FFT followed by depression treatment emerged as the most effective condition and produced significantly better SU outcomes (percentage of days of AOD use) at 1-year FU than the condition in which FFT and depression treatment occurred simultaneously. All three conditions were associated with improved depression symptoms, with no between-treatment differences emerging. Horigian and colleagues (2015) completed a 3- to 7-year FU of a trial testing BSFT against usual outpatient care that was included in the 2014 EBU (Robbins et al., 2011). As before there were no between-condition differences in frequency of AOD use, although BSFT produced larger reductions in externalizing problems and arrests.
Motivational Interviewing/Motivational Enhancement Therapy
Three studies tested MI/MET as a standalone treatment compared to no-treatment controls. Continuing a trend noted in the 2014 EBU, these studies recruited non-treatment-seeking adolescents outside traditional clinic settings. Winters, Lee, Botzet, Fahnhorst, and Nicholson (2014) completed a 1-year FU of a trial reviewed in the 2014 EBU (Winters, Fahnhorst, Botzet, Lee, & Lalone, 2012) comparing MI Only (two sessions with adolescent alone) and MI + Parent (adding one session with a primary caretaker) against assessment only in school settings. Results showed that MI Only and MI + Parent had greater SU improvement (cannabis use frequency, drug use consequences) than control. The two experimental conditions did not differ from one another. de Gee, Verdurmen, Bransen, De Jonge, and Schippers (2014) tested MI against information only in youth recruited from various school and community locations. Among heavier cannabis users, MI reduced cannabis use (quantity/frequency) more than did control at 3-month FU. Walker and colleagues (2016) provided two initial MET sessions to all participants and then randomized youth to (a) a series of MET booster sessions delivered 4, 7, and 10 months postinitial or (b) assessment only. Results showed that boosters were more effective than control in maintaining initial treatment gains in cannabis use outcomes (frequency, symptoms, consequences) at 6 months, but this advantage disappeared at subsequent assessment points through the terminal 15-month FU.
Drug Counseling/12-Step Facilitation
Kelly and colleagues (2017) completed one of the first studies with adolescents enrolled in outpatient SU treatment that tested the effectiveness of DC/12 using contemporary standards of controlled trials, including treatment standardization, fidelity monitoring, and supervisor review of taped sessions. A 10-session MET/CBT model (containing eight CBT-G sessions) was the comparison condition. Results showed no between condition differences in several indices of AOD use and SU related consequences at 9-month FU; moreover, there was no detectable change in the main SU variable (percentage days of AOD abstinence) across treatments.
Multicomponent Treatments
Three studies investigated multicomponent treatment packages. Stanger, Ryan, Scherer, Norton, and Budney (2015) compared three conditions using 12-session MET/CBT (containing 10 CBT-I sessions) as the base treatment in outpatient behavioral care: MET/CBT, MET/CBT + CM, and MET/CBT + CM + FBT-B. Youth in all conditions were offered 3 months of CM-based aftercare following treatment. Results indicated that adding CM, but not FBT-B, produced better SU results (percentage days of cannabis abstinence) during the treatment episode, but this advantage did not persist at 1-year FU. The conditions also showed equivalent improvements in adolescent psychopathology and parenting variables. Letourneau, McCart, Sheidow, and Mauro (2017) tested a three-component intervention consisting of FBT-E, family-based CM, and an educational intervention to reduce risky sexual behavior. In a drug-court setting, the experimental treatment produced no significant benefits over usual care in reducing frequency of AOD use or sexual risk at 1-year FU. The third study was the Kelly et al. (2017) trial previously described in which MET/CBT was a comparison condition.
Current Level of Support for ASU Outpatient Behavioral Treatment Approaches
The final Level of Support designations for ASU outpatient treatment approaches are presented in Table 4. Designations were determined based on the cumulative body of evidence to date, incorporating results covered in the 2014 EBU. Per JCCAP guidelines, interventions were classified by combining Format (individual, group, family) and Type (i.e., theoretical orientation/approach). Specific treatment models are listed under their respective approaches when appropriate. Regarding distinctions between Level of Support categories (Table 1), notable differences between Well-Established versus Probably Efficacious lie in the strength of the comparison condition (active treatment or placebo, vs. waitlist control) and demonstration of effects by an independent investigative team (required for the Well-Established level). The distinction between Probably Efficacious versus Possibly Efficacious is based primarily on the number of studies supporting the treatment in question.
TABLE 4.
Level of Support Designations for Adolescent Substance Use Treatment Approaches, with Supporting Citations
| Weil-Established Stand-Alone Treatments | |
|---|---|
| CBT-G | 2014 EBU |
| Burrow-Sánchez et al. (2015): culturally tailored CBT-G equivalent to standard CBT-G | |
| CBT-I |
|
| FBT-E |
|
| Well-Established Multicomponent Treatments | |
| MET/CBT | 2014 EBU |
| Kelly et al. (2017): Equivalent to DC/12 but no SU effects | |
| MET/CBT + FBT-B | 2014 EBU |
| Probably Efficacious Stand-Alone Treatments | |
| FBT-B | 2014 EBU |
| MI/MET | 2014 EBU |
| de Gee et al. (2014): Equivalent to information only Walker et al. (2016) (MET): MET boosters superior to MET only | |
| Winters et al. (2014) (MI + Parent session): Superior to assessment only; Equivalent to MI only | |
| Probably Efficacious Multicomponent Treatments | |
| FBT-E + CM | 2014 EBU |
| Letourneau et al. (2017): Equivalent to UC | |
| MET/CBT + FBT-B + CM | 2014 EBU |
| MET/CBT + CM | Stanger et al. (2015): Superior to MET/CBT |
| Possibly Efficacious Stand-Alone Treatments | |
| DC/12 | 2014 EBU |
| Kelly et al. (2017): Equivalent to MET/CBT but no | |
| SU effects | |
Note: A-CRA = adolescent community reinforcement approach; BSFT = brief strategic family therapy; CBT = cognitive-behavioral therapy; CBT-G = group cognitive-behavioral therapy; CBT-I = individual cognitive-behavioral therapy; CM = contingency management; DC/12 = drug counseling/12-step approach; EBU = evidence base update; FBT-B = behavioral family-based treatment; FBT-E = ecological family-based treatment; MDFT = multidimensional family therapy; MET = motivational enhancement therapy; MI = motivational interviewing; SU = substance use; UC = usual care.
A 2014 EBU reference maintains designations from previous review (Hogue et al., 2014). Please consult that review for references supporting specific designations.
Based on the current review, there are now five treatment approaches deemed Well-Established: FBT-E, CBT-G, CBT-I, MET/CBT, and MET/CBT + FBT-B. Another five approaches are deemed Probably Efficacious: FBT-B, MI/MET, FBT-E + CM, MET/CBT + CM, and MET/CBT + FBT-B + CM. One approach remains Possibly Efficacious: DC/12. These results provide strong continuity with the 2014 EBU, with only one newcomer (MET/CBT + CM) and no change in Level of Support designation for any holdover approach.
Key Factors in ASU Treatment Delivery
The 11 reviewed studies provide ongoing support for the effectiveness of a broad range of treatment approaches for ASU. Of course, equally important are factors that contribute to the success of these approaches. That is, whereas utilizing specific approaches clearly yields positive results, findings from comparative outcome studies generally fail to identify clinical processes that lead to successful outcomes. Next we discuss three treatment delivery factors that impact outcomes for evidence-based approaches: client engagement, fidelity and mediators, and predictors and moderators. In keeping with the focus of the current review, all studies included in this section evaluated approaches deemed Well-Established or Probably Efficacious.
Client Engagement
Examining client engagement is important for two reasons: Adolescents are notoriously difficult to engage in therapy (Lindsey et al., 2014), and engagement predicts outcomes (Diamond et al., 2006; Garnick et al., 2012; Joe, Knight, Becan, & Flynn, 2014). Definitions of client engagement vary widely and include the constructs of treatment attendance (Becker, Boustani, Gellatly, & Chorpita, 2017), service utilization (i.e., enrollment in an adjunctive service; Garnick et al., 2012), treatment readiness and motivation to change (De Jonge, Barelds, Schippers, & Schaap, 2009), and therapeutic relationships (e.g., therapeutic alliance, counselor rapport; Becker et al., 2017; Knight et al., 2016; Marcus, Kashy, Wintersteen, & Diamond, 2011). Engagement is most often operationalized as attendance (Lindsey et al., 2014), and although attendance alone does not fully capture a client’s strength of engagement (Becker et al., 2017), even this cursory index can be a valuable marker of success, as shown by positive associations between attendance and SU outcomes (Garner et al., 2009; Kelly et al., 2017; Walker et al., 2016).
Among the 11 studies in this review, six measured intervention-specific attendance, three measured service utilization, two measured motivation, and one measured youth satisfaction. Among those examining attendance, three documented no between-group differences (Burrow-Sánchez et al., 2015; Horigian et al., 2015; Stanger et al., 2015). Dakof and colleagues (2015) reported no group differences in monthly attendance, but MDFT was superior to CBT-G in retaining youth over time. Comparable between-group attendance rates were seen across conditions in Rohde et al. (2014); however, attendance was consistently lesser in the second of the sequenced FFT and depression interventions. Walker and colleagues (2016) reported lesser attendance in MET compared to assessment only. Regarding service utilization, Kelly and colleagues (2017) found greater participation in adjunctive 12-step meetings among youth in DC/12 compared to MET/CBT, and participation was associated with longer abstinence during early follow-up. But 12-step participation declined after treatment ended, suggesting the need for continuing care interventions. Youth in Walker et al. (2016) who received MET were more likely to initiate adjunctive CBT midway through the study; across conditions, youth with greater CBT participation had lower SU at 15-month follow-up. Winters and colleagues (2014) reported that MI + Parent interventions yielded increase use of additional services; also, the MI conditions overall fostered increased motivation to change compared to control. Few studies in the review pool examined other engagement constructs. Authors de Gee and colleagues (2014) measured treatment motivation but found no between-condition differences at 3-month follow-up. The single study that examined youth satisfaction reported high overall ratings but no differences between MET and assessment only (Walker et al., 2016).
These findings are consistent with prior research on the impact of evidence-based ASU treatment on client engagement. FBT-E has proven effective for increasing attendance compared to CBT-I (Hendriks, van der Schee, & Blanken, 2011), CBT-G (Dakof et al., 2015; Liddle, Dakof, Rowe, Henderson, & Greenbaum, 2009), and usual care (Rigter et al., 2013; Robbins et al., 2011). FBT-E also has a strong track record for strengthening therapeutic alliance (e.g., Diamond et al., 2006; Marcus et al., 2011; Robbins, Turner, Alexander, & Perez, 2003). MI/MET can increase treatment motivation (Dean, Britt, Bell, Stanley, & Collings, 2016; Winters et al., 2014), though advantages may not appear when intervention duration is brief (de Gee et al., 2014). It can also increase active participation (Stein et al., 2006) and youth satisfaction (D’Amico, Hunter, Miles, Ewing, & Chan Osilla, 2013; Walker et al., 2011). MI/MET is also effective for promoting adjunctive service use during treatment (Baer, Garrett, Beadnell, Wells, & Peterson, 2007; Walker et al., 2016), especially when featuring goal-setting and decisional balance activities (Tanner-Smith & Lipsey, 2015). Of interest, adding CM to multicomponent treatments that already include MI/MET may not further boost attendance (Stanger, Budney, Kamon, & Thostensen, 2009), though adding continuing care components may (Godley et al., 2010).
