Abstract
Objective
The 2019 novel coronavirus (COVID-19) is disproportionately impacting older individuals and healthcare workers. Otolaryngologists are especially susceptible with the elevated risk of aerosolization and corresponding high viral loads. This study utilizes a geospatial analysis to illustrate the comparative risks of older otolaryngologists across the United States during the COVID-19 pandemic.
Methods and materials
Demographic and state population data were extracted from the State Physician Workforce Reports published by the AAMC for the year 2018. A geospatial heat map of the United States was then constructed to illustrate the location of COVID-19 confirmed case counts and the distributions of ENTs over 60 years for each state.
Results
In 2018, out of a total of 9578 practicing U.S. ENT surgeons, 3081 were older than 60 years (32.2%). The states with the highest proportion of ENTs over 60 were Maine, Delaware, Hawaii, and Louisiana. The states with the highest ratios of confirmed COVID-19 cases to the number of total ENTs over 60 were New York, New Jersey, Massachusetts, and Michigan.
Conclusions
Based on our models, New York, New Jersey, Massachusetts, and Michigan represent states where older ENTs may be the most susceptible to developing severe complications from nosocomial transmission of COVID-19 due to a combination of high COVID-19 case volumes and a high proportion of ENTs over 60 years.
Keywords: COVID-19, Novel coronavirus 2019, Otolaryngology, Nosocomial transmission, Age
1. Introduction
The 2019 novel coronavirus (COVID-19) is a global pandemic that has rapidly spread across the world. Although the virus infects individuals of all ages, epidemiological reports demonstrate that older age is a significant contributing factor for symptomatic presentation, severe disease course, and death [1]. This is illustrated by the significant increase in case fatality rates (CFR) with age. In China, the CFR of the general populace is 2.3% with rates skyrocketing to 8.0% and 14.8% in patients 70–79 and over 80, respectively [2]. In Italy, reports of case fatality are even higher, with 8.6% in individuals 60–69 years, 12.8% in individuals 70–79 years, and 20.2% in individuals over 80 years [2].
In addition to age, nosocomial exposure also serves as a significant risk factor, rendering health care workers particularly susceptible. Early data from Wuhan, China reported that nearly 29% of COVID-19 infections in a single hospital system were comprised of health care workers [3]. The novel coronavirus' dramatic impact on medical personnel parallels the epidemiology of the 2003 severe acute respiratory disease (SARS) outbreak in which 21% of global cases were health care worker infections [4].
COVID-19 colonizes the upper respiratory mucosa with a high viral load, whether a patient is symptomatic or asymptomatic [5]. As COVID-19 demonstrates the potential for both respiratory and aerosol transmission, otolaryngologists (ENTs) are at an elevated risk working in close proximity to the upper respiratory tract within the head and neck region [6,7]. Due to the vast diversity in diagnostic and operative procedures performed on the upper airway within ENT, there is a high risk of aerosolization, leading to the potential for transmission of high viral loads to the provider [8]. The director of an intensive care unit in Wuhan, China commented that otolaryngologists and ophthalmologists were infected at higher rates when compared to other doctors in the same hospitals, and the same trends are reported in Europe [9]. In response, an international collaboration among thirteen institutions has put forth recommendations to ensure the safety of the otolaryngology community throughout the course of this pandemic [10].
Protecting vulnerable members of the work force during these unprecedented times is of the utmost importance. The present study compares the geospatial distribution of COVID-19 confirmed cases against the distribution of ENTs over the age of 60 to highlight the potential risks to this segment of vulnerable health care providers.