Treatment Fidelity and Mediators
This section reviews studies of treatment fidelity (extent and quality of therapist delivery of prescribed interventions) and mediators (relations between proximal changes in targeted client functioning and ultimate change in SU outcomes). All studies evaluated approaches deemed Well-Established or Probably Efficacious for ASU—CBT-I, FBT-E, MI/MET—and all directly linked fidelity or mediators to client outcomes.
Research on fidelity-outcome relations has continued to grow since the 2014 EBU. A hallmark of recent fidelity studies is reliance on rigorous methods for assessing treatment delivery, including observational coding. For example Campos-Melady, Smith, Meyers, Godley, and Godley (2017) examined data from a multisite evaluation of A-CRA that included observer ratings of therapist adherence (number of specific A-CRA procedures completed) and competence (skillfulness in delivering each procedure). Competence predicted decreased SU, as did adherence, albeit with a smaller sample of youth who attended the 1-year follow-up. This is one of few ASU studies to establish a direct link between therapist competence and client outcome. Gillespie, Huey, and Cunningham (2017) reported that greater adherence to the guiding principles of MST during the 1st month of therapy predicted posttreatment decreases in alcohol use and externalizing symptoms. Within a 20-year portfolio of MST fidelity studies showing that strong model adherence is needed to achieve optimal outcomes (summarized in Gillespie et al.), this is the first to use observational fidelity coding.
Mediator analyses are of keen interest for illuminating mechanisms of change, that is, targeted areas of client functioning that are directly impacted by treatment procedures and that, in turn, catalyze improvement in clinical symptoms (Holmbeck, 1997). Isolating mechanisms of change is critical for validating the clinical theory underlying a given intervention model and may assist in enhancing or streamlining clinical procedures to optimize their effectiveness and transportability (Kazdin, 1994). Despite the promise that such research holds for articulating how efficacious treatments work, the 2014 EBU identified only one mediator study of an evidence-based approach—an FBT-E model. The mediator research base on ASU treatments has expanded since that time, with at least seven new studies representing MI/MET and CBT.
In a study in the current review pool Winters and colleagues (2014) included mediator analyses demonstrating that improvements in motivation to change SU, parenting practices, and utilization of additional treatment services measured at 6 months following MI subsequently predicted decreases in SU at 12-month follow-up. Similarly, Blevins, Banes, Stephens, Walker, and Roffman (2016) found that positive change in SU motives during MET, particularly in youth rationale for consuming substances as a coping strategy, was associated with postintervention declines in SU and consequences of use. Barnett and colleagues (2014) reported that increases in client change talk—client verbalizations regarding intentions to change their SU patterns, which has been identified as a consistent mediator of MI effects in adult SU samples (Moyers et al., 2007)—mediated the relation between observer report of therapist MI skill and SU, such that more change talk predicted larger decreases in use. D’Amico and colleagues investigated a group-based MI intervention and determined that greater collective expressed commitment to reducing SU (“change talk”) mediated relations between observer-rated MI skill and reductions in SU intentions, expectancies, and consumption (D’Amico et al., 2015, 2013); conversely, verbalizations related to not reducing SU (“sustain talk”) were associated with worse outcomes (D’Amico et al., 2015). Regarding CBT, in a multisite implementation effort (the same data source used by Campos-Melady et al., 2017), Hunter, Godley, Hesson-McInnis, and Roozen (2014) found that delivery of A-CRA procedures predicted posttreatment reductions in youth illegal activity; moreover, reductions in illegal activity were partially explained by concurrent reductions in SU. Kaminer, Ohannessian, McKay, Burke, and Flannery (2018) showed that midtreatment therapist-reported commitment to abstinence goals, but not harm reduction goals, predicted improved outcomes in CBT for adolescents with alcohol use disorders.
Treatment Predictors and Moderators
Outcome predictor research addresses client, therapist, and contextual factors that enhance or mitigate treatment outcome relations (Holmbeck, 1997), supplying programmatic data about which treatments are most effective for which clinical groups (Kazdin, 1994), data that can be used to support the tailoring of treatments to fit the presenting problems of a given group or individual (Chorpita & Daleiden, 2014). There are two main categories of outcome predictors (Kraemer, Wilson, Fairburn, & Agras, 2002): Predictors, which refer to baseline factors that have a main effect on outcome, that is, predict client response equivalently across treatments, and Moderators, which refer to factors that have an interactive effect on outcome, that is, predict different response levels for different treatments.
Recent predictor studies by and large confirm long-standing findings that the presence of (a) more severe SU symptoms and/or (b) co-occurring behavioral disorders at baseline predict worse long-term SU outcomes. Babbin, Stanger, Scherer, and Budney (2016) reported that across three studies testing various combinations of MET/CBT and CM, more severe cannabis use predicted poorer long-term treatment response. Godley and colleagues (2017) found that opioid users participating in A-CRA, who collectively exhibited increased SU and emotional problems at intake, did not attain improvement levels reached by nonopioid users at 12-month follow-up, though they did show comparable client engagement and a steeper improvement curve. Yet, although greater baseline ASU severity usually portends worse outcomes, this effect must be interpreted with caution. As discussed by Godley et al., and others (e.g., Hogue, Henderson, & Schmidt, 2016), youth with worse baseline impairment can show relatively greater treatment progress due to there being “more room to grow,” though they do not typically pull even with less impaired youth. It is also important to note that the effect of co-occurring disorders on ASU treatment outcomes is not consistently negative. A review of 13 studies by Hersh, Curry, and Kaminer (2014) concluded that comorbid depression exerted a range of impacts on treatment attendance and outcomes: negative, positive, and nonsignificant.
An innovative study by Brown, Budney, Thostenson, and Stanger (2013) focused on a dynamic predictor variable: treatment progress. They determined that adolescents with a negative (vs. positive) urine screen at intake were more likely to register at least 1 week of abstinence by Week 6 of MET/CBT + CM. As important, virtually every teen who reported any abstinence during follow-up also registered at least 1 week of abstinence during the first 6 treatment weeks, leading the authors to surmise that the 6-week mark may represent a “responder” tipping point: If a teen shows no positive response by that mark, switching to higher treatment intensity or a different treatment approach may be warranted.
Regarding treatment moderators, Piehler and Winters (2017) showed that youth with impulsive/avoidant decision-making styles benefitted more from parental involvement in school-based MI than did those with constructive/rational styles, underscoring the value of caregiver involvement for teens who are more inclined to make riskier decisions. Another moderator study answered the 2014 EBU call for research that systematically integrates multiple similar data sets to generate enhanced power to explore subgroup effects (Curran & Hussong, 2009). Greenbaum and colleagues (2015) combined data from five trials testing MDFT against an active comparison group, aggregating 646 cases with 12-month outcomes. MDFT proved more effective than alternative approaches for male, African American, and White non-Hispanic youth, groups for which the pooled comparison conditions showed no mean improvement. Still, it remains true that race/ethnicity-based moderators rarely produce consistent results across studies. To wit: The 2014 EBU reported that another FBT-E model, BSFT, was effective for Hispanic but not African American youth (Robbins et al., 2008). And more recently Smith, Tabb, Fisher, and Cleeland (2014) found that racial status did not predict differences in SU outcomes for youth who did or did not participate in refusal skills training during A-CRA. A similar lack of consistency in moderator effects was reported in the 2014 EBU for another demographic characteristic, adolescent age. Finally, as previously discussed a meta-analysis Van der Pol and colleagues (2017) found that MDFT demonstrated greater benefits than various comparison treatments for youth with more severe baseline SU.
DISCUSSION
This review of the evidence base on outpatient behavioral treatment for ASU can serve several purposes for clinicians, researchers, and policymakers. Perhaps foremost is presenting Level of Support designations that can inform decisions about which treatments to adopt and retain for a given population of substance-using youth. Upon analyzing the 11 comparative trials selected for the current review, it is clear that the treatment selection guidelines articulated in the 2014 EBU remain fundamentally unchanged. Specifically, first, FBT-E is the preeminent Well-Established approach for ASU, and there are several manualized models from which to choose, including four (BSFT, FFT, MDFT, MST) managed by purveyor organizations that provide implementation support internationally, at substantial cost.
Second, CBT-I and CBT-G are Well-Established as stand-alone approaches. One specific CBT-I model, A-CRA, made the leap to being itself a Well-Established treatment. CBT-G may be optimally effective when combined with MI in the well-validated MET/CBT package, which comes in a variety of dosing options (five-, seven-, 10-, and 12-session versions). No cautionary studies surfaced to suggest that evidence-based group treatments such as CBT-G are prone to significant iatrogenic effects in the form of deviancy training among group members (Dodge, Dishion, & Lansford, 2006). Third, MI/MET continues to generate mixed evidence as a stand-alone approach and remains only Probably Efficacious for effecting long-term reductions in SU among treatment-seeking teenagers. It will be interesting to note how this designation matures over time as variations of MI, such as peer network counseling (Mason, Sabo, & Zaharakis, 2016), continue to be developed.
Fourth, there continues to be a dearth of comparative trials featuring DC/12, and the single study netted in the current review (Kelly et al., 2017) did not move the evidence needle beyond Possibly Efficacious. Controlled research on this widely practiced approach, including harm-reduction versions such as the Seven Challenges model (e.g., Korchmaros & Stevens, 2014), is a major priority for the field. Fifth, CM, though not tested or typically delivered as a stand-alone approach (Randall, 2017), is a popular ingredient of several multicomponent treatments that are Well-Established or Probably Efficacious. CM can be used as an individually oriented, clinic-based incentive system (e.g., Stanger et al., 2015) or incorporated into family-based interventions wherein parents collaborate with therapists to monitor teen performance and manage home-based incentive schedules (e.g., Letourneau et al., 2017; Stanger et al., 2015).
Along with Level of Support designations, a few significant themes emerged within the review pool. This pool continues the trend of focusing on treatments that include a FBT component (Rohde et al., 2014; Stanger et al., 2015), two of which (Dakof et al., 2015; Letourneau et al., 2017) were implemented in juvenile drug courts, a trend also observed in the 2014 EBU. This is not surprising given the success of FBT approaches for ASU and, from a developmental perspective, the centrality of family members in adolescents’ lives. This trend also reflects the impact of drug courts on policy innovations for addressing ASU. Notably, three of these studies showed positive FBT-E impacts on co-occurring symptoms. Another major takeaway is that multicomponent treatments continue to proliferate, accumulating an impressive empirical base for reducing ASU. Examples in the review pool are MET/CBT (Kelly et al., 2017; Stanger et al., 2015), MET/CBT + CM (Stanger et al., 2015), and FBT-E + CM (Letourneau et al., 2017). The pool also contains a test of an intervention tailored to a specific cultural group, in this case Hispanic youth (Burrow-Sánchez et al., 2015), illustrating potentially large benefits of developing culturally adapted ASU treatments (Steinka-Fry et al., 2017).
As this review illustrates, since the 2014 EBU there have been limited advances in discovering treatment delivery factors that contribute to successful outcomes in evidence-based approaches. Regarding the critical proximal outcome of client engagement, FBT-E is particularly effective at promoting treatment attendance and therapeutic alliance, whereas other approaches show mixed success. MI/MET has compelling evidence for improving SU treatment motivation and active participation, and evidence-based approaches overall are decidedly more effective than alternative treatment at increasing utilization of adjunctive services. Against that backdrop, identifying interventions that specifically promote all facets of engagement remains an urgent research priority. Kim and colleagues (2012) identified individual- (e.g., reminder calls) and family-oriented (e.g., intensive involvement with a parent) strategies as important for increasing attendance early in treatment, whereas service delivery-level strategies (e.g., attendance planning with the client) are valuable for ongoing retention and active participation. Other promising engagement practices include utilizing evidence-based assessment methods and promoting service accessibility (Lindsey et al., 2014), emphasizing psychoeducation and goal-setting interventions (Becker et al., 2017), incorporating family members in youth engagement efforts (Kirby et al., 2015), and directly targeting problem identification and motivation among youth (Becan, Knight, Crawley, Joe, & Flynn, 2015; Knight et al., 2016).
Recent studies on treatment fidelity reaffirmed that adherence to specific intervention techniques prescribed by empirically supported ASU treatments promotes better client outcomes for SU and also co-occurring problems. One study (Campos-Melady et al., 2017) also registered competence-outcome relations for a CBT-I model, an unusual finding that awaits replication for that approach and others. A relative bounty of five MI/MET collectively make a strong case that fidelity to MI/MET prompts increases in youth motivation to reduce SU and in their verbalized plans to reduce, which in turn predict improvements in several treatment outcomes. Finally, baseline SU severity and co-occurring problems have remained consistent (though clinically complex) predictors of posttreatment success, and new evidence suggests that positive clinical gains achieved early in therapy portend better outcomes. These predictors are therefore salient factors for guiding treatment tailoring and case planning. In contrast, reliable road maps for treatment selection and tailoring based on client demographics do not yet exist.
Multicomponent versus Multidomain ASU Treatments
Future reviews of outpatient treatments for ASU may find it useful to distinguish between multicomponent treatments, which contain multiple intervention components that target ASU, and multidomain treatments, which contain at least one component that targets a specific co-occurring disorder or behavioral problem. Treatment packages that target multiple domains of adolescent functioning are a vital asset for evidence-based ASU practice, given that the vast majority of youth receiving SU services also present with comorbid mental health disorders (Chan, Dennis, & Funk, 2008; Turner, Muck, Muck, Stephens, & Sukumar, 2004). One kind of multidomain treatment package is Combined treatment, in which ASU behavioral treatment is coordinated with pharmacological treatment for a given mental health disorder (e.g., Hogue, Evans, & Levin, 2017; Riggs et al., 2011; for attention disorders, 2007; for mood disorders). Protocols are available to help ASU clinicians incorporate medication decision-making interventions and medication management support into behavioral therapy sessions (e.g., Hogue, Lichvar, & Bobek, 2016).
A second kind of multidomain treatment package is Integrated treatment, in which at least one behavioral component targeting ASU is coordinated with at least one behavioral component targeting a co-occurring problem. Integrated models often proceed with concurrent delivery: implementing the two components simultaneously throughout treatment, as seen in Letourneau et al. (2017) for sexual risk reduction. ASU clinicians frequently incorporate aspects of trauma-focused CBT (see Morina, Koerssen, & Pollet, 2016) into treatment planning for their trauma-exposed clients (Suarez, Belcher, Briggs, & Titus, 2012). However, whereas Integrated SU plus Trauma interventions have produced success with adult populations (Roberts, Roberts, Jones, & Bisson, 2015), they have not been rigorously evaluated with ASU clients. A second option for Integrated treatment is to proceed with sequential delivery in which treatment focuses first on one disorder and then the other, as exemplified by Rohde et al. (2014) for depression. Sequential delivery may be preferred to concurrent delivery if the latter has negative evidence (see Babowitch & Antshel, 2016; Rohde et al., 2014; regarding depression) or the former has greater clinical appeal (see Adams et al., 2016 regarding trauma).
Overall, because focal behavioral treatment of ASU problems does not generally “spill over” to produce clinical gains for mental health symptoms (Ramchand, Griffin, Slaughter, Almirall, & McCaffrey, 2014), further research on Combined and Integrated packages for youth with co-occurring problems is needed to guide treatment planning. To serve this end we encourage the continued progression of component analysis studies on multicomponent and multidomain ASU treatments. As a prime example, additional research on the sequencing and timing of discrete treatment components within integrated models that promote best gains in both SU and co-occurring outcomes (as in Rohde et al., 2014) is sorely needed. Such research can deepen our understanding of which component interventions, delivered in which sequence and at what dose, yield optimal outcome and cost–benefit results for which kinds of clients.
Other Commonly Practiced Treatments
This review focused on ASU behavioral interventions supported by controlled research, which constitute the scientific foundation for evidence-based practice (Roberts, Blossom, Evans, Amaro, & Kanine, 2017). Yet there are numerous treatments commonly used in clinical practice that have not been tested in comparative trials, and several of these are endorsed by credible sources. One prevalent approach is recovery support services, which are broadly recommended by SAMHSA under the Recovery Oriented Systems of Care (ROSC) framework (see Laudet & Humphreys, 2013). Recovery support services comprise a range of interventions intended to support a lifestyle of sobriety, such as educational/vocational training, case management, and selfhelp methods, along with focal SU treatment. Specific ROSC models that target youth include (a) recovery management interventions (Fisher, 2014), such as assertive continuing care (Godley et al., 2002), that provide posttreatment support in the form of client engagement procedures, motivation enhancement, and normative SU feedback; (b) peer-based support services such as recovery coaching by peers in advanced stages of sobriety (Reif et al., 2014) and alternative peer groups that offer sober social gatherings along with standard recovery supports (Collier, Hilliker, & Onwuegbuzie, 2014); and (c) recovery high schools in which all students are enrolled in ASU treatment or aftercare (Finch, Moberg, & Krupp, 2014). The ROSC framework has not been formally tested for effectiveness (Laudet & Humphreys, 2013), and among the models listed here, only recovery management has empirical support for adolescents (but see Finch, Tanner-Smith, Hennessy, & Moberg, 2017, for promising quasi-experimental data on recovery high schools).
Another well-regarded approach is mindfulness-based relapse prevention, which seeks to reduce negative affect and substance cravings by increasing sensation/cognition awareness, positive reappraisals, and flexible responding to SU triggers (McConnell & Froeliger, 2015; Witkiewitz et al., 2014). Strong evidence exists for mindfulness-based interventions as a standalone treatment and when integrated with other approaches for adult SU (Li, Howard, Garland, McGovern, & Lazar, 2017; Witkiewitz et al., 2014). However, mindfulness has not established a solid research base for youth behavior problems (Kallapiran, Koo, Kirubakaran, & Hancock, 2015), and it remains virtually untested for ASU (Li et al., 2017).
Promising Horizons in ASU Treatment Science
By some yardsticks the intervening years between the 2014 EBU (which reviewed 19 studies) and the current review could be judged a relatively fallow period for ASU treatment science. Only 11 studies met the reasonable JCCAP inclusion criteria for methodological rigor, which de facto select for controlled trials; of these, two were alternative study designs—one tailoring (Burrow-Sánchez et al., 2015) and one parametric (Walker et al., 2016) study—and two reported follow-up results from previous trials (Horigian et al., 2015; Winters et al., 2014). Also, the review pool prompted no change in Level of Support for any approach and graduated only one stand-alone model to Well-Established. Disappointing? Or, instead, evidence that ASU treatment science has begun to retrench itself in earnest, exerting less effort pursuing (still indisputably valuable) comparative trials, and more effort pursuing strategies to help substance-using teens benefit from existing evidence-based interventions? With the latter pursuit in mind, we introduce three promising horizons in ASU science that, in conjunction with comparative trials, can help accelerate innovations in reducing unmet treatment needs and increasing the implementation and sustainment of quality treatment in routine service settings.
Improving Youth Identification and Access
Despite the abundance of empirically supported approaches and models to treat ASU, more than 90% of adolescents who meet diagnostic criteria for a SU disorder do not receive appropriate treatment (Center for Behavioral Health Statistics and Quality, 2015). This indicates that the well-validated interventions identified in this review are not reaching the vast majority of the intended consumer base, a treatment gap with significant individual and public health impacts (Hogue et al., 2014). The most endorsed strategy to remedy the troubling underidentification of ASU is widespread use of SBIRT procedures across youth-involved settings. SBIRT is a continuum-of-care approach designed to promote universal screening for SU in settings where adolescents can be readily accessed, such as schools, pediatric care, and child welfare services (SAMHSA, 2013). Universal screening is then followed by application of basic algorithms to match a given adolescent to the appropriate level of care: (a) brief advice; (b) a stand-alone brief intervention, typically rooted in the MI/MET approach, to modify SU behavior and enhance readiness to seek treatment; or (c) a brief intervention paired with referral to more intensive interventions (see Mitchell, Gryczynski, O’Grady, & Schwartz, 2013).
In theory these SBIRT elements are ideally suited to improve the detection of youth at risk for SU, create a viable pathway for those in need of services, and help to close the gap between treatment need and utilization (SAMHSA, 2013). These elements conform to comparable “services cascade” models that delineate best practices for helping at-risk youth transition across SU screening, assessment, referral, treatment initiation, and continuing care services (see Belenko et al., 2017, for an example from juvenile justice). In practice, however, data in support of SBIRT for ASU have been limited. The U.S. Preventative Services Task Force recently reviewed the evidence base in support of SBIRT and deemed it insufficient to recommend routine use of the model in pediatric primary care: Data on the effectiveness of screening plus brief intervention were inconsistent, and virtually no prior studies evaluated the effectiveness of referral to treatment (Moyer, 2013). As detailed in a recent review (Ozechowski, Becker, & Hogue, 2016), a primary reason why SBIRT has failed to fulfill its potential among adolescents may be insufficient consideration of the developmental appropriateness of the model. Building upon the extant literature and developmental theory, the authors recommended a set of adaptations to the SBIRT model to more optimally serve adolescents, including reliance on proactive (vs. reactive) procedures to identify and engage youth, involvement of a primary caregiver in all stages of the approach, and use of technology to streamline service delivery.
Indeed, technology-delivered assessment methods are an exciting and timely avenue for identifying substance-using youth and engaging them in services. Adolescents enjoy exceptional comfort with technology (Lenhart, 2015), perceive technology-delivered questionnaires to be more confidential than paper-based ones (Pedersen, Grow, Duncan, Neighbors, & Larimer, 2012), and report higher (and presumably more accurate) levels of SU on technology-delivered measures (Brener, Billy, & Grady, 2003). For providers, conducting assessments using computers or tablets can reduce administrative burden, decrease the likelihood of missed or inaccurate data, enable instantaneous scoring to inform assessment decisions, and seamlessly enhance existing medical records (Substance Abuse and Mental Health Services Administration, 2015). Technology-delivered assessment also allows for balancing flexibility with fidelity—content can be individually tailored and delivered at low cost and burden to providers (Substance Abuse and Mental Health Services Administration, 2015).
Another innovative strategy for reducing the ASU treatment gap is application of direct-to-consumer (DTC) marketing strategies to encourage adolescents and caregivers to request SU screening and intervention services, akin to strategies used to market psychiatric medication (Becker, 2015; Santucci, McHugh, & Barlow, 2012). Data from the National Household Survey on Drug Use and Health (Substance Abuse and Mental Health Services Administration, 2015) suggest that primary barriers to seeking ASU treatment include beliefs that treatment can’t help and lack of knowledge about where to look. DTC marketing (e.g., commercial advertisements, consumer education campaigns, informational pamphlets displayed in high-traffic areas) can increase client awareness of, and motivation to engage in, quality ASU care. DTC marketing efforts could also encourage parents to request comprehensive behavioral health screening from gateway service providers in a range of settings. Successes in other public health DTC marketing campaigns, including those focused on requests for medical services (Myers et al., 2006) and pharmaceutical treatments (Becker & Midoun, 2016), indicate that this approach may be useful for promoting ASU behavioral treatments as long as the language used is clear, easily understandable, and relevant to the target population (Becker, 2015). In recent years several national organizations that support behavioral health research, such as the National Institute on Drug Abuse and American Psychological Association, have attempted to promote health education about ASU for the public (see https://teens.drugabuse.gov/parents and http://www.effectivechildtherapy.com). However, work is needed to improve these campaigns by soliciting feedback from target groups about their unmet needs and communication preferences (Becker, Spirito, & Vanmali, 2016).