2. Methods
We utilized the State Physician Workforce Reports published by the American Association of Medical Colleges (AAMC) to extract demographic information on active ENT physicians during the year 2018 [11]. The resulting dataset included the number of total ENTs per state, the number of ENTs older than age 60 by state, the proportion of ENTs older than age 60, and the 2018 U.S. Census Bureau state populations. We subsequently calculated the ratio of state population per ENT provider for each state by dividing the total state population by the total number of ENTs for that state. Next, we obtained coordinates of all confirmed COVID-19 cases from a disease-specific data repository published by the Environmental Systems Research Institute (ESRI) [12]. Both datasets were then imported into the geospatial mapping software QGIS (version 3.12.1), and superimposed onto state boundary files published by the U.S. Census Bureau.
The percentage of ENTs above age 60 variable was used to group states into discrete quintiles with a graded color scheme for each quintile. Similarly, a logarithmic scale of confirmed COVID-19 case numbers was deployed to adjust the size of all coordinate data points to create a heat map demonstrating the distribution of ENTs over 60 years and the distribution of COVID-19 confirmed cases in the U.S. Determination of states with the highest risk for older otolaryngologists was assessed by dividing the total number of confirmed COVID-19 cases by the total number of otolaryngologists over the age of 60.
The number of ENTs over 60 in each state was totaled and averaged over all of the states within each U.S. census region (Midwest, Northeast, South, and West). A one-way ANOVA was performed to analyze statistical differences in the average proportion of ENTs over 60 across each census region.
The present study was considered exempt from the University Hospitals Cleveland Medical Center IRB approval process (Study 20200433).
3. Results
A total of 9578 practicing U.S. ENT surgeons were identified by AAMC in 2018; 3081 were older than 60 years (32.2%). The states with the highest proportion of ENTs over 60 years were documented along with the total number of ENTs for that state (Table 1 ). The proportion of ENTs over age 60 ranged from 25.9% in Kansas to 58.8% in Maine (Appendix A). Ratios representing the total state population divided by the number of total ENTs for that state were also documented (Table 1). Of the 20 states with the highest proportion of ENTs over 60 years, state populations per ENT provider ranged from 20,897 to 48,086 (Table 1).
Table 1.
Demographic information of ENTs in the states with the highest proportion of Otolaryngologists ≥60 yrs [n (%)].a
| State | Otolaryngologists ≥60 yrs [n (%)] | Total ENTs per state | State population per ENT provider |
|---|---|---|---|
| Maine | 20 (58.8) | 34 | 39,365 |
| Delaware | 12 (48.0) | 25 | 38,687 |
| Hawaii | 18 (43.9) | 41 | 34,646 |
| Louisiana | 93 (41.7) | 223 | 20,897 |
| Alabama | 69 (40.4) | 171 | 28,584 |
| Connecticut | 46 (40.0) | 115 | 31,067 |
| Rhode Island | 11 (39.3) | 28 | 37,761 |
| Nebraska | 25 (39.1) | 64 | 30,145 |
| New Mexico | 20 (38.5) | 52 | 40,293 |
| New Jersey | 98 (38.3) | 256 | 34,799 |
| Idaho | 16 (38.1) | 42 | 41,767 |
| New York | 272 (37.6) | 723 | 27,029 |
| West Virginia | 21 (37.5) | 56 | 32,247 |
| Oklahoma | 30 (36.6) | 82 | 48,086 |
| Florida | 210 (36.0) | 584 | 36,471 |
| Mississippi | 28 (35.9) | 78 | 38,289 |
| Pennsylvania | 139 (35.8) | 389 | 32,923 |
| Indiana | 60 (35.3) | 170 | 39,364 |
| Tennessee | 65 (35.1) | 185 | 36,595 |
| Washington | 77 (34.8) | 221 | 34,098 |
This table is organized by states with the highest percentage of ENTs over 60 years in descending order.