Full Commitment to Pragmatic Implementation: Descending the Treatment Specification Ladder
To advance the progress of implementation of evidence-based interventions (EBIs), treatment developers attempt to specify essential techniques and procedures in a manner that can be replicated with fidelity in routine care (McHugh & Barlow, 2010). EBIs exist along a continuum of specification defined by three intersecting dimensions: articulation of prescribed interventions, elaboration of ruledriven procedures for when and how interventions should be delivered, and customization of interventions for given clinical profiles. This continuum might be conceptualized as a treatment specification ladder, with upper rungs reaching ever-higher degrees of intervention prescription, formulaic service delivery, and target group delineation. Historically, EBI developers have perched on the highest rungs of the ladder, favoring a top-down implementation approach that emphasizes rigorous, multifaceted quality assurance procedures intended to bolster treatment standardization: extensive manuals and training toolkits, intensive on-site training, treatment integrity measures with feedback procedures, ongoing consultation with model experts, and renewable provider certification (Hogue, 2010). Higherrung quality procedures incur steeper adoption and sustainability costs due to accommodations required in agency infrastructure and supervision practices; resources needed for technical support; and workforce readiness barriers associated with clinician knowledge, incentives, and attitudes toward manualized EBIs (Gallo & Barlow, 2012).
A complementary but underutilized implementation strategy is a bottom-up approach that starts at what might be deemed the lowest rung of the treatment specification ladder: endeavor to bolster usual care practices that are already effective. Among the more surprising developments in the past two decades of effectiveness research on behavioral treatments is that usual care performs on par with manualized EBIs when the respective quality procedures (e.g., therapist hiring and training, clinical supervision) are roughly equivalent in scope and rigor. This pattern holds true for adult SU (e.g., Carroll et al., 2006; Morgenstern, Blanchard, Morgan, Labouvie, & Hiyaki, 2001), as well as youth behavioral health broadly (see Weisz, Krumholz, Santucci, Thomassin, & Ng, 2015) and may well apply to ASU, as suggested by a recent study in which FBT delivered by community therapists in everyday care achieved empirical benchmarks for treatment fidelity and long-term ASU outcome that had been established by research therapists in controlled trials (Hogue, Dauber, & Henderson, 2016). Defining the conditions that enable existing practices to achieve research-delineated outcome effects is an exciting new direction for ASU treatment science.
The second rung of the treatment specification ladder might contain brief EBIs delivered in one to two sessions, in line with principles advocating minimal intervention needed for change (Glasgow et al., 2014). A prime example are single-session interventions: mechanism-targeted interventions designed to deliver a cohesive and high-impact message that counters a specific maladaptive belief or behavior thought to underlie a given behavior problem (Schleider & Weisz, 2017a). Single-session interventions can produce lasting change in youth behavior across the spectrum of problem type and severity, often producing effect sizes comparable to those earned by multisession EBIs (Schleider & Weisz, 2017b). Introducing ASU-focused psychoeducation of this kind at the outset of treatment, perhaps integrated with brief MI interventions, could increase the potential for lasting treatment impacts among clients who dropout early (Becker et al., 2017).
The third rung of the specification ladder might contain a reduced set of EBIs that are common ingredients in multiple manualized treatments representing a given treatment approach for ASU. These distilled ingredients of full treatment models, known as core elements (Chorpita, Daleiden, & Weisz, 2005), are clinically granular and transdiagnostic interventions that can be (more) readily adopted by community providers, and (more) flexibly applied to a larger set of clinical problems, than full models (Weisz, Bearman, Santucci, & Jensen-Doss, 2017). Core element interventions for youth behavior problems have proven equivalent or superior to manualized treatment as well as usual care (Chorpita et al., 2017; Weisz et al., 2012), with effects maintained over two-year follow-up (Chorpita et al., 2013) and superior favorability among practitioners with regard to perceived effectiveness and flexibility (Chorpita et al., 2015). For ASU, core elements have been distilled for the FBT-E approach (Hogue, Bobek, et al., 2017) though not yet empirically tested: family engagement, relational reframe, relational emphasis, and interactional change interventions. Given the findings of this review, the path seems clear to distill core elements for CBT and perhaps DC/12 as well, with a “core practices” foundation for those two approaches already laid using adult SU models (Magill et al., 2016).
The fourth and highest rung of the specification ladder would contain focal manualized models designed for one specific disorder or problem cluster (Weisz et al., 2017). This is the most common variety of EBIs and constitutes the bulk of ASU treatments (stand-alone and multicomponent) in this review. As mentioned, focal models are usually supported by extensive quality assurance methods and thereby encounter stiff implementation barriers. If focal models are to thrive in usual care, providers will need to deliberately wean from demanding quality procedures coordinated by off-site model experts, supplanting those with intramural procedures maintained via routine agency resources. Research-supported, pragmatic options for reinforcing high-fidelity delivery of EBIs include in-house observational fidelity evaluation, tracking fidelity and outcome metrics against research-delineated benchmarks, and cultivating local expertise in clinical supervision of the EBIs (Hogue, Ozechowski, Robbins, & Waldron, 2013).
Leveraging Lessons from Implementation Science
Although the evidence base for ASU treatment continues to build, EBI adoption and implementation in ASU service contexts are inconsistent at best (Knudsen, 2009; National Institutes of Health, 2017). In complex service settings, organizational change efforts often require transdisciplinary teams and iterative approaches to implementation (Bauer, Damschroder, Hagedorn, Smith, & Kilbourne, 2015). In response, the growing field of implementation science has produced comprehensive theoretical frameworks that explicate the components required for successful EBI implementation (e.g., Aarons, Hurlburt, & Horwitz, 2011; Damschroder & Hagedorn, 2011; Simpson & Flynn, 2007). These frameworks provide research-informed guidance on the multilevel factors that influence the success of adopting, implementing, and sustaining EBIs in various settings. To conclude this EBU, we consolidate some primary lessons learned by implementation science and suggest how they might be applied to EBIs for ASU.
To prepare properly for change, significant time must be invested in exploration—the first stage in the organizational change process (Aarons et al., 2011; Langley et al., 2009). Initial exploration activities prior to ASU EBI roll-out might include identifying potential EBIs, assessing inner and outer context factors in the current environment, and identifying strategies to facilitate implementation. Outer context factors such as costs and training requirements can directly influence EBI adoption decisions (Damschroder & Hagedorn, 2011). Whereas the intensive training and certification requirements of some ASU EBIs boost fidelity (e.g., FBT-E models, MI), the cost to train staff may be prohibitive for underresourced agencies (Hogue et al., 2013). State or federal initiatives that encourage EBI use can promote widespread uptake, especially when accompanied by funding mechanisms (e.g., Godley, Garner, Smith, Meyers, & Godley, 2011). Inner context factors, such as organizational readiness to change, can also influence EBI implementation success. Targeted efforts to prepare an organization for change through agency self-assessment (Lehman, Simpson, Knight, & Flynn, 2011) and leadership training (Aarons, Ehrhart, Farahnak, & Hurlburt, 2015) show promise for promoting readiness. Tools to assist with exploration are available, including many endorsed by SAMHSA (https://www.samhsa.gov/EBI-web-guide/substance-abuse-treatment).
With regard to selecting implementation strategies that might be most effective within the local context, Powell and colleagues (2015) identified 73 discrete strategies that facilitate planning, educating staff, financing, restructuring the service delivery system, managing quality, and attending to policy issues. Strategy selection may depend in part on which EBI is being implemented. For example, when adding CM to a fully adopted FBT-E protocol, training alone (without intensive quality assurance) may be sufficient (see Henggeler, Chapman, Rowland, Sheidow, & Cunningham, 2013). Regrettably, there is scant research on how to select an effective implementation strategy, or on which strategies work best within which service contexts for which EBIs.
Even in organizations that are well prepared for change and for which suitable implementation strategies have been selected, modifications to the EBI itself may be necessary to ensure initial EBI-agency fit. To accomplish this, providers work closely with stakeholders to proactively modify elements of the EBI (retaining core elements; see earlier) as well as the service delivery environment, so that the new practice is comfortably integrated within existing clinical policies and procedures (Aarons et al., 2012). Balancing the seemingly opposing priorities of fidelity and feasibility often requires painstaking attention to all facets of EBI implementation, including measurement of EBI fidelity and impacts (Schoenwald et al., 2011).
Efforts to identify an appropriate EBI, prepare the setting, and implement the new (modified) practice should include EBI sustainment planning throughout the process (McHugh & Barlow, 2010). Recently, a promising sustainment strategy has emerged in which ongoing EBI adaptation takes precedence over fidelity to original protocols. Akin to rapid-cycle testing wherein EBI implementation activities are carried out incrementally (Langley et al., 2009; Taylor et al., 2013), a “dynamic” sustainment strategy (Aarons et al., 2012; Chambers, Glasgow, & Stange, 2013) is driven by balanced research-community partnerships wherein EBIs are continuously tested and improved to fit an evolving service context (a distinct departure from translational science methods aimed at optimizing EBIs and their mechanisms in a research crucible and then laboriously preparing agency environments for faithful protocol delivery). Progress toward meaningful sustainment of EBIs may depend on how adroitly each given service agency, and the field as a whole, negotiates the continuum defined by quality assurance versus dynamic improvement strategies. Data-oriented strategies specifically designed to foster the dynamic sustainability of EBIs in everyday settings may be particularly useful for facilitating this process (e.g., Chambers, Feero, & Khoury, 2016; Knight, Belenko, et al., 2016).
Finally, perhaps the most promising of all horizons in ASU treatment science is development of technology-delivered interventions, not only to support continuum-of-care procedures (as discussed in the Improving Youth Identification and Access section) but also to support the implementation of EBIs themselves. Technology-based communication has particular relevance for ASU treatment given the appeal of digital messaging and social media outlets among adolescents (Harris et al., 2017). Outcomes associated with technology-delivered interventions appear comparable to some counselor-led interventions (Bickle, Christensen, & Marsch, 2011) and have the added benefit of enhanced intervention fidelity, user responsiveness and enjoyment, cost efficiency, and treatment access (Carroll, 2013). In addition, widespread implementation of technology-delivered EBIs appears significantly more feasible than clinician-dependent EBIs, and electronic platforms can facilitate client customization (e.g., adapting intervention content and/or sequence to accommodate individual needs and preferences). For example, E-TREAT (VanDeMark et al., 2010) combines MI and support for change and tailors delivery of its intervention content based on a client’s responses to questions. Such customization is potentially appealing to providers and clients alike, maximizing the likelihood of uptake. Technology can also be a cost-efficient vehicle for supporting various facets of EBI implementation (provider training, ongoing evaluation and accountability, etc.). Noteworthy advances in technology-delivered EBIs have been made for treatments representing CBT (e.g., Carroll et al., 2008), MI/MET (e.g., VanDeMark et al., 2010), and FBT (Doss, Feinberg, Rothman, Roddy, & Comer, 2017), among others. As we march inexorably forward, technology-savvy research efforts will be invaluable for discovering which EBIs are most amenable to technology-based adaptations, how evolving technology can promote ever wider adoption and implementation efforts, and under what circumstances (e.g., for which clients in what settings) technology-delivered EBIs are best suited.
ACKNOWLEDGMENTS
We thank the librarian of the Center on Addiction, David Man, for his invaluable assistance in conducting the primary article search and reviewing abstracts for initial study inclusion.
Contributor Information
Aaron Hogue, Center on Addiction.
Craig E. Henderson, Department of Psychology, Sam Houston State University
Sara J. Becker, Center for Alcohol and Addictions Studies, Brown University School of Public Health
Danica K. Knight, Institute of Behavioral Research, Texas Christian University
REFERENCES
- Aarons GA, Ehrhart MG, Farahnak LR, & Hurlburt MS (2015). Leadership and organizational change for implementation (LOCI): A randomized mixed method pilot study of a leadership and organization development intervention for evidence-based practice implementation. Implementation Science, 10, 11. doi: 10.1186/s13012-014-0192-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Green AE, Palinkas LA, Self-Brown S, Whitaker DJ, Lutzker JR, … Chaffin MJ (2012). Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implementation Science, 7, 32. doi: 10.1186/1748-5908-7-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Hurlburt M, & Horwitz SM (2011). Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research, 38, 4–23. doi: 10.1007/s10488-010-0327-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams ZW, McCauley JL, Back SE, Flanagan JC, Hanson RF, Killeen TK, & Danielson CK (2016). Clinician perspectives on treating adolescents with co-occurring post-traumatic stress disorder, substance use, and other problems. Journal of Child & Adolescent Substance Abuse, 25, 575–583. doi: 10.1080/1067828X.2016.1153555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babbin SF, Stanger C, Scherer EA, & Budney AJ (2016). Identifying treatment response subgroups for adolescent cannabis use. Addictive Behaviors, 59, 72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babowitch JD, & Antshel KM (2016). Adolescent treatment outcomes for comorbid depression and substance misuse: A systematic review and synthesis of the literature. Journal of Affective Disorders, 201, 25–33. doi: 10.1016/j.jad.2016.04.018 [DOI] [PubMed] [Google Scholar]
- Baer JS, Garrett SB, Beadnell B, Wells EA, & Peterson PL (2007). Brief motivational intervention with homeless adolescents: Evaluating effects on substance use and service utilization. Psychology of Addictive Behaviors, 21, 582–586. doi: 10.1037/0893-164X.21.4.582 [DOI] [PubMed] [Google Scholar]
- Barnett E, Moyers TB, Sussman S, Smith C, Rohrback LA, Sun P, & Spruijt-Metz D (2014). From counselor skill to decreased marijuana use: Does change talk matter? Journal of Substance Abuse Treatment, 46, 498–505. doi: 10.1016/j.jsat.2013.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer MS, Damschroder L, Hagedorn HJ, Smith J, & Kilbourne AM (2015). An introduction to implementation science for the non-specialist. BMC Psychology, 3, 32. doi: 10.1186/s40359-015-0089-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becan JE, Knight DK, Crawley RD, Joe GW, & Flynn PM (2015). Effectiveness of the treatment readiness and induction program for increasing adolescent motivation for change. Journal of Substance Abuse Treatment, 50, 38–49. doi: 10.1016/j.jsat.2014.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker KD, Boustani M, Gellatly R, & Chorpita BF (2017). Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology, 47, 1–23. doi: 10.1080/15374416.2017.1326121 [DOI] [PubMed] [Google Scholar]
- Becker SJ (2015). Direct-to-consumer marketing: A complementary approach to traditional dissemination and implementation efforts for mental health and substance abuse interventions. Clinical Psychology: Science and Practice, 22, 85–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SJ, & Midoun MM (2016). Effects of direct-to-consumer advertising on patient prescription requests and physician prescribing: A systematic review of psychiatry-relevant studies. The Journal of Clinical Psychiatry, 77(10), e1293–e1300. doi: 10.4088/JCP.15r10325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SJ, Spirito A, & Vanmali R (2016). Perceptions of ‘Evidence-Based Practice’ among the consumers of adolescent substance use treatment. Health Education Journal, 5, 358–369. doi: 10.1177/0017896915581061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belendiuk KA, & Riggs P (2014). Treatment of adolescent substance use disorders. Current Treatment Options in Psychiatry, 1, 175–188. doi: 10.1007/s40501-014-0016-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belenko S, Knight D, Wasserman GA, Dennis ML, Wiley T, Taxman FS, … Sales J (2017). The Juvenile Justice Behavioral Health Services Cascade: A new framework for measuring unmet substance use treatment services needs among adolescent offenders. Journal of Substance Abuse Treatment, 74, 80–91. doi: 10.1016/j.jsat.2016.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickle WK, Christensen DR, & Marsch LA (2011). A review of computer-based interventions used in the assessment, treatment, and research of drug addiction. Substance Use and Misuse, 46, 4–9. doi: 10.3109/10826084.2011.521066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CE, Banes KE, Stephens RS, Walker DD, & Roffman RA (2016). Change in motives among frequent cannabis-using adolescents: Predicting treatment outcomes. Drug and Alcohol Dependence, 167, 175–181. doi: 10.1016/j.drugalcdep.2016.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener N, Billy J, & Grady W (2003). Assessment of factors affecting the validity of self-reported health-risk behaviors among adolescents: Evidence from the scientific literature. Journal of Adolescent Health, 33, 436–457. doi: 10.1016/S1054-139X(03)00052-1 [DOI] [PubMed] [Google Scholar]
- Brewer S, Godley MD, & Hulvershorn LA (2017). Treating mental health and substance use disorders in adolescents: What is on the menu? Current Psychiatry Reports, 19, 5. doi: 10.1007/s11920-017-0755-0 [DOI] [PubMed] [Google Scholar]
- Brown PC, Budney AJ, Thostenson JD, & Stanger C (2013). Initiation of abstinence in adolescents treated for marijuana use disorders. Journal of Substance Abuse Treatment, 44, 384–390. doi: 10.1016/j.jsat.2012.08.223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burrow-Sánchez JJ, Minami T, & Hops H (2015). Cultural accommodation of group substance abuse treatment for Latino adolescents: Results of an RCT. Cultural Diversity and Ethnic Minority Psychology, 21, 571–583. doi: 10.1037/cdp0000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos-Melady M, Smith JE, Meyers RJ, Godley SH, & Godley MD (2017). The effect of therapists’ adherence and competence in delivering the Adolescent Community Reinforcement Approach on client outcomes. Psychology of Addictive Behaviors, 31, 117–129. doi: 10.1037/adb0000216 [DOI] [PubMed] [Google Scholar]
- Carney T, Myers BJ, Louw J, & Okwundu CI (2016). Brief school-based interventions and behavioural outcomes for substance-using adolescents. Cochrane Database of Systematic Reviews, Issue 1, Art. No.: CD008969. doi: 10.1002/14651858.CD008969.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM (2013). Treatment integrity and dissemination: Rethinking fidelity via the stage model. Clinical Psychology: Science and Practice, 20, 99–106. [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, … Rounsaville BM (2008). Computer-assisted delivery of cognitive-behavioral therapy for addiction: A randomized trial of CBT4CBT. American Journal of Psychiatry, 165, 881–888. doi: 10.1176/appi.ajp.2008.07111835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, … Woody GE (2006). Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: A multisite effectiveness study. Drug and Alcohol Dependence, 81, 301–312. doi: 10.1016/j.drugalcdep.2005.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUH Series H-50). Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16–4984, NSDUH Series H-51). Rockville, MD: Substance Abuse and Mental Health Services Administration; Retrieved from http://www.samhsa.gov/data/ [Google Scholar]
- Cerdá M, Santaella J, Marshall BD, Kim JH, & Martins SS (2015). Nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: A national study. The Journal of Pediatrics, 167, 605–612. doi: 10.1016/j.jpeds.2015.04.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers DA, Feero WG, & Khoury MJ (2016). Convergence of implementation science, precision medicine, and the learning health care system: A new model for biomedical research. Jama, 315, 1941–1942. doi: 10.1001/jama.2016.3867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers DA, Glasgow RE, & Stange KC (2013). The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implementation Science, 8, 117. doi: 10.1186/1748-5908-8-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless DL, & Hollon S (1998). Defining empirically supported therapies. Journal of Consulting and Clinical Psychology, 66, 7–18. doi: 10.1037/0022-006X.66.1.7 [DOI] [PubMed] [Google Scholar]
- Chambless DL, & Ollendick TH (2001). Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology, 52(1), 685–716. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Sanderson WC, Shoham V, Bennett Johnson S, Pope KS, Crits-Christoph P, & McCurry S (1996). An update on empirically validated therapies. The Clinical Psychologist, 49, 5–18. [Google Scholar]
- Chan YF, Dennis ML, & Funk RR (2008). Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment, 34, 14–24. doi: 10.1016/j.jsat.2006.12.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, & Daleiden EL (2014). Structuring the collaboration of science and service in pursuit of a shared vision. Journal of Clinical Child & Adolescent Psychology, 43, 323–338. doi: 10.1080/15374416.2013.828297 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Park AL, Ward AM, Levy MC, Cromley T, … Krull JL (2017). Child STEPs in California: A cluster randomized effectiveness trial comparing modular treatment with community implemented treatment for youth with anxiety, depression, conduct problems, or traumatic stress. Journal of Consulting and Clinical Psychology, 85, 13–25. doi: 10.1037/ccp0000133 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, & Weisz JR (2005). Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research, 7, 5–20. doi: 10.1007/s11020-005-1962-6 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Park A, Tsai K, Korathu-Larson P, Higa-McMillan CK, Nakamura BJ, … Krull J (2015). Balancing effectiveness with responsiveness: Therapist satisfaction across different treatment designs in the Child STEPs randomized effectiveness trial. Journal of Consulting and Clinical Psychology, 83, 709–718. doi: 10.1037/a0039301 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Weisz JR, Daleiden EL, Schoenwald SK, Palinkas LA, & Miranda J; Research Network on Youth Mental Health. (2013). Long-term outcomes for the Child STEPs randomized effectiveness trial: A comparison of modular and standard treatment designs with usual care. Journal of Consulting and Clinical Psychology, 81, 999–1009. doi: 10.1037/a0034200 [DOI] [PubMed] [Google Scholar]
- Collier C, Hilliker R, & Onwuegbuzie A (2014). Alternative peer group: A model for youth recovery. Journal of Groups in Addiction & Recovery, 9, 40–53. doi: 10.1080/1556035X.2013.836899 [DOI] [Google Scholar]
- Curran PJ, & Hussong AM (2009). Integrative data analysis: The simultaneous analysis of multiple data sets. Psychological Methods, 14, 81–100. doi: 10.1037/a0015914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Houck JM, Hunter SB, Miles JN, Osilla KC, & Ewing BA (2015). Group motivational interviewing for adolescents: Change talk and alcohol and marijuana outcomes. Journal of Consulting and Clinical Psychology, 83, 68–80. doi: 10.1037/a0038155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Hunter SB, Miles JNV, Ewing BA, & Chan Osilla K (2013). A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first time alcohol or drug offense. Journal of Substance Abuse Treatment, 45, 400–408. doi: 10.1016/j.jsat.2013.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakof GA, Henderson CE, Rowe CL, Boustani M, Greenbaum PE, Wang W, … Liddle HA (2015). A randomized controlled trial of family therapy in juvenile drug court. Journal of Family Psychology, 29, 232–241. doi: 10.1037/fam0000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder LJ, & Hagedorn HJ (2011). A guiding framework and approach for implementation research in substance use disorders treatment. Psychology of Addictive Behaviors, 25, 194–205. doi: 10.1037/a0022284 [DOI] [PubMed] [Google Scholar]