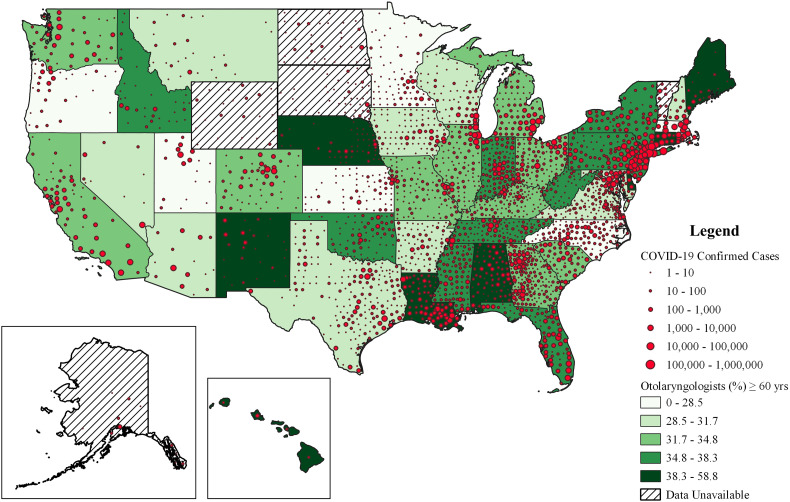
A heat map illustrating the U.S. states with the highest proportion of ENTs over 60 and the current geographic COVID-19 case volume was depicted in Fig. 1 . COVID-19 case volume was accurate as of April 14th, 2020. The highest risk states for older ENTs, defined by the ratio of total confirmed COVID-19 case volume to the total number of ENT providers over 60, were New York, New Jersey, Massachusetts, and Michigan, among others (Table 2 ). The highest number of confirmed COVID-19 cases per ENT over 60 years old was New York (721) and the lowest was Hawaii (28). Data for Vermont, North Dakota, South Dakota, Wyoming, and Alaska were not incorporated into the heat map as there were fewer than 10 ENT providers over 60 in each of these states, which was the AAMC's cut-off for publishing a given state's data.
Fig. 1.
Geographic distribution of older ENT's and COVID-19 confirmed case numbers.
Red bubbles reflect clusters of confirmed COVID-19 cases with sizes proportional to case number. The shading of states corresponds to percentage of ENT workforce over age 60 (with darker colors representing an older workforce). COVID-19 case volume data is accurate as of April 14th, 2020. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Table 2.
States with the highest ratios of COVID-19 confirmed cases to ENTs over the age of 60.a
| State | COVID-19 Cases per older ENT | COVID-19 case numbers | Otolaryngologists ≥60 yrs |
|---|---|---|---|
| New York | 721 | 196,146 | 272 |
| New Jersey | 659 | 64,584 | 98 |
| Massachusetts | 363 | 26,867 | 74 |
| Michigan | 320 | 25,635 | 80 |
| Connecticut | 291 | 13,381 | 46 |
| Rhode Island | 271 | 2976 | 11 |
| Louisiana | 226 | 21,016 | 93 |
| Nevada | 202 | 3031 | 15 |
| Illinois | 187 | 22,025 | 118 |
| Pennsylvania | 175 | 24,336 | 139 |
This table presents the top 10 states with the highest ratios of confirmed COVID-19 cases to ENT providers over 60. Data is accurate as of April 14th, 2020.
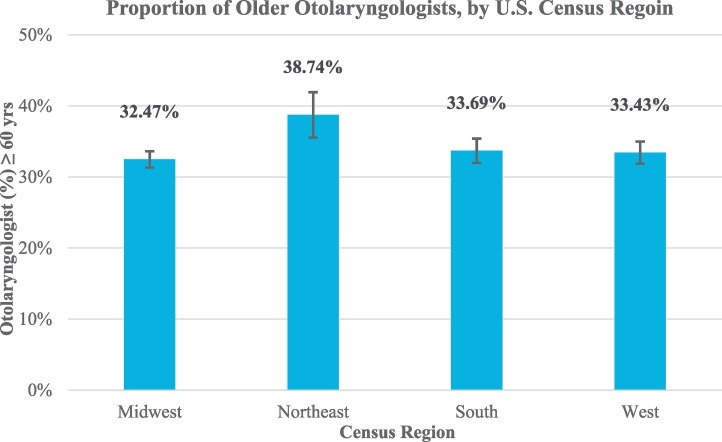
No statistically significant differences were found in the average proportion of ENTs over 60 by U.S. Census region (Fig. 2 ). The average percentages within the Midwest, Northeast, South, and West were 32.5%, 38.7%, 33.7%, and 33.4%, respectively (p = .38).
Fig. 2.
Average State Proportion of Older Otolaryngologists, by U.S. Census Region.
Additional demographic data for U.S. otolaryngologists and COVID-19 case counts for all 50 states is documented in the Appendix A.
4. Discussion
The present study illustrates the risk of older otolaryngologists during the COVID-19 pandemic. Our geospatial analysis demonstrates the U.S. states with both high combined confirmed COVID-19 cases and proportions of ENTs over 60 years, highlighting a segment of the healthcare workforce that could be at elevated risk of developing severe complications secondary to nosocomial transmission.
According to our findings, Maine, Delaware, Hawaii, and Louisiana have the highest proportions of ENTs over 60. However, with the exception of Louisiana, reported COVID-19 cases have been relatively low in these states. Therefore, ENT providers in these states may not be experiencing the same extent of viral exposure within healthcare settings as providers serving in New York, New Jersey, Massachusetts, and Michigan, which currently have the highest ratios of confirmed COVID-19 cases to the number of ENT providers over 60 years. These states will likely continue to be vulnerable with anticipated rises in case volumes or in the setting of a COVID-19 re-emergence.
Rates of nosocomial transmission and the susceptibility of all health care providers during this pandemic is frightening [13]. However, with careful precautions, it is possible to limit the risk unto health care workers and curb nosocomial transmission. With the proper personal protective equipment and adequate hand hygiene, a cohort of 41 health care workers was able to avoid nosocomial transmission while treating a confirmed COVID-19 patient with pneumonia despite exposure during ICU intubation and mechanical ventilation [14]. Various safety recommendations for ENTs during the COVID-19 pandemic have been proposed to achieve similarly successful outcomes.
For otolaryngologists specifically, routine, nonurgent appointments and elective surgeries have largely been postponed [10]. Some have recommended deferring all endoscopies unless deemed necessary to reduce 30-day morbidity, such as circumstances pertaining to malignancy and airway risk, among others [15]. For essential urgent and emergent procedures, which must proceed despite the risks, determination of whether to use powered air-purifying respirators (PAPRs) versus N95s should be assessed by each institution as both forms of masks offer distinct advantages and disadvantages [16]. However, at a minimum, otolaryngologists should don a respirator, gown, cap, eye protection, and gloves [17]. Moreover, studies from the Ebola outbreak reported that in some circumstances, up to 79.2% of providers self-contaminated while removing PPE [18]; therefore, careful consideration must be applied to doffing PPE during the COVID-19 pandemic.
Even after exercising adequate precautions, it is sensible to recommend that vulnerable demographics limit their exposure to possible COVID-19 infection as much as possible [19]. As rates of new cases start to decrease, otolaryngologists who are highly susceptible to severe complications from nosocomial transmission should exercise caution in their “return-to-work” planning in the coming weeks.
5. Limitations
The present study assesses the comparative risk of older otolaryngologists developing severe symptoms from COVID-19. However, there are many other variables that would need to be factored into this discussion to adequately predict the risks to ENTs in the United States. First, in addition to age, clinical comorbidities, male sex, and smoking history also play significant roles in the risk of developing severe complications secondary to COVID-19 infection [20]. Furthermore, risk of exposure is also highly dependent on local institutional practices, availability of resources such as personal protective equipment, and the scope of the hospital staff available to assist in the care for COVID-19 patients [21], which are not factored into our model. Although the provider data from 2018 was the most recent data available from the AAMC, it may not exactly reflect the current workforce in each state, since there may have been movement or retirements since the data was released in 2018.