- de Gee EA, Verdurmen JEE, Bransen E, de Jonge JM, & Schippers GM (2014). A randomized controlled trial of a brief motivational enhancement for non-treatment-seeking adolescent cannabis users. Journal of Substance Abuse Treatment, 47, 181–188. doi: 10.1016/j.jsat.2014.05.001 [DOI] [PubMed] [Google Scholar]
- de Jonge JM, Barelds DP, Schippers GM, & Schaap CP (2009). Motivation to change drinking habits: Development of a new instrument. Netherlands Journal of Psychology, 65, 102–111. doi: 10.1007/BF03080132 [DOI] [Google Scholar]
- Dean S, Britt E, Bell E, Stanley J, & Collings S (2016). Motivational interviewing to enhance adolescent mental health treatment engagement: A randomized clinical trial. Psychological Medicine, 46, 1961–1969. doi: 10.1017/S0033291716000568 [DOI] [PubMed] [Google Scholar]
- Diamond GS, Liddle HA, Wintersteen MB, Dennis ML, Godley SH, & Tims F (2006). Early therapeutic alliance as a predictor of treatment outcome for adolescent cannabis users in outpatient treatment. American Journal on Addictions, 15(Suppl 1), 26–33. doi: 10.1080/10550490601003664 [DOI] [PubMed] [Google Scholar]
- Dodge KA, Dishion TJ, & Lansford JE (2006). Deviant peer influences in programs for youth: Problems and solutions. New York, NY: Guilford Press. [Google Scholar]
- Doss BD, Feinberg LK, Rothman K, Roddy MK, & Comer JS (2017). Using technology to enhance and expand interventions for couples and families: Conceptual and methodological considerations. Journal of Family Psychology, 31, 983–993. doi: 10.1037/fam0000349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Forman-Hoffman VL, Winder CR, Heller DC, Kroutil LA, Lipari RN, & Colpe LJ (2015). Opioid abuse and depression in adolescents: Results from the National Survey on Drug Use and Health. Drug and Alcohol Dependence, 152, 131–138. doi: 10.1016/j.drugalcdep.2015.04.010 [DOI] [PubMed] [Google Scholar]
- Feingold A (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods, 14(1), 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filges T, Rasmussen PS, Andersen D, & Jørgensen AMK (2015). Multidimensional family therapy (MDFT) for young people in treatment for non-opioid drug use: a systematic review. Campbell Systematic Reviews, 11 (8). [Google Scholar]
- Finch AJ, Moberg DP, & Krupp AL (2014). Continuing care in high schools: A descriptive study of recovery high school programs. Journal of Child & Adolescent Substance Abuse, 23, 116–129. doi: 10.1080/1067828X.2012.751269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch AJ, Tanner-Smith E, Hennessy E, & Moberg DP (2017). Recovery high schools: Effect of schools supporting recovery from substance use disorders. The American Journal of Drug and Alcohol Abuse, 1–10. doi: 10.1080/00952990.2017.1354378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher EA (2014). Recovery supports for young people: What do existing supports reveal about the recovery environment? Peabody Journal of Education, 89, 258–270. doi: 10.1080/0161956X.2014.897104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo KP, & Barlow DH (2012). Factors involved in clinician adoption and nonadoption of evidence-based interventions in mental health. Clinical Psychology: Science and Practice, 19, 93–106. [Google Scholar]
- Garner BR, Godley SH, Funk RR, Dennis ML, Smith JE, & Godley MD (2009). Exposure to Adolescent Community Reinforcement Approach treatment procedures as a mediator of the relationship between adolescent substance abuse treatment retention and outcome. Journal of Substance Abuse Treatment, 36, 252–264. doi: 10.1016/j.jsat.2008.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnick DW, Lee MT, O’Brien PL, Panas L, Ritter GA, Acevedo A, … Godley MD (2012). The Washington circle engagement performance measures’ association with adolescent treatment outcomes. Drug and Alcohol Dependence, 124, 250–258. doi: 10.1016/j.drugalcdep.2012.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie ML, Huey SJ, & Cunningham PB (2017). Predictive validity of an observer-rated adherence protocol for multisystemic therapy with juvenile drug offenders. Journal of Substance Abuse Treatment, 76, 1–10. doi: 10.1016/j.jsat.2017.01.001 [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Fisher L, Strycker LA, Hessler D, Toobert DJ, King DK, & Jacobs T (2014). Minimal intervention needed for change: Definition, use, and value for improving health and health research. Translational Behavioral Medicine, 4, 26–33. doi: 10.1007/s13142-013-0232-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Hamilton AM, Powell BJ, Perron BE, Brown RT, & Ilgen MA (2015). Specialty substance use disorder services following brief alcohol intervention: A meta-analysis of randomized controlled trials. Addiction, 110, 1404–1415. doi: 10.1111/add.12950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk R, & Passetti LL (2002). Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. Journal of Substance Abuse Treatment, 23, 21–32. doi: 10.1016/S0740-5472(02)00230-1 [DOI] [PubMed] [Google Scholar]
- Godley MD, Passetti LL, Subramaniam GA, Funk RR, Smith JE, & Meyers RJ (2017). Adolescent community reinforcement approach implementation and treatment outcomes for youth with opioid problem use. Drug and Alcohol Dependence, 174, 9–16. doi: 10.1016/j.drugalcdep.2016.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley SH, Garner BR, Passetti LL, Funk RR, Dennis ML, & Godley MD (2010). Adolescent outpatient treatment and continuing care: Main findings from a randomized clinical trial. Drug and Alcohol Dependence, 110, 44–54. doi: 10.1016/j.drugalcdep.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley SH, Garner BR, Smith JE, Meyers RJ, & Godley MD (2011). A large-scale dissemination and implementation model for evidence-based treatment and continuing care. Clinical Psychology: Science and Practice, 18, 67–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenbaum PE, Wang W, Henderson CE, Kan L, Hall K, Dakof GA, & Liddle HA (2015). Gender and ethnicity as moderators: Integrative data analysis of multidimensional family therapy randomized clinical trials. Journal of Family Psychology, 29, 919–930. doi: 10.1037/fam0000127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris SK, Aalsma MC, Weitzman ER, Garcia-Huidobro D, Wong C, Hadland SE, … Ozer EM (2017). Research on clinical preventive services for adolescents and young adults: Where are we and where do we need to go? Journal of Adolescent Health, 60, 249–260. doi: 10.1016/j.jadohealth.2016.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson CE, Wevodau AL, Henderson SE, Colvourn SL, Gharagozloo L, North LW, & Lotts VA (2016). An independent replication of the adolescent-community reinforcement approach with justice-involved youth. The American Journal on Addictions, 25, 233–240. doi: 10.1111/ajad.12366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks V, van der Schee E, & Blanken P (2011). Treatment of adolescents with a cannabis use disorder: Main findings of a randomized controlled trial comparing multidimensional family therapy and cognitive behavioral therapy in The Netherlands. Drug and Alcohol Dependence, 19, 64–71. doi: 10.1016/j.drugalcdep.2011.05.021 [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Chapman JE, Rowland MD, Sheidow AJ, & Cunningham PB (2013). Evaluating training methods for transporting contingency management to therapists. Journal of Substance Abuse Treatment, 45, 466–474. doi: 10.1016/j.jsat.2013.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez L, Lavingne A, Wood M, & Weirs RW (2015). Moderators and mediators of treatments for youth with substance use disorders In Maric M, Prins PJM, & Ollendick TH(Eds.), Moderators and mediators of youth treatment outcomes (pp. 174–209). New York, NY: Oxford University Press. [Google Scholar]
- Hersh J, Curry JF, & Kaminer Y (2014). What is the impact of comorbid depression on adolescent substance abuse treatment? Substance Abuse, 35, 364–375. doi: 10.1080/08897077.2014.956164 [DOI] [PubMed] [Google Scholar]
- Hogue A (2010). When technology fails: Getting back to nature. Clinical Psychology: Science and Practice, 17, 77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Bobek M, Dauber S, Henderson CE, McLeod BD, & Southam-Gerow MA (2017). Distilling the core elements of family therapy for adolescent substance use: Conceptual and empirical solutions. Journal of Child & Adolescent Substance Abuse, 26, 437–453. doi: 10.1080/1067828X.2017.1322020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Dauber S, & Henderson CE (2016). Benchmarking family therapy for adolescent behavior problems in usual care: Fidelity, outcomes, and therapist performance differences. Administration and Policy in Mental Health and Mental Health Services Research. doi: 10.1007/s10488-016-0769-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Evans SW, & Levin FR (2017). A clinician’s guide to co-occurring ADHD among adolescent substance users: Comorbidity, neurodevelopmental risk, and evidence-based treatment options. Journal of Child & Adolescent Substance Abuse, 26, 277–292. doi: 10.1080/1067828X.2017.1305930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Ozechowski TJ, & Robbins MS (2014). Evidence base on outpatient behavioral treatments for adolescent substance use: Updates and recommendations 2007–2013. Journal of Clinical Child and Adolescent Psychology, 43, 697–720. doi: 10.1080/15374416.2014.915550 [DOI] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, & Schmidt AT (2016). Multidimensional predictors of treatment outcome in usual care for adolescent conduct problems and substance use. Administration and Policy in Mental Health and Mental Health Services Research. doi: 10.1007/s10488-016-0724-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Lichvar E, & Bobek M (2016). Pilot evaluation of the medication integration protocol for adolescents with ADHD in behavioral care: Treatment fidelity, acceptability, and utilization. Journal of Emotional and Behavioral Disorders, 24, 223–234. doi: 10.1177/1063426615611648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Ozechowski TJ, Robbins MS, & Waldron HB (2013). Making fidelity an intramural game: Localizing quality assurance procedures to promote sustainability of evidence-based practices in usual care. Clinical Psychology: Science and Practice, 20, 60–77. [Google Scholar]
- Holmbeck GN (1997). Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology, 65, 599–610. doi: 10.1037/0022-006X.65.4.599 [DOI] [PubMed] [Google Scholar]
- Horigian VE, Feaster DJ, Robbins MS, Brincks AM, Ucha J, Rohrbaugh MJ, … Szapocznik J (2015). A cross-sectional assessment of the long term effects of brief strategic family therapy for adolescent substance use. American Journal on Addictions, 24, 637–645. doi: 10.1111/ajad.12278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter BD, Godley SH, Hesson-McInnis MS, & Roozen HE (2014). Longitudinal change mechanisms for substance use and illegal activity for adolescents in treatment. Psychology of Addictive Behaviors, 28, 507–515. doi: 10.1037/a0034199 [DOI] [PubMed] [Google Scholar]
- Joe GW, Knight DK, Becan JE, & Flynn PM (2014). Recovery among adolescents: Models for post-treatment gains in drug abuse treatments. Journal of Substance Abuse Treatment, 46, 362–373. doi: 10.1016/j.jsat.2013.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston L, O’Malley P, Bachman J, & Schulenberg J (2016). Monitoring the future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Retrieved from http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf
- Kallapiran K, Koo S, Kirubakaran R, & Hancock K (2015). Effectiveness of mindfulness in improving mental health symptoms of children and adolescents: A meta-analysis. Child and Adolescent Mental Health, 20, 182–194. doi: 10.1111/camh.12113 [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Ohannessian CM, & Burke RH (2017). Adolescents with cannabis use disorders: Adaptive treatment for poor responders. Addictive Behaviors, 70, 102–106. doi: 10.1016/j.addbeh.2017.02.013 [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Ohannessian CM, McKay JR, Burke RH, & Flannery K (2018). Goal commitment predicts treatment outcome for adolescents with alcohol use disorder. Addictive Behaviors, 76, 122–128. doi: 10.1016/j.addbeh.2017.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE (1994). Methodology, design, and evaluation in psychotherapy research In Bergin A& Garfield S (Eds.), Handbook of psychotherapy and behavior change (4th ed., pp. 19–71). New York, NY: Wiley. [Google Scholar]
- Kelly JF, Kaminer Y, Kahler CW, Hoeppner B, Yetarian J, Cristello JV, & Timko C (2017). A pilot randomized clinical trial testing integrated 12-step facilitation (iTSF) treatment for adolescent substance use disorder. Addiction, 112, 2155–2166. doi: 10.1111/add.13920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Brady JE, & Li G (2015). Effects of minimum legal drinking age on alcohol and marijuana use: Evidence from toxicological testing data for fatally injured drivers aged 16 to 25 years. Injury Epidemiology, 2, 1. doi: 10.1186/s40621-014-0032-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Munson MR, & McKay MM (2012). Engagement in mental health treatment among adolescents and young adults: A systematic review. Journal of Child and Adolescent Social Work, 29, 241–266. doi: 10.1007/s10560-012-0256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KC, Versek B, Kerwin ME, Meyers K, Benishek LA, Bresani E, … Meyers RJ (2015). Developing Community Reinforcement and Family Training (CRAFT) for parents of treatment-resistant adolescents. Journal of Child & Adolescent Substance Abuse, 24, 155–165. doi: 10.1080/1067828X.2013.777379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight DK, Belenko S, Wiley T, Robertson AA, Arrigona N, Dennis M, … Wasserman GA (2016). Juvenile Justice—Translational Research on Interventions for Adolescents in the Legal System (JJ-TRIALS): A cluster randomized trial targeting system-wide improvement in substance use services. Implementation Science, 11, 57–74. doi: 10.1186/s13012-016-0423-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight DK, Joe GW, Crawley RD, Becan JE, Dansereau DF, & Flynn PM (2016). The effectiveness of the Treatment Readiness and Induction Program (TRIP) for improving during-treatment outcomes. Journal of Substance Abuse Treatment, 62, 20–27. doi: 10.1016/j.jsat.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen HK (2009). Adolescent-only substance abuse treatment: Availability and adoption of components of quality. Journal of Substance Abuse Treatment, 36, 195–204. doi: 10.1016/j.jsat.2008.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korchmaros JD, & Stevens SJ (2014). Examination of the role of therapeutic alliance, treatment dose, and treatment completion in the effectiveness of the seven challenges. Child and Adolescent Social Work Journal, 31, 1–24. doi: 10.1007/s10560-013-0307-3 [DOI] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883. doi: 10.1001/archpsyc.59.10.877 [DOI] [PubMed] [Google Scholar]
- Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, & Provost LP (2009). The improvement guide: A practical approach to enhancing organizational performance. New York, NY: Wiley & Sons. [Google Scholar]
- Laudet AB, & Humphreys K (2013). Promoting recovery in an evolving policy context: What do we know and what do we need to know about recovery support services? Journal of Substance Abuse Treatment, 45, 126–133. doi: 10.1016/j.jsat.2013.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehman WEK, Simpson DD, Knight DK, & Flynn PM (2011). Integration of treatment innovation planning and implementation: Strategic process models and organizational challenges. Psychology of Addictive Behaviors, 25, 252–261. doi: 10.1037/a0022682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart A (2015). Teens, social media, and technology overview. Pew Research Center. Retrieved from http://www.pewinternet.org/files/2015/04/PI_TeensandTech_Update2015_0409151.pdf
- Letourneau EJ, McCart MR, Sheidow AJ, & Mauro PM (2017). First evaluation of a contingency management intervention addressing adolescent substance use and sexual risk behaviors: Risk reduction therapy for adolescents. Journal of Substance Abuse Treatment, 72, 56–65. doi: 10.1016/j.jsat.2016.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Zhu S, Tse N, Tse S, & Wong P (2016). Effectiveness of motivational interviewing to reduce illicit drug use in adolescents: A systematic review and meta-analysis. Addiction, 111, 795–805. doi: 10.1111/add.v111.5 [DOI] [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, & Lazar M (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96. doi: 10.1016/j.jsat.2017.01.008 [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Rowe CR, Henderson C, & Greenbaum P (2009). Multidimensional family therapy for early adolescent substance abusers: Twelve month outcomes of a randomized controlled trial. Journal of Consulting and Clinical Psychology, 77, 12–25. doi: 10.1037/a0014160 [DOI] [PubMed] [Google Scholar]
- Lindsey MA, Brandt NE, Becker KD, Lee BR, Barth RP, Daleiden EL, & Chorpita BF (2014). Identifying the common elements of treatment engagement interventions in children’s mental health services. Clinical Child and Family Psychology Review, 17, 283–298. doi: 10.1007/s10567-013-0163-x [DOI] [PubMed] [Google Scholar]
- Magill M, Apodaca TR, Walthers J, Gaume J, Durst A, Longabaugh R, … Carroll KM (2016). The Alcohol Intervention Mechanisms Scale (AIMS): Preliminary reliability and validity of a common factor observational rating measure. Journal of Substance Abuse Treatment, 70, 28–34. doi: 10.1016/j.jsat.2016.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus DK, Kashy DA, Wintersteen MB, & Diamond GS (2011). The therapeutic alliance in adolescent substance abuse treatment: A one-with-many analysis. Journal of Counseling Psychology, 58, 449–455. doi: 10.1037/a0023196 [DOI] [PubMed] [Google Scholar]
- Mason MJ, Sabo R, & Zaharakis NM (2016). Peer network counseling as brief treatment for urban adolescent heavy cannabis users. Journal of Studies on Alcohol and Drugs, 78, 152–157. doi: 10.15288/jsad.2017.78.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Faden VB, Zucker RA, & Spear LP (2008). Underage drinking: A developmental framework. Pediatrics, 121(Suppl 4), S235–251. doi: 10.1542/peds.2007-2243A [DOI] [PubMed] [Google Scholar]
- McConnell PA, & Froeliger B (2015). Mindfulness, mechanisms and meaning: Perspectives from the cognitive neuroscience of addiction. Psychological Inquiry, 26, 349–357. doi: 10.1080/1047840X.2015.1076701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh R, & Barlow DH (2010). The dissemination and implementation of evidence-based psychological treatment: A review of current efforts. American Psychologist, 65, 73–84. doi: 10.1037/a0018121 [DOI] [PubMed] [Google Scholar]
- Mitchell SG, Gryczynski J, O’Grady KE, & Schwartz RP (2013). SBIRT for adolescent drug and alcohol use: Current status and future directions. Journal of Substance Abuse Treatment, 44, 463–472. doi: 10.1016/j.jsat.2012.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG; Prisma Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Blanchard KA, Morgan TJ, Labouvie E, & Hiyaki J (2001). Testing the effectiveness of cognitive-behavioral treatment for substance abuse in a community setting: Within treatment and posttreatment findings. Journal of Consulting and Clinical Psychology, 69, 1007–1017. doi: 10.1037/0022-006X.69.6.1007 [DOI] [PubMed] [Google Scholar]
- Morina N, Koerssen R, & Pollet TV (2016). Interventions for children and adolescents with posttraumatic stress disorder: A meta-analysis of comparative outcome studies. Clinical Psychology Review, 47, 41–54. doi: 10.1016/j.cpr.2016.05.006 [DOI] [PubMed] [Google Scholar]
- Moyer V (2013). Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine, 159, 210–218. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan JS, & Amrhein PC (2007). Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcholism, Clinical and Experimental Research, 31, 40s–47s. doi: 10.1111/j.1530-0277.2007.00492.x [DOI] [PubMed] [Google Scholar]
- Myers MF, Chang M-H, Jorgensen C, Whitworth W, Kassim S, Litch JA, … Irwin D (2006). Genetic testing for susceptibility to breast and ovarian cancer: Evaluating the impact of a direct-to-consumer marketing campaign on physicians’ knowledge and practices. Genetics in Medicine, 8, 361–370. doi: 10.1097/01.gim.0000223544.68475.6c [DOI] [PubMed] [Google Scholar]
- Nathan PE, & Gorman JM (2002). Efficacy, effectiveness, and the clinical utility of psychotherapy research In Nathan PE & Gorman JM (Eds.), A guide to treatments that work (2nd ed., pp. 642–654). New York, NY: Oxford University Press. [Google Scholar]
- National Center on Addiction and Substance Abuse. (2011). Adolescent substance use: America’s #1 public health problem. New York, NY: Author; Retrieved from http://www.centeronaddiction.org/addiction-research/reports/adolescent-substance-use [Google Scholar]
- National Institutes of Health. (2017). Office of behavioral and social sciences research strategic plan 2017–2021. Washington, DC: Author; Retrieved January 15, 2018, from, https://obssr.od.nih.gov/aboutus/strategic-plan/ [Google Scholar]
- Ozechowski TJ, Becker SJ, & Hogue A (2016). SBIRT-A: Adapting SBIRT to maximize developmental fit for adolescents in primary care. Journal of Substance Abuse Treatment, 62, 28–37. doi: 10.1016/j.jsat.2015.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passetti LL, Godley MD, & Kaminer Y (2016). Continuing care for adolescents in treatment for substance use disorders. Child and Adolescent Psychiatric Clinics, 25, 669–684. doi: 10.1016/j.chc.2016.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Grow J, Duncan S, Neighbors C, & Larimer ME (2012). Concurrent validity of an online version of the Timeline Followback assessment. Psychology of Addictive Behaviors, 26, 672. doi: 10.1037/a0027945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piehler TF, & Winters KC (2017). Decision-making style and response to parental involvement in brief interventions for adolescent substance use. Journal of Family Psychology, 31, 336–346. doi: 10.1037/fam0000266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, … Kirchner JE (2015). A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation Science, 10, 21. doi: 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchand R, Griffin BA, Slaughter ME, Almirall D, & McCaffrey DF (2014). Do improvements in substance use and mental health symptoms during treatment translate to long-term outcomes in the opposite domain? Journal of Substance Abuse Treatment, 47, 339–346. doi: 10.1016/j.jsat.2014.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall J (2017). Challenges and possible solutions for implementing contingency management for adolescent substance use disorder in community based settings. Journal of Child & Adolescent Substance Abuse, 26(4), 332–337. [Google Scholar]
- Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, … Delphin-Rittmon ME (2014). Peer recovery support for individuals with substance use disorders: Assessing the evidence. Psychiatric Services, 65, 853–861. doi: 10.1176/appi.ps.201400047 [DOI] [PubMed] [Google Scholar]