6. Conclusions
Across the world, countries have reported the disproportionate impact of COVID-19 on older individuals and health care workers. With otolaryngologists at increased susceptibility due to the nature of their work and the type of procedures they perform, protocols must be implemented to protect otolaryngologists, especially those most vulnerable. It is vital that, as the nation starts to recover from the COVID-19 pandemic, we evaluate how best older ENTs can serve while limiting their risk of exposure.
Funding
None.
Declaration of competing interest
None.
Appendix A.
| State | Otolaryngologists ≥60 yrs. [n (%)] | Total ENTs | COVID-19 cases | COVID-19 cases per older ENT (>60 years) |
|---|---|---|---|---|
| New York | 272 (37.6) | 723 | 196,146 | 721 |
| New Jersey | 98 (38.3) | 256 | 64,584 | 659 |
| Massachusetts | 74 (28.5) | 260 | 26,867 | 363 |
| Michigan | 80 (33.2) | 241 | 25,635 | 320 |
| Connecticut | 46 (40) | 115 | 13,381 | 291 |
| Rhode Island | 11 (39.3) | 28 | 2976 | 271 |
| Louisiana | 93 (41.7) | 223 | 21,016 | 226 |
| Nevada | 15 (31.3) | 48 | 3031 | 202 |
| Illinois | 118 (33.8) | 349 | 22,025 | 187 |
| Pennsylvania | 139 (35.8) | 389 | 24,336 | 175 |
| District of Columbia | 13 (27.7) | 47 | 1955 | 150 |
| Delaware | 12 (48) | 25 | 1761 | 147 |
| Indiana | 60 (35.3) | 170 | 8368 | 139 |
| Washington | 77 (34.8) | 221 | 10,725 | 139 |
| Georgia | 105 (34.4) | 305 | 13,621 | 130 |
| Colorado | 61 (33.2) | 184 | 7696 | 126 |
| Maryland | 71 (29.5) | 241 | 8936 | 126 |
| Texas | 116 (31.3) | 722 | 14,505 | 125 |
| Mississippi | 28 (35.9) | 78 | 2942 | 105 |
| Florida | 210 (36) | 584 | 21,019 | 100 |
| Utah | 24 (26.4) | 91 | 2363 | 98 |
| Idaho | 16 (38.1) | 42 | 1464 | 92 |
| Tennessee | 65 (35.1) | 185 | 5610 | 86 |
| Virginia | 72 (29.5) | 244 | 5828 | 81 |
| New Hampshire | 13 (31.7) | 41 | 1020 | 78 |
| Arizona | 48 (31.6) | 152 | 3705 | 77 |
| South Carolina | 46 (32.6) | 141 | 3439 | 75 |
| Missouri | 61 (33.5) | 182 | 4531 | 74 |
| Oklahoma | 30 (36.6) | 82 | 2069 | 69 |
| Arkansas | 22 (30.8) | 72 | 1480 | 67 |
| New Mexico | 20 (38.5) | 52 | 1345 | 67 |
| Kansas | 21 (25.9) | 81 | 1391 | 66 |
| Wisconsin | 52 (31.7) | 164 | 3428 | 66 |
| Ohio | 109 (33.1) | 330 | 6975 | 64 |
| Iowa | 27 (30.7) | 88 | 1710 | 63 |
| California | 388 (32.6) | 1189 | 24,372 | 63 |
| North Carolina | 85 (26.5) | 321 | 5007 | 59 |
| Alabama | 69 (40.4) | 171 | 3803 | 55 |
| Kentucky | 39 (34.8) | 112 | 2048 | 53 |
| Oregon | 38 (27.1) | 140 | 1584 | 42 |
| Montana | 10 (30.3) | 33 | 394 | 39 |
| Minnesota | 43 (28.5) | 151 | 1650 | 38 |
| Maine | 20 (58.8) | 34 | 698 | 35 |
| Nebraska | 25 (39.1) | 64 | 871 | 35 |
| West Virginia | 21 (37.5) | 56 | 633 | 30 |
| Hawaii | 18 (43.9) | 41 | 504 | 28 |
| Vermont | * | 21 | 752 | * |
| South Dakota | * | 28 | 868 | * |
| North Dakota | * | 14 | 331 | * |
| Wyoming | * | 16 | 275 | * |
| Alaska | * | 31 | 277 | * |
*The is stratified by the highest ratios of confirmed COVID-19 cases to ENT providers over 60 years in descending order. Data is accurate as of April 14th, 2020.
References
- 1.Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. BMJ. 2020;368 doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 2.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 3.Wang D. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnston L.B., Conly J.M. Severe acute respiratory syndrome: what have we learned two years later? Can J Infect Dis Med Microbiol. 2004;15(6):309–312. doi: 10.1155/2004/964258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zou L. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel Z., Fernandez-Miranda J., Hwang P., Nayak J., Dodd R., Sajjadi H. Precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery. 2020 doi: 10.1093/neuros/nyaa125. [published online ahead of print, 2020 Apr 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kowalski L.P. COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020 doi: 10.1002/hed.26164. [published online ahead of print, 2020 Apr 9] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tysome J.R., Bhutta M.F. COVID-19: protecting our ENT workforce. Clin Otolaryngol. 2020;45(3):311–312. doi: 10.1111/coa.13542. [DOI] [PubMed] [Google Scholar]
- 9.Europe's doctors repeat errors made in Wuhan, China medics say. March 16, 2020. https://www.bloomberg.com/news/articles/2020-03-17/europe-s-doctors-getting-sick-like-in-wuhan-chinese-doctors-say URL.
- 10.Givi B., Schiff B.A., Chinn S.B. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0780. [published online ahead of print, 2020 Mar 31] [DOI] [PubMed] [Google Scholar]
- 11.Association of American Medical Colleges, 2019 State physician workforce data report, in AAMC. vol. 2019: Washington, DC.
- 12.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;S1473-3099(20):30120–30121. doi: 10.1016/S1473-3099(20)30120-1. [published online ahead of print, 2020 Feb 19] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (covid-19) outbreak in china: summary of a report of 72-314 cases from the chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [published online ahead of print, 2020 Feb 24] [DOI] [PubMed] [Google Scholar]
- 14.Ng K., Poon B.H., Kiat Puar T.H. COVID-19 and the risk to health care workers: a case report. Ann Intern Med. 2020 doi: 10.7326/L20-0175. L20-0175. [published online ahead of print, 2020 Mar 16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vukkadala N., Qian Z.J., Holsinger F.C., Patel Z.M., Rosenthal E. COVID-19 and the otolaryngologist: preliminary evidence-based review. Laryngoscope. 2020 doi: 10.1002/lary.28672. [published online ahead of print, 2020 Mar 26] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wax R.S., Christian M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Directives concrètes à l’intention des équipes de soins intensifs et d’anesthésiologie prenant soin de patients atteints du coronavirus 2019-nCoV. Can J Anaesth. 2020;67(5):568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan J.Y.K., Wong E.W.Y., Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemic: an experience in Hong Kong. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0488. [published online ahead of print, 2020 Mar 20] [DOI] [PubMed] [Google Scholar]
- 18.Suen L.K.P. Self-contamination during doffing of personal protective equipment by healthcare workers to prevent Ebola transmission. Antimicrob Resist Infect Control. 2018;7:157. doi: 10.1186/s13756-018-0433-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li T. Diagnosis and clinical management of severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection: an operational recommendation of Peking Union Medical College Hospital (V2.0) Emerg Microbes Infect. 2020;9(1):582–585. doi: 10.1080/22221751.2020.1735265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen T. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020 doi: 10.1001/jama.2020.3972. [published online ahead of print, 2020 Mar 12] [DOI] [PubMed] [Google Scholar]