- Riggs PD, Mikulich-Gilbertson SK, Davies RD, Lohman M, Klein C, & Stover SK (2007). A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Archives of Pediatric and Adolescent Medicine, 161, 1026–1034. doi: 10.1001/archpedi.161.11.1026 [DOI] [PubMed] [Google Scholar]
- Riggs PD, Winhusen T, Davies RD, Leimberger JD, Mikulich-Gilbertson S, Klein C, & Liu D (2011). Randomized controlled trial of osmotic-release methylphenidate with cognitive-behavioral therapy in adolescents with Attention-Deficit/Hyperactivity Disorder and Substance Use Disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 903–914. doi: 10.1016/j.jaac.2011.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigter H, Henderson CE, Pelc I, Tossmann P, Phan O, Hendriks V, & Rowe CL (2013). Multidimensional family therapy lowers the rate of cannabis dependence in adolescents: A randomised controlled trial in Western European outpatient settings. Drug and Alcohol Dependence, 130, 85–93. doi: 10.1016/j.drugalcdep.2012.10.013 [DOI] [PubMed] [Google Scholar]
- Robbins MS, Feaster DJ, Horigian VE, Rohrbaugh M, Shoham V, Bachrach K, … Szapocznik J (2011). Brief strategic family therapy versus treatment as usual: Results of a multisite randomized trial for substance-using adolescents. Journal of Consulting and Clinical Psychology, 79, 713–727. doi: 10.1037/a0025477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins MS, Szapocznik J, Dillon FR, Turner CW, Mitrani VB, & Feaster DJ (2008). The efficacy of structural ecosystems therapy with drug-abusing/dependent African American and Hispanic American adolescents. Journal of Family Psychology, 22, 51–61. doi: 10.1037/0893-3200.22.1.51 [DOI] [PubMed] [Google Scholar]
- Robbins MS, Turner CW, Alexander JF, & Perez GA (2003). Alliance and dropout in family therapy for adolescents with behavior problems: Individual and systemic effects. Journal of Family Psychology, 17, 534–544. doi: 10.1037/0893-3200.17.4.534 [DOI] [PubMed] [Google Scholar]
- Roberts MC, Blossom JB, Evans SC, Amaro CM, & Kanine RM (2017). Advancing the scientific foundation for evidence-based practice in clinical child and adolescent psychology. Journal of Clinical Child & Adolescent Psychology, 46, 915–928. doi: 10.1080/15374416.2016.1152554 [DOI] [PubMed] [Google Scholar]
- Roberts NP, Roberts PA, Jones N, & Bisson JI (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review, 38, 25–38. doi: 10.1016/j.cpr.2015.02.007 [DOI] [PubMed] [Google Scholar]
- Rohde P, Waldron HB, Turner CW, Brody J, & Jorgensen J (2014). Sequenced versus coordinated treatment for adolescents with comorbid symptoms and substance use disorders. Journal of Consulting and Clinical Psychology, 82, 342–348. doi: 10.1037/a0035808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santucci LC, McHugh RK, & Barlow DH (2012). Direct-to-consumer marketing of evidence-based psychological interventions: Introduction. Behavior Therapy, 43, 231–235. doi: 10.1016/j.beth.2011.07.003 [DOI] [PubMed] [Google Scholar]
- Schleider JL, & Weisz JR (2017a). Can less be more? The promise (and perils) of single-session youth mental health interventions. The Behavior Therapist, 7, 256–261. [Google Scholar]
- Schleider JL, & Weisz JR (2017b). Little treatments, promising effects? Meta-Analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 107–115. doi: 10.1016/j.jaac.2016.11.007 [DOI] [PubMed] [Google Scholar]
- Schoenwald SK, Garland AF, Chapman JE, Frazier SL, Sheidow AJ, & Southam-Gerow MA (2011). Toward the effective and efficient measurement of implementation fidelity. Administration and Policy in Mental Health and Mental Health Services Research, 38, 32–43. doi: 10.1007/s10488-010-0321-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, & Hinshaw SP (2008). The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal Of Clinical Child & Adolescent Psychology, 37 (1), 1–7. [DOI] [PubMed] [Google Scholar]
- Simpson DD, & Flynn PM (2007). Moving innovations into treatment: A stage-based approach to program change. Journal of Substance Abuse Treatment, 33, 111–120. doi: 10.1016/j.jsat.2006.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DC, Tabb KM, Fisher D, & Cleeland L (2014). Drug refusal skills training does not enhance outcomes of African American adolescents with substance use problems. Journal of Substance Abuse Treatment, 46, 274–279. doi: 10.1016/j.jsat.2013.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southam-Gerow MA, & Prinstein MJ (2014). Evidence base updates: The evolution of the evaluation of psychological treatments for children and adolescents. Journal of Clinical Child & Adolescent Psychology, 43, 1–6. doi: 10.1080/15374416.2013.855128 [DOI] [PubMed] [Google Scholar]
- Stanger C, & Budney AJ (2010). Contingency management approaches for adolescent substance use disorders. Child and Adolescent Psychiatry Clinics of North America, 19, 547–562. doi: 10.1016/j.chc.2010.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Budney AJ, Kamon JL, & Thostensen J (2009). A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug and Alcohol Dependence, 105, 240–247. doi: 10.1016/j.drugalcdep.2009.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Lansing AH, & Budney AJ (2016). Advances in research on contingency management for adolescent substance use. Child and Adolescent Psychiatric Clinics of North America, 25, 645–659. doi: 10.1016/j.chc.2016.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Ryan SR, Scherer EA, Norton GE, & Budney AJ (2015). Clinic- and home-based contingency management plus parent training for adolescent cannabis use disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 445–453. doi: 10.1016/j.jaac.2015.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R, & Miranda R (2006). Enhancing substance abuse treatment engagement in incarcerated adolescents. Psychological Services, 3, 25–34. doi: 10.1037/1541-1559.3.1.0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L (2007). Risk taking in adolescence: New perspectives from brain and behavioral science. Current Directions in Psychological Science, 16, 55–59. doi: 10.1111/j.1467-8721.2007.00475.x [DOI] [Google Scholar]
- Steinka-Fry KT, Tanner-Smith EE, Dakof GA, & Henderson C (2017). Culturally sensitive substance use treatment for racial/ethnic minority youth: A meta-analytic review. Journal of Substance Abuse Treatment, 75, 22–37. doi: 10.1016/j.jsat.2017.01.006 [DOI] [PubMed] [Google Scholar]
- Suarez LM, Belcher HM, Briggs EC, & Titus JC (2012). Supporting the need for an integrated system of care for youth with co-occurring traumatic stress and substance abuse problems. American Journal of Community Psychology, 49, 430–440. doi: 10.1007/s10464-011-9464-8 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (1999). Treatment of adolescents with substance use disorders. Treatment improvement protocol (TIP) Series, No. 32. Rockwell, MD: SAMHSA. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2013). Systems-level implementation of screening, brief intervention, and referral to treatment. Technical Assistance Publication (TAP) Series 33. HHS Publication No. (SMA) 13–4741. Rockville, MD: SAMHSA. [Google Scholar]
- Substance Abuse and Mental Health Services Administration; (2014). Discharges from substance abuse treatment services (Treatment Episode Data Set (TEDS): 2011. BHSIS Series S-70, HHS Publication No. (SMA) 14–4846). Rockville, MD: SAMHSA. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2015). Results from the 2015 National Household Survey on Drug Use and Health Center for behavioral health statistics and quality. Rockville, MD: SAMHSA. [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 51, 1–18. doi: 10.1016/j.jsat.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Risser MD (2016). A meta-analysis of brief alcohol interventions for adolescents and young adults: Variability in effects across alcohol measures. The American Journal of Drug and Alcohol Abuse, 42, 140–151. doi: 10.3109/00952990.2015.1136638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, & Reed JE (2013). Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Quality & Safety. doi: 10.1136/bmjqs-2013-001862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner WC, Muck RD, Muck RJ, Stephens RL, & Sukumar B (2004). Co-occurring disorders in the adolescent mental health and substance abuse treatment systems. Journal of Psychoactive Drugs, 36, 455–462. doi: 10.1080/02791072.2004.10524428 [DOI] [PubMed] [Google Scholar]
- Van der Pol TM, Hoeve M, Noom MJ, Stams GJJ, Doreleijers TA, Domburgh L, & Vermeiren RR (2017). Research review: The effectiveness of multidimensional family therapy in treating adolescents with multiple behavior problems—A meta-analysis. Journal of Child Psychology and Psychiatry, 58, 532–545. doi: 10.1111/jcpp.12685 [DOI] [PubMed] [Google Scholar]
- VanDeMark NR, Burrell NR, LaMendola WF, Hoich CA, Berg NP, & Medina E (2010). An exploratory study of engagement in a technology-supported substance abuse intervention. Substance Abuse Treatment, Prevention, and Policy, 5, 10. doi: 10.1186/1747-597X-5-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron HB, & Turner CW (2008). Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology, 37, 238–261. doi: 10.1080/15374410701820133 [DOI] [PubMed] [Google Scholar]
- Walker DD, Stephens R, Roffman R, DeMarce J, Lozano B, Towe S, & Berg B (2011). A randomized controlled trial of motivational enhancement therapy with nontreatment-seeking adolescent cannabis users: A further test of the Teen Marijuana Check-Up. Psychology of Addictive Behaviors, 25, 474–484. doi: 10.1037/a0024076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Stephens RS, Blevins CE, Banes KE, Matthews L, & Roffman RA (2016). Augmenting brief interventions for adolescent marijuana users: The impact of motivational check-ins. Journal of Consulting and Clinical Psychology, 84, 983–992. doi: 10.1037/ccp0000094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz J, Bearman SK, Santucci LC, & Jensen-Doss A (2017). Initial test of a principle-guided approach to transdiagnostic psychotherapy with children and adolescents. Journal of Clinical Child & Adolescent Psychology, 46, 44–58. doi: 10.1080/15374416.2016.1163708 [DOI] [PubMed] [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman SK, … Gray J (2012). Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: a randomized effectiveness trial. Archives of General Psychiatry, 69(3), 274–282. doi: 10.1001/archgenpsychiatry.2011.147 [DOI] [PubMed] [Google Scholar]
- Weisz JR, Krumholz LS, Santucci L, Thomassin K, & Ng MY (2015). Shrinking the gap between research and practice: Tailoring and testing youth psychotherapies in clinical care contexts. Annual Review of Clinical Psychology, 11, 139–163. doi: 10.1146/annurev-clinpsy-032814-112820 [DOI] [PubMed] [Google Scholar]
- Winters KC, Fahnhorst T, Botzet A, Lee S, & Lalone B (2012). Brief intervention for drug abusing adolescents in a school setting: Outcomes and mediating factors. Journal of Substance Abuse Treatment, 42, 279–288. doi: 10.1016/j.jsat.2011.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Lee S, Botzet A, Fahnhorst T, & Nicholson A (2014). One-year outcomes and mediators of a brief intervention for drug abusing adolescents. Psychology of Addictive Behaviors, 28, 464–474. doi: 10.1037/a0035041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Harrop EN, Douglas H, Enkema M, & Sedgwick C (2014). Mindfulness-based treatment to prevent addictive behavior relapse: Theoretical models and hypothesized mechanisms of change. Substance Use & Misuse, 49, 513–524. doi: 10.3109/10826084.2014.891845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SS, Zhou B, Goebert D, & Hishinuma ES (2013). The risk of adolescent suicide across patterns of drug use: A nationally representative study of high school students in the United States from 1999 to 2009. Social Psychiatry and Psychiatric Epidemiology, 48, 1611–1620. doi: 10.1007/s00127-013-0721-z [DOI] [PubMed] [Google Scholar]


